Balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension concomitant with Klippel–Trenaunay–Weber syndrome
Abstract
Klippel–Trenaunay–Weber syndrome (KTWS) is a rare congenital disorder characterized by cutaneous capillary malformations, bone hypertrophy, and multiple venous or lymphatic malformations. KTWS is associated with chronic thromboembolic pulmonary hypertension (CTEPH), presumably due to thromboembolism from multiple vascular malformations. Here, we report the first case series of patients with KTWS-CTEPH who underwent balloon pulmonary angioplasty (BPA). Both patients are alive 20 years and 1 year after the initial diagnosis of CTEPH, respectively, and are stable with improved hemodynamics. BPA may be an effective treatment option for patients with KTWS-CTEPH.
INTRODUCTION
Klippel–Trenaunay–Weber syndrome (KTWS) is a rare congenital disorder characterized by bone hypertrophy and multiple capillary malformations.1, 2 Major complications of this syndrome include hemorrhage, recurrent infections, and thromboembolic events.1, 3 The probability of thromboembolic events in KTWS is reported to be up to 39%1, 2, 4, 5 and is presumably due to hypercoagulability at vascular malformations with blood stagnation and activated coagulation. Recurrent venous thromboembolism in a patient with KTWS has been reported despite adequate anticoagulation,6 potentially contributing to CTEPH.7
Pulmonary endarterectomy (PEA) is the treatment of choice for patients with operable CTEPH. CTEPH concomitant with KTWS (KTWS-CTEPH) has been effectively treated with PEA,8 whereas cases ineligible for PEA had poor outcomes.8
Balloon pulmonary angioplasty (BPA) has emerged as a treatment option for patients with CTEPH who are ineligible for PEA.9 Although there have been no previous reports of BPA for KTWS-CTEPH, the recent advance of BPA with improved safety and effectiveness10 seems to be promising for treating KTWS-CTEPH. Herein we report two cases of KTWS-CTEPH treated with BPA.
CASE DESCRIPTION
Case 1
A 62-year-old man with KTWS diagnosed at the age of 43 years was referred for the treatment of CTEPH. Bilateral limb varix was pointed out at his birth. He has been treated with anticoagulants for 10 years after the initial episode of pulmonary thromboembolism. Two years before referral, he suffered from severe dyspnea and was diagnosed with CTEPH even under anticoagulation. An inferior vena cava filter was implanted. At that time, riociguat was not yet available in our country, so bosentan 250 mg/day and tadalafil 40 mg/day were administered instead. His exertional dyspnea did not ameliorate, then he was referred to our hospital.
He was classified as World Health Organization functional class (WHO FC) III and required 4 L/min of oxygen administration. Right heart catheterization demonstrated a high mean pulmonary artery pressure (mPAP) of 44 mmHg and pulmonary vascular resistance (PVR) of 7.3 Wood units (WU). Pulmonary angiography revealed both proximal and distal thrombotic lesions of bilateral pulmonary arteries (Figure 1).
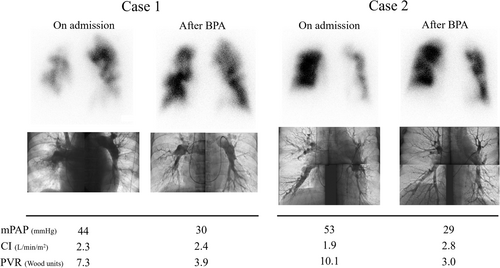
The patient was diagnosed as operable, but he was concerned about the potential risk of PEA for the recurrence of CTEPH with this syndrome; thus, he rejected it. Therefore, we performed BPA considering the advantage of its repeatability. Because of the existence of the inferior vena cava filter, we performed BPA by the right jugular vein approach. After a total of 21 sessions of BPA, both bosentan and tadalafil were discontinued. The mPAP and PVR improved and were stabilized around 30 mmHg and 3.9 WU, respectively. His symptoms improved from WHO FC III–II. The patient is alive 20 years after the diagnosis of CTEPH (and 10 years after the initial BPA) with a minimum oxygen requirement of 1 L/min.
Case 2
A 48-year-old man was referred for evaluation of progressive exertional dyspnea which had progressed over 8 years. Asymmetrical leg size was observed at birth. At the age of 17 years, left lower limb amputation and rectal resection were performed because of severe local infection of varix and uncontrollable bloody bowel discharge. Thus, the patient was diagnosed of having KTWS. He suffered from pulmonary thromboembolism, and anticoagulant therapy was administered at the age of 40 years. Eight years later, he visited the emergency room with recurrent exertional dyspnea. Severe pulmonary hypertension was pointed out and he was referred to our hospital for further examination.
He was classified as WHO FC IV and required 4 L/min of oxygen administration. Right heart catheterization revealed a high mPAP of 53 mmHg and PVR of 10.1 WU. Pulmonary angiography revealed proximal and multiple distal thrombotic lesions (Figure 1).
The patient was diagnosed as operable; however, he rejected it because of comorbidities such as obesity, fatty liver disease, and lung fibrosis and underwent BPA. After 12 BPA sessions, the mPAP and PVR improved to 29 mmHg and 3.0 WU without any selective pulmonary vasodilators, and his symptoms improved from WHO FC IV–II. The patient is alive 1 year after the diagnosis of CTEPH (and 1 year after the initial BPA) with decreased oxygen requirement at 2 L/min.
DISCUSSION
We reported BPA in patients with KTWS-CTEPH with proximal lesions. PEA provides a highly satisfactory improvement in the hemodynamic and functional status for the proximal type of CTEPH. It has also been reported to be effective for proximal-type KTWS-CTEPH.8 In addition, there had been no previous reports of BPA for KTWS-CTEPH. Therefore, our CTEPH team initially recommended PEA as the first choice. However, both patients eventually chose to undergo BPA according to their own situations. After several BPA sessions, both patients achieved improved hemodynamics with mPAP < 30 mmHg without any major complications.
BPA brought acceptable results in these two cases. In addition, BPA has the advantage of its repeatability, unlike PEA, since KTWS is also characterized as its tendency of recurrent thromboembolism.6 Patients suffering from this syndrome could potentially require several revascularization procedures to maintain improved hemodynamics, even after a successful intervention. It would not be challenging to perform additional BPA sessions in case of recurrence. Indeed, in Case 1, we had to carry out total of 21 BPA sessions because of latent total occlusion lesions distal to the proximal total occlusion lesion, hemodynamic deterioration during follow-up, or remaining distal lesions as shown in Figure 1. All these might be due to the tendency of recurrent thromboembolism, the characteristics of KTWS-CTEPH.
To the best of our knowledge, this is the first report of patients with KTWS-CTEPH who underwent BPA. BPA might be promising for patients with KTWS-CTEPH who are ineligible for PEA.
AUTHOR CONTRIBUTIONS
All authors reviewed, revised the manuscript, approved the final version to be published, and agreed to be accountable for all aspects of the work.
ACKNOWLEDGMENT
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
Documented informed consent for publication has been obtained from each patient.