NT-proBNP and BNP: biomarkers for heart failure management
Abstract
Guidelines for the pharmacological treatment of heart failure (HF) are based on results from large clinical trials demonstrating benefit. State of the art pharmacological management of HF assumes that target doses should be the same as those used in trials. Thus equal doses are recommended for all in practical guidelines, but this strategy might not fit individual needs. NT-proBNP and BNP emerged as potential biomarkers of clinical interest in HF management. NT-proBNP and BNP are related to HF severity and to clinical status. NT-proBNP and BNP are strongly associated with prognosis across the whole spectrum of HF patients. A pilot study has shown that NT-proBNP-guided therapy is associated with improved outcome in HF. Although at present there are still few data to make firm recommendations on the use of NT-proBNP or BNP levels as biomarkers for HF management, future studies will provide further insight on this issue.
1. Introduction
Results from clinical trials on heart failure (HF) have led to major improvements in patient care. The pharmacological treatment of HF is based on the results of these trials and consists mainly of ACE-inhibitors, beta-blockers and aldosterone antagonists plus diuretics 1–5. State of the art pharmacological management of HF assumes that target doses of these drugs should be the same as in the trials that dictate their use 6–8. However, this strategy, based on equal doses for all, as recommended in guidelines, might not fit individual needs. Should patients with different co-morbidities and different body mass indexes receive the same treatment= Should patients who are doing well on standard therapy have their treatment intensified based on poor prognostic indexes= These questions suggest that individualization of HF therapy might be necessary 9.
Measurement of brain natriuretic peptide (BNP) and the amino terminal portion of the pro-hormone (NT-proBNP) is already available for clinical use in many European countries and in the United States. European health authorities have approved BNP and NT-proBNP testing to assist clinicians in the diagnosis of HF 10–15. The prognostic value of BNP and NT-proBNP in HF patients is also established 16–20. Individualization of HF therapy based on NT-proBNP has also been suggested 21.
As in other diseases, in order to be clinically useful, a biomarker has to be sensitive and specific for the disease process, and its measurement has to be standardized and easy to perform. Additionally, the test should demonstrate biological validity, for instance, BNP levels must be related to the clinical status and/or prognosis of patients with HF; and/or variations in BNP levels should be related to changes in clinical status and in prognosis. If all of the above are fulfilled then optimization of BNP levels through changes in therapy should translate into improved clinical outcome.
2. NT-proBNP, BNP and clinical status in HF patients
There is a large body of evidence that NT-proBNP and BNP levels correlate well with the severity of HF 16,22–24. The more severe the HF the higher the BNP and NT-proBNP levels. Even among patients with mild HF, NT-proBNP levels, but not BNP levels, are significantly higher in class II compared to class I patients. The suggested pathophysiological explanation for this observation is related to the different clearance mechanism for BNP and NT-proBNP 25.
Clinical status in HF has been traditionally assessed by functional impairment. The most widely used instrument to accomplish this goal is the New York Heart Association (NYHA) classification. NYHA classification gives crude but clinically relevant information. Other ways to evaluate clinical status include quality of life scales and exercise performance. The 6-min walk test, although not routinely used, provides independent prognostic information 26. Patients with better exercise performance (evaluated by the 6-min walk test or by peak Vo2 consumption test) have lower levels of BNP 27. In a sample of HF patients in which the whole spectrum of NYHA classes was represented, an inverse correlation between BNP and the distance walked in 6 min has been reported. In this study, within the same NYHA class, patients who walked the shortest distance in 6 min had the highest BNP levels. These results suggest that BNP levels add information to the NYHA classification in the evaluation of clinical status in heart failure.
3. NT-proBNP, BNP and prognosis in HF
The identification of HF patients at high risk of cardiovascular events is critical to select those who will benefit from more aggressive intervention and referral to specialized services.
NT-proBNP and BNP concentrations are higher in patients with HF who have the most severe symptoms and ventricular dysfunction and the worst prognosis 28,29. Although BNP correlates with peak Vo2 and symptoms and the severity of LV dysfunction, its prognostic value is independent and superior to NYHA class, age, ejection fraction, Vo2 and prior myocardial infarction 20,30.
Recent studies have included patients on beta-blockers and spironolactone, as well as angiotensin II receptor blockers 31–33. NT-proBNP and BNP were consistently shown to have independent prognostic value.
In a recent study evaluating ‘traditional’ indexes as well as NT-proBNP in patients with severe HF, only NT-proBNP predicted death or urgent heart transplantation, supporting its potential role in selecting patients for heart transplantation.
4. Correlation of NT-proBNP and BNP levels with changes in clinical status
For NT-proBNP and BNP to be useful in clinical practice they should mirror modifications in clinical status. In a small sample of outpatients, only changes in BNP levels were associated with changes in NYHA class 22. Patients with improving NYHA class had decreasing levels of BNP, while patients with clinical deterioration had increasing BNP levels. The results of this small study suggest that the direction of BNP change parallels changes in clinical status. In hospitalized patients admitted with HF decompensation clinical improvement is associated with a significant decrease in BNP levels 34,35. Data on NT-proBNP are similar. In a recent study, we observed and followed for 6 months, 176 patients hospitalized due to decompensated HF. NT-proBNP was measured at admission and at the day of discharge. Twenty patients died in the hospital. Plasma levels of NT-proBNP (mean±S.D.) measured at admission in these patients were higher than in patients discharged alive (28 345.4±21 653.7 pg/ml vs. 14 463.8±24 859.5 pg/ml, P<0.001). NT-proBNP levels in patients who improved by at least two NYHA classes during hospitalization (n=85) decreased significantly more (30.1±49.1% vs. 3.2±75.7%, P=0.01) than in the other patients (n=71).
5. Association between changes in NT-proBNP and BNP and prognosis
Probably even more important is the association between changes in NT-proBNP and BNP and modification of prognosis. In other words, optimizing levels of natriuretic peptides through changes in therapy might translate into improved clinical outcomes.
ACE inhibitors improve outcome in heart failure 1,2. ACE-inhibitors can reduce BNP levels in patients with HF and even attain normal levels in patients with mild to moderate HF 36–38.
The effect of beta-blockers on BNP levels is less well known. We observed a decrease in patients with mild to moderate HF 8–12 months after the initiation of beta-blockers 39. Others have reported similar findings 18. Recent data showed that 3 months after initiation of beta-blockers in HF, there was no change or mild elevations in NT-proBNP levels, but at 6 and 12 months there was a significant decrease in NT-proBNP levels 40.
Results from the ValHeFT study showed that patients in the valsartan arm had a significant decrease in BNP levels while patients in the placebo arm had an increase in BNP 33. In the Rales Trial, patients in the treatment arm had significant decreases in BNP levels throughout the study period, while patients in the placebo arm had no significant changes in BNP levels. All these data demonstrate that drugs that modify prognosis in HF lead to a decrease in NT-proBNP and BNP levels.
The association between changes in NT-proBNP and BNP levels and prognosis may also be of interest. In patients with mild to moderate heart failure, we found that those with increasing BNP levels during an 8–12-month period had a significantly worse prognosis than those with decreasing levels 39. Furthermore, we found that patients with baseline BNP level above median and increasing BNP levels had the worst prognosis, while those with low and decreasing BNP levels had the best prognosis. In other words, serial evaluations of BNP can help identify high and low risk patients (Fig. 1).
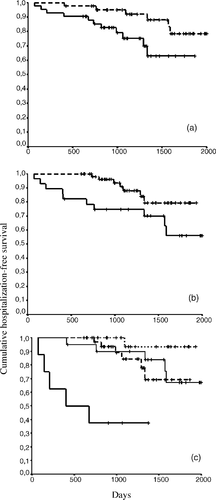
Results from the ValHeFT study confirm this hypothesis. In ValHeFT, BNP was measured at baseline and after 4 months 33. Patients with decreasing BNP levels had a significantly better prognosis than those with increasing BNP during this period.
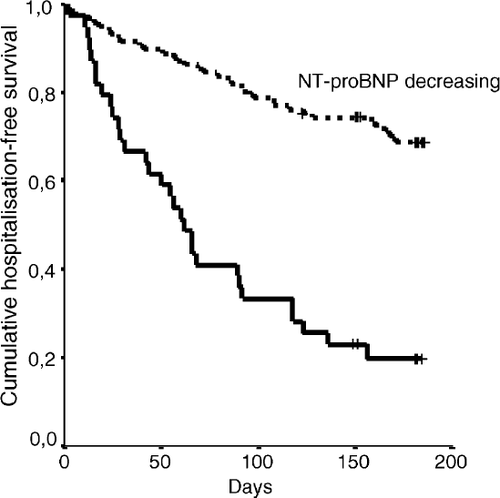
Results from hospitalized patients point in the same direction. We observed that BNP levels at hospital discharge are associated with outcome 34. Patients with increasing BNP levels during hospitalization had a worse prognosis than those with decreasing levels. BNP decreased more among patients without adverse events than in those with an adverse event during follow-up. The direction and the magnitude of BNP change during hospitalization of HF patients might help clinicians in planning hospital discharge. We found similar results with NT-proBNP in a group of 156 patients hospitalized due to HF decompensation. Patients with increasing NT-proBNP levels during hospitalization had significantly more re-hospitalizations or death than patients with decreasing NT-proBNP levels (Fig. 2). Multivariate Cox regression analysis showed that the percent decrease in the levels of NT-proBNP during hospitalization was the most powerful predictor of outcome (Table 1).
| Adjusted HR | 95% CI | P | |
|---|---|---|---|
| Male gender | 0.981 | 0.953–1.009 | 0.175 |
| Age (years) | 0.607 | 0.307–1.199 | 0.150 |
| Ischaemic etiology | 1.745 | 0.855–3.560 | 0.126 |
| Diabetes mellitus | 0.723 | 0.39–1.340 | 0.302 |
| Atrial fibrillation | 1.043 | 0.547–1.990 | 0.897 |
| Left ventricle systolic function | 0.037 | ||
| (vs. preserved) | |||
| Mildly-moderately depressed | 1.581 | 0.610–4.096 | 0.346 |
| Severely depressed | 1.185 | 0.404–3.477 | 0.757 |
| Not assessed | 3.727 | 1.273–10.911 | 0.016 |
| Systolic blood pressure (mmHg) | 1.007 | 0.987–1.026 | 0.511 |
| Diastolic blood pressure (mmHg) | 0.998 | 0.973–1.023 | 0.847 |
| Heart rate (beats/min) | 1.038 | 1.004–1.072 | 0.027 |
| Serum creatinine (mg/dl) | 0.481 | 0.276–0.839 | 0.010 |
| Serum urea (mg/dl) | 0.997 | 0.988–1.006 | 0.477 |
| Serum sodium (mEq/l) | 0.978 | 0.903–1.060 | 0.595 |
| Length of stay (days) | 1.015 | 0.981–1.052 | 0.389 |
| Diuretic at discharge | 0.427 | 0.029–6.386 | 0.538 |
| ACE-inhibitor at discharge | 0.740 | 0.310–1.767 | 0.498 |
| Beta-blocker at discharge | 2.374 | 1.178–4.784 | 0.016 |
| Spironolactone at discharge | 1.308 | 0.652–2.623 | 0.450 |
| NYHA class III/IV at discharge | 0.873 | 0.412–1.851 | 0.723 |
| Hypervolemia at discharge | 3.402 | 1.632–7.092 | 0.001 |
| Admission NT-proBNP (1000 pg/ml) | 1.010 | 0.993–1.028 | 0.258 |
| Discharge NT-proBNP (1000 pg/ml) | 1.017 | 0.997–1.036 | 0.090 |
| Percent decrease in NT-proBNP (%) | 0.998 | 0.984–0.993 | <0.001 |
6. NT-proBNP-guided therapy
These results suggest that monitoring HF therapy through NT-proBNP or BNP levels could be of value. A pilot study has evaluated NT-proBNP-guided therapy 40. Patients were randomly allocated to receive either symptom-guided treatment or treatment based on NT-proBNP levels. The group assigned to NT-proBNP based therapy received higher doses of ACE-inhibitors and diuretics. After 10 months, fewer events occurred in the group of patients treated according to NT-proBNP levels. A larger study is now ongoing in patients taking beta-blockers and spironolactone as well as diuretics and ACE-inhibitors. This study will hopefully provide evidence on whether NT-proBNP can be used as a surrogate end-point in the monitoring of HF treatment.




