Application of NT-proBNP and BNP measurements in cardiac care: a more discerning marker for the detection and evaluation of heart failure
Abstract
Background:
Measurement of brain natriuretic peptide (BNP) has become a potent diagnostic aid as a means of identifying patients with systolic or diastolic dysfunction. Due to better stability in circulating blood, we reasoned that measurement of N-terminal proBNP (NT-proBNP) may be a more discerning marker for the detection and evaluation of chronic heart failure.
Methods:
The relationships between plasma concentrations of NT-proBNP and BNP, and aetiology, New York Heart Association (NYHA) classification, and left ventricular ejection fraction (LVEF) were analyzed in 105 patients with chronic heart failure. Sixty-seven healthy volunteers were studied as the controls.
Results:
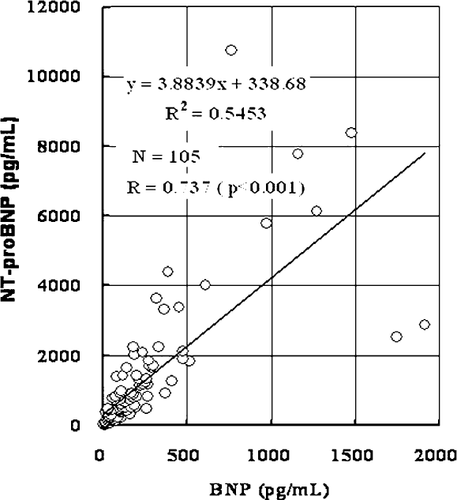
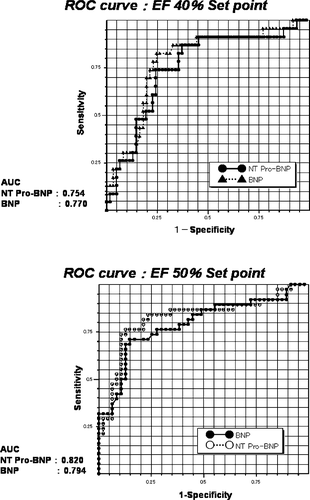
Both NT-proBNP and BNP showed progressive increases (P<0.001) in proportion to the NYHA classification; the increment of NT-proBNP was larger than that of BNP. Elevated NT-proBNP significantly correlated with BNP (r=0.737, P<0.001). Receiver operating characteristics analysis to detect LVEF<40% showed similar values (area under the curve, AUC: NT-proBNP 0.754 vs. BNP 0.770), however, AUC to detect LVEF<50% tended to be greater for NT-proBNP than that for BNP (NT-proBNP 0.820 vs. BNP 0.794).
Conclusion:
NT-proBNP may be a more discerning marker for the detection and evaluation of heart failure than BNP.
1. Introduction
Chronic heart failure is an increasingly common disease characterized by poor prognosis and quality of life. Recent ACC/AHA guidelines for the management of heart failure have emphasized the need for earlier identification and therapy for patients at high-risk of developing heart failure or asymptomatic left ventricular systolic dysfunction as well as those with symptomatic heart failure 1. The most commonly applied investigation to confirm the diagnosis of heart failure is echocardiography, which offers structural and functional information about the heart. However, detailed assessment of cardiac function by echocardiography is limited in many health care systems, especially in primary care.
Recently, measurement of circulating levels of brain natriuretic peptide (BNP), a biologically active peptide of 32 amino acids with vasodilating and natriuretic properties, has become a potential diagnostic aid to identify patients with elevated ventricular filling pressure who are likely to exhibit signs and symptoms of heart failure 2–4. Upon stress-induced secretion of BNP, proBNP (1-108) in cardiomyocytes is cleaved into the active hormone BNP (77-108) and inactive N-terminal proBNP (1-76, NT-proBNP). The ESC guidelines for the diagnosis and treatment of chronic heart failure have proposed that measurement of these natriuretic peptides can be most useful clinically as a rule-out test due to their consistent and very high negative predictive value 3,5,6. Because of better stability, both in circulating blood and after sampling, we reasoned that measurement of NT-proBNP may be a better marker for the detection and evaluation of chronic heart failure than BNP.
2. Patients and methods
We studied 67 healthy controls (six women and 61 men, mean age: 35.1±12.5 years) and 105 consecutive patients with CHF (21 women and 84 men, mean age: 64.4±18.7 years, mean LVEF: 41.9±12.5%) who visited the outpatient department at Nippon Medical School Hospital, Tokyo, between June and October 2001. The severity of chronic heart failure was modified New York Heart Association (NYHA) class I in 19 patients, class IIs in 50 patients, class IIm in 25 patients, class III in nine patients and NYHA IV in three patients. Class IIs or IIm in modified NYHA classification is defined as slight or moderate limitation of physical activity, respectively. The aetiology of chronic heart failure was dilated cardiomyopathy in 19 patients, hypertrophic cardiomyopathy in seven patients, previous myocardial infarction in 35 patients, hypertensive heart disease in 30 patients, valvular heart disease in seven patients, congenital heart disease in two patients, and others (adriamycin cardiomyopathy in two patients, and cardiac sarcoidosis in three patients). We strictly excluded subjects with blood pressure exceeding 140/90 mmHg, total cholesterol level exceeding 220 mg/ml, serum creatinine exceeding 1.2 mg/dl, any smoker, body mass index exceeding 25, or any abnormal laboratory findings from the healthy controls. Thus 67 out of 88 healthy volunteers firstly enrolled were finally selected as the healthy controls.
After informed consent for biochemical examinations had been obtained, blood samples were collected from the controls and the patients with chronic heart failure. The present investigation protocol was in agreement with the guideline of the institutional ethics committee. Samples were quickly centrifuged, and the plasma stored below −20 °C. Measurements of BNP were performed within 24 h of sample collection. Measurement of NT-proBNP was performed within 2 months of sample collection. NT-proBNP was measured by the electrochemiluminescence assay (Elecsys 2010, Roche Diagnostics, Germany), and BNP was measured by radioimmunoassay (Shionoria BNP kit, Tokyo, Japan).
The correlations of these markers with the underlying disease, modified NYHA classification, and left ventricular ejection fraction (LVEF) assessed by echocardiography were analyzed to compare the diagnostic efficacy of the markers. All values are expressed as the mean±S.D. Comparison of NT-proBNP and BNP levels between NYHA classifications were analyzed by ANOVA with Fisher's post hoc test. Linear regression analysis between NT-proBNP and BNP levels of simultaneously obtained samples was performed. The analysis receiver operating characteristics curves were developed to assess the area under the curve to detect LVEF less than 40, 45 or 50% for both NT-proBNP and BNP. Statistical significance was established at the P<0.05 level.
3. Results
3.1. NT-proBNP levels in the normals
The upper limit for the normals (mean+2 S.D.: 23.7+30.8) was assessed as 54.5 pg/ml (6.43 pmol/l) in this study. We did not find a significant correlation with age in the normals, which may be because we strictly excluded subjects with blood pressure exceeding 140/90 mmHg, total cholesterol exceeding 220 mg/ml, serum creatinine exceeding 1.2 mg/dl, any smoker, body mass index exceeding 25, or any abnormal laboratory findings from the normals. It may also have been due to the limited number of samples in the present investigation.
3.2. NT-proBNP and BNP levels in patients with chronic heart failure
When comparing NT-proBNP and BNP levels between the underlying diseases, we noticed much wider range of elevation in NT-proBNP in patients with previous myocardial infarction compared with other etiologies. Elevations in hypertensive heart disease, dilated cardiomyopathy, hypertrophic cardiomyopathy and valvular disease were similar. The increase of NT-proBNP levels was larger compared with BNP in all the underlying diseases (Table 1).
| DCM | HCM | Previous MI | HHD | VHD | |
|---|---|---|---|---|---|
| Patients | 19 | 7 | 35 | 30 | 7 |
| LVEF% | 39.4 (12.4) | 59.3 (19.1) | 40.2 (12.9) | 56.8 (12.6) | 57.1 (10.7) |
| NT-proBNP pg/ml | 533.7 (410.2) | 599.0 (620.4) | 1372.0 (1406.5) | 551.2 (475.2) | 837.2 (396.4) |
| BNP pg/ml | 99.2 (52.7) | 179.5 (158.0) | 258.5 (243.9) | 101.6 (48.3) | 168.0 (97.7) |
| Mean (S.D.), NT-ProBNP in controls; 23.7 (15.4) | |||||
- a Abbreviations: DCM dilated cardiomyopathy, HCM hypertrophic cardiomyopathy, MI myocardial infarction, HHD hypertensive heart disease, VHD valvular heart disease.
- b For the remaining seven patients, aetiology was congenital heart disease in two, adriamycin cardiomyopathy in two, and cardiac sarcoidosis in three patients.
3.3. NT-proBNP and BNP: relationship to modified NYHA classification
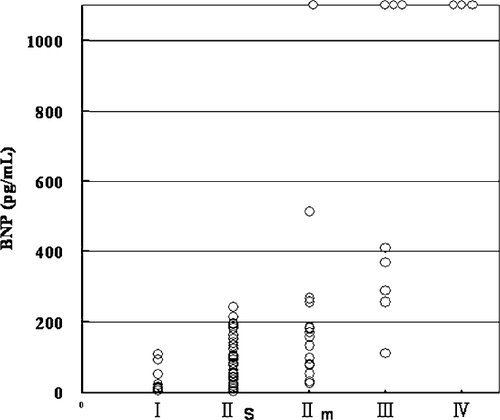
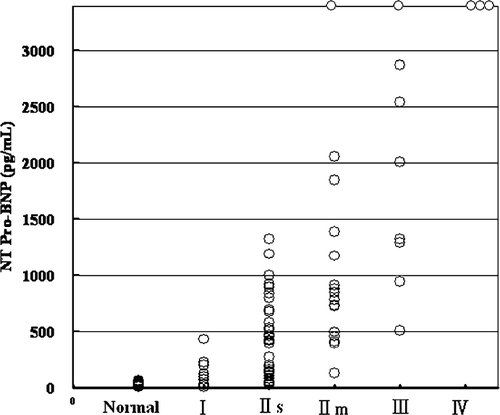
Plasma concentrations of BNP, NT-proBNP, and LVEF in patients grouped by NYHA classification are shown in Table 2. A progressive increase in BNP (P<0.001) and NT-proBNP (P<0.001) in proportion to NYHA classification was confirmed in this study. The BNP level in NYHA IIs was five times higher compared with that in NYHA I, 15 times higher in NYHA IIm, and 50 times higher in NYHA III (Fig. 1). The increment of NT-proBNP was much steeper compared with the BNP elevations. The increment of NT-proBNP in NYHA IIs was five times higher compared with that in NYHA I, 25 times higher in NYHA IIm, and 100 times higher in NYHA III (Fig. 2).
| NYHA-I | NYHA-IIs | NYHA-IIm | NYHA-III | |
|---|---|---|---|---|
| Patients | 19 | 50 | 25 | 9 |
| LVEF % | 57.5 (11.1) | 53.2 (13.2) | 44.3 (13.3) | 33.0 (6.3) |
| NT-ProBNP pg/ml | 103.4 (97.6) | 622.2 (472.7) | 2241.0 (1528.4) | 10 018.0 (12727.0) |
| BNP pg/ml | 24.9 (28.2) | 105.9 (67.3) | 388.3 (260.5) | 1438.2 (533.5) |
| Mean (S.D.), NT-ProBNP in the healthy normals; 23.7 (15.4) | ||||
There was a significant correlation between simultaneously obtained BNP and NT-proBNP levels (Fig. 3, r=0.737, P<0.001). Overall, the levels of NT-proBNP were four-fold or more higher compared with simultaneously obtained BNP levels.
3.4. Receiver operating characteristics analysis to detect LV dysfunction
When the predictive value for LVEF<40% was analyzed in the receiver operating characteristics curve, the area under the curves were almost identical. (NT-proBNP 0.754 vs. BNP 0.770, Fig. 4a.) However, that for LVEF<50% tended to be higher for NT-proBNP compared with that for BNP (NT-proBNP 0.820 vs. BNP 0.794, Fig. 4b), and the cut-off level was determined as 695 pg/ml for NT-proBNP and 135 pg/ml for BNP, giving a sensitivity of 85.4% and specificity of 73.2% for NT-proBNP, and sensitivity of 72.3% and specificity of 73.2% for BNP.
4. Discussion
4.1. Novel cardiac markers in chronic heart failure
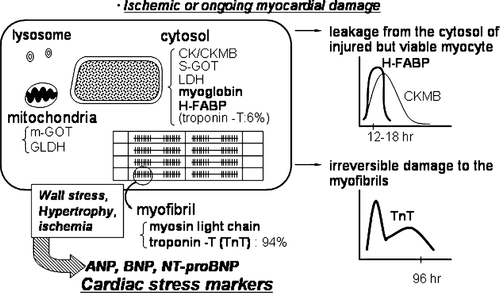
Progressive deterioration of ventricular function is frequently observed in patients with severe chronic heart failure. During the time-course of heart failure, LV function occasionally deteriorates following triggers such as infections, disturbance of renal function, anaemia, or inappropriate cessation of therapies, resulting in acute decompensation. A decompensation may lead to activation of neurohormonal systems such as the sympathetic nervous system, the renin–angiotensin–aldosterone system and natriuretic peptides. Progressive intrinsic contractile dysfunction is strongly associated with down-regulation of beta-receptor signaling, abnormal Ca handling at the sarcoplasmic reticulum and oxidative stress. Structural changes are observed in the myocardium; ventricular remodelling, myocytes slippage, interstitial fibrosis, and ongoing myocardial damage which can be detected by novel myofibril (troponin T) and cytosolic (heart-type fatty acid-binding protein) markers 7,8.
Fig. 5 shows the distribution of novel cardiac markers and differences in their release kinetics 7–10. Cytosolic markers such as creatine kinase (CK), CKMB, myoglobin (MB) or heart-type fatty acid-binding protein (H-FABP) are readily released into the circulating blood following ischaemic myocardial damage 9. However, myofibril markers such as troponin T or I show prolonged release kinetics following ischaemic or ongoing myocardial damage 7,8,10. We recently reported that measurements of cytosolic (H-FABP) and myofibril (Troponin T) markers detected ongoing myocardial damage, which independently predicted subsequent cardiac events in patients with chronic heart failure. Elevation of H-FABP reflects the severity of CHF more closely than Troponin T, and H-FABP as well as Troponin T is a sensitive marker for the detection and evaluation of ongoing myocardial damage in patients with chronic heart failure 7,8. A third group is cardiac stress markers, such as atrial natriuretic peptide (ANP), BNP or NT-proBNP. Elevation of plasma ANP indicates atrial overload, and elevation of BNP and/or NT-proBNP indicates left ventricular systolic dysfunction or diastolic dysfunction associated with elevated wall stress, or myocardial hypertrophy per se 11–15.
4.2. NT-proBNP and BNP in chronic heart failure
When comparing NT-proBNP and BNP levels between the underlying diseases in the present study, we noticed higher mean values and greater variability of NT-proBNP elevation in patients with previous-MI compared to other diagnostic groups. This may be related to the pathophysiological background of coronary artery disease, namely, different locations and sizes of infarct, inhomogeneous wall stress because of localized asynergy, ventricular remodeling following myocardial infarction, and residual or recurrent ischaemic insults. Recent reports have elucidated the prognostic value of NT-proBNP in patients with acute coronary syndrome 16,17. We have sought diagnostic value of NT-proBNP in patients with suspected acute coronary syndrome in the cardiac emergencies. NT-proBNP levels on admission did not correlate with CKMB, Troponin T, H-FABP and other cardiac markers for myocardial infarction, however, the receiver operating characteristics analyses of NT-proBNP revealed unique diagnostic value (high specificity) of NT-proBNP especially for patients with non-ST-elevation acute coronary syndrome which was documented in the early acute phase (within 2 h after the onset of chest pain, data not shown).
The increment of NT-proBNP was much steeper than that for BNP in relation to the severity of heart failure. While plasma levels of NT-proBNP and BNP in normal subjects were approximately equal (in mol unit), the NT-proBNP levels were two to five times higher than BNP levels in patients with heart failure. Clear separation between normal and abnormal values suggests that NT-proBNP may be more clinically useful. However, when the predictive value for LVEF <40% was analyzed in the receiver operating characteristics analysis, the area under the curves of BNP and NT-proBNP were almost identical. The area under the curve for LVEF<50% tended to be higher for NT-proBNP than BNP (0.820 vs. 0.794), and the cut-off level for the diagnosis of LVEF<50% was determined as 695 pg/ml for NT-proBNP and 135 pg/ml for BNP. These findings also suggest that NT-proBNP may be more discerning marker for the detection and evaluation of heart failure.
4.3. Clinical implication and limitation of the present study
This single center comparative study revealed that the plasma concentration and absolute increment of NT-proBNP exceed that of BNP, and reflect the severity of heart failure and decrease in LVEF more accurately. However, in this study, differences between the diagnostic performance of these two peptide measurements were not statistically significant, although they may well be clinically meaningful. A much larger population would have been required to confirm or refute this. While the aetiology of heart failure (coronary disease or non-coronary cardiomyopathy, or ischaemic or non-ischaemic condition), age, gender, and renal function (data not shown) had some influence on NT-proBNP elevation, a large scale prospective investigation should be established to clarify the characteristics of NT-proBNP evaluation and the novel utility in cardiac care.




