Liver transplantation for hepatocellular carcinoma: the Japanese experience
Abstract
Despite the wide spectrum of selection criteria used by living donor liver transplantation (LDLT) centers in Japan, LDLT for hepatocellular carcinoma (HCC) can achieve an acceptable outcome comparable to the outcome for deceased donor liver transplantation (DDLT) for HCC. One of the most crucial considerations in liver transplantation for HCC is the advent of expanded criteria that allow more patients with HCC to receive the organs and offer similar or even better results compared to the Milan of UCSF criteria. Expanded criteria for HCC are proposed from three single-center and one multicenter study in Japan. These criteria are based on the independent predictors for outcome derived from the analyses of the pretransplant factors and explant pathology. The beneficial effect of those proposed criteria can be predicted by the inclusion rates of the patients compared to the Milan or UCSF criteria in the same cohort and the outcome for those included patients. While application of the UCSF criteria increases the inclusion rate compared to the Milan criteria by 5–10%, these proposed criteria increase the inclusion rates by 5–54% compared to the Milan criteria. The higher inclusion rates compared to the application of the Milan criteria are achieved by criteria including tumor markers, either AFP or PIVKA II or both. Inclusion of tumor markers in addition to parameters of tumor morphology might be the key to establish the best criteria for liver transplantation for HCC.
Introduction
Primary liver cancer, 95% of which is hepatocellular carcinoma (HCC), is ranked third in men and fifth in women as a cause of death from malignancy in Japan 1. Since 1975 the numbers of deaths and death rate of HCC have gradually increased. These numbers peaked at 34,510 and 27.4/100,000, respectively, in 2004, but decreased to 33,662 annual deaths and a 26.7/100,000 death rate in 2006.
Hepatitis B virus (HBV) and hepatitis C virus (HCV) infections are both major causes of HCC in Japan. HBV- and HCV-related HCC represents 15 and 70% of all cases, respectively. While HBV hepatitis predominates in most Asian countries, HCV hepatitis is more predominant in Japan, like in Western countries. The incidence of HCC without both hepatitis B surface antigen (HBsAg) and antibodies to HCV (anti-HCV) accounts for 15% of HCC patients nationwide.
Although liver resection and loco-regional treatment are regarded as potential curative therapies for HCC, the limited functional reserve of the liver restricts their application, and there is a high chance of recurrence in the remnant liver.
Liver transplantation appears to be the only ideal treatment since it provides the potential for cure of both the HCC and the underlying liver disease. In Japan, however, there have been only 81 cases of diseased donor organ procurement over the last 12 years after the implementation of the brain-death law for organ transplantation in 1997. In addition to many traditional constraints, the scarcity appears to be the result of tight legal regulation of diseased-organ donation. Therefore, living donor liver transplantation (LDLT) has developed rapidly as an alternative to deceased donor liver transplantation (DDLT). By the end of 2008, more than 5,000 LDLTs had been performed in Japan. LDLT in adults has allowed timely grafting for HCC patients and tentative expansion of the criteria for transplant candidacy in patients with HCC—although such expansion is fraught with controversy.
We reviewed LDLT for HCC, focusing on the overall outcomes and proposed criteria to expand the Milan and UCSF criteria in Japan.
Living donor liver transplantation for HCC in Japan
Table 1 presents the demographics and outcomes of three single-center [2-4] and one multicenter study from Japan 5. All centers uniformly preclude HCC with extrahepatic tumor spread and macrovascular invasion to both the portal vein and hepatic vein as basic criteria. Table 2 shows the current indication of LDLT for HCC. Most of the centers in Japan do not have rigorous criteria and elect the candidates on a case-by-case basis. Since 2002, Tokyo University has used the criteria of HCC up to 5 nodules with a maximum tumor size ≤5 cm in diameter.
| Center | Year | LDLT for HCC (cases) | Liver disease (%) | Pre-treatment (%) | Mortality (%) | Recurrence (%) | Patient survival | Median follow-up (months) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HBV | HCV | 1 year (%) | 3 years (%) | 5 years (%) | |||||||
| Single-center studies | |||||||||||
| Kyoto University | 2007 | 136 | 35 | 56 | 74 | 25 | 15 | – | – | 70 | 27 |
| Kyusyu University | 2009 | 90 | 13 | 77 | 68 | – | 16 | 92 | 81 | 78 | 28 |
| Tokyo University | 2007 | 78 | – | 62 | 78 | 15 | 8 | 91 | 82 | 75 | 24 |
| Multicenter study | |||||||||||
| 49 centers | 2007 | 653 | 30 | 59 | 71 | 24 | 14 | 83 | 73 | 69 | 21 |
- LDLT Living donor liver transplantation, HCC hepatocellular carcinoma
| Center | Year | LDLT for HCC no | Basic criteria | Current criteria | Proposed criteria | Within Milan (%)a | Within proposed criteria (%)a |
|---|---|---|---|---|---|---|---|
| Single-center studies | |||||||
| Kyoto University | 2007 | 136 | ◯ | TN ≤ 10, TS ≤5 cm, PIVKA II ≤400 | 54 | 65 | |
| Kyusyu University | 2007 | 60 | ◯ | TS ≤5 cm, PIVKA II ≤300 | (40) | (94) | |
| Tokyo University | 2007 | 78 | ◯ | TN ≤5, TS ≤5 cm | 87 | 92 | |
| Multicenter studies | |||||||
| 49 centers | 2007 | 653 | ◯ | Milan criteria + AFP ≤200 and PIVKA II ≤100 (A-P level) | 54 (61) | 77 (81) |
- LDLT Living donor liver transplantation, HCC hepatocellular carcinoma, TN tumor number, TS maximum tumor size, AFP a fetoprotein, PIVKA II protein induced by vitamin K absence-2
- Basic criteria: no extrahepatic spread and no vascular invasion, ◯: fulfill the criteria
- a Percent within each criteria by pathology (by pretransplant imaging study)
Kyoto University experiences
The group at Kyoto University has a great deal of experience with LDLT for HCC. In 2008, Takada and coauthors published a retrospective analysis of 136 patients who underwent LDLT for HCC between 1999 and 2007 [2, 6]. Based on preoperative imaging studies, 74 patients met the Milan criteria, and 62 did not. The overall patient survival rate at 5 years was 70%. Patients who exceeded the Milan criteria but presented with ≤10 tumors, all ≤5 cm in diameter (n = 33), displayed a similar 5-year recurrence rate to those within the Milan criteria (7 vs. 10%). Based on the results of multivariate analysis of risk factors for recurrence, the author defined the new criteria as n ≤10 tumors, all ≤5 cm in diameter and PIVKA II ≤400 mAU/ml. The 5-year recurrence rate for the 83 patients who met the new criteria was significantly lower than for the 44 patients who exceeded them (5 vs. 61%, p < 0.0001). Similarly, patients who met the new criteria showed a significantly better 5-year survival rate (87 vs. 37%, p < 0.0001). The selection criteria may be safely extended up to n ≤10, all ≤5 cm in diameter and PIVKA II ≤400 mAU/ml with acceptable outcomes.
Kyusyu University experiences
The group at Kyusyu University retrospectively analyzed the 90 patients who received LDLT for HCC between 1996 and 2007 [7, 8]. The recurrence-free survival rates of all 90 patients were 86.0, 81.3, and 81.3% at 1, 3, and 5 years, respectively. Fourteen of 90 patients developed a recurrence of tumor after the LDLT. In a multivariate analysis, both the tumor size of less than 5 cm (P = 0.0202) and the des-gamma-carboxy prothrombin (DCP: same as PIVKA II) level of less than 300 mAU/ml (P = 0.0001) were found to be independent factors for the recurrence of HCC after LDLT. Therefore, the authors devised new selection criteria for HCC patients (tumor size of <5 cm or a DCP of <300 mAU/ml). The 1-, 3-, and 5-year overall or recurrence-free survival rates of the 85 patients who met the new criteria were 92.3, 85.9, and 82.7%, or 90.5, 87.0, and 87.0%, respectively, which were significantly different from those of the five patients who did not meet the new criteria (P < 0.0001). The author concluded that the combination of two factors, the tumor size and DCP level, was found to be useful for expanding the selection of LDLT candidates for HCC.
Tokyo University experiences
The group at Tokyo University has also spearheaded successful LDLT for HCC 4. Their 2007 publication demonstrates that a total of 78 adult patients underwent adult LDLT between April 1996 and October 2005. Overall and recurrence-free survivals at 5 years after transplantation were 75 and 90%, respectively, with a median follow-up of 2 years. When stratified by the 5–5 rule, recurrence-free survival at 3 years for patients fulfilling the criteria and those exceeding the criteria was 94 and 50%, respectively. The author concluded that the indication for HCC might be expanded from the Milan criteria with equivalent outcomes. Further study, however, is necessary to justify the general application of the 5–5 rule. Our institutional guideline for HCC in LDLT has been up to 5 nodules with a maximum diameter of 5 cm (5–5 rule).
Multicenter study in Japan
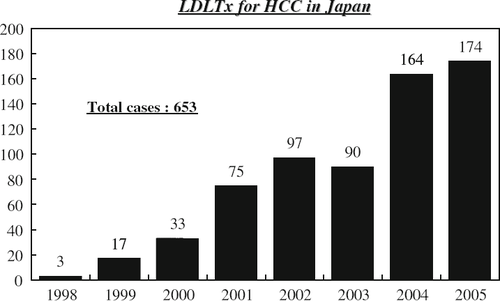
A large survey was conducted of 49 centers in Japan, and a total of 653 patients with HCC who received LDLT was reported 5 (Fig. 1). Median age was 56 years (range, 21–70 years). Males were three times more predominant than females. HCV infection was a leading cause of liver cirrhosis, occurring in 385 recipients (59%) versus HBV for 199 (30%). Half the patients had advanced liver failure with Child C, whereas 30% had Child B and 10% Child A.
Of the 653 recipients, 497 (76.1%) were alive without (n = 451) or with (n = 46) HCC recurrence; 156 (23.9%) had died of recurrent HCC (n = 46) or for other reasons (n = 110). A median follow-up period was 21.5 months. Actuarial patient survival was 82.6% at 1 year, 72.6% at 3 years, and 68.9% at 5 years; actuarial disease-free survival was 77.4% at 1-year, 65.1% at 3 years, and 61.5% at 5 years (Fig. 2). By univariate analysis, alfa-fetoprotein (AFP) and protein induced by vitamin K absence factor II (PIVKA II, or DCP, des-gamma carboxy prothrombin), MELD score, and tumor characteristics of explanted livers were found to be important risk factors for patient survival. AFP and PIVKA II/DCP were found to be independent risk factors for patient survival by multivariate analysis.
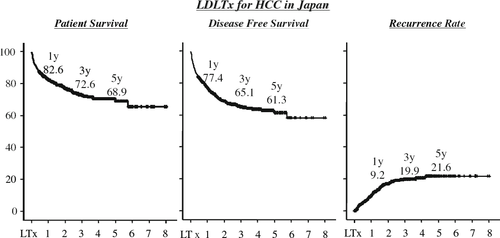
Ninety-two recipients (14.1%) developed recurrence after LDLT. The cumulative recurrence rate was 9.2% at 1 year, 19.9% at 3 years, and 21.6% at 5 years. Tumor stage, age, AFP, PIVKA II, and pathological characteristics of tumors (e.g., number and size of tumors, distribution, vascular invasion, and differentiation) were closely associated with HCC recurrence by univariate analysis. By multivariate analysis, AFP, PIVKA II, vascular invasion, and number, distribution, and size of tumors were found to be independent risk factors for recurrence.
Based on the fact that high serum AFP and PIVKA II levels before LDLT were closely associated with biological aggressiveness of HCC as expressed by macroscopic vascular invasion, larger tumor size, and more nodules, and related to worse patient survival and disease-free survival, new proposed criteria including AFP and PIVKA II (referred as the A-P level) were introduced. AFP ≤200 ng/ml and PIVKA II ≤100 mAU/ml were set as cutoff values.
By postoperative pathological study, 5-year disease-free survival of those who met (n = 325) and exceeded (n = 272) the Milan criteria were 95.3 and 66.4%, respectively. When the A-P levels were below the criteria, the 5-year disease-free survival of the patients who were within and exceeded the Milan criteria were 99.5% (n = 208) and 84.3% (n = 124), respectively, while those with higher A-P levels had a 5-year disease-free survival of 85.0% (n = 96) and 45.0% (n = 131), respectively. Half the patients who exceeded the criteria but who satisfied the A-P levels were found to survive as long as those who met the criteria (Fig. 3). Similar results were obtained from a preoperative imaging study.
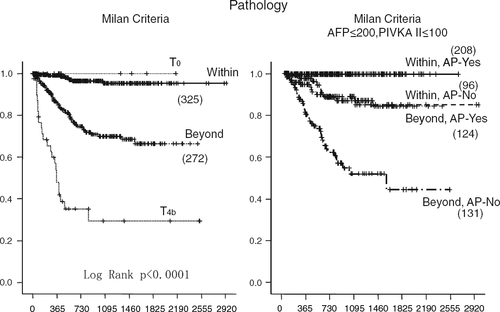
The authors concluded that by using the Milan criteria and the A-P levels, they could differentiate the outcome of the recipients who were beyond the Milan criteria into 2 groups: low A-P level patients (50%) with satisfactory survival without recurrence and high A-P level patients (50%) with high recurrence rates in both LDLT and DDLT.
Ethical issues
An ethical dilemma in LDLT for HCC is whether the selection criteria should be the same as for DDLT. While a deceased donor graft is a scarce resource in the allocation system, a living donor liver graft is a gift to a dedicated recipient. While the decision for a DDLT is based on a comparison of the outcome of two recipients, the decision for LDLT is a balance of the risks and benefits for the donor and recipient. This special relationship between a donor and recipient can provide a recipient with the opportunity to undergo LDLT even for advanced HCC. Patients with advanced lesions cannot always be considered as having a contraindication. A high probability of tumor recurrence, however, provokes ethical issues concerning risks to the living donor. The present dilemma is that there are no accepted criteria for patients with tumors outside the conventional criteria. A living donor is not a public resource, but is occasionally directed to a certain recipient with advanced HCC. Because of the unique features of LDLT, the indeterminate survival outcome, such as a 5-year patient survival rate of 50%, can be justified without critical impairment of donor ethics. There is another ethical dilemma in LDLT for advanced HCC concerning whether re-transplantation using a deceased donor graft should be allowed if living donor graft failure occurred, since these patients were not eligible for deceased donor graft allocation in the first place 9.
Proposed criteria for use of LDLT for HCC
There is a major difference between LDLT and DDLT in developing the expanded criteria for HCC. While DDLT centers mainly in the Western hemisphere are expanding the selection criteria, LDLT centers mainly in the Eastern hemisphere, including Japan, are tightening the selection criteria. Since the application of the Milan criteria in 1996, most DDLT centers have had an allocation system based on either these criteria or similar ones 10. Some DDLT centers have expanded the criteria, like the UCSF 11, because of the concern that the Milan criteria are too stringent. Most LDLT centers, on the other hand, do not have rigorous criteria in the first place and elect the candidates on a case-by-case basis. Therefore, to develop expanded criteria means tightening their criteria for LDLT centers.
Expanded criteria are proposed from three single-center and one multicenter study in Japan (Table 2). Those criteria are based on the independent predictors for outcome derived from the analyses of the pretransplant factors and explant pathology.
The proposed criteria are tumor size ≤5 cm, tumor number ≤10, and PIVKA II ≤400 in Kyoto University [2, 6]; tumor size ≤5 cm and PIVKA II ≤300 in Kyusyu University [3, 8]; and Milan criteria with AFP ≤200 and PIVKA II ≤100 in a Japanese multicenter study 5.
To date, the gold standard for selection of HCC patients for both DDLT and LDLT is the Milan criteria, and the UCSF criteria are regarded as acceptable expanded guidelines. Both criteria are based on tumor morphology, including tumor size and number. Most of those proposed criteria from LDLT centers include tumor markers such as AFP and PIVKA II in addition to factors of tumor morphology, such as tumor size and number.
The beneficial effect of these proposed criteria can be predicted by the inclusion rates of the patients compared to Milan or UCSF criteria in the same cohort, and the outcome of these included patients. While application of the UCSF criteria increases inclusion rates by 5–10% compared to the Milan criteria, these proposed criteria increase inclusion rates by 5–54% compared to the Milan criteria (Table 2). The higher inclusion rates compared to the application of the Milan criteria are achieved by the criteria that include tumor markers, either AFP or PIVKA II or both. Inclusion of tumor markers in addition to parameters of tumor morphology might be the key to establishing the best criteria for liver transplantation for HCC.
Pretransplant treatment
The rationale for using pretransplant treatment in liver transplantation is (1) to prevent dropouts from waiting list, (2) to improve the posttransplant survival, and (3) down-staging the tumor to meet currently available criteria (e.g., Milan) to perform liver transplantation. Thus, in case of LDLT the aim of pretreatment is (2) and (3).
Of the 653 recipients in the Japanese multicenter study, 466 (71.4%) received various adjuvant treatments, alone or in combination, before LDLT: transarterial chemoembolization (n = 374; 57%), percutaneous ethanol injection (n = 187; 29%), radiofrequency ablation or microwave coagulation therapy (n = 92; 14%), and liver resection (n = 69; 11%) 5. Neither pretransplant treatments nor the type of modalities showed any influence on the patient survival and recurrence rate compared with those of the recipients who received no treatment. An intriguing study was reported by Kyoto University 12. The patients were divided into three groups based on pretransplant therapy: patients without any therapy (group 1), patients with one or two sessions of ablative treatment (group 2), and patients with three or more sessions of treatment (group 3), reflecting differences in the median time elapsed from the diagnosis of HCC to LDLT. The patients who received one or two sessions of ablative therapy had the best 4-year survival (80% for group 2 vs. 52% for group 1, and 58% for group 3) and the lowest recurrence rate (9% for group 2 vs. 9% for group 1 and 37% for group 3). It seems that one or two sessions of pre-transplant treatment brings the best outcome after liver transplantation. This should be confirmed in a further study with a larger cohort.
Summary
Despite a wide spectrum of selection criteria among LDLT centers in Japan, LDLT for HCC can achieve an acceptable outcome, which is comparable to the outcome of DDLT for HCC. One of the most crucial requirements in liver transplantation for HCC is the advent of expanded criteria that allow more patients with HCC to receive the organs and offer similar or even better results compared to the Milan or UCSF criteria. Apparently many criteria have been proposed by LDLT centers, which mostly include the tumor markers such as AFP and PIVKA II in addition to the factors of tumor morphology. Validation of novel criteria, verified and selected from these criteria, will be a major advance in clarifying the indications for liver transplantation for HCC.