A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression
Abstract
No network meta-analysis has examined the relative effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression, while this is a very important clinical issue. We conducted systematic searches in bibliographical databases to identify randomized trials in which a psychotherapy and a pharmacotherapy for the acute or long-term treatment of depression were compared with each other, or in which the combination of a psychotherapy and a pharmacotherapy was compared with either one alone. The main outcome was treatment response (50% improvement between baseline and endpoint). Remission and acceptability (defined as study drop-out for any reason) were also examined. Possible moderators that were assessed included chronic and treatment-resistant depression and baseline severity of depression. Data were pooled as relative risk (RR) using a random-effects model. A total of 101 studies with 11,910 patients were included. Depression in most studies was moderate to severe. In the network meta-analysis, combined treatment was more effective than psychotherapy alone (RR=1.27; 95% CI: 1.14-1.39) and pharmacotherapy alone (RR=1.25; 95% CI: 1.14-1.37) in achieving response at the end of treatment. No significant difference was found between psychotherapy alone and pharmacotherapy alone (RR=0.99; 95% CI: 0.92-1.08). Similar results were found for remission. Combined treatment (RR=1.23; 95% CI: 1.05-1.45) and psychotherapy alone (RR=1.17; 95% CI: 1.02-1.32) were more acceptable than pharmacotherapy. Results were similar for chronic and treatment-resistant depression. The combination of psychotherapy and pharmacotherapy seems to be the best choice for patients with moderate depression. More research is needed on long-term effects of treatments (including cost-effectiveness), on the impact of specific pharmacological and non-pharmacological approaches, and on the effects in specific populations of patients.
Mental disorders are a major cause of global health burden, accounting for 23% of years lived with disability1. With 350 million people affected in the world, depressive disorder is the second leading cause of global burden2. The high direct and indirect costs of major depression are substantially due to significant deficits in treatment provision3. There are a number of efficacious interventions for depressive disorder, and the key challenge is how best to implement currently available effective treatments4.
It is well-established that psychotherapies and pharmacological therapies are effective in the treatment of adult depression. Psychotherapies have shown superior effects compared to control conditions in numerous clinical trials. Moreover, different psychotherapeutic types – e.g., cognitive behavior therapy (CBT) and interpersonal therapy – have comparable outcomes in depression5. Another large body of research has shown that different classes of antidepressants are effective in the treatment of depression6, including selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs) and several others.
Although the absolute effectiveness of psychotherapies and pharmacotherapies is well documented, the evidence supporting their relative effects remains inconclusive. Conventional meta-analyses of trials directly comparing psychotherapies and pharmacotherapies have suggested that, as classes of treatments, they have comparable effects, with no or only minor differences7, 8, although there may be some influence of placebo effects9, sponsorship bias10, and possibly the superiority of some medications over others6. Other pairwise meta-analyses have found that the combination of psychotherapy and pharmacotherapy may be more effective than either of these alone11, 12, although the evidence is not conclusive13, 14. Moreover, some studies suggest that the two monotherapies result in differential effects over long-term follow-ups, with psychotherapy having enduring effects on depression when pharmacotherapy is discontinued.
Several issues regarding the differential effects of combined treatment, psychotherapies and pharmacotherapies remain unsolved. Existing meta-analyses have compared only two interventions at a time: psychotherapy vs. pharmacotherapy15, combined treatment vs. psychotherapy14, and combined treatment vs. pharmacotherapy11, 12. To get a better understanding of the relative effectiveness of these treatments, it is necessary to combine direct and indirect evidence from all clinical trials. Network meta-analyses can combine multiple comparisons in one analysis, are able to use direct and indirect evidence, and thus make optimal use of all available evidence. These analyses consequently make better estimates of the differences between treatments, have more statistical power to examine moderators of outcome, and can present consolidated comparisons among alternative treatments16.
Further important questions have not yet been answered. The majority of randomized trials in this field may be prone to methodological bias; no information is available for different populations of patients (e.g., mild vs. chronic or treatment-resistant depression); and acceptability of the treatments has not been examined extensively so far.
We therefore conducted a network meta-analysis based on randomized trials in which a psychotherapy and a pharmacotherapy for depression were compared with each other, or in which the combination of a psychotherapy and a pharmacotherapy was compared with either one alone.
METHODS
Identification and selection of studies
The protocol for this network meta-analysis was registered at PROSPERO (CRD42018114961). For the identification of studies, we used a database of randomized trials examining the effects of psychotherapies in depression, that was developed through a comprehensive literature search (from 1966 to January 1, 2018)17. Four major bibliographical databases (PubMed, PsycINFO, EMBASE and the Cochrane Library) were searched by combining index and text words indicative of depression and psychotherapies, with filters for randomized controlled trials. All records and full texts were screened by two independent researchers. Any disagreement was solved through discussion.
We included studies in which a psychotherapy and a pharmacological treatment for depression were directly compared with each other, and studies in which the combination of a psychotherapy and a pharmacological treatment was compared with either one alone. When these trials included pill placebo or the combination of psychotherapy and pill placebo, we included such arms as well.
We defined psychotherapy as “the informed and intentional application of clinical methods and interpersonal stances derived from established psychological principles for the purpose of assisting people to modify their behaviors, cognitions, emotions and/or other personal characteristics in directions that the participants deem desirable”18. We allowed any type of psychotherapy8 in any delivery format (individual, group, face-to-face, telephone, or self-help including Internet) and any type of oral antidepressant treatment within the therapeutic dose range.
We only included studies recruiting patients with acute depressive disorder according to modern operationalized and validated criteria. Comorbid mental or somatic disorders were not excluded. We did not set a maximum or minimum concerning the length of treatment or the duration of follow-up7.
When a study contained two or more arms to be included in the same node (for example, when one study compared two types of psychotherapy with one pharmacotherapy condition), we considered them as separate comparisons and subdivided the comparisons appropriately in order to avoid double counting19. We also conducted sensitivity analyses in which the two comparable arms were pooled into one arm.
Risk of bias and data extraction
Two independent researchers assessed the risk of bias of included studies using four criteria of the Cochrane tool20. Disagreements were solved through discussion. Pharmacotherapy studies were also assessed regarding the use of therapeutic dose6 and the titration schedule (i.e., therapeutic dose achieved within three weeks). The pharmacotherapy was deemed adequate if both criteria were met. Psychotherapies were assessed with respect to using a treatment manual, provision of therapy by specially trained therapists, and verification of treatment integrity21, 22.
We also coded participant characteristics (type of depressive disorder, recruitment method, target group); the type of psychotherapy and the number of treatment sessions; the type of medication; whether or not a placebo condition was included in the trial (because then patients were blinded for medication or placebo)9; the time between pre-test and post-test (in weeks); and the country where the study was conducted.
Outcome measures
Treatment response, defined as a 50% reduction in depressive symptomatology according to a standardized rating scale, was chosen as the primary outcome. When not reported, we imputed response rate using a validated method23. The timepoint for the primary outcome was the end of the therapy. We also calculated response rates at follow-up of 6 months, between 6 and 12 months, and more than 12 months.
Remission rate was defined as the number of patients with a score for depressive symptoms below a specific cut-off on a validated rating scale. We also calculated the standardized mean difference (SMD) between pairs of conditions, expressing the size of the intervention effect in each study relative to the variability observed in that study. Acceptability of the treatment formats was operationalized as study drop-out for any reason during the acute phase treatment.
Meta-analyses
We conducted pairwise meta-analyses for all comparisons, using a random effects pooling model. To quantify heterogeneity, we calculated the I2 statistic with 95% confidence intervals (CIs), using the non-central chi-squared-based approach within the heterogi module for Stata24. We tested for small study effects, including publication bias, with Egger's test25.
The comparative effectiveness was evaluated using the network meta-analysis methodology. First, we summarized the geometry of the network of evidence using network plots for the main outcome26. Second, we conducted contrast-based analyses to assess comparative efficacy and acceptability27. Given the expected clinical and methodological heterogeneity of treatment effects among the studies, we adopted the multivariate random effect models28. Relative risks (RRs) and SMDs were reported with their 95% CIs. The ranking of treatment formats was estimated according to the “surface under the cumulative ranking” (SUCRA), based on the estimated multivariate random effects models26. We checked the consistency of the network using tests of local and global inconsistency29, 30.
Further analyses
We conducted separate pairwise and network meta-analyses for studies examining chronic or treatment-resistant depression. We also selected studies that reported the baseline score on the Hamilton Depression Rating Scale (HAM-D)31 and examined in a meta-regression analysis whether baseline severity was associated with outcome. We then conducted separate pairwise and network meta-analyses for mild, moderate and severe depression according to the baseline severity of the sample, using the thresholds proposed by Zimmerman et al32. In addition, we performed a multivariate meta-regression analysis to examine possible sources of heterogeneity.
We carried out a series of sensitivity analyses with studies in which pharmacotherapy was optimized; those in which psychotherapy met all the above-mentioned quality criteria; those at low risk of bias; and those in which no placebo was included. A sensitivity analysis was also conducted in which all patients randomized to different arms in the same node (e.g., two types of psychotherapy) in a given study were pooled, so that there was only one arm for each condition.
All analyses were conducted in Stata/SE 14.2.
RESULTS
Studies included and their characteristics
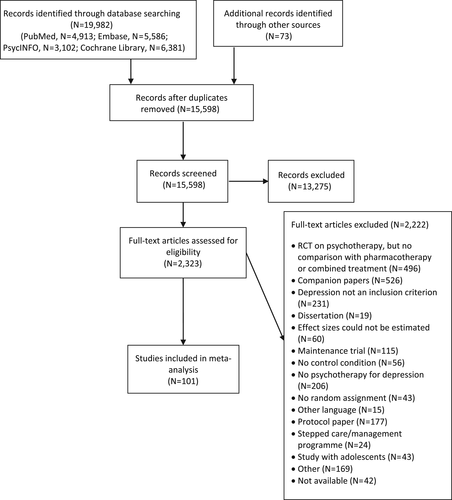
After examining a total of 19,982 abstracts (15,598 after removal of duplicates), we retrieved 2,323 full-text papers for further consideration. The PRISMA flow chart describing the inclusion process is presented in Figure 1. A total of 101 studies met inclusion criteria (11,910 participants overall: 2,587 randomized to combined treatment, 3,625 to psychotherapy, 4,769 to pharmacotherapy, 632 to placebo and 297 to psychotherapy plus placebo)33-133.
Selected characteristics of the included studies are summarized in Table 1. In 12 studies two types of psychotherapy were examined as separate arms; in one study two types of pharmacotherapy were included62; and in one other study the therapy was separated into two arms with different providers (general practitioners or nurses)105. In total, 115 comparisons were available in the studies.
| Study | Conditions | Psychotherapy | Therapy quality | Pharmacotherapy | Adequate therapy | Risk of bias |
|---|---|---|---|---|---|---|
| Ahmadpanah et al33 | Combined vs. pharmacotherapy | MBCT | – – – | SSRI | Yes | + + + + |
| Combined vs. pharmacotherapy | Stress management | – – – | SSRI | Yes | + + + + | |
| Altamura et al34 | Psychotherapy vs. pharmacotherapy | IPT | + + – | SSRI | Yes | + – + – |
| Appleby et al35 | Combined vs. pharmacotherapy vs. placebo vs. psychotherapy + placebo | CBT | – + – | SSRI | No | + – + + |
| Ashouri et al36 | Combined vs. pharmacotherapy | CBT | – – – | Other | No | – – sr – |
| Combined vs. pharmacotherapy | MBCT | – – – | Other | No | – – sr – | |
| Barber et al37 | Psychotherapy vs. pharmacotherapy vs. placebo | DYN | + + – | Other | Yes | + – + + |
| Barrett et al38 | Psychotherapy vs. pharmacotherapy vs. placebo | PST | + + – | SSRI | Yes | + – + – |
| Beck et al39 | Combined vs. psychotherapy | CBT | + + – | TCA | Yes | – – – – |
| Bedi et al40 | Psychotherapy vs. pharmacotherapy | Not specified | – + – | Other | No | – + sr – |
| Bellack et al41 | Combined vs. pharmacotherapy vs. psychotherapy + placebo | Social skills | + + – | TCA | Yes | – – + – |
| Bellino et al42 | Combined vs. pharmacotherapy | IPT | + + – | SSRI | Yes | – – + – |
| Blackburn et al43 | Combined vs. psychotherapy vs. pharmacotherapy | CBT | – – – | TCA | Yes | – – – – |
| Blackburn & Moore44 | Psychotherapy vs. pharmacotherapy | CBT | – + – | Other | No | – – + – |
| Bloch et al45 | Combined vs. psychotherapy + placebo | DYN | – + + | SSRI | Yes | + + + + |
| Blom et al46 | Combined vs. psychotherapy vs. pharmacotherapy vs. psychotherapy + placebo | IPT | + + + | Other | Yes | – – + + |
| Browne et al47 | Combined vs. psychotherapy vs. pharmacotherapy | IPT | + + + | SSRI | Yes | + + + – |
| Burnand et al48 | Combined vs. pharmacotherapy | DYN | – + + | Other | Yes | – – + – |
| Chibanda et al49 | Psychotherapy vs. pharmacotherapy | PST | + + + | TCA | No | + – sr – |
| Corruble et al50 | Combined vs. pharmacotherapy | Social rhythms | + + + | Other | No | + + + – |
| Covi & Lipman51 | Combined vs. psychotherapy | CBT | + + + | TCA | Yes | – – sr – |
| David et al52 | Psychotherapy vs. pharmacotherapy | CT | + + + | SSRI | Yes | – – + + |
| Psychotherapy vs. pharmacotherapy | REBT | + + + | SSRI | Yes | – – + + | |
| De Jonghe et al53 | Combined vs. pharmacotherapy | DYN | + + + | Other | No | – – + + |
| De Jonghe et al54 | Combined vs. psychotherapy | DYN | + + + | Other | No | – – + – |
| de Mello et al55 | Combined vs. pharmacotherapy | IPT | + + – | Other | Yes | – – + – |
| Dekker et al56 | Psychotherapy vs. pharmacotherapy | DYN | + + + | Other | No | – – + – |
| Denton et al57 | Combined vs. pharmacotherapy | EFT | + + + | Other | No | + + + + |
| DeRubeis et al58 | Psychotherapy vs. pharmacotherapy | CBT | + + + | SSRI | Yes | – – + + |
| Dimidjian et al59 | Psychotherapy vs. pharmacotherapy | BAT | + + + | SSRI | Yes | + – + + |
| Psychotherapy vs. pharmacotherapy | CBT | + + + | SSRI | Yes | + – + + | |
| Dozois et al60 | Combined vs. pharmacotherapy | CBT | + + + | Other | No | – + – – |
| Dunlop et al61 | Psychotherapy vs. pharmacotherapy | CBT | + – – | SSRI | Yes | – + + – |
| Dunlop et al62 | Psychotherapy vs. pharmacotherapy | CBT | + + + | Other | Yes | + + + + |
| Psychotherapy vs. pharmacotherapy | CBT | + + + | SSRI | Yes | + + + + | |
| Dunn63 | Combined vs. pharmacotherapy | CBT | – – – | Other | No | – – sr – |
| Dunner et al64 | Psychotherapy vs. pharmacotherapy | CBT | + + + | SSRI | Yes | – – + – |
| Eisendrath et al65 | Combined vs. pharmacotherapy | MBCT | + + + | Other | No | + + + + |
| Elkin et al66 | Psychotherapy vs. pharmacotherapy vs. placebo | CBT | + + + | TCA | Yes | + + + + |
| Psychotherapy vs. pharmacotherapy vs. placebo | IPT | + + + | TCA | Yes | + + + + | |
| Faramarzi et al67 | Psychotherapy vs. pharmacotherapy | CBT | + – – | SSRI | Yes | – – sr – |
| Finkenzeller et al68 | Combined vs. psychotherapy vs. pharmacotherapy | IPT | + – – | SSRI | Yes | + – + + |
| Frank et al69 | Psychotherapy vs. pharmacotherapy | IPT | + + + | SSRI | Yes | – – + + |
| Gater et al70 | Combined vs. psychotherapy vs. pharmacotherapy | Social group | + + + | Other | No | + + + + |
| Gaudiano et al71 | Combined vs. pharmacotherapy | ABT | + + + | Other | No | – – + + |
| Hautzinger et al72 | Combined vs. psychotherapy vs. pharmacotherapy | CBT | – – – | TCA | Yes | – – + + |
| Hegerl et al73 | Psychotherapy vs. pharmacotherapy vs. placebo | CBT | + – + | SSRI | Yes | + + + + |
| Hellerstein et al74 | Combined vs. pharmacotherapy | Cognitive-interpersonal | + + + | SSRI | Yes | – – – + |
| Hollon et al75 | Combined vs. psychotherapy vs. pharmacotherapy | CBT | + + + | TCA | Yes | – – + + |
| Hollon et al76 | Combined vs. pharmacotherapy | CBT | + + + | Other | No | + + + + |
| Hsiao et al77 | Combined vs. pharmacotherapy | BMS | + + – | Other | No | + – sr + |
| Husain et al78 | Psychotherapy vs. pharmacotherapy | CBT | + – – | Other | No | + + + + |
| Jarrett et al79 | Psychotherapy vs. pharmacotherapy vs. placebo | CBT | + + + | Other | Yes | – + + + |
| Keller et al80 | Combined vs. psychotherapy vs. pharmacotherapy | CBASP | + + + | Other | Yes | + + + + |
| Kennedy et al81 | Psychotherapy vs. pharmacotherapy | CBT | + + + | Other | Yes | – – – – |
| Lam et al82 | Combined vs. pharmacotherapy | CBT | + + + | SSRI | Yes | + + + + |
| Lesperance et al83 | Combined vs. pharmacotherapy vs. placebo vs. psychotherapy + placebo | IPT | + + + | SSRI | Yes | + + + + |
| Lynch et al84 | Combined vs. pharmacotherapy | DBT | – + + | Other | No | – – – – |
| Macaskill & Macaskill85 | Combined vs. pharmacotherapy | CBT | + – – | TCA | Yes | – – – – |
| Maina et al86 | Combined vs. pharmacotherapy | DYN | – + + | SSRI | Yes | + + + + |
| Maldonado López87 | Psychotherapy vs. pharmacotherapy | CBT | – – – | Other | No | – – + – |
| Psychotherapy vs. pharmacotherapy | BAT | – – – | Other | No | – – + – | |
| Maldonado López 88 | Combined vs. pharmacotherapy | CBT | – – – | Other | No | – – + – |
| Combined vs. pharmacotherapy | BAT | – – – | Other | No | – – + – | |
| Markowitz et al89 | Combined vs. psychotherapy | SUP | + + + | TCA | Yes | + + + + |
| Markowitz et al90 | Combined vs. psychotherapy vs. pharmacotherapy | IPT | + + + | SSRI | Yes | + + + + |
| Psychotherapy vs. pharmacotherapy | SUP | + + + | SSRI | Yes | + + + + | |
| Marshall et al91 | Psychotherapy vs. pharmacotherapy | CBT | + + + | Other | No | – – – – |
| Psychotherapy vs. pharmacotherapy | IPT | + + + | Other | No | – – – – | |
| Martin et al92 | Psychotherapy vs. pharmacotherapy | IPT | + + – | Other | Yes | – – – + |
| McKnight et al93 | Psychotherapy vs. pharmacotherapy | CBT | + + – | TCA | No | – – sr – |
| McLean & Hakstian94 | Psychotherapy vs. pharmacotherapy | CBT | + + + | TCA | Yes | – – sr – |
| Psychotherapy vs. pharmacotherapy | DYN | + + + | TCA | Yes | – – sr – | |
| Menchetti et al95 | Psychotherapy vs. pharmacotherapy | IPT | + – – | SSRI | No | + + – + |
| Milgrom et al96 | Combined vs. psychotherapy vs. pharmacotherapy | CBT | + – + | SSRI | Yes | + + sr + |
| Miranda et al97 | Psychotherapy vs. pharmacotherapy | CBT | + + + | Other | No | + + + + |
| Misri et al98 | Combined vs. pharmacotherapy | CBT | + + – | SSRI | No | + – + + |
| Mitchell et al99 | Combined vs. pharmacotherapy | PST | + – + | Other | No | + + + + |
| Mohr et al100 | Psychotherapy vs. pharmacotherapy | CBT | + – + | SSRI | Yes | – – – + |
| Psychotherapy vs. pharmacotherapy | SEG | + – + | SSRI | Yes | – – – + | |
| Moradveisi et al101 | Psychotherapy vs. pharmacotherapy | BAT | + + + | SSRI | Yes | + + + + |
| Murphy et al102 | Combined vs. psychotherapy vs. pharmacotherapy vs. psychotherapy + placebo | CBT | + + + | TCA | Yes | + + – + |
| Murphy et al103 | Psychotherapy vs. pharmacotherapy | CBT | + + + | TCA | Yes | + – – – |
| Mynors-Wallis et al104 | Psychotherapy vs. pharmacotherapy vs. placebo | PST | + + – | TCA | Yes | – + + – |
| Mynors-Wallis et al105 | Psychotherapy vs. pharmacotherapy | PST | + – + | SSRI | Yes | + + + + |
| Combined vs. psychotherapy vs. pharmacotherapy | PST | + – + | SSRI | Yes | + + + + | |
| Naeem et al106 | Combined vs. pharmacotherapy | CBT | + + + | SSRI | Yes | + + sr + |
| Parker et al107 | Psychotherapy vs. pharmacotherapy | CBT | + + – | Other | Yes | + + + – |
| Petrak et al108 | Psychotherapy vs. pharmacotherapy | CBT | + + – | SSRI | Yes | + + + + |
| Quilty et al109 | Psychotherapy vs. pharmacotherapy | CBT | + + + | Other | No | – – – + |
| Ravindran et al110 | Combined vs. pharmacotherapy vs. placebo vs. psychotherapy + placebo | CBT | + + – | SSRI | Yes | + + + – |
| Reynolds et al111 | Combined vs. pharmacotherapy vs. placebo vs. psychotherapy + placebo | IPT | + + + | TCA | Yes | – – + + |
| Rodriguez Vega et al112 | Combined vs. pharmacotherapy | Narrative | + + + | SSRI | Yes | + + sr + |
| Roth et al113 | Combined vs. psychotherapy | Self-control | + + + | TCA | Yes | – – – – |
| Rush et al114 | Psychotherapy vs. pharmacotherapy | CBT | + – + | TCA | Yes | – – + + |
| Rush & Watkins115 | Combined vs. psychotherapy | CBT | + – + | Other | No | – – sr + |
| Salminen et al116 | Psychotherapy vs. pharmacotherapy | DYN | – + – | SSRI | Yes | – – – + |
| Schiffer & Wineman117 | Combined vs. psychotherapy + placebo | Three types | – – – | TCA | Yes | – – – – |
| Schramm et al118 | Psychotherapy vs. pharmacotherapy | CBASP | + + + | SSRI | Yes | + – + + |
| Schulberg et al119 | Psychotherapy vs. pharmacotherapy | IPT | + + + | TCA | Yes | – – + + |
| Scott & Freeman120 | Psychotherapy vs. pharmacotherapy | CBT | + + – | TCA | Yes | – + + – |
| Psychotherapy vs. pharmacotherapy | SUP | – – – | TCA | Yes | – + + – | |
| Shamsaei et al121 | Combined vs. psychotherapy vs. pharmacotherapy | CBT | – – – | SSRI | Yes | + – sr – |
| Sharp et al122 | Psychotherapy vs. pharmacotherapy | SUP | – + + | Other | No | + + sr + |
| Souza et al123 | Combined vs. pharmacotherapy | IPT | + + + | Other | No | + + + + |
| Stravynski et al124 | Combined vs. psychotherapy | CBT | – – – | TCA | Yes | – – + – |
| Targ et al125 | Combined vs. psychotherapy + placebo | PST | – – + | SSRI | Yes | – – + – |
| Thompson et al126 | Combined vs. psychotherapy vs. pharmacotherapy | CBT | + – – | TCA | No | – – – + |
| Weissman et al127 | Combined vs. psychotherapy vs. pharmacotherapy | IPT | + – – | TCA | Yes | – – + – |
| Wiles et al128 | Combined vs. pharmacotherapy | CBT | + – + | Other | No | + + sr + |
| Wiles et al129 | Combined vs. pharmacotherapy | CBT | + + + | Other | No | + + sr + |
| Williams et al130 | Psychotherapy vs. pharmacotherapy vs. placebo | PST | + + – | SSRI | Yes | + + + + |
| Wilson131 | Combined vs. pharmacotherapy vs. placebo vs. psychotherapy + placebo | BAT | + – – | TCA | Yes | – – + – |
| Zisook et al132 | Combined vs. psychotherapy + placebo | SUP | – – – | SSRI | Yes | – – + + |
| Zu et al133 | Combined vs. psychotherapy vs. pharmacotherapy | CBT | – + + | SSRI | Yes | + – + – |
- Risk of bias: + means low risk, – means high or unclear risk, “sr” means that only a self-report instrument was used
- ABT – acceptance-based behavior therapy, BAT – behavioral activation therapy, BMS – body-mind-spirit therapy, CBASP – cognitive behavioral analysis system of psychotherapy, CBT – cognitive behavior therapy, CT – cognitive therapy, DBT – dialectical behavioral therapy, DYN – psychodynamic therapy, EFT – emotion-focused therapy, IPT – interpersonal psychotherapy, MBCT – mindfulness-based cognitive therapy, PST – problem-solving therapy, REBT – rational-emotive behavior therapy, SEG – supportive-expressive group psychotherapy, SUP – supportive therapy, SSRI – selective serotonin reuptake inhibitor, TCA – tricyclic antidepressant
The aggregated characteristics of the included studies are presented in Table 2. In brief, 47 trials recruited patients exclusively from clinical samples, and 75 were aimed at unselected adults. Thirteen studies were aimed at patients with chronic or treatment-resistant depression. CBT was the most commonly used psychotherapy (48 trials); an individual format was used in 81 psychotherapy studies; 45 trials met all three quality criteria. SSRIs were the most frequently used medications; pharmacotherapy was judged adequate in 67 trials. The time from pre- to post-test ranged from 4 to 36 weeks, with the majority of comparisons (78%) ranging from 8 to 16 weeks. In 36 of 51 trials reporting the mean baseline HAM-D score, the severity of depression was moderate.
| All studies | Combined vs. psychotherapy | Combined vs. pharmacotherapy | Psychotherapy vs. pharmacotherapy | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Patients | |||||||||
| Recruitment | Community | 35 | 34.7 | 9 | 40.9 | 14 | 29.2 | 21 | 36.8 |
| Clinical | 47 | 46.5 | 11 | 50.0 | 28 | 58.3 | 26 | 45.6 | |
| Other | 19 | 18.8 | 2 | 9.1 | 6 | 12.5 | 10 | 17.5 | |
| Target group | Adults | 75 | 74.3 | 17 | 77.3 | 33 | 68.8 | 46 | 80.7 |
| Specific group | 26 | 25.7 | 5 | 22.7 | 15 | 31.3 | 11 | 19.3 | |
| Chronic or treatment-resistant depression | 13 | 12.9 | 3 | 13.6 | 11 | 22.9 | 5 | 8.8 | |
| Psychotherapy | |||||||||
| Type | CBT | 48 | 47.5 | 12 | 54.5 | 21 | 43.8 | 31 | 54.4 |
| Other | 52 | 52.5 | 10 | 45.5 | 27 | 56.3 | 26 | 45.6 | |
| Format | Individual | 81 | 80.2 | 15 | 68.2 | 38 | 79.2 | 47 | 82.5 |
| Group/mixed | 20 | 19.8 | 7 | 31.8 | 10 | 20.8 | 10 | 17.5 | |
| Optimized | 45 | 44.6 | 11 | 50.0 | 22 | 45.8 | 26 | 45.6 | |
| Pharmacotherapy | |||||||||
| Type | SSRI | 38 | 37.6 | 6 | 27.3 | 17 | 35.4 | 24 | 42.1 |
| TCA | 26 | 25.7 | 11 | 50.0 | 11 | 22.9 | 15 | 26.3 | |
| Other | 37 | 36.6 | 5 | 22.7 | 20 | 41.7 | 18 | 31.6 | |
| Optimized | 67 | 66.3 | 18 | 81.8 | 28 | 58.3 | 43 | 75.4 | |
| General study characteristics | |||||||||
| Country | US | 53 | 52.5 | 14 | 63.6 | 23 | 47.9 | 29 | 50.9 |
| Europe | 32 | 31.7 | 5 | 22.7 | 15 | 31.3 | 20 | 35.1 | |
| Other | 16 | 15.8 | 3 | 13.6 | 10 | 20.8 | 8 | 14.0 | |
| Low risk of bias | 28 | 27.7 | 5 | 22.7 | 17 | 35.4 | 13 | 22.8 | |
- CBT – cognitive behavior therapy, SSRI – selective serotonin reuptake inhibitor, TCA – tricyclic antidepressant
There was moderate to high risk of bias in most trials. A total of 48 studies reported an adequate sequence generation; 40 reported allocation to conditions by an independent (third) party; and 81 reported blinding of outcome assessors or used only self-report outcomes. Intention-to-treat analyses were conducted in 58 studies. Twenty-three studies met all four quality criteria (28 when self-report was rated as low risk of bias), 19 met three criteria, another 19 met two criteria, and the remaining 40 studies met one or none of the criteria.
Meta-analyses
Table 3 shows the main results of the pairwise meta-analyses for the response rates. Combined treatment was more effective than both psychotherapy alone (RR=1.25, 95% CI: 1.09-1.43) and pharmacotherapy alone (RR=1.27, 95% CI: 1.12-1.43). The difference between psychotherapy alone and pharmacotherapy alone was not significant (RR=0.98, 95% CI: 0.91-1.06). Heterogeneity was low to moderate in most comparisons. In the comparisons with more than 10 studies, only heterogeneity of combined treatment versus pharmacotherapy was higher than 50%. Egger's test was only significant for combined treatment versus pharmacotherapy (p=0.02) and for combined treatment versus psychotherapy plus placebo (p=0.02).
| N | Pairwise meta-analyses | Network meta-analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | I2 | 95% CI | Egger | RR | 95% CI | ||
| Response | ||||||||
| Combined vs. psychotherapy | 19 | 1.25 | 1.09-1.43 | 44 | 0-66 | 0.36 | 1.27 | 1.14-1.39 |
| Combined vs. pharmacotherapy | 46 | 1.27 | 1.12-1.43 | 58 | 39-69 | 0.02 | 1.25 | 1.14-1.37 |
| Combined vs. psychotherapy + placebo | 10 | 1.19 | 0.95-1.52 | 39 | 0-69 | 0.02 | 1.30 | 1.06-1.59 |
| Combined vs. placebo | 4 | 1.15 | 0.73-1.79 | 60 | 0-84 | 0.39 | 1.47 | 1.20-1.75 |
| Psychotherapy vs. pharmacotherapy | 59 | 0.98 | 0.91-1.06 | 41 | 16-57 | 0.38 | 0.99 | 0.92-1.08 |
| Psychotherapy vs. psychotherapy + placebo | 2 | 0.88 | 0.60-1.30 | 16 | NA | NA | 1.03 | 0.84-1.27 |
| Psychotherapy vs. placebo | 8 | 1.20 | 0.93-1.59 | 46 | 0-74 | 0.67 | 1.16 | 0.98-1.39 |
| Pharmacotherapy vs. psychotherapy + placebo | 6 | 1.05 | 0.76-1.45 | 53 | 0-79 | 0.45 | 1.04 | 0.85-1.27 |
| Pharmacotherapy vs. placebo | 12 | 1.25 | 1.09-1.45 | 0 | 0-50 | 0.68 | 1.18 | 0.99-1.39 |
| Psychotherapy + placebo vs. placebo | 4 | 1.00 | 0.76-1.30 | 0 | 0-68 | 0.29 | 0.88 | 0.69-1.12 |
| Remission | ||||||||
| Combined vs. psychotherapy | 15 | 1.20 | 1.02-1.41 | 25 | 0-59 | 0.76 | 1.22 | 1.08-1.39 |
| Combined vs. pharmacotherapy | 25 | 1.28 | 1.10-1.52 | 57 | 27-72 | 0.22 | 1.23 | 1.09-1.39 |
| Combined vs. psychotherapy + placebo | 6 | 1.18 | 0.71-1.92 | 67 | 0-84 | 0.79 | 1.09 | 0.82-1.45 |
| Combined vs. placebo | 2 | 1.52 | 1.02-2.22 | 0 | NA | NA | 1.59 | 1.27-2.00 |
| Psychotherapy vs. pharmacotherapy | 47 | 1.01 | 0.93-1.10 | 29 | 0-50 | 0.90 | 1.01 | 0.93-1.10 |
| Psychotherapy vs. psychotherapy + placebo | 1 | 0.66 | 0.40-1.05 | NA | NA | NA | 0.89 | 0.67-1.19 |
| Psychotherapy vs. placebo | 7 | 1.37 | 1.05-1.79 | 41 | 0-74 | 0.03 | 1.30 | 1.05-1.59 |
| Pharmacotherapy vs. psychotherapy + placebo | 4 | 0.81 | 0.32-2.04 | 84 | 47-92 | 0.42 | 0.89 | 0.67-1.19 |
| Pharmacotherapy vs. placebo | 9 | 1.33 | 1.10-1.64 | 22 | 0-64 | 0.04 | 1.28 | 1.05-1.59 |
| Psychotherapy + placebo vs. placebo | 2 | 1.25 | 0.76-2.04 | 0 | NA | NA | 0.69 | 0.49-0.96 |
| Acceptability | ||||||||
| Combined vs. psychotherapy | 18 | 1.08 | 0.92-1.28 | 0 | 0-44 | 0.99 | 1.06 | 0.89-1.26 |
| Combined vs. pharmacotherapy | 41 | 1.29 | 1.13-1.47 | 0 | 0-33 | 0.74 | 1.23 | 1.05-1.45 |
| Combined vs. psychotherapy + placebo | 9 | 0.96 | 0.59-1.58 | 18 | 0-62 | 0.50 | 0.98 | 0.66-1.46 |
| Combined vs. placebo | 4 | 1.35 | 0.56-3.27 | 24 | 0-75 | 0.12 | 1.25 | 0.94-1.66 |
| Psychotherapy vs. pharmacotherapy | 58 | 1.16 | 1.02-1.31 | 28 | 0-48 | 0.04 | 1.17 | 1.02-1.32 |
| Psychotherapy vs. psychotherapy + placebo | 2 | 0.54 | 0.13-2.36 | 36 | NA | NA | 0.93 | 0.62-1.38 |
| Psychotherapy vs. placebo | 8 | 1.34 | 0.86-2.09 | 62 | 0-81 | 0.15 | 1.18 | 0.91-1.53 |
| Pharmacotherapy vs. psychotherapy + placebo | 7 | 0.72 | 0.43-1.21 | 27 | 0-69 | 0.67 | 0.77 | 0.50-1.19 |
| Pharmacotherapy vs. placebo | 12 | 0.98 | 0.72-1.33 | 40 | 0-68 | 0.38 | 1.02 | 0.79-1.30 |
| Psychotherapy + placebo vs. placebo | 4 | 1.06 | 0.57-1.95 | 0 | 0-68 | 0.31 | 0.79 | 0.51-1.21 |
| Standardized mean difference (SMD) | N | SMD | 95% CI | I 2 | 95% CI | Egger | SMD | 95% CI |
| Combined vs. psychotherapy | 19 | 0.15 | –0.05 to 0.35 | 69 | 45-79 | 0.05 | 0.30 | 0.14-0.45 |
| Combined vs. pharmacotherapy | 41 | 0.37 | 0.23-0.53 | 68 | 54-76 | 0.03 | 0.33 | 0.20-0.47 |
| Combined vs. psychotherapy + placebo | 7 | 0.07 | –0.20 to 0.34 | 12 | 0-63 | 0.61 | 0.16 | –0.18 to 0.49 |
| Combined vs. placebo | 2 | 0.08 | –0.40 to 0.55 | 0 | NA | NA | 0.43 | 0.10-0.76 |
| Psychotherapy vs. pharmacotherapy | 50 | 0.00 | –0.13 to 0.12 | 68 | 55-75 | 0.03 | 0.04 | –0.09 to 0.16 |
| Psychotherapy vs. psychotherapy + placebo | 2 | –0.19 | –0.57 to 0.18 | 0 | NA | NA | –0.14 | –0.49 to 0.21 |
| Psychotherapy vs. placebo | 4 | 0.19 | –0.37 to 0.75 | 82 | 34-91 | 0.89 | 0.13 | –0.19 to 0.45 |
| Pharmacotherapy vs. psychotherapy + placebo | 4 | –0.24 | –0.58 to 0.10 | 16 | 0-73 | 0.76 | –0.18 | –0.52 to 0.16 |
| Pharmacotherapy vs. placebo | 6 | 0.19 | –0.13 to 0.50 | 48 | 0-77 | 0.84 | 0.10 | –0.22 to 0.41 |
| Psychotherapy + placebo vs. placebo | 2 | –0.11 | –0.59 to 0.38 | 0 | NA | NA | –0.27 | –0.71 to 0.16 |
- RR – relative risk, NA – not available
- Significant results are highlighted in bold prints
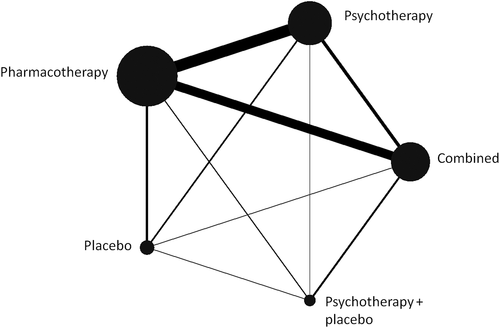
The network for response rates is graphically represented in Figure 2. The main results of the network meta-analysis are presented in Table 3. Combined treatment was superior to either psychotherapy alone or pharmacotherapy alone in terms of response (RR=1.27, 95% CI: 1.14-1.39, and RR=1.25, 95% CI: 1.14-1.37, respectively), remission (RR=1.22, 95% CI: 1.08-1.39 and RR=1.23, 95% CI: 1.09-1.39), and SMD (0.30, 95% CI: 0.14-0.45 and 0.33, 95% CI: 0.20-0.47). No significant difference was found between psychotherapy alone and pharmacotherapy alone concerning response (RR=0.99, 95% CI: 0.92-1.08), remission (RR=1.01, 0.93-1.10), and SMD (SMD=0.04, 95% CI: –0.09 to 0.16). Acceptability was significantly better for combined treatment compared with pharmacotherapy (RR=1.23, 95% CI: 1.05-1.45), as well as for psychotherapy compared with pharmacotherapy (RR=1.17, 95% CI: 1.02-1.32).
In the relatively few relevant studies included in the network meta-analysis, response rate was significantly higher for combined treatment compared to psychotherapy plus pill placebo (RR=1.30, 95% CI: 1.06-1.59) and for combined treatment compared to pill placebo (RR=1.47, 95% CI: 1.20-1.75). Remission rate was significantly higher for combined treatment compared to pill placebo (RR=1.59, 95% CI: 1.27-2.00). Combined treatment also resulted in a significantly higher SMD than pill placebo (0.43, 95% CI: 0.10-0.76).
The consistency of the network was examined using the loop-specific approach. No inconsistency factors were found to be significant, although this cannot be considered as evidence for the absence of inconsistency, because of low power in some of the loops, especially in the presence of large heterogeneity in pairwise comparisons. The design-by-treatment interaction model did not indicate global inconsistency in the network (X2=10.51, df=10, p for the null hypothesis of consistency in the network: 0.40).
In the SUCRA analyses, combined treatment ranked clearly best for response (99.9), remission (93.0) and SMD (95.6), as well as for acceptability (78.7). Psychotherapy ranked better than pharmacotherapy for remission (45.0 vs. 40.8), SMD (43.5 vs. 29.1) and acceptability (63.2 vs. 17.4), whereas pharmacotherapy ranked better than psychotherapy for response (54.2 vs. 49.6).
Further analyses
The results of the sensitivity analyses are reported in Table 4. The main outcomes were comparable across all analyses, with combined treatment being superior to psychotherapy or pharmacotherapy alone, and no significant difference between psychotherapy and pharmacotherapy.
| Pairwise meta-analyses | Network meta-analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | RR | 95% CI | I2 | 95% CI | Egger | RR | 95% CI | χ2 (df), p | |
| Optimized pharmacotherapy | |||||||||
| Combined vs. psychotherapy | 15 | 1.27 | 1.08-1.49 | 53 | 0-73 | 0.38 | 1.20 | 1.08-1.35 | 1.20 (3), 0.75 |
| Combined vs. pharmacotherapy | 25 | 1.16 | 1.02-1.33 | 52 | 15-68 | 0.91 | 1.19 | 1.06-1.33 | |
| Psychotherapy vs. pharmacotherapy | 45 | 0.99 | 0.91-1.08 | 44 | 14-60 | 0.75 | 0.99 | 0.91-1.08 | |
| Optimized psychotherapy | |||||||||
| Combined vs. psychotherapy | 9 | 1.33 | 1.18-1.52 | 14 | 0-60 | 0.42 | 1.25 | 1.08-1.47 | 0.47 (3), 0.93 |
| Combined vs. pharmacotherapy | 19 | 1.27 | 1.06-1.49 | 72 | 53-81 | 0.33 | 1.27 | 1.10-1.45 | |
| Psychotherapy vs. pharmacotherapy | 30 | 1.00 | 0.90-1.11 | 49 | 15-66 | 0.44 | 1.00 | 0.89-1.12 | |
| Low risk of bias (self-report rated as low risk) | |||||||||
| Combined vs. psychotherapy | 6 | 1.33 | 0.98-1.79 | 49 | 0-78 | 0.24 | 1.45 | 1.16-1.82 | 1.06 (3), 0.79 |
| Combined vs. pharmacotherapy | 17 | 1.32 | 1.02-1.67 | 70 | 45-80 | 0.88 | 1.27 | 1.05-1.54 | |
| Psychotherapy vs. pharmacotherapy | 16 | 0.87 | 0.76-0.99 | 41 | 0-66 | 0.08 | 0.87 | 0.74-1.03 | |
| Low risk of bias (self-report rated as high risk) | |||||||||
| Combined vs. psychotherapy | 5 | 1.52 | 1.32-1.75 | 0 | 0-64 | 0.59 | 1.43 | 1.15-1.79 | 0.02 (3), 1.00 |
| Combined vs. pharmacotherapy | 13 | 1.27 | 0.96-1.67 | 70 | 39-81 | 0.87 | 1.23 | 1.02-1.49 | |
| Psychotherapy vs. pharmacotherapy | 14 | 0.88 | 0.79-1.00 | 30 | 0-62 | 0.04 | 0.86 | 0.74-1.01 | |
| Placebo controlled excluded | |||||||||
| Combined vs. psychotherapy | 16 | 1.28 | 1.10-1.49 | 50 | 0-70 | 0.56 | 1.32 | 1.18-1.47 | 0.66 (3), 0.88 |
| Combined vs. pharmacotherapy | 39 | 1.30 | 1.15-1.47 | 58 | 37-70 | 0.02 | 1.27 | 1.15-1.41 | |
| Psychotherapy vs. pharmacotherapy | 48 | 0.94 | 0.87-1.03 | 40 | 10-57 | 0.68 | 0.96 | 0.88-1.05 | |
| One effect size per study | |||||||||
| Combined vs. psychotherapy | 19 | 1.25 | 1.09-1.43 | 46 | 0-67 | 0.40 | 1.25 | 1.12-1.39 | 0.27 (3), 0.97 |
| Combined vs. pharmacotherapy | 43 | 1.27 | 1.12-1.43 | 61 | 43-71 | 0.02 | 1.25 | 1.14-1.37 | |
| Psychotherapy vs. pharmacotherapy | 50 | 0.99 | 0.90-1.08 | 50 | 26-63 | 0.45 | 1.00 | 0.92-1.09 | |
- RR – relative risk
- Significant results are highlighted in bold prints
We conducted separate pairwise and network meta-analyses limited to studies on chronic or treatment-resistant depression (only for response), whose results are presented in Table 5. Although the number of studies was relatively small, the findings were comparable to the main analyses, with superior effects for combined treatment versus psychotherapy or pharmacotherapy alone (RR=1.59, 95% CI: 1.23-2.04 and RR=1.39, 95% CI: 1.15-1.67), and comparable effects for psychotherapy and pharmacotherapy (RR=0.87, 95% CI: 0.68-1.10).
| Pairwise meta-analyses | Network meta-analyses | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | RR | 95% CI | I2 | 95% CI | Egger | RR | 95% CI | χ2 (df), p | |
| Chronic or treatment-resistant depression | |||||||||
| Combined vs. psychotherapy | 3 | 1.45 | 1.16-1.79 | 55 | 0-86 | 1.00 | 1.59 | 1.23-2.04 | 2.47 (2), 0.29 |
| Combined vs. pharmacotherapy | 10 | 1.41 | 1.12-1.75 | 73 | 41-84 | 0.37 | 1.39 | 1.15-1.67 | |
| Psychotherapy vs. pharmacotherapy | 6 | 0.84 | 0.70-1.00 | 25 | 0-70 | 0.37 | 0.87 | 0.68-1.10 | |
| Severe depression | |||||||||
| Combined vs. psychotherapy | 2 | 1.35 | 0.85-2.17 | 65 | NA | NA | 1.33 | 0.91-1.92 | 0.66 (3), 0.88 |
| Combined vs. pharmacotherapy | 6 | 1.45 | 1.14-1.82 | 35 | 0-73 | 0.80 | 1.45 | 1.10-1.89 | |
| Psychotherapy vs. pharmacotherapy | 4 | 1.18 | 0.70-1.96 | 54 | 0-83 | 0.33 | 1.09 | 0.72-1.64 | |
| Moderate depression | |||||||||
| Combined vs. psychotherapy | 11 | 1.14 | 0.99-1.30 | 0 | 0-51 | 0.30 | 1.19 | 1.05-1.37 | 0.48(30), 0.92 |
| Combined vs. pharmacotherapy | 18 | 1.28 | 1.10-1.47 | 34 | 0-62 | 0.03 | 1.23 | 1.09-1.41 | |
| Psychotherapy vs. pharmacotherapy | 32 | 1.02 | 0.93-1.12 | 23 | 0-50 | 0.35 | 1.03 | 0.94-1.14 | |
| Mild depression | |||||||||
| Combined vs. psychotherapy | 1 | 1.39 | 0.65-2.94 | 0 | NA | NA | 0.97 | 0.52-1.82 | 0.89(1), 0.35 |
| Combined vs. pharmacotherapy | 1 | 0.85 | 0.56-1.30 | 0 | NA | NA | 1.04 | 0.57-1.89 | |
| Psychotherapy vs. pharmacotherapy | 5 | 1.14 | 0.77-1.69 | 52 | 0-81 | 0.79 | 1.08 | 0.75-1.54 | |
- RR – relative risk, NA – not available
- Significant results are highlighted in bold prints
In the meta-regression analysis including the studies that reported the baseline severity of depression on the HAM-D, this severity was not associated with response rate in the combined treatment versus psychotherapy comparison (coefficient=–0.2, SE=0.02, p=0.29) or in the combined versus pharmacotherapy comparison (coefficient=–0.02, SE=0.2, p=0.13).
We also conducted separate network meta-analyses for mild, moderate and severe depression (Table 5). In severe depression, combined treatment was more effective than pharmacotherapy alone (RR=1.45, 95% CI: 1.10-1.89), while there were only two comparisons of combined treatment with psychotherapy alone. In moderate depression, combined treatment was more effective than either psychotherapy or pharmacotherapy alone (RR=1.19, 95% CI: 1.05-1.37, and RR=1.23, 95% CI: 1.09-1.41), and there was no significant difference between psychotherapy and pharmacotherapy (RR=1.03, 95% CI: 0.94-1.14). Unfortunately, there were too few studies in patients with mild depression.
In the multivariate meta-regression analysis conducted to examine possible sources of heterogeneity, with response as outcome and with the three main nodes (combined treatment, psychotherapy and pharmacotherapy), only one predictor was found to be significant (“other” pharmacotherapy versus SSRI: coefficient=–0.55, SE=0.22, p=0.01).
Long-term effects
We calculated response rates for studies reporting follow-up outcomes at 6 to 12 months. The pairwise meta-analyses indicated that combined treatment was more effective than pharmacotherapy at 6 to 12 months follow-up (RR=0.71, 95% CI: 0.60-0.84). The other two comparisons did not indicate a significant difference. The network meta-analysis, however, indicated that combined treatment was not only more effective than pharmacotherapy (RR=0.72, 95% CI: 0.62-0.83) but also than psychotherapy (RR=0.84, 95% CI: 0.71-0.99), and that psychotherapy was more effective than pharmacotherapy (RR=0.85, 95% CI: 0.74-0.98).
The design-by-treatment interaction model did not indicate global inconsistency in the network (X2=0.12, df=3, p for the null hypothesis of consistency in the network: 0.99). Because the time to follow-up varied between 6 and 12 months, we conducted a meta-regression analysis to examine whether time to follow-up was associated with the outcome, but this association was not found (all p values >0.32).
DISCUSSION
In this network meta-analysis, we assessed comparative data from 101 randomized trials and found that combination treatment was more effective than psychotherapy or pharmacotherapy alone in the treatment of adult depression, and that there were no significant differences between psychotherapy and pharmacotherapy.
We also found that acceptability, defined on the basis of study drop-out for any reason, was higher in combined treatment than in pharmacotherapy alone, and in psychotherapy than in pharmacotherapy. Acceptability of antidepressants may be lower due to side effects or because many patients prefer psychotherapy over pharmacotherapy134. Combined treatment may therefore be the best option for the treatment of depression both in terms of efficacy and acceptability and, from the perspective of acceptability, pharmacotherapy alone may be not optimal.
The majority of studies were aimed at patient populations with moderate depression. However, this must be considered with caution. We used the average depression scores per study, meaning that within each study the severity of depression could still range from mild to severe. In the relatively few studies on severe depression, we also found that combined treatment was more effective than pharmacotherapy. Unfortunately, only two studies examined combined treatment versus psychotherapy alone among patients with severe depression, so we cannot be certain whether combined treatment is superior for these people. Individual patient data meta-analyses have suggested that baseline depression severity does not moderate the efficacy of CBT versus antidepressant treatment135, or CBT over pill placebo136. This supports the notion that combined treatment should be the first option for moderate and probably also severe depression. Unfortunately, there were too few studies in patients with mild depressive disorders to say anything about the relative effects of combined treatment, psychotherapy and pharmacotherapy.
There is evidence suggesting that a significant proportion of patients with depression receive psychotropic medication without psychotherapy137, 138. The results of our meta-analysis suggests that this is probably not the optimal option in terms of quality of care. Although the effects of psychotherapy and pharmacotherapy are comparable and individual patients may have different clinical situations and specific preferences, psychotherapy is on average more acceptable than pharmacotherapy alone. Findings from this paper clearly show that combined treatment is the best option in moderate depression, and in routine clinical care it would be better to consider psychotherapy as the first choice when only one treatment is offered to a patient. The National Health Service in the UK and other health care systems in the world, including low and middle income countries139, should model themselves accordingly and invest more resources in non-pharmacological interventions for depression.
In real-world settings, pharmacotherapy and psychotherapy are typically provided by different clinicians and sometimes even at different clinics, with antidepressant medication often being prescribed in primary care and psychotherapy delivered in secondary care or settings outside of the hospital. Moreover, funding of services varies across countries, with different structures for medication and psychotherapy. This may complicate the use of combined treatments. From this perspective, collaborative care offers good opportunities for the dissemination of combined treatments140.
In the majority of trials included in this meta-analysis, psychotherapy was delivered in an individual format. Only a limited number of trials examined group psychotherapies, and none of the trials used guided self-help or Internet-based psychotherapies. It is known from other research that psychotherapies can effectively be delivered in several different formats, including in groups, by telephone, through guided self-help, and via the Internet141, 142. There are no indications that treatment format is associated with different effects of psychotherapy, as long as at least some personal support is given by a professional. It would be useful to further explore such different therapy formats in combined treatment, because these formats require less resources and are often easier to implement than intensive individual therapies. This could potentially facilitate the use of combined treatments in routine care.
We also found that combined treatment was superior to psychotherapy and pharmacotherapy alone in chronic or treatment-resistant depression. That should be considered with caution, because we pooled all studies of chronic and treatment-resistant depression into one group, and may have missed specific outcomes for the two conditions. However, this finding is important from a clinical perspective and suggests that combined treatment should be preferred also in this problematic group.
It should be noted that there was some variability among the included studies in terms of the quality of pharmacotherapy administered, the quality of psychotherapy delivered and/or the quality of the study design and conduct. However, all sensitivity analyses limiting to trials of optimized pharmacotherapy, optimized psychotherapy or at low risk of bias produced very similar results. We therefore believe that our conclusions about the relative values of the three treatments are robust.
Unfortunately, the long-term effects of the treatments are still unknown. We calculated response rates for studies reporting follow-up outcomes at 6 months or longer. The only three studies reporting outcome data at more than 12 months were excluded from the analyses. The remaining studies were still heterogeneous in terms of continuation of treatment: in most studies no psychotherapy was given during follow-up, whereas pharmacotherapy was continued during the whole follow-up period in some studies, and tapered at some point during follow-up in some others. Other studies were completely naturalistic. We did find indications that, at 6 to 12 months after treatment start, combined treatment is more effective than psychotherapy or pharmacotherapy alone, and that psychotherapy is more effective than pharmacotherapy. However, these findings should be regarded as preliminary, because the studies varied widely in terms of what happened during follow-up. The finding that psychotherapy may be more effective than pharmacotherapy in the longer term is in line with previous meta-analytic research143, and it has also been established previously that combined treatment may be more effective than pharmacotherapy alone14. The results of the analyses should, however, be considered with caution. Further research is clearly very much needed on the long-term effects of treatments for depression.
Very few studies have compared the effects of combined treatment with placebo. That is unfortunate, because a comparison with placebo would allow to better estimate the actual effects of combined treatment. Previous meta-analytic research suggested that the effects of combined treatment in depression and anxiety are the sum of the effects of psychotherapy and those of pharmacotherapy11. These findings were very preliminary, because of the broad CIs around the effect sizes found. However, they do suggest that the effects of psychotherapy and pharmacotherapy may be independent of each other, and can be applied separately. Unfortunately, the present meta-analysis did not find enough studies to confirm or falsify this finding.
We also found only a limited number of studies comparing the combination of psychotherapy and pharmacotherapy with the combination of psychotherapy and placebo. This comparison allows to examine the contribution of medication to the effects of combined treatment. A previous pairwise meta-analysis suggested that the medication contributed to the effects of combined treatment with a small effect size144. On the other hand, a comparison of psychotherapy plus placebo with psychotherapy alone would allow to estimate the impact of psychotherapy in addition to placebo effects.
This study has several strengths, but also some limitations. The number of trials was too small in specific subsamples, for example in severe or mild depression. Moreover, the majority of trials had at least one domain at high risk of bias. Finally, previous research has indicated that there may be some differences in efficacy and acceptability among specific types of medications6. In our network meta-analysis, we merged all antidepressants in one node, as we did not have enough studies across different medications to examine that in sufficient detail.
In conclusion, combined treatment is more effective than psychotherapy or pharmacotherapy alone in the short-term treatment of moderate depression, and there are no significant differences between psychotherapy and pharmacotherapy. This is also true in chronic and treatment-resistant depression, and probably also in severe depression. Acceptability is significantly better in combined treatment and psychotherapy, compared with pharmacotherapy. These findings suggest that guidelines should recommend combined treatment as the first option in the treatment of depression and, because of the higher acceptability, may recommend psychotherapy before pharmacotherapy, depending on the preferences of patients.
ACKNOWLEDGEMENTS
This study was partially funded by the National Institute for Health Research (NIHR) Oxford Health Biomedical Research Centre, grant BRC-1215-20005 (to A. Cipriani). A. Cipriani is also supported by the NIHR Oxford Cognitive Health Clinical Research Facility and by an NIHR Research Professorship (grant RP-2017-08-ST2-006). The views expressed in the paper are those of the authors and not necessarily those of the UK National Health Service, the NIHR, or the UK Department of Health.




