The NT-proBNP assay identifies very elderly nursing home residents suffering from pre-clinical heart failure
Abstract
Background
Little is known about the prevalence of heart failure among very old people, although hospitalisation rates for chronic heart failure are very high. Recently, brain natriuretic peptides have emerged as important diagnostic and prognostic serum markers for congestive heart failure.
Aims
The main purpose of our study was to determine whether there is a cut-off for NT-proBNP for detecting the echocardiographic features of left ventricular systolic and/or diastolic dysfunction and clinical heart failure among old people living in nursing homes. Secondarily, we investigated the medium-term prognostic power of the neurohormone levels.
Methods
We screened 101 old people (80% females, aged 84±9 years) from two nursing homes. We prospectively evaluated whether we could effectively stratify patients using a combination of (1) restrictive clinical criteria, (2) NT-proBNP measurements (Elecsys System, Roche Diagnostics) and (3) echocardiography for all patients.
Results
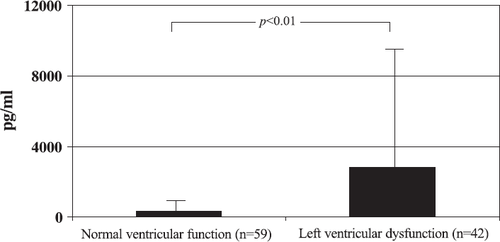
Forty-two percent of the subjects had left ventricular dysfunction: 11% systolic, 23% diastolic and 8% both systolic and diastolic. The mean NT-proBNP concentration was 2806±7028 pg/ml in the 42 patients with left ventricular systolic and/or diastolic dysfunction, compared with 365±456 pg/ml in the 59 patients with normal left ventricular function (p<0.01, Z=−4.8 Mann–Whitney U test). The neurohormone proved to be a good predictor of events within 6 months [area under the receiver-operated curve (ROC)=0.79].
Conclusions
Blood NT-proBNP concentrations can play an important role in stratifying old people into left ventricular dysfunction risk groups. The neurohormone is an independent marker for death or admission for heart failure in the medium term.
1. Introduction
Heart failure is a frequent cause of hospitalisation. There were 139,659 cases in Italy in the year 2000, accounting for a total of 1,424,522 days of hospitalisation (http://www.ministerosalute.it). Hospitalisation rates are very high among the elderly population, which accounts for 70% of admissions for chronic heart failure 1 and also presents high percentages of short-term readmission to hospital: up to 50% after 3–6 months 2. This is particularly true of nursing home residents, among whom the prevalence of heart failure is very high, the application of Guideline recommendations 3 insufficient and hospitalisation rates worrying 4,5. In particular, in our Local Health District (ASL 10—“East Venetia”), which has a population of 198,000, there were 546 admissions for chronic heart failure in the year 2000, which is 2.75 admissions per 1000 inhabitants. However, among the 400 residents of a nursing home in the same LHD, the hospitalisation rate was 6%. This means that 0.2% of the population accounted for 4% of total hospital admissions for heart failure. Finally, the prognosis quoad vitam of nursing home residents after hospitalisation for heart failure is very poor 6.
It is now widely accepted that rationalisation and full application of behavioural, dietary and therapeutic measures for heart failure patients can significantly improve their clinical history (see Refs. 7,8 for review), with particularly good results in the elderly 9. New drugs (beta-blockers 10 11 12 and spironolactone 13) and traditional drugs (ACE inhibitors 14,15 and digoxin 16) have been proven to have a significant effect on survival and hospitalisation rates.
Screening tests for left ventricular systolic and/or diastolic dysfunction among high-risk subjects 17 (such as frail elderly nursing home residents 4,5) are therefore required to enable implementation of intervention protocols to limit the pandemic increase in hospitalisation for chronic heart failure . It is well known that the clinical criteria for diagnosis of heart failure are unsatisfactory, due to the high percentage of false positives, leading to an explosion in costs, as has been demonstrated by “open access” echocardiography studies 18 19 20. Hence, there is a need for a cheaper, more accessible and widespread mass screening tests, which would improve the efficiency of the system by excluding as many false positives as possible from echocardiography tests.
Recently, natriuretic peptides (BNP and NT-proBNP) have been shown to be a powerful diagnostic tool for both asymptomatic left ventricular systolic and/or diastolic dysfunction and overt heart failure 21 22 23 24 25 26. Normal values of this neurohormone almost rule out the possibility of underlying left ventricular dysfunction, its negative predictive value being close to 100% 21 22 23 24 25 26. BNP (and its N-terminal fragment NT-pro-BNP) are secreted by the ventricles in the event of a volume or pressure overload 27,28. The plasma concentrations of BNP and NT-proBNP increase in asymptomatic and symptomatic systolic and diastolic dysfunction, and are reduced after treatment with drugs of proven efficacy in heart failure 29 30 31 32 33 as a result of the improvement in filling pressures 34,35. This latter aspect helps to explain the recently reported association between BNP values and the short/medium-term prognosis in patients suffering from heart failure (see Ref. 36 for review), which suggests its use as a prognostic stratification tool in various clinical scenarios. Although the prognostic role of natriuretic peptides is very promising, knowledge is still limited, especially in the case of elderly people (see Ref. 36 for review).
That being said, the main purpose of our study was to determine whether a cut-off exists for NT-pro BNP in detecting the echocardiographic features of left ventricular systolic and diastolic dysfunction among elderly nursing home residents, using a combined approach: clinical screening with “restrictive” criteria+NT-proBNP assay+echocardiography examination. Secondarily, we investigated the medium-term prognostic power of the neurohormone.
2. Methods
2.1. Subjects
The residents of the Caorle and San Donà di Piave (Venetia-NE Italy) nursing homes were studied (n=101). The characteristics of the population studied are reported in Table 1 and were described in an earlier paper 5 for residents in 1999–2000.
2.2. Clinical screening for heart failure
A review of the clinical documentation of residents of the nursing home identified 16 persons suffering from heart failure on the basis of clinical screening, based on only two criteria: (1) prior hospitalisation for chronic heart failure; and (2) prior instrumental diagnosis of left ventricular systolic and/or diastolic dysfunction.
2.3. NT-proBNP
All subjects were given blood tests to assay NT-proBNP, and the samples were immediately analysed with the Elecsys method (Roche). This is an immuno-chemo-luminescence method which requires a plasma volume of 10 μl (200 μl in case of automatic aspiration), with a lower detection limit of 5 pg/ml. The assay is completed in 15 min, and the approximate cost is 28 Euros per determination 37.
2.4. Echocardiography
Echocardiography tests were conducted during the first evaluation with a portable Sonosite machine, before the determination of NT-proBNP. Left ventricular systolic dysfunction was defined as an ejection fraction (EF)<50%. For the diagnosis of diastolic dysfunction one of the following patterns was required: (1) impaired relaxation (E/A<0.8 and deceleration time >140 ms in subjects >55 years old); (2) pseudonormal (1<E/A<2 and DT>140 ms; diastolic wave of pulmonary veins on Doppler test superior to the systolic wave for differentiation from the normal pattern); (3) restrictive (E/A>2 and DT≤140 ms) 38. The presence of one of these patterns, in the presence of a normal EF (>50%), was defined as isolated diastolic dysfunction. In patients suffering from atrial fibrillation at the time of the echocardiogram, diastolic function was classified as: (1) restrictive pattern (DT≤140 ms) or (2) indeterminate (DT>140 ms).
2.5. Clinical diagnosis of heart failure
Patients were also classified on the basis of their symptoms, to establish the prevalence of clinically manifested heart failure. The diagnosis was made on the basis of criteria widely accepted in the literature 39, namely the presence of two major criteria or one major criterion+two minor criteria according to the Framingham score.
2.6. The prognostic value of NT-proBNP
In the 6 months after determination of NT-proBNP, we recorded (for all residents of the nursing home) deaths, hospitalisations for chronic heart failure (DRG 127) and cases of acute heart failure treated by the nursing home's doctor on the premises, without hospitalisation. In view of the small size of the sample, the three types of event were used as a combined endpoint for the purpose of the subsequent analyses.
3. Cost analysis
Only direct costs were measured. The Ministry of Health Tariff Scale was used to quantify the value of the instrumental examinations 40. A recent estimate taken from the literature was used for the cost of NT-proBNP 37.
4. Statistics
The data are expressed as mean±standard deviation. A value of p<0.05 was considered significant. As the data did not have a normal distribution, we used the Mann–Whitney U test to compare the samples, while the Spearman test was used for the correlations. The association between variables was verified with Fisher's exact test. Logistic multivariate regression analysis was used to examine the relation of clinical variables, BNP levels, and echocardiographics parameters with the incidence of the combined endpoint during the 6 months after discharge. A receiver-operated curve (ROC) was traced to test whether NT-proBNP values could be used to identify patients with left ventricular systolic and/or diastolic dysfunction among a general population of frail elderly persons.
5. Results
5.1. Clinical and demographic characteristics
Table 1 sets out the demographic, clinical, laboratory and instrumental characteristics of the patients identified as suffering from left ventricular systolic and/or diastolic dysfunction and the remaining members of the sample studied. The population in question had a very high average age (84±9, range: 56–100), were mainly female (80%) and suffered from numerous co-morbidities, especially diabetes mellitus (10%), atrial fibrillation (8%), COPD (3%) and renal failure (2%). Of the sample, 7% and 27% suffered from ischaemic heart disease and hypertension respectively, and 6% of the population were affected by valve disease (Table 1). Most of the patients were asymptomatic; only 23% complained of dyspnoea and/or ankle oedema (Table 1). The prescription of drugs of proven efficacy was high, demonstrating a class “B” population 41 with a high prevalence of cardiovascular disease, known to the local health facilities (Table 1). The patients suffering from ventricular dysfunction differed from the others in terms of age, functional class, history of valve disease and hypertension, presence of atrial fibrillation, prior clinical diagnosis of heart failure and drug prescription (Table 1).
| Parameter | Left ventricular systolic and/or diastolic dysfunction (n=42) | Normal ventricular function (n=59) | All (n=101) |
|---|---|---|---|
| Age (years) | 87±7 | 81±10** | 84±9 |
| Male gender (%) | 12 | 25 | 20 |
| NYHA functional class | 1.7±1.0 | 1.2±0.5** | 1.4±0.8 |
| Clinical diagnosis of heart failure (%) | 31 | 2a | 16 |
| Echocardiographic parameters (%) | |||
| Systolic dysfunction (EF<50 %) | 26 | – | 11 |
| Isolated diastolic dysfunction | 55 | – | 23 |
| Impaired relaxation pattern | 38 | – | 16 |
| Pseudonormal pattern | 10 | – | 4 |
| Restrictive pattern | 7 | – | 3 |
| Systodiastolic dysfunction | 19 | – | 8 |
| NT-proBNP (pg/ml) | 2806±7028 | 365±456** | 1380±4672 |
| Co-morbidities (%) | |||
| Ischaemic heart disease | 12 | 4 | 7 |
| Hypertension | 32 | 24 | 27 |
| Valve disease | 12 | 0a | 6 |
| Atrial fibrillation | 17 | 2a | 8 |
| Kidney failure (creatinine>2.5 mg/dl) | 5 | 0 | 2 |
| COPD | 0 | 5 | 3 |
| Diabetes mellitus | 10 | 9 | 10 |
| Current treatment (%) | |||
| ACE inhibitors | 44 | 15a | 28 |
| Angiotensin receptor blockers | 0 | 8b | 6 |
| Beta-blockers | 7 | 6 | 6 |
| Spironolactone | 10 | 6 | 7 |
| Digitalis | 22 | 8b | 14 |
| Furosemide and thiazide diuretics | 30 | 22 | 26 |
- a Data are expressed as mean±S.D.
- * p<0.05; Mann–Whitney U test.
- ** p<0.01 Mann-Whitney U test.
- a p<0.01; Fisher's exact test.
- b p<0.05; Fisher's exact test.
5.2. Prevalence of left ventricular systolic and diastolic dysfunction
A total of 42 patients out of 101 (42%) were diagnosed as suffering from left ventricular systolic and/or diastolic dysfunction. Of these patients, systolic insufficiency represented 26% of the total, whereas diastolic insufficiency accounted for 55% and systo-diastolic insufficiency for 19%. Eight patients presented a restrictive diastolic pattern, and in five cases this was combined with a reduced ejection fraction. The aetiology was largely associated with hypertension, and to a lesser extent with ischaemic or valvular heart disease (Table 1). The distribution of the 42 left ventricular dysfunction patients by NYHA class was as follows: 62% in I, 14% in II, 17% in III and 7% in IV.
5.3. Prevalence of clinical heart failure
A clinical diagnosis of heart failure (based on the restrictive criteria set out above) was made in 16 cases (16%), 4 of them (4%) on the basis of a prior instrumental diagnosis of left ventricular systolic and/or diastolic dysfunction and 12 (12%) on the basis of prior hospitalisation for chronic heart failure. However, three of the latter proved not to suffer from left ventricular systolic and/or diastolic dysfunction when the echocardiogram was performed. The prevalence of symptomatic ventricular dysfunction in the study sample was therefore 13%. The distribution of the 13 patients with a previous diagnosis of heart failure (and documented left ventricular systolic and/or diastolic dysfunction) by NYHA class was as follows: 39% in I–II, 61% in III–IV. Of these patients, systolic insufficiency represented 23% of the total, whereas diastolic insufficiency accounted for 39% and systodiastolic insufficiency for 38%.
5.4. NT-proBNP and echocardiography
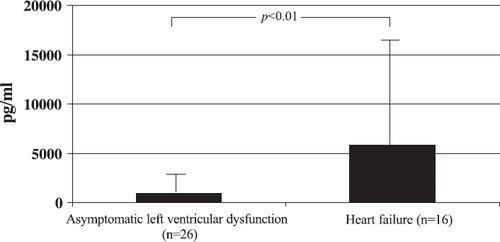
The average value of NT-proBNP in the study population was 1380±4672 pg/ml (range: 14–35000 pg/ml); the NT-proBNP values proved to be correlated with age and NYHA class (Spearman's Rho=0.443, p<0.01 and 0.403, p<0.01, respectively). The NT-proBNP values were lower in the 59 patients with normal ventricular function (365±456 pg/ml) than in the 42 patients with left ventricular systolic and/or diastolic dysfunction (2806±7028 pg/ml; Z=−4.78; p<0.01; Mann–Whitney U test, fig. Fig. 1). There was also a difference in relation to symptoms, which were associated with higher NT-proBNP values (5853±10589 (n=16) vs. 930±2030 (n=26); Z=−3.19; p<0.01; Mann–Whitney U test, fig. Fig. 2). In the patients with left ventricular dysfunction, the NT-proBNP value also varied according to the type of dysfunction, being lower in diastolic (n=23; 452±361 pg/ml) than systolic dysfunction (n=19; 5655±9833 pg/ml; Z=−4.4; p<0.01; Mann–Whitney U test). In the ambit of isolated diastolic dysfunction (n=23), the NT-proBNP values were higher in the 3 patients with a restrictive pattern than in the other 20 (1132±307 vs. 349±239 pg/ml, Mann–Whitney U test Z=−2.66, p<0.01).
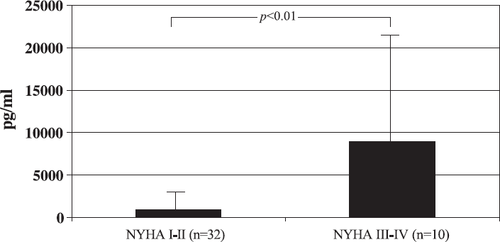
Among the patients diagnosed as suffering from patent heart failure, the NT-proBNP values were also directly correlated with NYHA class (Spearman's Rho=0.527, p<0.01), as the values of the neurohormone increased with functional class: NYHA I–II=890±1830 pg/ml (n=32), NYHA III–IV=8935±12596 pg/ml (n=10) (Z=−3.57; p<0.01, Mann–Whitney U test; fig. Fig. 3).
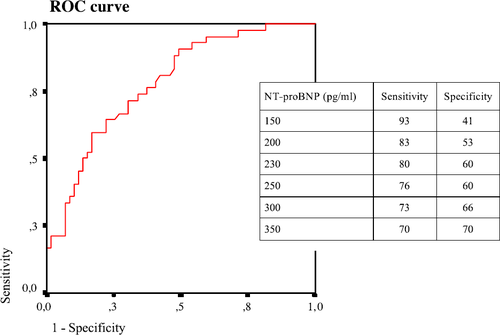
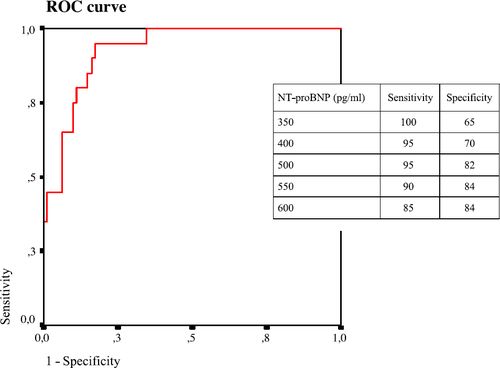
5.5. Cut-off values on ROC analysis
The capacity of NT-proBNP to distinguish between subjects with and without left ventricular systolic and/or diastolic dysfunction is illustrated by the ROC curve in fig. Fig. 4. The value of 0.78 (with a confidence interval of 0.69–0.87) for the area under the curve indicates an acceptable discriminating power. Some cut-off values are proposed; in particular, an NT-proBNP value of 230 pg/ml has a sensitivity of 80% and a specificity of 60% (fig. Fig. 4). If the test is restricted to distinguishing patients with systolic and/or serious diastolic dysfunction (restrictive pattern) from those with slight (impaired relaxation pattern) or moderate (pseudonormal pattern) isolated diastolic dysfunction and those with no left ventricular dysfunction, the NT-proBNP values demonstrate an excellent discriminating power. The associated ROC curve (fig. Fig. 5) has an area under the curve of 0.93 (confidence interval 0.88–0.98), and an NT-proBNP value of >500 pg/ml has a sensitivity of 95% and a specificity of 82% in identifying these subjects.
5.6. Cost–efficacy analysis
Review of the prior clinical documentation enabled a diagnosis of heart failure to be made in 16 subjects (16% of cases), on the basis of the two criteria used (1—prior hospitalisation for chronic heart failure; 2—prior instrumental diagnosis of left ventricular systolic and/or diastolic dysfunction). In the remaining 85 patients (84%), a high NT-proBNP value (using a cut-off value of 230 pg/ml) was found in 57 cases (57% of the total). A screening examination for the diagnosis of heart failure in frail elderly persons which subordinates echocardiography to clinical evaluation and analysis of pathological NT-proBNP values (>230 pg/ml) would have referred 51 of the 100 subjects examined for echocardiography. The introduction of such screening would considerably reduce the costs of the model: from 10,300 to 7605 per 100 patients examined. Moreover, the application of a cut-off value of 230 pg/ml, which identifies 80% of the subjects suffering from left ventricular systolic and/or diastolic dysfunction (presenting the best accuracy (Table 2)), would mean “missing” 20 cases out of 100, and including 3 false positives for heart failure among the patients with clinical criteria. However, this approach would avoid 49 echocardiograms for every 100 patients studied, with a cost saving of 26% on the entire model (Table 2).
| Examination | Number of patients | Unit cost () | Total cost () |
|---|---|---|---|
| Echocardiographic approach | |||
| Echocardiogram | 100 | 103 | 10,300 |
| Total cost per 100 patients | 10,300 | ||
| Present approach | |||
| BNP>230 pg/ml (51% of patients) | |||
| Positive case history of heart failure | 16 | – | – |
| BNP assay | 84 | 28 | 2352 |
| Echocardiogram | 51 | 103 | 5253 |
| Total cost per 100 patients | 7605 | ||
| Total saving per 100 patients studied | 2695 |
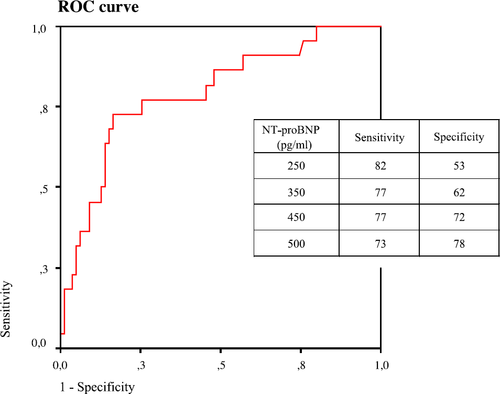
5.7. NT-proBNP and prognosis
During the 6-month follow-up we recorded 15 deaths and 2 hospitalisations for acute pulmonary oedema, while 5 more patients presented acute heart failure but were successfully treated in the nursing home. The NT-proBNP values of those who presented one of these events (n=22) were 3571±7747 pg/ml vs. 770±3177 pg/ml for the remaining patients (Z=−3.0; p<0.01; Mann–Whitney U test). The ability of the BNP values to discriminate between patients with events and event-free patients is illustrated by the ROC curve in fig. Fig. 6. The value of 0.79 for the area under the curve indicates an acceptable discriminating power (confidence interval 0.68–0.90). Some cut-off values have been proposed, but an NT-proBNP value of 350 pg/ml seems to represent the best compromise for risk stratification, with sensitivity and specificity values of 77% and 62% respectively. Finally, Table 3 shows the superiority of NT-proBNP as a prognostic index compared with the variables normally used for prognostic purposes, as demonstrated by multivariate regression analysis, which confirms that the values of the neurohormone are the only significant predictor of events (OR=8.3; p<0.05).
| Variable | Significance | OR |
|---|---|---|
| NT-proBNP (first tertile: 112±45; 14–176 pg/ml) | 0.055 | – |
| NT-proBNP (second tertile: 318±107; 182–492 pg/ml) | 0.431 | – |
| NT-proBNP (third tertile: 3672±7613; 494–35000 pg/ml) | 0.028 | 8.302 |
| Age (years) | 0.215 | – |
| Systolic dysfunction (no vs. yes) | 0.331 | – |
| Restrictive pattern (no vs. yes) | 0.334 | – |
| Previous diagnosis of heart failure (no vs. yes) | 0.678 | – |
| NYHA class (1 vs. 2–4) | 0.328 | – |
| Left ventricular systolic and/or diastolic dysfunction (no vs. yes) | 0.264 | – |
6. Discussion
6.1. Problems associated with the prevalence and current approach to chronic heart failure and its identification
The pandemic trend in the last decade and demographic projections for the future classify heart failure as the cardiovascular disease with the greatest financial burden. Heart failure currently absorbs 1–2% of the health budgets of countries comparable to Italy 42. Increased demand for health care has led to a greater investment in managerial intervention strategies designed to limit health spending and partially redistribute resources. The current cost of hospitalisation for the higher NYHA classes (III–IV) alone is five times greater than for the lower classes 43.
In therapeutic terms, studies of new drugs (beta-blockers 10 11 12 and spironolactone 13) and traditional pharmacological treatments (ACE inhibitors 14,15) and digoxin 16 have led to a significant reduction in the morbidity and mortality of patients with manifest heart failure. However, little is done for patients in the early stages, when the same action could potentially inhibit the progression of the disease. The importance of early identification of heart failure in order to implement measures of proven efficacy and influence the clinical outcome was recently confirmed 17, although in patients with isolated diastolic dysfunction (well represented by our sample), it is not clear that any drug intervention changes the prognosis 44.
In the real world, making a correct diagnosis of heart failure is still problematic, because the specificity of the signs and symptoms is limited, especially in the early stages when decompensation is slight. In most cases, diagnostic confirmation is based on a subsequent instrumental examination, especially echocardiography. In all the studies conducted on the subject, especially those on “open access” echocardiography 18 19 20, the patient selection criteria proved unsatisfactory, with a high percentage of false positives and a resulting cost explosion.
Only half of the cases with an initial diagnosis of heart failure are subsequently confirmed when an instrumental examination is performed. This can be explained by the fact that in routine clinical practice this type of patient (ideally at the stage of transition from class “B” to class “C” of the ACC/AHA guidelines 2001) 41 is difficult to identify, and frequently not recognised. In elderly patients in particular, the diagnostic difficulty is increased by the low specificity of the symptoms (e.g., effort dyspnoea and fatigue) and the presence of co-morbidity (COPD).
Finally, the design of a screening programme requires the availability of a cheaper, more accessible and widespread diagnostic test than echocardiography, which would improve the managerial efficiency of the system by excluding as many false positives for heart failure as possible. If a process similar to that for ischaemic heart disease and oncology is followed, the choice might fall on a specific biohumoral test which would reliably exclude the diagnosis of heart failure in a pre-defined clinical context in patients at risk of heart failure.
6.2. Managerial efficiency of NT-proBNP as a first screening test
Although progress has been made, there are a number of problems associated with selection of the most appropriate test for the diagnosis of heart failure. The clinical diagnosis of new-onset heart failure inevitably involves general practitioners; however, due to cultural and organisational problems which are currently (and in the immediate future) almost insuperable, the patient is generally referred for instrumental confirmation when the disease is already manifest 45. Moreover, in nursing homes, adherence to the guidelines for diagnostic investigations and treatment is notoriously lax 4,5. However, correct diagnosis of a disease is the first necessary step towards its treatment. The availability of a practical, relatively inexpensive test for the early screening of patients which can easily be performed locally could help solve this problem.
According to data obtained from population studies, the use of neurohormonal markers for routine screening of asymptomatic ventricular dysfunction does not appear to be a practical strategy (see Ref. 46 for review). Our research suggests that as the first screening test for elderly patients, the NT-proBNP assay rules out the presence of left ventricular systolic and/or diastolic dysfunction with an excellent degree of accuracy for values under 230 pg/ml, and could represent a guide for general practitioners when referring the patient for further instrumental examinations. This type of approach would reduce the number of patients referred for echocardiograms, limiting the poor managerial efficiency of “open access” echocardiography, which is usually characterised by a high rate of false positives due to poor selection of candidates 18 19 20.
In strictly financial terms, a cut-off value of 230 pg/ml would identify 80% of symptomatic heart failure patients and reduce health spending by 26%: from 10,300 to 7605 for every 100 patients studied. Having established that 100 residents of a nursing home account for 18 chronic heart failure admissions per annum 5, each costing 2206 (estimated on the basis of the corresponding DRG 127 tariff), it would be sufficient to reduce such admissions by 10% with a dedicated programme to achieve managerial efficiency, thereby offsetting the costs of a screening programme like the present one. It should be borne in mind that in the present study, the combination of NT-proBNP+echocardiography demonstrated a 42% prevalence of left ventricular systolic and/or diastolic dysfunction, whereas an earlier survey conducted on the same population with clinical criteria, estimated the prevalence of manifest heart failure at 23%. The subsequent intervention programme conducted on patients identified as suffering from heart failure in the year 2000 entirely prevented readmission to hospital, but five patients not identified by the clinical survey were hospitalised the following year, demonstrating the disadvantages of incomplete identification of patients with left ventricular systolic and/or diastolic dysfunction.
The favourable cost–efficacy ratio of our study demonstrates that screening for left ventricular systolic and/or diastolic dysfunction with restrictive clinical criteria+determination of NT-proBNP+echocardiography is a practical option in selected populations at high risk of heart failure. This methodology overcomes the problem of the limited managerial efficiency of natriuretic peptide screening in the general population due to the low prevalence of heart failure 47,48. Managerial efficiency would be maximised if the model were used to diagnose the highest-risk forms of left ventricular dysfunction (systolic and/or restrictive diastolic), in which the discriminating capacity of NT-proBNP is definitely greatest, as demonstrated by the ROC curve (fig. Fig. 5).
6.3. Unsolved problems in the organisation of heart failure treatment for elderly patients
Elderly patients represent the majority (70%) of patients admitted to hospital with chronic heart failure; hospitalisation is lengthy, and readmission is very frequent 1,2,49,50. This is particularly true of people >80 years old, who represent 50% of all hospital admissions for chronic heart failure (DRG 127) in the Veneto regional database, with average hospital stays of 14±14 days in geriatric wards 51. This cohort of patients is consequently characterised by very high health expenditure due to the large component of hospital costs. Programmes designed to limit health expenditure on heart failure must have the main objective of reducing hospitalisation costs, which account for 70% of the total 52. A reduction in hospitalisation costs for chronic heart failure in elderly people would be possible 9, if only by making full use of drugs of proven efficacy, which are seriously underused among nursing home residents 4,5. A pilot study 53 of the same population as studied in the present research suggests that hospitalisation for chronic heart failure can be reduced with highly cost-effective approaches if an early diagnosis is made.
6.4. Usefulness of the prognostic value of NT-proBNP as a health planning tool
Organising treatment for heart failure requires the definition and validation of organisational models dedicated to specific cohorts of patients 17,54: out-patient follow-up protocols for patients discharged after admission for chronic heart failure to reduce readmission to hospital, home care for patients with refractory heart failure and telephone monitoring for patients with uncomplicated heart failure (see Refs. [7,8] for review), since only a differentiated approach can make treatment of heart failure cost-effective, its social costs being entirely out of control 42,43. Our findings confirm other authors' results 36 on the role of natriuretic peptides as a prognostic index in patients with heart failure, and extends these observations to the special case of frail elderly people. The predictive power of NT-proBNP has proved to be an essential tool for identifying frail elderly patients at risk of events so that preventive measures can be concentrated on them, and supports its use in intervention programmes. In this respect, NT-proBNP is particularly useful for its ability to identify not only patients with systolic dysfunction but also those with a restrictive diastolic pattern, as demonstrated by ROC analysis in our study. Restrictive diastolic pattern has a particularly unfavourable prognosis when present alone, and even more so when associated with systolic ventricular dysfunction 55.
6.5. Prevalence of left ventricular systolic and/or diastolic dysfunction and heart failure
In addition, we should mention that the overall prevalence of left ventricular insufficiency found in our population was very high, as reported in the literature 56. The prevalence of symptomatic heart failure is also high and consistent with the findings reported in other elderly populations (see Ref. 57 for review), as is severe diastolic dysfunction (restrictive pattern), which in our sample amounted to 3% (3.5% in a recent survey in the USA 56), perhaps due to the particularly high age of the patients, and emphasises the importance of screening in this population bracket, due to the increasing frequency of diastolic insufficiency in the hospital epidemiology of chronic heart failure 58. NT-proBNP may enable diastolic dysfunction to be identified, and the finding of values which are significantly lower than for systolic dysfunction is useful from the diagnostic standpoint, as it allows screening to be limited to systolic dysfunction, for which measures of proven efficacy are available.
7. Conclusions
Our study demonstrates that NT-proBNP is useful in investigating heart failure in frail elderly people and may constitute the missing link for drawing up intervention protocols designed to reduce the rate of hospitalisation of these subjects for chronic heart failure. Our data also confirm that the prevalence of asymptomatic left ventricular systolic and/or diastolic dysfunction among nursing home residents is very high. Finally, we can confirm that NT-proBNP values can be used for prognostic stratification even in frail elderly people.
Acknowledgements
We wish to thank Anna Maria Catto (Don Moschetta Nursing Home, Caorle), Giuseppe Di Tano (Cardiology Unit, Messina), Roberto Gnan (Don Moschetta Nursing Home, Caorle), Monica Penzo (Cardiology Unit, San Donà di Piave), Nicola Proto (Basic Health Services Department 1, San Donà di Piave), Enrico Simoli (Management Control Unit, “East Veneto” Local Health District 10) and all the nursing and technical staff of the Caorle and San Donà di Piave nursing homes. Special thanks go to Teresa Moretto and Daniela Di Vece (Don Moschetta Nursing Home, Caorle). The NT-proBNP assays were gifts from Roche Diagnostics.




