Lung growth and pulmonary function after prematurity and bronchopulmonary dysplasia
Abstract
Bronchopulmonary dysplasia (BPD) still carries a heavy burden of morbidity and mortality in survivors of extreme prematurity. The disease is characterized by simplification of the alveolar structure, involving a smaller number of enlarged alveoli due to decreased septation and a dysmorphic pulmonary microvessel growth. These changes lead to persistent abnormalities mainly affecting the smaller airways, lung parenchyma, and pulmonary vasculature, which can be assessed with lung function tests and imaging techniques. Several longitudinal lung function studies have demonstrated that most preterm-born subjects with BPD embark on a low lung function trajectory, never achieving their full airway growth potential. They are consequently at higher risk of developing a chronic obstructive pulmonary disease-like phenotype later in life. Studies based on computer tomography and magnetic resonance imaging, have also shown that in these patients there is a persistence of lung abnormalities like emphysematous areas, bronchial wall thickening, interstitial opacities, and mosaic lung attenuation also in adult age. This review aims to outline the current knowledge of pulmonary and vascular growth in survivors of BPD and the evidence of their lung function and imaging up to adulthood.
1 INTRODUCTION
Rates of preterm birth (gestational age < 37 weeks) have increased globally and now account for 11% of live births.1 Thanks to remarkable advances in perinatal care, more than 95% of subjects born preterm survive and reach adulthood.2 The improved survival rate may come at the expense of future health risks, however, including bronchopulmonary dysplasia (BPD), which is the most common complication of prematurity.
BPD affects between 10% and 89% of preterm infants and about 45% of those born at less than 29 weeks of gestation (WG), depending on the countries and the definition used,3-5 remains a major cause of mortality and long-term respiratory consequences in these populations.5-8
The lungs of survivors of prematurity with and without BPD face a deranged parenchymal and vascular growth, and with frequent respiratory infections in the first 2 years of life. In addition, several of these patients fail to reach the optimal peak of lung function in early adulthood.9
BPD and prematurity are clear examples of how a perinatal insult can be associated with a functional impairment that persists into adult age.10 Pulmonary disease is just one of the multiple morbidities experienced by individuals born preterm. In parallel with aberrant lung development, preterm birth also interrupts the development and maturation of several other organ systems. In fact, it has been suggested that prematurity be considered a chronic condition itself, given its adverse consequences in terms of growth failure, neurodevelopmental sequelae, systemic hypertension, pulmonary hypertension, chronic kidney disease, type 1 and type 2 diabetes, ischemic heart disease in mid-adulthood, and mortality rate.11 Subjects born prematurely require early assessment, long-term follow-up, and preventive action to reduce the risk of multiple chronic diseases later in life.
In this review, we describe the effects of BPD on lung growth, function, and structure in infants who survive the disease.
2 LUNG AND VASCULAR GROWTH IN SURVIVORS OF BPD
In term-born healthy infants, multiplication of the alveoli and maturation of the microvasculature in the lung start in utero and continue in postnatal life.12, 13 Alveolarization persists throughout childhood and adolescence, and even into adulthood,14 resulting in a 20-fold increase in the surface area from birth (0–50 million alveoli) to adulthood (>300 million). Similarly, intra-acinar arteries and veins continue to develop after birth by angiogenesis as long as the alveoli increase in number and size.15 Blood vessel formation and alveolar growth are inter-related processes, with the former actively promoting the latter, and contributing to maintaining the alveolar structures for the rest of an individual's life.16-19
Extremely low gestational age newborns (i.e., <28 WG) are born before the alveoli precursors (saccules, alveolar ducts, alveolar air sacs) have formed, the capillary bed has increased,12, 17, 20 and a sufficient amount of surfactant has been produced by Type II cell (AT2 cells).13, 16 In addition to this picture of lung immaturity, BPD is also a clinical syndrome in which alveolarization and microvascular development are disrupted, resulting in abnormal gas exchange and lung mechanics.13
Most of our current knowledge of BPD histology comes from autoptic findings in infants who died of severe BPD (which happened more frequently in the last century than in recent years, which have seen a reduction in BPD-related mortality). The oldest evidence comes from the pre-surfactant era, when generalized emphysematous changes were found in mechanically ventilated extremely premature infants who died of BPD.21 These findings were also confirmed in the post-surfactant era by Husain et al.22 and classically described what is called “old” BPD.
Premature infants born in more recent years, since the introduction of early rescue surfactant treatment, antenatal glucocorticoids, and more gentle ventilation techniques, show a modified BPD histology or the so-called “new” BPD. This form of the disease is characterized by less severe injury in very immature lungs. The picture is dominated by a simplified alveolar and a smaller number of enlarged alveoli due to reduced septation, associated with a dysmorphic pulmonary microvessel growth that leads to a decreased surface area for alveolar-capillary gas exchange. Histological specimens from infants up to 3 years of age13 and imaging studies in BPD survivors reveal areas of reduced alveolarization, cystic emphysema, fibrosis, and some airway alterations like trachea- and bronchomalacia, and subglottic stenosis.23 The small airways may be affected as well, with mucus gland hyperplasia, epithelial edema, and smooth muscle cell proliferation causing bronchoconstriction. Recent animal studies suggest that immune cells, such as macrophages, may be causally implicated in the disruption of postnatal lung organogenesis.24, 25
It is still unclear how these abnormalities evolve, however, as lung specimens of grown-up BPD patients are rare. Some information may be inferred indirectly from lung function studies assessing pulmonary gas exchange, which confirm a decreased alveolar-capillary membrane function by showing a lower carbon monoxide diffusing capacity in BPD subjects.26, 27 One of the few studies exploring the histopathology of grown-up BPD survivors was recently published by Galderisi et al.,28 who analyzed endobronchial biopsy specimens from three adolescents with reduced lung function and recurrent wheezing exacerbations. They revealed a lymphocytic infiltrate pointing to an ongoing active inflammatory process in the airways and a prominent bronchial vascular density reflecting increased angiogenesis.29
The vascular aspect of the “new” form of BPD is particularly intriguing, since angiogenesis and vessel branching drive alveolar growth.17, 19 The alveolar-capillary membrane grows considerably between 22 and 32 weeks of gestation, and that is why prematurity and lung injury during the neonatal period impair the growth, branching, and distribution of the pulmonary vasculature.30-32 The vascular abnormalities typical of BPD include dysmorphic growth and an altered vascular remodeling, tone, and reactivity, with a higher risk of pulmonary hypertension beyond the first few months of life. Various animal models of BPD and autopsy studies on humans who died of BPD have consistently shown a reduction in the number of small arteries, and an abnormal distribution of vessels in the distal lung.33 The current working hypothesis, the so-called “vascular hypothesis,”34 is that disrupted angiogenesis interferes with alveolarization, while preserved vascular growth and endothelial survival promote growth and sustain the architecture of the distal airspace.19 Vascular endothelial growth factor (VEGF) seems to be the most critical angiogenic growth factor for both vascular and alveolar development. Interestingly, among the avenue of promising future therapies for BPD are mesenchymal stem/stromal cells (MSCs) or their effectors, the extracellular vesicles (EV-MSCs), which proved encouraging results in preclinical studies and are now under testing in Phase 1 and Phase 2 trials. These new drugs have shown clear histological improvements in animal models of BPD,35 with evidence of larger numbers of smaller-sized alveoli, and a reduction in medial arteriolar thickness compared with sham-treated animals. These effects are thought to stem from the paracrine effects of MSC-derived humoral factors, such as interleukin (IL)-6, IL-8, VEGF, collagen, and elastin.36, 37
3 RESPIRATORY OUTCOMES AND LUNG FUNCTION IN INFANCY AND CHILDHOOD
Being born preterm predisposes infants to a high risk of respiratory sequelae in both the short term and the long term.9
Children with BPD have a hospitalization rate of as high as 50% during the first 2 years of life.38, 39 This figure varies among studies, and shows no significant difference between preterm infants with and without BPD.40 Respiratory syncytial virus (RSV) and rhinovirus may increase the risk of hospital admissions in this age group, as they frequently precipitate pulmonary exacerbations.41 This may be due to the infants' immature humoral and adaptive immunity, which increases the risk of severe viral respiratory infections in the first 2 years of life,42 and of earlier and more frequent respiratory symptoms compared to their term counterparts.43, 44 Respiratory infections and exacerbations in infancy and childhood may worsen an already impaired lung structure, giving rise to frequent coughing and recurrent wheezing disorders.40, 45 Furthermore, neonates with BPD and tracheobronchomalacia, a common comorbidity of BPD, are more likely to be mechanically ventilated upon discharge and longer hospitalized compared to their peers without tracheobronchomalacia.46
Lung function in infants and pre-school age can be assessed using tidal flow–volume loops, multiple breath washout, whole-body plethysmography, single-breath occlusion, rapid thoracho-abdominal compression technique (RVRTC) or forced oscillation technique. Studies on neonatal lung function have mostly failed to predict BPD development or duration of mechanical ventilation and supplemental oxygen,47 but lung mechanics measurements reflecting severity of neonatal disease have shown a correlation with a reduced lung function in BPD toddlers.48
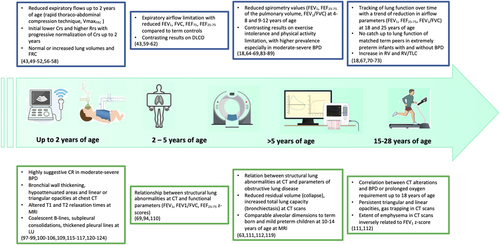
Studies applying the raised volume rapid thoraco-abdominal compression technique and the measurement of the maximal expiratory flow at functional residual capacity (VmaxFRC) on preterm infants with and without BPD have shown reduced expiratory flows up to 2 years of age,43, 49-52 with infants having lower respiratory system compliance at 10–20 days of life demonstrating lower forced expiratory flows at the 2-year follow-up.51 Ventilation with high-frequency oscillatory ventilation (HFOV) during neonatal hospitalization, in combination with surfactant treatment, may lessen the neonatal lung injury with positive effects on later lung function.53 In children with BPD, the need for supplemental oxygen or ventilation at 2 years has been associated with a worse VʹmaxFRC/FRC.54
Respiratory morbidity at the time of follow-up may better predict airway function and respiratory compliance than BPD severity at 36 weeks postmenstrual age (PMA), as demonstrated by a longitudinal cohort of preterm infants where those with BPD and respiratory symptoms had lower VʹmaxFRC, forced mid-expiratory flows (MEF50) and respiratory system compliance (Crs) compared to those without symptoms at 6 and 18 months of postnatal age.55
Whereas lung compliance seems to improve with increasing age, lung volumes and FRC measured with dilution techniques51, 56 and plethysmography55, 57, 58 tend to normalize or even rise by 1 year, suggesting obstructive airway disease with air trapping. Parameters of airway function (forced expiratory volume in 0.5 s (FEV0.5), forced expiratory flow at 75% (FEF75) and FEF25–75), instead, tend to remain low up to 3 years of age.59 Interestingly, Sheperd and colleagues proposed a classification of pulmonary function in BPD survivors based on infant pulmonary function testing (PFT) at approximately 52 weeks PMA, recognizing an obstructive, a restrictive, and a mixed phenotype according to functional residual volume in 0.5 s (FRV0.5), forced vital capacity (FVC), and total lung capacity (TLC). Patients with characteristics of obstruction were about a half (51%) of the total and were also more responsive to bronchodilators (74%).60
The airflow limitation, however, affects infants born preterm without BPD as well, although infants with a previous diagnosis of BPD show lower z scores of airflow parameters. Ethnic differences should be taken into account when conducting PFT in nonwhite infants, as differences in expiratory parameters may derive from ethnicity and not to worse lung function or disease, as occurs in older subjects.61
Expiratory airflow limitation persists at school age and beyond in former preterm infants with and without BPD43 compared with their term-born peers,62 with no apparent catch-up growth in the former's lung function. On the other hand, structural imaging studies at school age (10–14 years) show that, despite their lower forced expiratory volume in 1 s (FEV1), children born extremely preterm have comparable alveolar dimensions to those of term-born and mildly preterm children.63 This may be partly explained by the concept of dysanapsis.
4 RESPIRATORY OUTCOMES AND LUNG FUNCTION IN ADOLESCENCE AND ADULTHOOD
Several longitudinal studies following up cohorts of preterm-born infants with and without BPD demonstrate tracking of lung function over time, as measured by FEV1—a powerful spirometric parameter of flow limitation—regardless of whether subjects were born before or after the introduction of surfactant.64, 65, 67 According to a review and meta-analysis on patients aged 5–23 years, the %FEV1 deficit in those born preterm with and without BPD was about 16.8% and 7.2%, respectively.66 Some reports reveal a gradual decline in lung function with age, raising concern that children with BPD are at higher risk of early-onset chronic obstructive pulmonary disease (COPD).18, 68 In a recent Australian study, Simpson et al. found that preterm infants had a worrying decline in spirometric values from 4 to 12 years of age (0.1 z score per year for FEV1, FEF25–75, and FEV1/FVC), with the poorest trajectories in BPD survivors. Children with bronchial wall thickening on chest computed tomography (CT) (suggestive of inflammation), those exposed to tobacco smoke, born at earlier gestational age, or requiring more supplemental oxygen after birth showed a faster decline in FEV1 (Figure 1).69 Another study conducted by Doyle et al. demonstrated a reduction in all lung function variables reflecting airflow in a BPD group at a mean age of 18.9 years. In 42.4% of this sample, the FEV1/FVC ratio was <75% (the recognized threshold for airway obstruction). This value deteriorated more between 8 and 18 years old than in previous years.70
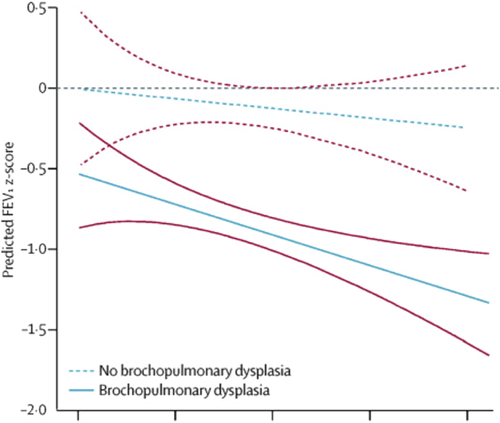
Other authors, however, did not report such an early decline of airflow parameters. Hurst et al.71 documented impaired FEV1 z score and higher bronchodilator reversibility at 19 years of age in subjects born before 26 GW compared to controls, but with similar differences compared to a previous evaluation at 11 years. Similarly, Vollsæter et al.72 found a significant reduction in z scores for FEV1, FEF25–75, and FEV1/FVC in subjects born extremely preterm (GA ≤ 28 GW) only from 18 to 25 years of age, but these lung function changes were similar in the term-born group and there were no trends related to BPD. Children born preterm in 1999–2000 compared to those born in the early 1990s apparently show better pulmonary outcomes, suggesting positive effects of antenatal steroids and surfactant treatment.73
Although the decline of lung function and the time at which it may occur are still a matter of debate, it is clear that preterm infants with and without BPD do not catch up to the lung function of their matched term peers, failing to reach the normal peak at 20–25 years of age and being therefore at risk for early chronic obstructive lung disease.18
Factors contributing to chronic lung dysfunction in children with BPD may include nonsynchronous increases in lung size and airway caliber, chronic airway inflammation, air trapping, and emphysematous changes.13, 74, 75 The concept of “dysanaptic growth,” meaning a disproportionate growth between lung size and airway caliber, may explain the difference in expiratory flows between individuals with BPD and term-born ones despite similar lung sizes.76, 77 Dysanapsis may also explain other spirometric alterations characteristic of adult survivors of very preterm birth, with and without BPD, such as a significantly higher average slope ratio throughout the effort-independent portion of the maximal expiratory flow–volume curve compared with adult controls. This higher slope ratio during early expiration may indeed be due to structural and mechanical properties of the airways,78 and to the persistence of active airway inflammation, as demonstrated by studies on exhaled breath condensate and nitric oxide.79, 80
Available data show that most preterm-born infants and BPD patients embark on a lower than normal lung function trajectory with a higher risk of developing a COPD-like phenotype later in life.20, 54-57 To better understand the evolution of pulmonary function in preterm-born subjects with and without BPD, clinicians and researchers should be encouraged to follow-up these patients longitudinally into adult age. More insight on this topic could come from the new ERS Clinical Collaboration on Chronic Airway Diseases Early Stratification (CADSET).81
Lung function should be considered as a global health biomarker. Poor lung development early in life can point to a poor development of other organ systems too, possibly predisposing to non-communicable diseases later in life.82
5 EXERCISE PERFORMANCE
Preterm-born children with and without BPD may show a higher prevalence of exercise intolerance and reduced physical activity at school-age (8–12 years) compared to their term-matched peers,83, 84 although some follow-up studies do not report exercise limitation in this population.85, 86 Several studies demonstrate that impaired exercise tolerance is predominant in survivors of moderate-severe BPD87-89 and may stem from different pathophysiological changes, from expiratory flow limitation,83, 84, 89, 90 to decreased peak oxygen consumption and anaerobic threshold,87, 91, 92 to altered respiratory mechanics.88, 90 The lower aerobic exercise capacity, derived from the impaired and inadequate respiratory and cardiopulmonary systems to the challenge, may persist into adolescence and adulthood.93 Nevertheless, prematurity regardless of BPD appears to be related to a more sedentary behavior as monitored by accelerometry87 despite the still contrasting results.85, 92
Finally, the few studies conducted in the post-surfactant era have produced conflicting results regarding the diffusing capacity of the lung for carbon monoxide (DLCO) in BPD survivors. Some found a significantly lower DLCO in infants and children born very preterm with BPD, while others showed no difference.94 Nevertheless, despite a decrease in DLCO with the reduction in both membrane component of diffusion capacity (Dm) and pulmonary capillary blood volume (Vc) in infants with BPD, Chang et al.95 found a constant Dm/Vc, indicating both impaired alveolar development and reduced pulmonary vascular bed.
6 IMAGING
Various imaging methods have been used to shed light on BPD ever since the first description published by Northway et al.96 They have initially involved chest radiography (CR), classically supported by CT, but magnetic resonance imaging (MRI) and lung ultrasound (LU) have also recently gained in importance.
All these imaging techniques can at least partially visualize the structural changes that occur in the lung of patients with BPD, and monitor their evolution over time. They are currently used as descriptive tools, but there is increasing evidence to support their application for predictive and prognostic purposes as part of the BPD diagnostic package.
7 CHEST RADIOGRAPHY
CR has demonstrated its capability to predict the evolution of BPD in preterm infants at high risk. Hyödynmaa et al.97 showed that most (89.5%) of the patients who would develop moderate-to-severe BPD at 36 weeks PMA had one of the two radiological patterns of leaky lung syndrome (LLS) with hazy/opaque lungs, or cystic BPD (cBPD) with bubbly lung changes. Oxygen demand at discharge is an independent risk factor for cBPD (odds ratio OR 3).98 So far, CR performed at 7 days of life has been tested as a predictor of BPD or death before 36 weeks PMA,99 with satisfactory results: an interstitial pneumonia pattern had a positive predictive value of 89% and a negative predictive value of 66%.
8 COMPUTED TOMOGRAPHY
CT has been used to assess former preterm infants at various ages, from discharge home after birth up to adulthood.100 When Boechat et al.101 applied a scoring system based on High-resolution computed tomography (HRCT) abnormalities to the youngest infants, they found it was able to identify those likely to develop respiratory morbidities in the first year of life. Other studies confirmed a good correlation between CT abnormalities and clinical scores at 36 weeks PMA, duration of oxygen therapy, and risk of hospitalization for respiratory tract infections.102-104 HRCT abnormalities correlate better with BPD than CR.98, 105
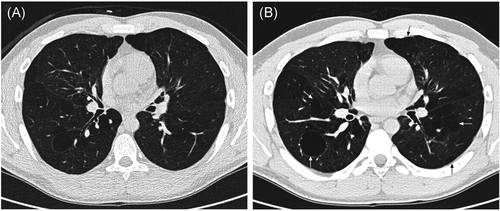
Chest CT frequently shows bronchial wall thickening, hypoattenuation, emphysematous areas and linear or triangular opacities in preterm-born infants and toddlers with BPD,104, 106 and these signs tend to decrease with age.103, 107
An interesting feature that can be analyzed with CT is airway cross-sectional area, which has been found larger in the upper airways and smaller in the lower airways of patients with BPD compared with controls.108, 109
Some studies examined the correlation between CT scoring outcomes and lung function results. Mahut et al.104 reported an inverse correlation between CT score and FRC, while Sarria et al.107 did not found such relationships between CT scores and forced expiratory flows or pulmonary diffusing capacity.
Regarding school age, Simpson et al.94 described the persistence of an extensive damage in preterm-born infants with BPD compared with controls. Comparing these data with functional test results, the authors found that infants with increased subpleural opacities, bronchial wall thickening, and hypoattenuated lung areas had more signs of obstructive lung disease, as expressed by decreased FEV1, FEV1/FVC, and FEV25–75 z scores. Lower z scores for residual volume were associated with areas of collapse and consolidation, while a higher TLC was characteristic of infants with bronchiectasis. The same group recently suggested that infants with CT changes reflecting inflammation (bronchial wall thickening, subpleural opacities or hypoattenuation on inspiratory scans) have the poorest respiratory trajectories, and may be at greater risk of chronic lung disease in elder life.69 Similarly, Ronkainen et al.110 confirmed the inverse relationship between structural CT lung abnormalities and FEV1 on spirometry in school children with a history of BPD.
A few studies focused on chest CT in adult BPD patients. Wong et al. described the common presence of triangular, linear opacities and gas trapping,111 and more importantly reported that the extent of radiological emphysema was inversely related to the FEV1 z score (Figure 2).112
The main issue related to CT is the use of ionizing radiation, limiting the chance to repeat the exam. Another reported problem is the possible need for sedation in young children, increasing the procedural risk. Modern pos-processing techniques are particularly well suited to demonstrate previously unevaluable areas of low attenuation alternated with others of higher attenuation (variegate mosaic attenuation) seen in patients with BPD with small airways obstruction components.113
9 MAGNETIC RESONANCE IMAGING
The evaluation of lung parenchyma with MRI has the advantage of using a nonionizing technique, allowing repeated exams. One limitation, however, is the lower spatial resolution compared with CT (0.86 mm3 vs. 0.2 mm3). Additionally, the low proton density of lung tissue with many air–tissue interfaces can determine extremely low levels of rapidly decaying signal, resulting in the formation of extremely low-resolution images of the lung parenchyma.113 Also, different relaxation times between fibrotic and inflamed tissues and normal and hypodense ones (alveolar simplification, emphysema, cysts) could limit MRI lung evaluation. These issues are partially addressed using ultrashort echo times, as shown by Higano et al.23 Many authors have explored the use of MRI as a diagnostic tool for BPD in recent years. Hahn et al.114 identified a significantly higher signal from the lung parenchyma of BPD patients compared with controls, and attributed this to a greater degree of lung disease (fibrosis, edema, and atelectasis). Walkup et al.115 reported instead that the most severe cases had a drop of signal that they attributed to alveolar simplification. Forster et al.116 found a longer lung T2 relaxation time and a shorter T1 relaxation time as indicators of BPD. When scores similar to those used for CT were applied to the lung MRI findings in BPD patients, Walkup et al.115 described higher scores in the BPD group than in controls, and Higano et al.23 described a good correlation between MRI scores and the duration of respiratory support. Yoder et al.117 demonstrated that MRI can quantify hyperinflation in BPD patients and that their lung volume parameters (FRC, tidal volume, and minute ventilation) increased consistently with disease severity.
Narayanan et al.63 used MRI to study older patients (10–14 years). When they analyzed alveolar size, they found similar results for survivors of extreme prematurity and term-born children, suggesting a catch-up of alveolarization. Contrasting results were published by Flors et al.,118 who described a significantly greater apparent diffusion coefficient (a surrogate of average alveolar dimensions) in patients with BPD, but same lung volumes as age-matched healthy controls, consistently with BPD patients' alveoli being fewer in number and larger in size.
10 LUNG ULTRASOUND
Ultrasound interaction with the highly reflective pleura produces different artifact patterns which correlate with pulmonary aeration.119 LU does not expose the preterm infant to ionizing radiation or require a transfer from the neonatal intensive care unit.
When studied with LU, BPD appears as a nonhomogeneous disease with coalescent B-lines interspersed with intact areas, and always accompanied by multiple different-sized subpleural consolidations, as well as thickened pleural lines. LU has also proved capable of detecting coexisting diseases like atelectasis, pulmonary edema, or consolidations. This suggests that LU could also be of preventive value, guiding treatment decisions and reducing the risk of ventilator-induced lung injury.120, 121
A few studies tested LU as a predictor of BPD development. It seems promising as a way to identify infants that will develop the disease using a semi-quantitative score (with a different sensibility and specificity depending on the cutoff applied and the time of the assessment).122, 123 A recently published large multicenter study has corroborated previous evidence of the predictive power of LU. The method has revealed a good capacity to monitor lung aeration and function in extremely preterm infants, with LU scores correlating significantly with oxygenation metrics and work of breathing. Scores adjusted for gestational age can also significantly predict the occurrence of BPD, starting from the seventh day of life.124
Figure 3 represents the pulmonary structure–function relationship in survivors of BPD and preterm birth.
11 CONCLUSION
Several longitudinal lung function studies have demonstrated that most preterm newborn and BPD patients embark on a low lung function trajectory, never achieve their full airway growth potential, and are at a higher risk of developing a COPD-like phenotype later in life.
To improve the care of BPD survivors and prevent long-term respiratory morbidities, it is fundamental to develop a structured and standardized cardiopulmonary follow-up, and to identify early predictive biomarkers to guide treatment decisions. Lung function and imaging techniques are essential surrogates for monitoring survivors of prematurity with and without BPD from infancy to adult age.125, 126 The long-term surveillance and treatment of these subjects should be strongly promoted.127 Not only pediatricians, but also chest physicians, internists, and family doctors should be aware of their potential for developing a “novel” chronic obstructive lung disease and the multiple associated adverse sequelae.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Laura Moschino: Resources (equal); visualization (equal); writing—original draft (equal). Luca Bonadies: Resources (equal); visualization (equal); writing—original draft (equal).