Clinical analysis of first branchial cleft anomalies in children
Abstract
Importance
First branchial cleft anomaly (FBCA) is a rare disease that is difficult to diagnose and is associated with a high rate of complications. However, the difference between two types of FBCA and how to avoid complications are not clear enough.
Objective
We retrospectively analyzed type I and II (Work's classification) FBCAs in children to demonstrate the difference between the two types of FBCAs, especially with respect to understanding the relationship between FBCAs and the facial nerve
Methods
We retrospectively reviewed patients with FBCAs who were treated in Beijing Children's Hospital from 2013 to 2017. The patients’ clinical data, relationship of the FBCA with the facial nerve, and postoperative complications were recorded.
Results
The study included 70 patients with FBCAs. In total, 41 (58.6%) patients had a type I FBCA, and 29 (41.1%) had a type II FBCA. A cystic mass was present in 34 (48.6%) patients. Sixty-two (88.6%) patients had a history of incision and drainage and nine (12.8%) had a history of excision surgery in other hospitals. The accuracy rate of magnetic resonance imaging was higher than ultrasound and much higher than computed tomography. Thirty-eight (92.7%) type I FBCAs had no close relationship with the facial nerve. The facial nerve in 14 (48.3%) patients with type II FBCAs was located superficial to and above the mass. Fifteen (51.7%) type II facial nerves were located on the deep side of the mass. All patients in the study had an abnormal external auditory canal (EAC). Three patients had temporary facial palsy that resolved within one week. Eleven patients with type I FBCAs had mild EAC stenosis. No recurrence was observed.
Interpretation
Type II FBCAs had a close relationship with the facial nerve, especially when the lesion was located in the mandible angle. All patients with FBCAs had an EAC abnormality. The abnormal skin and cartilage of the EAC should be excised together to avoid recurrence.
INTRODUCTION
Four types of branchial cleft anomalies exist in children. First branchial cleft anomalies (FBCAs) account for <8% of the four types. An FBCA is a rare disease that is difficult to diagnose and is associated with a high rate of complications, such as facial nerve paralysis. The typical clinical presentation of FBCA is purulent drainage from the external auditory canal (EAC) or swelling in the parotid area or postauricular area. Many classifications of FBCAs have been proposed. In 1972, Work1 divided FBCAs into two types based on their anatomical and histological features. A type I FBCA is a cystic mass in the postauricular area extending to the posterior wall of the EAC.2 The lesion is of ectodermal origin. A type II FBCA is located from the earlobe to the mandible angle. These lesions are both ectodermal and mesodermal and might present as a fistula or cyst. In 1980, Olsen et al3 divided FBCAs into cysts, sinuses, and fistulas according to their morphology. A fistula was defined as a tract with two openings, a sinus was defined as a tract with a single opening, and a cyst was defined as a tract with no opening. The classification described by Work1 is considered to be more effective in the clinical setting. Surgical excision of FBCA is the best treatment choice, but it is associated with a high risk of facial palsy after surgery. In the present study, we retrospectively analyzed patients with FBCAs at Beijing Children's Hospital (BCH) from 2013 to 2017. The purpose of the study was to demonstrate the relationship between type I/II FBCAs and the facial nerve, an understanding of which could help to decrease postoperative complications.
METHODS
Patients
We retrospectively analyzed 70 patients with FBCAs treated at BCH from January 2013 to December 2017. We obtained approval from the institution's research ethics board. The diagnosis of FBCA was defined as a recurrent mass or draining sinus in the postauricular region or neck over the mandible angle. A pathological examination was performed to confirm the diagnosis in all cases.
Classification
The FBCAs were classified according to Work1: a type I FBCA was a cystic mass in the postauricular area extending to the posterior wall of the EAC, and a type II FBCA was a mass located from the earlobe to the mandibular angle.
Surgical method
All operations were performed under general anesthesia in BCH.
Type I
A fusiform incision was made, including the infected area in the post-aurum. Another straight incision was made from the top of the fusiform incision to the top wall level of the EAC.
Type II
A fusiform incision was made, including the opening of the fistula or sinus. Another straight incision was made from the top of the fusiform incision to the inferior wall of the EAC.
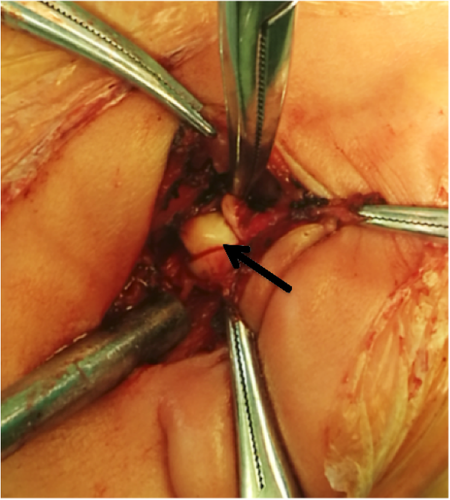
After exposure of the mass, we used a microscope and facial nerve monitor to more clearly expose the mass and nerve. For type I FBCAs, we routinely spilt the cartilage of the posterior wall of the EAC, allowing us to visualize the lesion in its totality. For type II FBCAs, we gently separated the subcutaneous tissue because the variant facial nerve might be very superficial in some patients.
Recorded information
The following basic clinical information was recorded: sex, age, chief complaint, side of cyst/sinus/fistula, history of surgery and drainage, and results of magnetic resonance imaging (MRI), ultrasound, or computed tomography (CT). We also recorded the relationship among the FBCA, facial nerve, and EAC during surgery. Type I FBCAs were subdivided into two types: no close relationship between the facial nerve and FBCA, and location of the facial nerve inferior to the FBCA. Type II FBCAs were subdivided into three types: no close relationship between the facial nerve and FBCA, location of the facial nerve superficial to and above the FBCA, and location of the facial nerve on the deep side of the FBCA. Additionally, facial palsy and EAC stenosis were recorded as postoperative complications.
Statistical analysis
We used JMP 10.0 for the statistical analysis.
RESULTS
Clinical information
The study cohort included 70 patients (35 male, 35 female). Thirty-six (51.4%) lesions were located on the left, 33 (47.2%) were located on the right, and only one (1.4%) was bilateral. The patients’ ages ranged from 10 months to 14 years (median age, 4 years). Forty-one (58.6%) patients had type I FBCAs and 29 (41.1%) had type II FBCAs. Thirty-four (48.6%) patients presented with a cystic mass, 22 (31.4%) presented with a fistula, and 14 (20.0%) presented with a sinus. Sixty-two (88.6%) patients had a history of incision and drainage and nine (12.8%) had a history of excision surgery in other hospitals (Table 1).
| Characteristics | Number of patients | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 35 | 50.0 |
| Female | 35 | 50.0 |
| Side | ||
| Left | 36 | 51.4 |
| Right | 33 | 47.2 |
| Bilateral | 1 | 1.4 |
| Work's classification | ||
| Type I | 41 | 58.6 |
| Type II | 29 | 41.1 |
| Olsen classification | ||
| Cyst | 34 | 48.6 |
| Fistular | 22 | 31.4 |
| Sinus | 14 | 20.0 |
| Incision and Drainage History | ||
| Yes | 62 | 88.6 |
| No | 8 | 11.4 |
| Surgical History | ||
| Yes | 9 | 12.8 |
| No | 61 | 87.2 |
Auxiliary examination
Before surgery, all 70 patients underwent MRI (without contrast) and ultrasound to obtain a diagnosis, and 46 patients also underwent a CT scan (without contrast). In a comparison of these imaging findings with the postoperative pathology results, the accuracy rate of MRI was higher than that of ultrasound and much higher than that of CT (Figure 1).
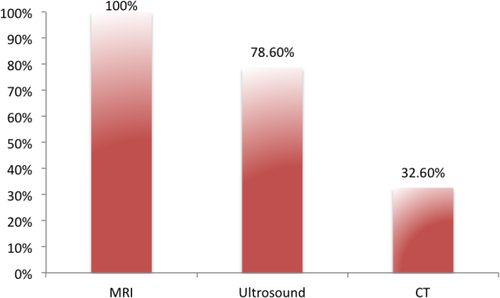
The accurate rate of MRI, Ultrasound and CT.
MRI, magnetic resonance imaging; CT, computed tomography.
Relationship between FBCAs and facial nerve
Among all 70 patients, 38 (92.7%) type I FBCAs did not have a close relationship with the facial nerve. In three (7.3%) patients with type I FBCAs, the facial nerve was located inferior to the mass. In 14 (48.3%) patients with type II FBCAs, the facial nerve was located superficial to and above the mass. In 15 (51.7%) patients with type II FBCAs, the facial nerve was located on the deep side of the mass (Figure 2). In six (85.7%) of seven patients with type II FBCAs with the lesion located below the mandibular angle, the facial nerve was located just superficial to and above the mass (Table 2).
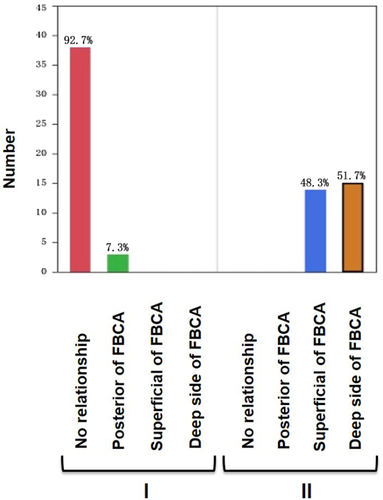
| Location | Number | Superficial to FBCA | Percentage (%) |
|---|---|---|---|
| Below the earlobe | 22 | 8 | 36.4 |
| At or below mandibular angle | 7 | 6 | 85.7 |
- FBCA, first branchial cleft anomaly
Relationship between FBCAs and EAC
All patients with FBCAs had an EAC deformity. All patients with type I FBCAs had an abnormality in the posterior wall of the EAC, and 96.6% of patients with type II FBCAs had an abnormality in the inferior wall of the EAC (Figure 3).
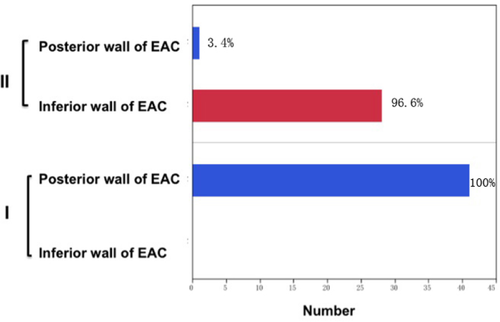
The relationship between FBCA and EAC.
FBCA, first branchial cleft anomaly; EAC, external auditory canal.
Surgical duration of type I and II FBCAs
The surgical duration ranged from 40 minutes to 3.6 hours. The median duration for type I and II FBCAs was 1 and 2 hours, respectively (Figure 4).

Follow-up
The follow-up period ranged from 10 months to 5 years. The median follow-up period was 2 years 5 months. Three patients with type II FBCAs developed temporary facial palsy that recovered within 1 week with hormone treatment. Two of these patients had a history of more than one incision and drainage procedure. Eleven patients with type I FBCAs developed mild EAC stenosis, but the stenosis did not influence the ear examination. No patients developed recurrence, and all patients’ wounds healed well.
DISCUSSION
An FBCA develops as a result of incomplete fusion of the cleft between the first and second branchial arches.4 FBCAs are difficult to diagnose and treat. Many patients with FBCAs develop a recurrent mass or draining sinus in the postauricular region (type I) or in the neck over the mandibular angle (type II) (Figures 5, 6).5 Thus, FBCAs can influence the quality of children's lives.


The present study demonstrated that MRI is the best diagnostic technique for FBCAs. The MRI results are more accurate than ultrasound and CT. FBCAs are hypointense on T1-weighted MRI and hyperintense or isointense on T2-weighted MRI. This can help us to recognize the relationship among the lesion, parotid, and EAC, which will be useful for planning the surgery. The ultrasound results may be influenced by the doctor's experience. CT is not a good choice because it does not show the quality of the mass and induces high radiation damage.
Facial palsy and EAC stenosis are the most common complications of FBCA surgery.6 These complications increase the difficulty of the surgery.
The present study demonstrates that type II FBCA has a close relationship with the facial nerve. The facial nerve and its muscles migrate upward between the sixth and eighth weeks of development.7 The FBCA migrates between the sixth and seventh weeks. Thus, which one develops first determines the relationship of the facial nerve with the FBCA. Liston8 proposed that the developing facial muscles were responsible for this variation. If the facial musculature migrated inferior to the first cleft, the facial nerve would be deep to the lesion.
Surgical excision is the only treatment choice. Because of the close relationship between the lesion and facial nerve, the risk of facial nerve damage is high. A previous study showed a high (22%) incidence of facial nerve palsy even with prior identification of the facial nerve.8 If we can evaluate this risk before surgery, we could more confidently protect the nerve and communicate with patients and their families. D'Souza et al6 considered that extra care and caution should be exercised in younger patients (< 6 months), those with fistulous tracts, and those with a tract opening in a location other than the EAC. In the present study, we did not consider the relationship between age and the facial nerve. We demonstrated that for type II FBCA, if the lesion was located in the mandibular angle, the facial nerve might lay more superficial to and above the mass. If the surgeon does not pay sufficient attention, the facial nerve may be cut off when the subcutaneous tissue is separated. We consider four points to be important for protecting the facial nerve. First, diagnosis and treatment should be performed as early as possible. One of our patients was misdiagnosed with a lymphatic malformation. She had received four pingyangmycin injections at other hospital. During the FBCA surgery, we observed numerous fibrotic adhesions between the mass and facial nerve, and separation of the mass was very difficult. The incorrect diagnosis and treatment made the excision more difficult. The second important point is that a sufficient preoperative evaluation should be performed. We consider that type I FBCA does not have a close relationship with the facial nerve; however, type II has a high risk of facial nerve injury. The third and perhaps most important point is to ensure familiarity with the facial nerve anatomy. Finally, auxiliary equipment such as a microscope and facial nerve monitor should be used during the surgery.
Different surgeons have different opinions on operative techniques. Solares et al7 considered that successful treatment of FBCA requires complete resection and stated that complete resection requires full exposure of the facial nerve. We recommend making the incision as described by Zhang and Ni et al9 instead of the traditional “S” or “Y” shaped incision. For type I FBCAs in the present study, a fusiform incision was made, including the infected area in the post-aurum. Another straight incision was made from the top of the fusiform incision to the top wall level of the EAC. For type II FBCAs, a fusiform incision was made, including the opening of the fistula or sinus. We made another straight incision from the top of the fusiform incision to the inferior wall of the EAC. Such an incision could adequately expose the base of the mass. During the surgery, a microscope and facial nerve monitor should be routinely used, especially for type II FBCAs. We did not consider that we must first expose the facial nerve. Whether facial nerve injury occurs was not determined by total exposure of the nerve but instead by careful dissection of the nerve. For type I FBCAs, we considered routinely splitting part of the cartilage of the posterior wall of the EAC. After splitting the cartilage, we could clearly see the base of the mass (Figure 7).
Our study showed that all patients with FBCAs had an EAC abnormality. Such abnormalities could present as a depressed EAC, a promontory, or a fistula. Therefore, it was very important to assess the EAC during the physical examination. Our study included 11 patients with type I FBCAs who developed postoperative EAC stenosis. We considered that too much skin or cartilage of the EAC was resected after we split the auricular cartilage, resulting in the EAC stenosis. Fortunately, the mild stenosis did not lead to more complications such as canal cholesteatoma or keratosis obliterans.
Type II FBCAs have a close relationship with the facial nerve, especially when the lesion is located in the mandibular angle. This is because the facial nerve may be located more superficial to and above the fistula. All patients with FBCAs in this study had an EAC abnormality. The abnormal skin or cartilage of the EAC should be excised together to avoid recurrence.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.