Dynamic multidisciplinary team discussions can improve the prognosis of metastatic castration-resistant prostate cancer patients
Abstract
Background
Multidisciplinary team (MDT) management is a popular treatment paradigm in managing cancer patients, which provides fully-discussed, interdisciplinary treatment recommendations for patients. However, there has been a lack of data on its actual impact on the overall survival (OS) of metastatic castration-resistant prostate cancer (mCRPC) patients. mCRPC is the end stage of prostate cancer, facing a treatment dilemma of overwhelming options; therefore, we hypothesize dynamic MDT discussions can be helpful in comprehensively managing these patients.
Methods
We retrospectively collected 422 mCRPC patients' clinical information from 2013 to 2020 from our institute. Patients can voluntarily choose whether to enroll in the dynamic MDT group, which includes discussions at CRPC diagnosis and subsequent disease progression. All patients were followed up regularly, and OS from CRPC diagnosis to death was set as the endpoint of this study.
Results
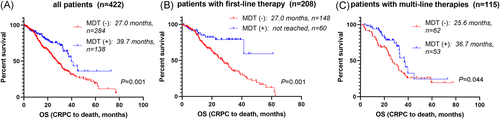
Participating in MDT discussions is a favorable independent indicator of longer overall survival (median OS: MDT (+): 39.7 months; MDT (−): 27.0 months, hazard ratio: 0.549, p = .001). Moreover, this survival benefit of MDT remained in subgroups with first-line therapy [median OS: MDT (+): not reached; MDT (−): 27.0 months, p = .001) and with multi-line therapy until the end of follow-up (median OS: MDT (+): 36.7 months; MDT (−): 25.6 months, p = .044).
Conclusion
Therefore, regular MDT discussions are valuable in the management of mCRPC patients. Clinicians are encouraged to tailor MDT discussions dynamically to provide mCRPC patients with a better and more individualized treatment plan and more prolonged survival.
Take-home messages
- ●
The MDT model is defined as dynamic MDT discussions at the time of mCRPC diagnosis and each time they progressed later on throughout the disease management.
- ●
Prostate cancer MDT usually includes specialists in urologic oncology, pathology, chemotherapy, radiotherapy, ultrasound, imaging and nuclear medicine.
- ●
MDT model can benefit mCRPC patients in terms of overall survival.
1 INTRODUCTION
Prostate cancer is the leading cancer type for the estimated new cancer cases in elderly men.1 While prostate cancer harboring the highest incidence rate, it represents a rather long disease spectrum, which requires clinicians to make comprehensive and personalized treatment algorithms throughout the disease to improve the prognosis and the quality of life for patients. In the course of prostate cancer development, metastatic castration-resistant prostate cancer (mCRPC) is the final stage with the highest disease burden and an abundance of therapies available at the same time. China has yet to enter the prostate-specific antigen (PSA) screening era, and a considerable proportion of Chinese prostate cancer patients are diagnosed at a relatively late stage. As a result, the management of mCRPC patients is of great clinical value. Thus, how to make an optimized treatment plan is essential to the patients and their families.
A multidisciplinary team (MDT) is a group of health professionals who meet regularly to discuss and contribute independently to the diagnostic and treatment decisions about providing personalized therapeutic plans for patients. This disease management model has been increasingly popular for cancer patients and has already been applied in various cancer types at many medical centers around the world.2 MDT counsel is well suited for selecting the most suitable therapy in terms of disease control as well as the financial burden. Consequently, MDT now comes into being in genitourinary cancers and is endorsed by the current guidelines for managing mCRPC patients.3
Studies have shown numerous advantages of multidisciplinary care over the traditional urologist-to-patient treatment model in prostate cancer. Overall, this shared decision-making process is proven to improve patient satisfaction, change patients' management plans and lead to greater adherence to treatment guidelines.4-7 Specifically, in prostate cancer patients, MDT brings timely oncological treatment with a reduced effort,4 such as increased treatment plan alteration, cross-referral rate, and clinical trial inclusion rate.5 Patients receiving radical prostatectomy can have a better prognosis if they participate in MDT discussions and adhere to the adjuvant radiotherapy recommendations accordingly.8 Besides, a well-structured MDT team goes beyond merely MDT discussions by providing health education and specially-assigned follow-up for patients and thesis learning for healthcare providers, focusing on the latest study trend.
As a result, Chinese Society of Clinical Oncology guidelines put a great emphasis on the use of MDT in their latest guidelines: MDT model should be the cornerstone of mCRPC treatment, and they also define the necessary components, discussion items, and daily routine of the team construction.9 Internationally speaking, counseling, managing, and treating mCRPC patients in an MDT manner has strong evidence according to EAU guidelines,10 though it is not mentioned in NCCN guidelines.
Currently, there is a lack of data on the impact of MDT on mCRPC patients, especially the actual survival influence. Here we present clinical and follow-up data of mCRPC patients at our institute to investigate whether MDT discussions influence their survival outcomes.
2 MATERIALS AND METHODS
2.1 Study design and patient population
The study population initially comprised 433 retrospectively obtained mCRPC patients diagnosed at West China Hospital (Sichuan University) from 2013 to 2020. We retrospectively collected their basic demographics, imaging information, pathological reports, electronic medical records, and laboratory results at the time of CRPC diagnosis.
Dynamic MDT schemes include MDT discussions at the time of CRPC diagnosis and each time they progressed. Patients who were entering the mCRPC stage were free to choose whether they participated in this dynamic MDT scheme or not. Prostate cancer MDT roundtable discussions in our institute were held weekly and includes doctors with complementary skills, qualifications, and experience. An interdisciplinary opinion is typically composed of recommendations from doctors in urologic oncology, pathology, chemotherapy, radiotherapy, ultrasound, imaging and nuclear medicine, sometimes including professionals in nursing, nephrology, anesthesiology, general surgery, and endocrinology.
2.2 Follow-up
Patients were required to visit our department once every month if their condition remained stable and once every two weeks if they showed signs of progressive disease. If the patients could not visit the outpatient department for various reasons, our follow-up team would instead conduct telephone visits. Eleven patients lost to follow-up during the process; therefore, a total of 422 patients were included in the analyses. Each routine follow-up visit contained history-taking, physical examination, and laboratory tests, including PSA, blood routine examination, renal and liver function. Single-photon emission computed tomography, chest and abdomen CT, positron emission tomography-computed tomography was performed when necessary. All patients were follow-up until death or the last study visits. The study endpoint was overall survival (OS) from CRPC diagnosis to death.
2.3 Statistics
Chi-squared test was used to compare the baseline characteristics between patients with and without MDT. Kaplan–Meier curve and log-rank test were applied in comparing the OS of patients in two groups. Cox regression was applied in the univariate and multivariate analyses of OS. In the Cox regression, factors with p < .05 in univariate analyses were included in the multivariate analyses. Data analyses in this study were performed using SPSS (version 25.0; IBM Corp.). All tests were two-sided, and p < .05 was considered statistically significant.
3 RESULTS
3.1 Patients and baseline characteristics
Among 422 mCRPC patients, MDT records were found in 138/422 (32.7%) patients. The median follow-up time was 27.3 months for the whole cohort, and 184 patients died at the end of follow-up. The OS of the entire cohort was 31.6 months.
Baseline PSA (p = .765), visceral metastasis rate (p = .509), castration resistant-free survival (CFS) (p = .936), Gleason score (p = .371), and repeated biopsy rate (p = 1.000) were balanced between the two cohorts. There was a borderline difference in pathological neuroendocrine differentiation (NED) between the two cohorts (49/138, 35.5% vs. 74/284, 26.0%, p = .059). Patients who chose to attend MDT discussions tended to be younger than those who did not (age >70: 56/138, 40.5% vs. 182/284, 64.0%, p < .001). In addition, patients with MDT experiences harbored lower PSA at CRPC diagnosis (PSA at CRPC diagnosis >100 ng/ml: 19/138, 13.7% vs. 66/284, 23.2%, p = .036), higher positivity of androgen receptor splice variant-7 (AR-V7; 25/138, 18.1% vs. 30/284, 10.6%, p = .045) and aldo-keto reductase family 1 member C3 (AKR1C3; 52/138, 37.7% vs. 67/284, 23.6%, p = .004) (Table 1).
| MDT (−) (n = 284) | MDT ( + ) (n = 138) | All patients (n = 422) | p value | |
|---|---|---|---|---|
| Baseline PSA, ng/ml | 0.765 | |||
| ≤100 | 110 (38.7) | 53 (38.4) | 163 (38.6) | |
| >100 | 152 (53.5) | 80 (57.9) | 232 (54.9) | |
| NA | 22 (7.7) | 5 (3.6) | 27 (6.3) | |
| Age | <0.001 | |||
| ≤70 | 102 (35.9) | 82 (59.4) | 184 (43.6) | |
| >70 | 182 (64.0) | 56 (40.5) | 238 (56.3) | |
| Visceral metastasis | 0.509 | |||
| Present | 264 (92.9) | 125 (90.5) | 389 (92.1) | |
| Absent | 20 (7.0) | 13 (9.4) | 33 (7.8) | |
| CFS, months | 0.936 | |||
| ≤12 | 129 (45.4) | 64 (46.3) | 193 (45.7) | |
| >12 | 155 (54.5) | 74 (53.6) | 229 (54.2) | |
| PSA at CRPC diagnosis, ng/ml | 0.036 | |||
| ≤100 | 213 (75.0) | 115 (83.3) | 328 (77.7) | |
| >100 | 66 (23.2) | 19 (13.7) | 85 (20.1) | |
| NA | 5 (1.7) | 4 (2.8) | 9 (2.1) | |
| Multi-line therapy | <0.001 | |||
| No | 222 (78.1) | 85 (61.5) | 307 (72.7) | |
| Yes | 62 (21.8) | 53 (38.4) | 115 (27.2) | |
| AR-V7 | 0.045 | |||
| Negative | 254 (89.4) | 113 (81.8) | 367 (86.9) | |
| Positive | 30 (10.5) | 25 (18.1) | 55 (13.0) | |
| AKR1C3 | 0.004 | |||
| Negative | 217 (76.4) | 86 (62.3) | 303 (71.8) | |
| Positive | 67 (23.6) | 52 (37.7) | 119 (28.1) | |
| NED | 0.059 | |||
| Negative | 210 (73.9) | 89 (64.4) | 299 (70.8) | |
| Positive | 74 (26.0) | 49 (35.5) | 123 (29.1) | |
| GS | 0.371 | |||
| ≤8 | 72 (25.3) | 27 (19.5) | 99 (23.4) | |
| >8 | 181 (63.7) | 97 (70.2) | 278 (65.8) | |
| Not evaluable | 31 (10.9) | 14 (10.1) | 45 (10.6) | |
| Repeated biopsy | 1.000 | |||
| No | 166 (58.4) | 80 (57.9) | 246 (58.2) | |
| Yes | 118 (41.5) | 58 (42.0) | 176 (41.7) |
- Note: p values were calculated through χ 2 test.
- Abbreviations: AKR1C3, aldo-keto reductase family 1 member C3; AR-V7, androgen receptor splice variant-7; CFS, castration resistant free survival; CRPC, castration-resistant prostate cancer; GS, Gleason score; MDT, multidisciplinary team; NED, neuroendocrine differentiation; PSA, prostate-specific antigen.
3.2 Survival analyses
Univariate survival analyses showed attending MDT discussions could significantly increase patients' (median OS: MDT [+]: 39.7 months; MDT [−]: 27.0 months, hazard ratio [HR]: 0.542, p = .001) (Figure 1A), and this impact remained in multivariate analyses (HR: 0.420 [0.274, 0.614], p < .001), as well as other five factors being independent indexes, including CFS > 12 months (HR: 0.469 [0.340, 0.647], p < .001), PSA at CRPC diagnosis greater than 100 ng/ml (HR: 1.933 [1.361, 2.775], p < .001]), AR-V7 (+) (HR: 1.586 [1.067, 2.357], p = .016), NED (+) (HR: 1.421 [1.021, 1.977], p = .037) and Gleason score greater than 8 (HR: 1.726 [1.128, 2.64], p = .012) (Table 2).
| Univariate analyses | Multivariate analyses | |||
|---|---|---|---|---|
| HR (lower limit, upper limit) | p value | HR (lower limit, upper limit) | p value | |
| MDT (+) | 0.542 (0.376, 0.781) | 0.001 | 0.420 (0.274, 0.614) | <0.001 |
| Baseline PSA > 100 ng/mL | 0.909 (0.671, 1.232) | 0.538 | ||
| Age > 70 | 0.930 (0.692, 1.250) | 0.631 | ||
| Visceral metastasis (+) | 1.739 (1.110, 2.723) | 0.016 | 1.283 (0.779, 2.112) | 0.328 |
| CFS > 12 months | 0.472 (0.352, 0.632) | <0.001 | 0.469 (0.340, 0.647) | <0.001 |
| PSA at CRPC diagnosis > 100 ng/mL | 1.974 (1.417, 2.751) | <0.001 | 1.933 (1.361, 2.775) | <0.001 |
| Multi-line therapy (+) | 0.864 (0.632, 1.182) | 0.362 | ||
| AR-V7 (+) | 1.458 (1.004, 2.119) | 0.048 | 1.586 (1.067, 2.357) | 0.016 |
| AKR1C3 (+) | 1.289 (0.942, 1.764) | 0.113 | ||
| NED (+) | 1.409 (1.033, 1.922) | 0.030 | 1.421 (1.021, 1.977) | 0.037 |
| GS > 8 | 1.848 (1.231, 2.775) | 0.003 | 1.726 (1.128, 2.643) | 0.012 |
| Repeated biopsy (+) | 1.252 (0.935, 1.677) | 0.132 | ||
- Abbreviations: AKR1C3, aldo-keto reductase family 1 member C3; AR-V7, androgen receptor splice variant-7; CFS, castration resistant free survival; CRPC, castration-resistant prostate cancer; GS, Gleason score; HR, hazard ratio; MDT, multidisciplinary team; NED, neuroendocrine differentiation; PSA, prostate-specific antigen.
As for treatment details, patients who attended MDT tended to be more active in the treatment process (higher percentage of multi-line therapy: MDT [+]: 53/138, 38.4%; MDT [−]: 62/284, 21.8%, p < .001). Subsequently, we analyzed the impact of MDT on the OS within subgroups with first or multi-line therapy. The data showed no matter within patients who remained first-line therapy until the end of follow-up (median OS: MDT [+]: not reached; MDT [−]: 27.0 months, p = .001) (Figure 1B) or within patients who received multi-line therapy (median OS: MDT [+]: 36.7 months; MDT [−]: 25.6 months, p = .044) (Figure 1C), dynamic MDT discussions were both correlated with longer survival.
4 DISCUSSION
In this study, we analyzed eligible mCRPC patients in our institute within seven years to explore the influence of MDT discussions on the patients' survival. Results showed that attending MDT helped prolong the OS of mCRPC patients and the survival benefit of MDT remained in subgroups of first-line therapy and multi-line therapy. Besides, patients choosing MDT in this study had undergone more treatments, which resulted in higher rates of AR-V7 and AKR1C3 positivity and possibly higher rates of NED (indicated by lower PSA at CRPC diagnosis and the borderline significance in NED in this group). The more severe disease in patients attending MDT should have biased them toward poorer survival, while they maintained better survival outcomes. In general, our findings can serve as direct support for promoting MDT by validating the statistically significant survival benefit of MDT in the mCRPC patient treatment process.
The MDT approach has been vastly applied in uro-oncological patients nowadays; it can be influential in the clinical decision-making process across the cancer types and prostate cancer, specifically.5, 11, 12 Currently, most of the available studies focus on localized prostate cancer patients, probably since they are the most common patients in western countries nowadays with the help of mass PSA screening.5, 8, 13 It is found to increase active surveillance rate in low-risk patients and the adherence to evidence-based national guidelines in localized prostate cancer across multiple risk groups.6, 14, 15 In patients with a high risk of recurrence, following the recommendations of MDT is also likely to improve the patients' oncologic outcomes.8
While apart from localized prostate cancers, clinicians are also eager to figure out how to maximize the benefit which metastatic patients can get from our comprehensive treatment management.16 Betschart et al.4 shared their experience of using their joint urological-oncological clinic model to treat uro-oncological cases, including advanced and metastatic prostate cancer patients. They reported an improved, non-delayed oncological treatment and a reduced effort for these patients, but they did not perform a direct comparison concerning the survival data.
Besides the patient population issue, the choice of study endpoints is also debatable. Most studies about MDT in prostate cancer focus on the change in treatment plans. However, we perceive that this is not an informative enough indicator in cancer clinical studies, and there are also contradictive results against the influence of MDT on treatment plan alterations.17-20 Although MDT meetings are theoretically able to improve clinical outcomes, there is a lack of evidence for this assumption, except for several reports with heterogeneous designs in different cancer types.11, 12, 21 Consequently, we believe a direct comparison of the overall survival of mCRPC patients to explore the value of MDT can be intriguing and provide more appropriate clinical indications.
mCRPC is considered the lethal stage in the prostate cancer spectrum. Thus, plenty of effort is being put into drug development for these patients. Over the past decade, the growth of mCRPC therapies has been explosive. Urologists nowadays are equipped with a wide span of treatment remedies with various mechanisms and evidence levels, even after patients have progressed on first-line therapies. However, acquiring proficiency in each therapeutic option can be highly overwhelming for doctors in any specialty, especially with the integration of the latest molecular profiling, genomics, and imaging predictors.22
A survey has pointed out that urologists have limited exposure to and lack understanding of the medical and radiation oncology,23 which would likely transform into an unsatisfactory prognosis for their patients. This current situation, understandably, poses significant challenges for urologists to personalize treatment and to develop an optimal sequential treatment plan. Although there are several guidelines for promoting optimal treatment selection, disparities in patient race and socioeconomics, and the inherent dissimilarities among the guidelines make it difficult for clinicians to apply those recommendations fully. Evidence suggests that increasing clinical and research collaboration between urologists and specialties from other professions through the MDT process can improve patient care by providing them with broader access to the latest medical advances. Thus, we believe regular MDT meetings would be the most efficient solution to this hurdle by cross-pollinating the interdisciplinary opinions for patients and providing necessary medical oncology training for urologists.
The strength of this study lies in that we performed a direct comparison of the survival data to explore the influence of MDT on mCRPC patients, in a relatively large cohort. In contrast, most other studies focus on localized prostate cancer patients and choose short-term endpoints for analyses. This finding would be a start to invite more in-depth studies with proof of principle in this area. Our limitations include that this is a single-center retrospective study and a lack of quality-of-life and cost-effectiveness data. Future well-designed prospective studies are needed to validate our findings.
5 CONCLUSION
By and large, we demonstrated that MDT discussions directly correlate with the overall survival in mCRPC patients. These results add to a critical component to the modern management of mCRPC patients; thus, we believe this message should be passed to urological clinicians. More institutes are advised to consider this treatment model for these patients.
ACKNOWLEDGMENTS
This study was supported by the Natural Science Foundation of China (NSFC 81974398), China Postdoctoral Science Foundation (2020M673239), 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (No.0040205301E21), and Science and Technology Support Program of Sichuan Province (2018SZ0221).
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.