Visual aid for pediatric virtual musculoskeletal exams: A Barbie girl in a telehealth world
Abstract
Background
Telehealth is rapidly advancing, yet musculoskeletal physical examinations pose a unique challenge with limited clinically tested tools.
Objective
To measure whether visual aid use improves accuracy and efficiency of musculoskeletal exam maneuvers within a mock pediatric telehealth encounter.
Design
Randomized controlled trial.
Setting
Mock telehealth encounter.
Participants
A total of 30 volunteer dyads of children aged 4–17 years old and their parent/guardian. To be eligible to participate, the parent/guardian was required to speak and read English proficiently and have access to Zoom technology on a personal electronic device.
Intervention
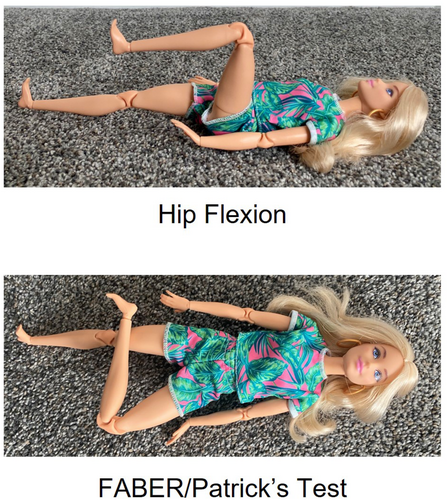
The control group received verbal prompts to complete 12 musculoskeletal exam maneuvers. The intervention group had the addition of a Barbie (Mattel) visual aid.
Main Outcome Measures
Primary outcomes were accuracy (number of completed maneuvers) and efficiency (total verbal prompts, total time). Secondary outcomes were ratings of comfort using telehealth technology, ease of understanding, and perceived usefulness of the visual aid. Standard multiple regression analysis was employed, with significance defined as a p value <.05.
Results
The intervention group completed an average of 11.67 ± 0.7 maneuvers versus 11.27 ± 1.0 in the control group (p = .21), 13:31 ± 4.02 total time (mm:ss) versus 14:47 ± 4:04 (p = .05), and 4.87 ± 4.4 verbal prompts versus 8.40 ± 4.6 (p = .04), respectively. The overall model of group allocation controlling for age was not statistically significant for total maneuvers (p = .255), total time (p = .061) or total verbal prompts (p = .095). However, group allocation significantly predicted total verbal prompts (p = .032), with participants in the intervention group requiring an average of 4.1 fewer prompts. All participants in the intervention group rated the visual aid as ‘definitely helpful’.
Conclusion
Visual aid use improved virtual musculoskeletal exam maneuver ease and efficiency in a pediatric population.
INTRODUCTION
Telehealth adoption has accelerated rapidly over recent years.1, 2 With this rapid change, patients and clinicians have experienced both benefits and challenges in a new health care environment. The majority of patient-related barriers for telehealth use involve technological difficulties (slow internet speed, poor network signal, difficult to use systems), environmental challenges (insufficient space, lack of privacy, frequent distractions), as well as negative perceptions of telehealth and patient's preference for face-to-face communication. Patients often negatively perceive online interaction due to the lack of eye contact as well as decreased physical and social contact. Some patients also show concern due to system security and their personal privacy.3 Common barriers for telehealth adoption among clinicians include difficulties with technically unsavvy staff, resistance to change, difficulties with reimbursement, as well as age and education level of the patient.4
For those clinicians willing and able to adopt telehealth into their practice, the physical examination presents a unique challenge. For many specialties, including physical medicine and rehabilitation, family medicine, and orthopedics, an accurate musculoskeletal exam is essential for high-quality patient care. Anecdotally, patient confidence and satisfaction with the quality of a virtual encounter, including the physical exam, can also contribute to whether they continue to elect for telehealth opportunities for future health care delivery. Some validated tools exist to help clinicians glean information from a completed virtual exam, including virtual goniometers and digital photography.5-7 However, there are few studies of tools or interventions to aid the facilitation of a successful virtual physical exam. Most of the existing literature focuses on exam techniques best suited to telehealth, suggested verbal scripts and camera setup without an interventional component to determine effectiveness.8-10 The purpose of this study was to address this gap in knowledge by evaluating the effectiveness of an inexpensive visual aid to facilitate virtual musculoskeletal exams in a pediatric population. Our primary objective was to determine if using a visual aid would improve the accuracy (number of successfully completed maneuvers) and efficiency (total verbal prompts and/or total time) of a virtual physical exam. Secondary objectives included exploring parental comfort with technology, their ease of understanding instructions, and their perceptions of using a visual aid.
METHODS
Sample participants and recruitment
The child participants had to be aged 4 through 17 years and be accompanied by one parent/guardian. The parent/guardian was required to speak and read English proficiently and have access to Zoom technology on a nonstationary personal electronic device such as a phone, tablet, or laptop. Participants were excluded if they had previously been seen by a physical medicine and rehabilitation (PM&R) physician, had previously participated in virtual care physical or occupational therapy within the last 2 years, or had current pain or physical problems that would limit body movement. Participants were also excluded if a parent, guardian, or other member of the household was currently employed as a health care professional.
The study was approved by the University of Michigan Medical Institutional Review Board. Adult participants completed online consent for themselves and on behalf of their child. For children aged 4–9, the research study was described at the beginning of the Zoom video and verbal assent was obtained. For children aged 10–17, online assent documents were completed before the initiation of the Zoom video. If any child demonstrated distress or unwillingness to participate in the study, the study was stopped. Recruitment was completed through the health system's research recruitment website and Facebook. Interested participants completed a prescreening questionnaire to determine eligibility. Each participant dyad received $10 as incentive for completing the study. Data collection took place between February 4 through March 2, 2022.
Intervention and control conditions
Examination maneuvers were selected based on common examination techniques performed in a pediatric rehabilitation clinic, with a focus on exams of the lower extremity (Table 1). Twelve maneuvers were chosen by practicing rehabilitation physicians, with prioritization toward maneuvers that were thought to be difficult to for an examiner to describe verbally or demonstrate physically from a typical seated, chest and above camera view. A verbal script directing the examination maneuvers was created based on physical exam maneuvers described in a commonly used PM&R textbook11 and was tested on a single volunteer dyad prior to data collection, confirming that the exam maneuvers could be completed correctly using the verbal script alone, and that the study protocol could be completed within a reasonable amount of time for the participants. The order of the exam maneuvers was formulated to minimize the need for positional/camera changes. Participants were randomly allocated to intervention or control conditions using block randomization. The control group worked through the set of maneuvers directed by the verbal script. For the intervention group, a Barbie Fashionista 165 (Mattel) with articulated joints was used as a visual aid to demonstrate the maneuvers in addition to the verbal prompts (Figure 1). The Barbie used in this study can be passively moved in the following motions: ankle dorsiflexion/plantarflexion, knee flexion/extension, hip flexion/extension/external rotation/internal rotation, as well as limited thoracic flexion/extension/rotation and side bend. Barbie cannot be moved to demonstrate ankle inversion/eversion. Numerous upper extremity movements are also possible but were not studied here as these could also be demonstrated in an encounter by an examiner with typical upper extremity function and usual camera setup.
| 1. Ankle range of motion with knee flexed, then with knee extended |
| 2. FABER/Patrick's test |
| 3. Hip flexion |
| 4. Straight leg raise |
| 5. Popliteal angle |
| 6. Hip abduction/adduction |
| 7. Galeazzi test |
| 8. Hip internal and external rotation |
| 9. Thigh foot angle |
| 10. Knee flexion/extension |
| 11. Hip extension |
| 12. Forward bend |
- Abbreviation: FABER, flexion, abduction and external rotation.
During a live Zoom encounter (audio and video recorded) facilitated by a PM&R medical resident physician (A.K.C.), the parent/guardian acted as the hands-on examiner, performing passive range of motion and positioning assistance. Participants were instructed to wait until cued to start each of the maneuvers and progress to complete each bilaterally, when applicable. Additional prompts needed to aid in completion of each maneuver were provided verbatim from the standardized script. Additional prompts were provided only when requested by the participant or if the participant stopped the maneuver prior to successful completion. Progression to the next task occurred after successful completion of the prior maneuver or once a maximum of seven additional verbal prompts were provided. After completion of all 12 maneuvers, the parent or guardian completed a brief online survey that was developed by the research team. If interruptions occurred, such as a pet or additional family member entering the examination area, the script was paused and resumed when the distraction was no longer present. All participants were asked to wear comfortable clothing and participate in a private place where they would not be interrupted. Participants were allocated into intervention and control groups using block randomization. After completion of all 12 maneuvers, the parent/guardian was prompted to complete a post encounter survey. The randomization schedule was generated by online randomization tool by C.Z.K. in blocks of four; the list was maintained by A.K.C. who allocated participants to intervention and control conditions when they joined the Zoom encounter.
Study outcomes
The primary outcomes of the study included successfully completed maneuvers, total verbal prompts, and total time. Successfully completed maneuvers were defined as the number of maneuvers that were completed with complete visualization of the joint in proper positioning. The total verbal prompts were the additional verbal prompts that were given verbatim from the verbal script. Total time was the summation of the time to complete each separate maneuver, which excluded the time to transition between maneuvers. The secondary outcomes assessed comfort of using telehealth technology (5-point Likert scale of comfort), the ease of understanding instructions (5-point Likert scale of difficulty), and the perceived usefulness of the visual aid (5-point Likert scale of helpfulness).
Coding procedures
The recorded videos were reviewed by a board-certified pediatric rehabilitation medicine attending physician (A.K.D.) and fellow physician (B.M.P.). For each video, the reviewers determined the number of verbal prompts, number of successfully completed maneuvers, total time (minutes and seconds), and times for individual task completion. The reviewers used the same point within the script to begin timing each maneuver and followed specific parameters for rating a maneuver as successfully completed, such as complete visualization of the tested joint and proper positioning of the extremity. When discrepancies in rating occurred, they were resolved by an additional review and discussion to reach mutual consensus. Total time was taken as the sum of all exam maneuver times, in order to account for only time spent performing the physical examination itself. Other activities during the Zoom encounter, such as time for obtaining assent or participant needs (clothing changes, moving items in the exam space between tasks), were not included. Reviewers also monitored for adherence to the verbal script, consistent use of verbal prompts, and adequate completion of each task before progressing to the next.
Statistical analysis
We used standard multiple regression to model successfully completed maneuvers, total time, and verbal prompts by group allocation and controlling for age. A p value of below .05 was considered statistically significant. Prior to analysis, we tested assumptions of linearity by inspection of a scatter plot and independence of observations using the Durbin–Watson statistic and assessing the normality of residuals by visually inspecting the normal probability plot. Homoscedasticity, or whether the variance of errors is consistent across independent variables, was assessed by visual inspection of a plot of standardized residuals versus standardized predicted values. Multicollinearity, or when two or more independent variables are highly correlated, was assessed by tolerance values greater than 0.1. Outliers or other highly influential points were assessed by examining studentized deleted residuals greater than ±3 SDs, leverage values >0.2, and values for Cook's distance >1. The normality of residuals was assessed by a Q-Q Plot. We used a Student's t-test to assess group differences in the experience of the examination.
RESULTS
Participant characteristics
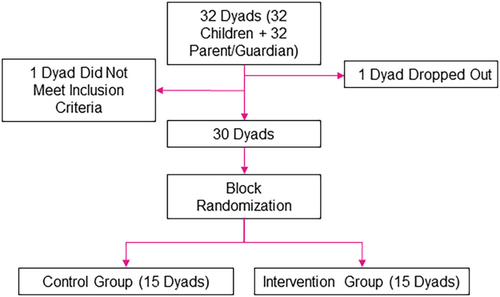
A total of 32 dyads were evaluated for eligibility (32 children +32 parents/guardians) and 30 were enrolled. One dyad did not meet inclusion criteria, and another withdrew due to the child expressing a preference not to participate. The remaining 30 dyads were equally allocated into intervention and control groups (Figure 2).
Descriptive data including gender, race or ethnicity, technology used, and parental education can be found in Table 2. The majority of participants used a laptop to facilitate the virtual encounter. The majority of the parents/guardians had obtained a bachelor's degree or higher. The only significant difference between the groups was a higher mean age of children in the control group versus intervention group (10.5 versus 7.7, p = .019).
| Characteristic | Control group (N = 15) | Intervention group (N = 15) |
|---|---|---|
| Mean age, years (range)* | 10.5 (6–17) | 7.7 (5–11) |
| Child gender: N (%) | ||
| Female | 9 (60.0) | 4 (26.7) |
| Male | 6 (40.0) | 10 (66.7) |
| Nonbinary | 0 (0.0) | 1 (6.7) |
| Parent/guardian gender: N (%) | ||
| Female | 14 (93.3) | 11 (73.3) |
| Male | 1 (6.7) | 4 (26.7) |
| Race or ethnicity: N (%) | ||
| Asian or Pacific Islander | 1 (6.7) | 2 (13.3) |
| Black or African American | 1 (6.7) | 0 (0.0) |
| White | 12 (80.0) | 13 (86.7) |
| Multiracial or biracial | 1 (6.7) | 0 (0.00) |
| Technology used: N (%) | ||
| Mobile phone | 4 (26.7) | 4 (26.7) |
| Tablet | 0 (0.0) | 3 (20.0) |
| Laptop | 11 (73.3) | 8 (53.3) |
| Parent/guardian education: N (%) | ||
| Bachelor's degree or higher | 14 (93.3) | 12 (73.4) |
- * p = .019.
Maneuvers, time, and verbal prompts
Our primary outcomes included number of successfully completed maneuvers, total time, and total verbal prompts. In univariate analysis, the intervention group completed an average of 11.67 ± 0.7 maneuvers versus 11.27 ± 1.0 in the control group (p = .21). For total time (mm:ss), the intervention group required an average of 13:31 ± 4:02 versus 14:47 ± 4:04 in the control group (p = .052). For verbal prompts, the intervention group required 4.87 ± 4.4 versus 8.40 ± 4.6 verbal prompts in the control group (p = .042).
In terms of testing assumptions for the regression models (successful maneuvers, total time, and verbal prompts), there was independence of residuals for all outcomes (Durbin–Watson statistic of 2.265, 1.799, and 1.932, respectively). For all outcomes, no outliers were identified, there was homoscedasticity, residuals were normally distributed, and there was no evidence of multicollinearity.
For successful maneuvers, group allocation was not statistically significant (p = .113). For total time to complete the exam, group allocation also was not statistically significant (p = .061). For the total number of prompts needed, group allocation was statistically significant (p = .032), such that participants in the intervention group needed 4.1 fewer prompts, on average, that those in the control group. Regression coefficients and SEs are given in Table 3.
| Primary outcomes | 95.0% CI for B | |||||
|---|---|---|---|---|---|---|
| B | LL | UL | SE B | β | ||
| Completed maneuversa | (Constant) | 10.93 | 8.33 | 11.85 | 0.86 | |
| Group allocation | 0.56 | −0.14 | 1.26 | 0.34 | 0.33 | |
| Child age | 0.06 | −0.05 | 0.168 | 0.05 | 0.22 | |
| Total timeb | (Constant) | 506.77 | 294.41 | 719.14 | 103.50 | |
| Group allocation | −80.63c | −165.38 | 4.12 | 41.30 | −0.39 | |
| Child age | −2.23 | −15.44 | 10.98 | 6.44 | −0.07 | |
| Total verbal promptsd | (Constant) | 14.98 | 5.51 | 24.45 | 4.61 | |
| Group allocation | −4.16 | −7.94 | −0.39 | 1.84 | −0.44 | |
| Child age | −0.23 | −0.82 | 0.36 | 0.29 | −0.16 | |
- Abbreviations: B, unstandardized coefficient; CI, confidence interval; LL, lower limit and UL, upper limit; SE B, standardized error of the coefficient; β, standardized coefficient.
- a R2 of 9.6%, adjusted R2 of 2.9%; F(2, 27) = 1.44, p = .255.
- b R2 of 13.2%, adjusted R2 of 6.7%; F(2, 27) = 2.05, p = .148.
- c Unit = seconds.
- d R2 of 16%; adjusted R2 of 9.8%; F(2, 27) = 2.57, p = .095.
Experience of the examination
Of the participants, 77% felt either somewhat or extremely comfortable using video conference technology in general and 73% felt comfortable when using this technology in a health care setting. There were few group differences in the experience of the examination with the exception of significantly less difficulty among those in the intervention groups (see Table 4).
All intervention group participants rated the visual aid as “definitely helpful.” In the control group, 60% believed that the addition of a visual aid would have been helpful while 33.3% were unsure. The majority of participants (83%) found the experience “somewhat” or “extremely enjoyable.”
| Survey question | Intervention group mean | Control group mean | t | Sig. | 95% CI |
|---|---|---|---|---|---|
| How comfortable are you using video conference technology in general? | 4.33 | 3.80 | −1.02 | .32 | (−1.607 to 0.541) |
| Comfort using video conference technology for health care | 4.27 | 3.60 | −1.48 | .15 | (−1.589 to 0.255) |
| Comfort assisting child in physical exam | 4.00 | 4.00 | 0.00 | >.99 | (−0.894 to 0.894) |
| How difficult was it to understand the movements? | 4.33 | 3.47 | −2.33 | .03 | (−1.629 to 0.105) |
| How confident were you that the examiner was able to see what they needed? | 4.13 | 3.80 | −0.83 | .42 | (−1.159 to 0.493) |
| How enjoyable was this experience? | 4.27 | 4.20 | −0.22 | 0.83 | (−0.688 to 0.555) |
- Note: Italics in this table are to highlight the statistically significant survey question and results.
DISCUSSION
This study is the first to investigate a tool to improve virtual musculoskeletal exams in the pediatric population. The visual aid used in this study is inexpensive, widely available, and can be found in different genders and skin tones. The study maneuvers were well tolerated by both the adults and children, with no participants discontinuing the study during the scripted examination. No significant difference was found in completion rates between the groups. This supports the clarity of the verbal script and that the exam was feasible to complete in both groups. There was no statistically significant difference in the time to complete the entirety of the 12 physical exam maneuvers. However, roughly four fewer prompts from the facilitator were needed when the visual aid was present, and the postencounter survey confirmed improved understanding with use of the visual aid. This decrease in additional guidance/verbalization demonstrates improved efficiency of the encounter. Given the significant differences in age between the two participant groups, it is notable that the younger-aged intervention group was able to complete the same tasks with fewer prompts and without additional time.
A strength of this study is that the participants completed the exam maneuvers in their own home using their own laptop, phone, or tablet. Using the same technology within the same environment allowed us to simulate a real virtual health care encounter. However, with this came numerous factors that could not be controlled for, such as differences in video technology, internet speed, lighting quality, and environment setup.
The home environment sometimes allowed for unexpected distractions/interruptions by pets and other members of the household. To account for these factors, we measured total time as the sum of all exam maneuvers, allowing our team to account for only time spent performing the physical examination itself. We did not estimate sample size a priori; our sample size of 30 dyads was relatively small and limited by resource constraints. As such, results should be considered preliminary and replicated in larger samples. Due to the nature of the intervention, the facilitator and video reviewers could not be blinded, raising the possibility of bias. Measures aimed at minimizing any bias included a consistent facilitator throughout all 30 interviews, adherence to specific rules for when and how to provide additional prompts, as well as quality control by the study's coders.
Although the two study groups did not differ significantly in gender of the child or parent, race, educational level, or technology used, the average age of the child participants in the control (no visual aid) group was significantly older despite randomization. Another limitation of our study is the lack of diversity in the parent participants. The study population was largely composed of highly educated White females. These participants are likely representative of a higher socioeconomic status, with the vast majority having obtained a bachelor's degree or higher. This highly educated participant population likely stems from the primary recruitment source, a university-maintained website that allows potential research participants to voluntarily register and receive updates about actively recruiting studies. Willingness to learn about and voluntarily participate in research likely indicates a recruitment pool with higher health literacy and educational attainment.12 However, the education levels were similar between the two groups, still allowing us to evaluate the effect of using a visual aid. The use of a visual aid could potentially be more beneficial in the general population, as it may provide a useful supplement for those with lower receptive language functioning, hearing impairment, or cognitive limitations.
CONCLUSION
Telehealth encounters have rapidly expanded to represent a significant portion of health care delivery in the United States. As patients and clinicians make choices about when and how to integrate this into their own practices, it is important to have tools to preserve the efficiency and clarity of the physical examination. We conclude that the Barbie visual aid is a useful tool for improving musculoskeletal examinations in a virtual setting for both the provider and the patient.
ACKNOWLEDGMENTS
We would like to thank the Christopher Family SOAR foundation for funding our visual aid and for providing the monetary incentive for our participants. Many thanks to Allison and David Daunter for assisting with the trial run and providing feedback on the verbal script. The authors received no financial support for the research, authorship, and/or publication of this article. Funding for participant incentives and purchasing the visual aid was provided by the Christopher Family SOAR Foundation.
DISCLOSURE
The authors declare that there is no conflict of interest.




