Bedside tests of B-type natriuretic peptide in the diagnosis of left ventricular diastolic dysfunction in hypertensive patients
Abstract
Aims:
To investigate the value of B-type natriuretic peptide (BNP) in diagnosing left ventricular diastolic dysfunction in patients with hypertension.
Methods:
The left ventricular diastolic function and plasma BNP levels were assessed prospectively in 135 hypertensive patients.
Results:
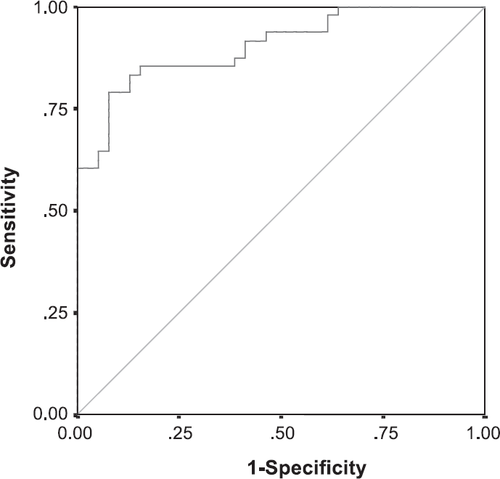
The plasma BNP in patients with (n=61) and without (n=74) diastolic dysfunction was 122±105 and 18±16 pg/ml, respectively (p<0.001). Increased BNP levels were associated with systolic blood pressure (p<0.05), left ventricular mass index (p<0.001), the E/A ratio of transmitral flow (p<0.01) and the isovolumic relaxation time (p<0.01). A receiver-operator characteristic curve showing the sensitivity and specificity of BNP against the echocardiography diagnosis of diastolic dysfunction revealed an area under the curve (accuracy) of 0.904 (p<0.01). Using a cut-off value of >40 pg/ml, the sensitivity and specificity of plasma BNP in diagnosing left ventricular diastolic dysfunction were 79% and 92%, respectively.
Conclusions:
The plasma BNP levels in patients with hypertension are closely related to left ventricular hypertrophy and filling impairment. Plasma BNP may be used to facilitate the diagnosis of left ventricular diastolic dysfunction.
1. Introduction
Diastolic left ventricular failure is now increasingly recognized as a condition leading to morbidity, hospitalisations and death. Recent studies suggest that isolated diastolic heart failure occurs in 30–60% of all patients presenting to hospitals with evidence of congestive heart failure (CHF) 1–4. Many patients with diastolic heart failure are due to left ventricular remodeling secondary to hypertension 5. The diagnosis of diastolic heart failure has been difficult because patient's clinical symptoms or signs of CHF are usually nonspecific. In addition, laboratory evidence of ventricular diastolic dysfunction, such as echocardiographically measured E/A ratio, may not be very sensitive or specific, especially when the heart failure is less advanced 6,7. Improved objective ways of detecting diastolic dysfunction, especially at the early stage of the condition, is therefore of great clinical importance.
B-type natriuretic peptide (BNP) is a neurohormone produced mainly by ventricular myocytes in response to increased end-diastolic pressure, or volume, of the ventricles 8–10. BNP produces diuresis, natriuresis and vasodilation which reduce the load on the heart 10. Patients with ventricular dysfunction tend to have high levels of plasma BNP; therefore BNP has been used as a diagnostic test for systolic dysfunction 11–16. A recent study has shown that patients with diastolic function had a higher level of plasma BNP as well 17. In addition, an increase in plasma BNP has been shown to reflect the prolongation in left ventricular relaxation time, increase in left ventricular end-diastolic pressure, and the left ventricular mass index (LVMI) in patients with hypertension 18. The primary purpose of the study was to assess the value of rapid bedside testing of BNP in the diagnosis of diastolic function impairment in hypertensive patients.
2. Patients and methods
2.1. Patient selection
The investigation was approved by the Human Ethics Committee of Lishui Central Hospital, and conforms to the principles outlined in the Declaration of Helsinki. Between September 2002 and October 2003, 135 consecutive Chinese patients (85 males, average age 70±10 years, range 35–86 years) presented to the Cardiology Department of Lishui City Central Hospital were selected for the study. All patients gave written informed consent to participate in the study.
Patients had a history of hypertension by an average of 9.3±7.8 years (1–30 years). None of these patients had chest trauma, pericardial effusion, angina or renal dysfunction prior to the study. Fifty-one patients had congestive heart failure symptoms, such as exertional dyspnoea or ankle oedema. Thirty-five had New York Heart Association (NYHA) class I, and 16 had NYHA class II. Twenty-four patients had an increased level of plasma BUN, and 17 had a previous history of ischemic stroke.
A detailed medical history and a thorough physical examination were performed in all patients, followed by a routine chest X-ray. The left ventricular function was assessed by two-dimensional and Doppler echocardiography (Acuson Sequoia 512, transducer frequency 2.5–3.5 MHz) by two experienced cardiologists. Standard two-dimensional images were obtained in the parasternal long and short axes, and in the apical four- and two-chamber views. Pulsed-wave Doppler tracings of mitral valve inflow were recorded at the leaflet tips. Left ventricular volumes and Doppler tracings were analysed using a digital echocardiography workstation. BNP was tested in all patients right after the clinical and echocardiographic examinations.
The thickness of the ventricular walls and the interventricular septum, and the diameter of the left ventricle were measured by M-mode echocardiography. The left ventricular mass (LVM) and mass index (LVMI) was also calculated. Left ventricular mass index (LVMI) was calculated using the equation described by Devereux et al. 19: {1.04 [(IVST+LVIDd+LVPWT)−LVIDd]−13.6}; where IVST is the interventricular septal thickness, LVIDd is the left ventricular internal diastolic diameter, and LVPWT is the left ventricular posterior wall thickness. Left ventricular hypertrophy was defined as LVMI >116g/m2 (male) or >104 g/m2 (female).
The diastolic function was assessed by Doppler echocardiography of transmitral flow, where the E and A peaks, the diastolic time and the isovolumic relaxation time were measured.
The definition of diastolic heart failure was based on three criteria: (1) The presence of signs or symptoms of congestive heart failure; (2) the echocardiographically measured left ventricular ejection fraction was more than 50%; and (3) echocardiographic evidence of abnormalities of left ventricular relaxation: E/A ratio <1.0 (<55 years old) or <0.8 (>55 years old); E peak deceleration time of more than 240 ms or isovolumic relaxation time of less than 90 ms 7.
2.2. Measurement of plasma BNP
BNP levels were measured by the previously reported methods 8. Venous blood samples were kept in EDTA tubes at room temperature and analysed within 4 h of the collection. The whole blood was then analysed in triplicate with the Triage BNP assay, a sandwich immunoassay that consists of a disposable device to which 250 μl of EDTA-anticoagulated whole blood was added. The Triage meter was used to measure the BNP concentrations by detecting a fluorescent signal that reflects the amount of BNP in the sample.
Once 250 μl of whole blood was added to the device, the cells were separated from the plasma by a filter, and the plasma containing BNP was put in a reaction chamber containing fluorescent-tagged BNP antibodies to form a reaction mixture. The reaction mixture was incubated for about 2 min and then migrated through the diagnostic lane by capillary action to a zone of immobilized antibody that would bind the desired BNP–fluorescent antibody complex. After about 15 min, the device was placed into the Triage meter and the fluorescence intensity of the BNP assay zone was measured. An internal calibration curve was used to correlate the Triage meter and the fluorescence measurement to the BNP concentration. The assay was completed in approximately 15 min.
2.3. Statistical analysis
Data were expressed as means±S.D. ANOVA test was used to analyse the difference in clinical parameters between groups. Chi-square test was used to assess the differences in percentage data. The correlations between BNP and the left ventricular anatomy or function were also assessed. The accuracy of plasma BNP in diagnosing diastolic dysfunction was assessed by a receiver-operator characteristic curve. p<0.05 was considered to be statistically significant.
3. Results
3.1. General findings
Eighty-four patients were treated with anti-hypertensive agents at the time of the study. Only 47 of the 135 patients had a blood pressure <140/90 mm Hg. BP was above 160/95 mm Hg in 44 patients. The average systolic and diastolic pressure in the 135 patients was 147.1±27.0 (100–198) mm Hg and 85.3±16.3 (68–116) mm Hg, respectively. All patients had a left ventricular ejection fraction of more than 50%.
3.2. Relationship between BNP and left ventricular mass
As shown in Table 1, univariate analysis showed a moderate correlation between BNP, the thickness of left ventricular posterior wall, the interventricular septum and the LVMI. A significant increase in the level BNP was found in patients with a LVMI of more than 140 g/m2 (Fig. Fig. 1).
| Pearson correlation coefficient | p | |
|---|---|---|
| Interventricular septum thickness | 0.468 | 0.001 |
| LV posterior wall thickness | 0.374 | 0.001 |
| LV mass index | 0.365 | 0.001 |
| Systolic blood pressure | 0.224 | 0.01 |
| LV ejection fraction | −0.261 | 0.006 |
| E/A ratio | 0.47 | 0.009 |
| Isovolumic relaxation time | 0.389 | <0.001 |
- a LV: left ventricle.
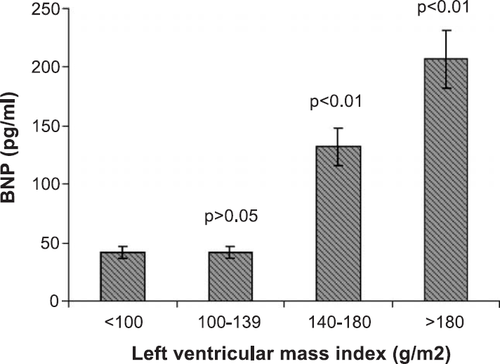
A positive correlation was also found between the levels of BNP and the systolic blood pressure (Table 1). There was an inverse correlation between the left ventricular ejection fraction and the BNP levels (Table 1).
Multivariate regression analysis showed that LVMI, the E/A ratio and the isovolumic relaxation time were independent predictors of elevated plasma BNP (p<0.01).
3.3. BNP and diastolic dysfunction
Based on the clinical symptoms and echocardiography examinations, left ventricular diastolic function impairment was identified in 61 patients (Table 2). The main echocardiographic abnormalities in these patients were reduced E/A ratio, whereas the average deceleration time of the E peak was similar between the two groups. The average isovolumic relaxation time in the diastolic dysfunction group was shorter than that of the normal diastolic function group (Table 2).
| Parameters | Diastolic dysfunction (n=61) | Normal diastolic function (n=74) | p |
|---|---|---|---|
| Age | 70±10 | 66±13 | >0.05 |
| Male | 37 (68%) | 48 (65%) | >0.05 |
| Duration of hypertension, months | 107±100 | 114±105 | >0.05 |
| LV hypertrophy | 42 (69%) | 15 (20%) | <0.01 |
| LV diameter, mm | 45±10 | 44±9 | >0.05 |
| LV septum, mm | 11.5±1.7 | 10.3±1.8 | 0.001 |
| LV posterior wall, mm | 9.9±1.5 | 9.4±1.4 | 0.004 |
| LV mass index, g/m2 | 132±38 | 103±34 | <0.001 |
| LV ejection fraction, % | 65±8 | 67±9 | >0.05 |
| Deceleration time, ms | 182±68 | 181±48 | >0.05 |
| Isovolumic relaxation time, ms | 107±68 | 160±152 | 0.006 |
| E/A ratio | 0.68±0.21 | 1.61±0.72 | <0.001 |
| BNP, pg/ml | 122±105 | 18±16 | <0.001 |
- a LV: left ventricle.
More patients in the diastolic dysfunction group had left ventricular hypertrophy (Table 2). In the 74 patients with normal diastolic function, the BNP in those with left ventricular hypertrophy (n=15) and those without ventricular hypertrophy (n=59) was 24±9 and 18±11 pg/ml, respectively (p>0.05).
There was a significant correlation between the plasma BNP levels and E/A ratio or isovolumic relaxation time in the 135 patients (Table 1). The average BNP level in patients with diastolic dysfunction was higher than that in those with normal ventricular diastolic function (Table 2). A receiver-operator characteristic curve was used to show the sensitivity and specificity of BNP against the echocardiography diagnosis of diastolic dysfunction. The area under the receiver-operator curve was 0.904 (0.843–0.966, p<0.01) (Fig. Fig. 22). Using a cut-off value of 40 pg/ml, the sensitivity and specificity of plasma BNP in diagnosing diastolic dysfunction were 79% and 92%, respectively.
4. Discussion
4.1. BNP levels in patients with hypertension
Previous studies have found that BNP was increased in patients with hypertension 20,21. The level of BNP was associated with left ventricular mass index in these patients 20–22. Our study also showed a significant correlation between the plasma level of BNP and left ventricular mass index in the hypertensive patients. However, left ventricular wall thickness does not appear to be the only determinant factor for BNP, because BNP was not elevated in normotensive athletes who had a similar increase in left ventricular mass index to hypertensive patients 23. In the present study, a normal level of plasma BNP was identified in 15 patients who had an increased left ventricular mass index but normal diastolic function on echocardiography.
It seems that left ventricular diastolic filling impairment, partly due to left ventricular hypertrophy, is mainly responsible for the increased plasma levels of BNP in hypertensive patients. An earlier multivariate analysis demonstrated that E/A ratio is related to plasma BNP in hypertensive patients, independent of age and blood pressure or left ventricular mass index 24. In our patients, a significant correlation was identified between the plasma level of BNP and the E/A ratio or isovolumic relaxation time. Multivariate regression analysis also showed that E/A ratio and the isovolumic relaxation time are independent predictors of plasma BNP.
4.2. Role of plasma BNP in diagnosing diastolic dysfunction
Although BNP has been consistently shown in a number of studies to have a high sensitivity and specificity in diagnosing systolic heart failure 11–16, its role in the diagnosis of diastolic dysfunction is less certain. Recent studies have demonstrated that BNP levels in patients with diastolic dysfunction are higher than that in normal controls 17,21, but it was less than that in patients with systolic dysfunction 17. The sensitivity and specificity of elevated BNP in detecting prolonged isovolumic relaxation time and increased left end-diastolic pressure were 0.63–0.85 and 0.70–0.76, respectively 18.
Our study assessed the value of BNP in the diagnosis of left ventricular diastolic dysfunction in hypertensive patients. The results showed that BNP, when rapidly tested at bedside, has a moderate sensitivity but an excellent specificity in detecting ventricular diastolic dysfunction in these hypertensive patients. The clinical implications of these findings are that, although BNP may not be ideal as a screening test for diastolic dysfunction, it is a very useful tool to confirm the diagnosis prompted by other diagnostic means, such as echocardiography.
A recent study by Motrram et al. 25 on a small patient population has indicated that, although the plasma level of BNP in patients with hypertension-caused diastolic dysfunction was higher than those with normal diastolic function, more than 70% patients with diastolic dysfunction had BNP levels within the normal range. The major difference between this study and ours or other previous reports 26 where BNP was also found to have a high sensitivity and specificity in diagnosing filling impairment was that the average BNP level (46+48 pg/ml) in their patients with diastolic dysfunction was much lower than that of our patients and the others 26. This is very likely due to the different degree of diastolic dysfunction between the patients.
It is worth noting that only 84 out of the 135 patients who had at least 1-year history of hypertension were on antihypertensive therapy at the time of the study. This may reflect the inadequacy of hypertension management and/or patient's compliance to medical therapy in the community where the study was conduced. Further investigations on the potential causes hindering hypertension management in the region are warranted. In addition, we used a combination of echocardiographic parameters to assess diastolic dysfunction. It is generally considered that isovolumic relaxation time is more reliable than E/A ratio as an indicator of diastolic dysfunction. Therefore, further studies are required to assess the impact of different echocardiographic parameters on the diagnostic values of BNP in hypertensive patients.
In conclusion, this prospective study has shown that plasma BNP was increased in patients with left ventricular hypertrophy and filling impairment secondary to hypertension. Elevated BNP levels can be used to facilitate the diagnosis of left ventricular diastolic dysfunction in these patients.




