The effect of central nervous system involvement and irradiation in childhood acute lymphoblastic leukemia: Lessons from the NOPHO ALL-92 and ALL-2000 protocols
Mervi Taskinen and Trausti Oskarsson contributed equally to the writing of the manuscript.
[This article was corrected on 3 November 2016 because one abbreviation in the article title needed to be spelled out.]
Abstract
Background
Central nervous system irradiation (CNS-RT) has played a central role in the cure of acute lymphoblastic leukemia (ALL), but due to the risk of long-term toxicity, it is now considered a less-favorable method of CNS-directed therapy.
Procedures
Retrospectively, we estimated the effect of CNS involvement and CNS-RT on events and overall survival (OS) in 835 children treated for high-risk ALL in the Nordic Society of Paediatric Haematology and Oncology (NOPHO) ALL-92 and ALL-2000 trials.
Results
We did not observe a statistically significant difference in the OS or event-free survival (EFS) in patients with CNS involvement at diagnosis, but the risk of isolated CNS relapse was higher (hazard ratio [HR] 7.09, P < 0.001). CNS-RT was given to 169 of the 783 patients in first complete remission, of which 16 had CNS involvement at diagnosis. In general, CNS-RT improved EFS (HR 0.58, P < 0.05) but not OS (HR 0.69, P = n.s.). The adjusted HRs for all relapses, isolated bone marrow relapse, CNS-involving relapse, and isolated CNS relapse, were 0.47 (P < 0.01), 0.50 (P < 0.05), 0.34 (P < 0.01), and 0.12 (P < 0.01), respectively, in irradiated patients.
Conclusions
CNS-RT was associated with an advantage in EFS by decreasing the risk of relapse but without improving OS.
ABBREVIATIONS
-
- ALL
-
- acute lymphoblastic leukemia
-
- BM
-
- bone marrow
-
- CNS
-
- central nervous system
-
- CNS1-2
-
- no central nervous system leukemia
-
- CNS3
-
- central nervous system leukemia
-
- CNS-RT
-
- central nervous system irradiation
-
- CR1
-
- first complete remission
-
- CSF
-
- cerebrospinal fluid
-
- DCR1
-
- death in first complete remission
-
- EFS
-
- event-free survival
-
- EI
-
- extra-intensive
-
- HR
-
- hazard ratio
-
- HSCT
-
- hematopoietic stem cell transplantation
-
- IT
-
- intrathecal
-
- MLL
-
- mixed-lineage leukemia
-
- MRD
-
- minimal residual disease
-
- MTX
-
- methotrexate
-
- NOPHO
-
- Nordic Society for Paediatric Haematology and Oncology
-
- OS
-
- overall survival
-
- SMN
-
- second malignant neoplasm
-
- T-ALL
-
- T-cell acute lymphoblastic leukemia
-
- VHR
-
- very high risk
-
- VI
-
- very intensive
-
- WBC
-
- white blood cell count
1 INTRODUCTION
The survival of children with acute lymphoblastic leukemia (ALL) has improved over the last five decades from anecdotal cases to above 90% in the best contemporary clinically and biologically risk-stratified treatment programs.1-3 The therapy has been increasingly risk-adapted using biological features of leukemia,4 sensitive methods for measurement of the response to therapy,5 and exploiting improved understanding of the pharmacology of antileukemic agents. Since a large fraction of patients in early trials suffered central nervous system (CNS) relapses, an important part of a comprehensive approach is CNS-directed prophylactic therapy.6-8
The CNS and the testicles are pharmacological sanctuaries of leukemic cells. With advances in modern ALL treatment, testicular relapses are now very uncommon. Although the frequency of CNS relapses has decreased, they remain a clinical challenge. A majority of patients who relapse in the CNS also have bone marrow (BM) involvement, at least on the minimal residual disease (MRD) level.9 Before the addition of CNS-directed therapy, 50% of all patients relapsed in the CNS,1, 6 but on contemporary ALL-protocols with CNS-directed prophylactic therapy, CNS-involving relapses occur in only 4–5% of the patients.2, 10
The most commonly applied approaches to CNS-directed therapy have been CNS irradiation (CNS-RT), intrathecal (IT) chemotherapy with methotrexate (MTX), or IT triples (MTX, prednisolone, cytarabine). In addition, systemic high-dose chemotherapy with MTX or cytarabine is frequently used,1 although the impact is uncertain.11 Cure rate from childhood ALL was at 15–20% before the era of prophylactic CNS-directed therapy but improved with development of systemic and IT chemotherapy and prophylactic CNS-RT.6 Along with the development of ALL treatment, the doses of prophylactic CNS-RT have been reduced and even omitted from some of the most recent ALL protocols.7, 10, 12, 13 At the same time, dexamethasone,14 asparaginase,15 and 6-thioguanine16 have played a role in the systemic approach to CNS-directed therapy.
The aims of this study were to evaluate the impact of CNS involvement at diagnosis (central nervous system leukemia [CNS3]) and CNS-RT on the risk of adverse events and overall outcome in high-risk ALL-patients treated on the Nordic Society of Paediatric Haematology and Oncology (NOPHO) ALL-92 and ALL-2000 protocols.
2 PATIENTS AND METHODS
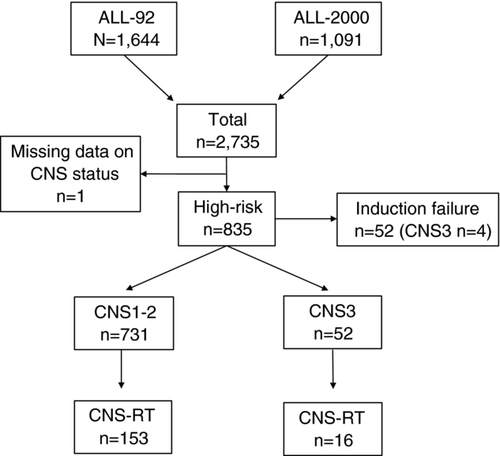
The NOPHO ALL-92 and ALL-2000 studies were open for recruitment from January 1992 to October 2001 and from January 2002 to July 2008, respectively. Both protocols included patients from the age of 1.0 up to 14.9 years. Altogether, 2,735 children with ALL were treated on the NOPHO ALL-92 (N = 1,644) and ALL-2000 protocols (N = 1,091) in the five Nordic countries (Denmark, Finland, Iceland, Norway, and Sweden).10 Of these, 836 patients were stratified to the high-risk arms, including 462 ALL-92 and 374 ALL-2000 patients (Fig. 1). One patient did not have CNS status registered and was excluded from the study cohort resulting in 835 high-risk patients in the analyses. The median follow-up time was 7.8 (range 0.07–20.9) years.
2.1 The definition of the CNS status
CNS3 was defined as an elevated cerebrospinal fluid (CSF) white blood cell count (WBC) (≥5 mononuclear cells/μl) and a cytospin preparation demonstrating leukemic blasts. CNS3 was also diagnosed when the CSF leukocyte count was normal, but clinical (cranial nerve palsy) or neuroimaging signs (two patient diagnosed solely by imaging and symptoms and no blast in the CSF) of CNS involvement were present. CNS3 diagnoses have been re-evaluated by one of the researchers (ML).
2.2 High-risk criteria
CNS3 status at diagnosis stratified the patient into the high-risk therapy in both NOPHO ALL-92 and ALL-2000 protocols.10 The other high-risk criteria for both protocol cohorts were WBC ≥50 × 109 l–1, T-cell immunophenotype, lymphomatous features, testicular leukemia, or slow response (day 15 marrow M3 and/or day 29 marrow ≥M2). The stratifying high-risk cytogenetics in the ALL-92 protocol were t(9;22)(q34;q11), mixed-lineage leukemia (MLL) rearrangements (11q23), (22q-), t(8;14)(q24;q32), t(2;8)(p12;q24), or t(8;22)(q24;q11) and in the ALL-2000 protocol were t(9;22)(q34;q11), t(4;11)(q21;q23), t(1;19)(q23;p13.3), and hypodiploidy (modal chromosomal number <45).
The three high-risk subgroups in the ALL-92 protocol era were very high risk (VHR, age ≥5 years with CNS3, poor early response, or T-cell acute lymphoblastic leukemia [T-ALL] with another high-risk feature), high-risk-1 (age <5 years and high risk) and high-risk-2 (rest of the high-risk patients). The ALL-2000 protocol also included three high-risk subgroups, which were extra-intensive (high-risk-EI, any age and high-risk cytogenetics, poor early response, or WBC >200×109 l–1), very intensive group (high-risk-VI, age ≥5 years and CNS3, T-ALL, or WBC 100–200 × 109 l–1), and intensive group (high-risk I, rest of the high-risk patients).
2.3 Systemic chemotherapy
Both protocols had a three-drug induction (prednisolone at 60 mg/m2, four vincristine injections at 2.0 mg/m2, and two [ALL-2000] to four [ALL-92] doxorubicin infusions at 40 mg/m2) followed by a consolidation with alternating high-dose MTX (8 g/m2) and high-dose cytarabine (12 g/m2) and a delayed intensification.10 In addition, the ALL-2000 protocol had an early intensification phase (cyclophosphamide, 6-thioguanine, and low-dose cytarabine) before the consolidation. The maintenance therapy in the ALL-92 protocol consisted of oral 6-mercaptopurine and MTX combined with pulses of vincristine and prednisone. However, all VHR ALL-92 patients and all (N = 98) Finnish high-risk-1 and high-risk-2 ALL-92 patients (as part of a pilot cohort) were given LSA2L2 maintenance therapy throughout their maintenance therapy.17 The maintenance therapy in the ALL-2000 protocol (high-risk-I and high-risk-VI patients) included two cycles of LSA2L2 regimen (with cycling pulses of thioguanine plus cyclophosphamide, hydroxyurea plus daunorubicin, peroral methotreaxate plus carmustine, and cytrarabine plus vincristine) followed by per oral 6-mercaptopurine and MTX combined with pulses of vincristine and dexamethasone. The total duration of the therapy was 104 weeks in both protocols.10
2.4 CNS-directed therapy (prophylaxis and CNS3 therapy)
MTX was used in the IT prophylactic therapy. The cumulative number of the IT injections varied from eight (ALL-2000 high-risk-EI) to 17 (ALL-92 high-risk VHR). Patients with CNS3 were given additional IT triple chemotherapy in the induction until clearance of CNS blasts.
Patients older than 5 years with WBC 100 × 109 l–1 or more or T-cell immunophenotype with lymphomatous features (ALL-92 VHR and ALL-2000 high-risk-VI) received prophylactic cranial irradiation (Table 1).10 All patients less than 5 years of age and patients 5 years or older but with WBC less than 100 × 109 l–1 (ALL-92 high-risk-1 and high-risk-2, ALL-2000 high-risk-I) received no prophylactic CNS-RT, but instead two additional courses of both high-dose MTX and high-dose cytarabine. CNS3 patients treated on ALL-92 protocol were given craniospinal irradiation. In the ALL-2000 protocol, no irradiation was given to CNS3 patients less than 5 years of age, but cranial irradiation was given to the CNS3 patients aged at least 5 years.
| Prophylactic CNS-RT | Therapeutic CNS-RT | |||
|---|---|---|---|---|
| ALL-92 | ALL-2000 | ALL-2000 | ALL-2000 | |
| Risk features | Age ≥5 years and
|
Any age and
|
Any age, CNS3 | ≥5 years and CNS3 |
| CNS-RT dose | Cranial 18 Gy | Cranial 18 Gy | Cranial 24 Gy/spinal 12 Gy | Cranial 24 Gy |
- *High-risk features in these protocols were CNS3, WBC ≥50 × 109 l–1, T-cell immunophenotype, lymphomatous features, testicular leukemia, or slow response (day 15 marrow M3 and/or day 29 marrow ≥M2), high-risk cytogenetics, which were in ALL-92 trial t(9;22)(q34;q11), MLL rearrangements (11q23), (22q-), t(8;14)(q24;q32), t(2;8)(p12;q24), or t(8;22)(q24;q11), and in ALL-2000 trial t(9;22)(q34;q11), t(4;11)(q21;q23), t(1;19)(q23;p13.3), and hypodiploidy (modal chromosomal number <45).
- **Low hypodiploidy, <34 chromosomes.
- D, day; Gy, Gray.
The protocol time for CNS-RT was slightly different in the NOPHO ALL-92 and 2000 protocols, that is, days 308 and 259, respectively.
A major problem in this study was to address the issue of protocol adherence to the recommendations for CNS-RT. Thirteen patients received CNS-RT, although the protocol did not recommend it and 72 patients did not receive CNS-RT despite protocol recommendations (Supplementary Table S1). There were country-specific differences in the use of CNS-RT and individual interpretations of the recommendations. During the trial periods, the cumulative evidence for the adverse effects of CNS-RT made CNS-RT a less attractive treatment option for many clinicians. Among the patients included in the outcome analyses (n = 783), 110 underwent hematopoietic stem cell transplantation (HSCT) in first complete remission (CR1); three of them received CNS-RT before starting the conditioning process.
2.5 Statistical analyses
The analyses were performed based on the therapy given in each case. Baseline variables were compared between the two protocols using Fisher exact tests for categorical variables and the Mann–Whitney U-test for continuous variables. The Kaplan–Meier method was used for generating event-free (EFS) and overall survival (OS) estimates. Relapse, death in first complete remission (DCR1) and second malignancy (SMN) were classified as events. We chose the protocol recommendations as the landmark time in the Kaplan–Meier survival analyses. Accordingly, ALL-92 patients with any event occurring before 308 days and ALL-2000 patients before 259 days were excluded from the Kaplan–Meier analyses concerning the impact of irradiation. This adjusts for the overestimation of effect of CNS-RT on survival, since patients who die or have relapses before the landmark time would have a negative impact on the comparison group. Two-sided log-rank test was used for comparing patient groups in the Kaplan–Meier analyses with P values less than 0.05 considered statistically significant.
Fifty-two patients (including four CNS3 patients) did not reach complete remission by the end of induction. Thus, the final study population for the analyses of the role of CNS-RT consisted of the 783 high-risk-patients (including 52 CNS3 patients) who achieved CR1 by the end of induction (Fig. 1).
Poisson regression was utilized to model mortality and incidence rates. CNS-RT and HSCT in CR1 were included as discrete time-varying covariates. When the endpoints were relapse, DCR1 or SMN, competing risks regression was applied to estimate cumulative incidence and sub-hazard ratios. We observed a significant lack of proportionality of the hazard curves for mortality over time before and after irradiation. In all regression models, the standard errors of the regression coefficients were estimated by applying a cluster-robust estimator.18 To adjust for factors associated with outcome, we included age, immunophenotype, WBC at diagnosis, and cytogenetics in the regression models. Protocol was added to the final regression model to adjust for the differences in treatment and adherence to CNS-RT recommendations during the trial periods.
The cytogenetic analyses were not always successful and thus these data were incomplete. Accordingly, we divided the cytogenetic results into four groups representing patients with normal karyotype, favorable (t(12;21)(p12;q22), high hyperdiploidy with modal chromosomal number ≥50), unfavorable (MLL rearrangements (11q23), t(9;22) (q34;q11) or hypodiploidy), or undefined (missing/failed/other) togenetics.
3 RESULTS
3.1 Patient characteristics and outcome by CNS status
CNS3 was detected in 56 of 2,735 patients (2.0%) and, accordingly, in 56 of 835 high-risk patients (6.7%). The majority of the CNS3 patients (51.8%) were those with WBC below 50 × 109 l–1 (Table 2). No statistically significant differences were observed in the incidence of CNS3 among the high-risk patients when stratified by gender, age, or cytogenetics. Also, the proportion of patients with CNS3 was the same between pre-B and T-ALL, 36 of 549 (6.6%) and 18 of 256 (7.0%), respectively. Complete remission rate, OS, EFS, and cumulative incidence of relapse were similar in patients with or without CNS3 (Table 2). Induction failures occurred in four of the 56 CNS3 patients. Among the 15 CNS3 patients who relapsed, seven had a CNS-involving relapse. All of the CNS-involving relapses among the CNS3 patients were isolated CNS relapses, but only 22 of the 220 (10%) were isolated CNS relapses in the no central nervous system leukemia (CNS1-2) group.
| CNS1-2, n = 779 | CNS3, n = 56 | P value | |
|---|---|---|---|
| Age | NS | ||
| 1–4 years | 357 (46%) | 22 (39%) | |
| 5–9 years | 229 (29%) | 14 (25%) | |
| 10–14 years | 193 (25%) | 20 (36%) | |
| Gender | NS | ||
| Male | 481 (62%) | 34 (61%) | |
| Female | 298 (38%) | 22 (39%) | |
| WBC (x109 l–1) | 0.001 | ||
| ≤50.0 | 286 (37%) | 29 (52%) | |
| 50.1–100.0 | 240 (31%) | 5 (9%) | |
| 100.1–200.0 | 137 (17%) | 8 (14%) | |
| ≥200.1 | 116 (15%) | 14 (25%) | |
| Immunophenotype | NS | ||
| BCP | 513 (66%) | 36 (64%) | |
| T-ALL | 258 (33%) | 20 (36%) | |
| Unknown | 8 (1%) | 0 | |
| Cytogeneticsa | NS | ||
| Normal karyotype | 201 (26%) | 18 (32%) | |
| Favorable | 170 (22%) | 11 (20%) | |
| Unfavorable | 106 (13%) | 5 (9%) | |
| Other | 302 (39%) | 22 (39%) | |
| Primary events | NS | ||
| Induction failure | 20 (3%) | 4 (7%) | |
| Resistant disease | 28 (4%) | 0 | |
| CR1 | 479 (61%) | 34 (61%) | |
| Relapse | 220 (28%) | 15 (27%) | |
| DCR1 | 24 (3%) | 3 (5%) | |
| SMN | 8 (1%) | 0 | |
| Survival (±SE) | NS | ||
| 5-year EFS | 64.1% ± 1.7 | 60.6% ± 6.5 | |
| 10-year EFS | 63.0% ± 1.7 | 60.6% ± 6.5 | |
| 5-year OS | 76.7% ± 1.5 | 71.3% ± 6.1 | |
| 10-year OS | 74.4% ± 1.6 | 69.3% ± 6.2 |
- a Favorable: t(12;21)(p12;q22), high hyperdiploidy with modal chromosomal number ≥50; Unfavorable: t(9;22)(q34;q11), MLL rearrangements (11q23), hypodiploidy (modal chromosomal number <45); Other: Non-stratifying or non-specific cytogenetic aberrations and missing values.
- The CNS status was defined as CNS1, no leukocytes in CSF, CNS2, 1–5 mononuclear cells/μl of CSF, and CNS3, ≥5 mononuclear cells/μl of CSF. BCP, B-cell precursor.
3.2 The impact of irradiation on events
Of the 783 patients in CR1, 169 (22%) underwent CNS-RT (Table 3). The proportion of patients undergoing CNS-RT was higher during ALL-92 compared with ALL-2000, being 27% (118/439) versus 15% (51/344) (P < 0.001).
| Nonirradiated, n = 614 (78%) | Irradiated, n = 169 (22%) | P value | |
|---|---|---|---|
| Age | <0.001 | ||
| 1–4 years | 353 (58%) | 8 (5%) | |
| 5–9 years | 145 (24%) | 82 (48%) | |
| 10–14 years | 116 (19%) | 79 (47%) | |
| Gender | 0.043 | ||
| Male | 369 (60%) | 116 (69%) | |
| Female | 245 (40%) | 53 (31%) | |
| WBC (x109 l–1) | 0.001 | ||
| ≤50.0 | 216 (35%) | 77 (45%) | |
| 50.1–100.0 | 203 (33%) | 31 (18%) | |
| 100.1–200.0 | 102 (17%) | 39 (23%) | |
| ≥200.1 | 93 (15%) | 22 (14%) | |
| Immunophenotype | <0.001 | ||
| BCP | 457 (74%) | 63 (37%) | |
| T-ALL | 156 (25%) | 100 (59%) | |
| Unknown | 1 (0.2%) | 6 (4%) | |
| Cytogeneticsa | <0.001 | ||
| Normal karyotype | 136 (22%) | 66 (39%) | |
| Favorable | 155 (25%) | 19 (11%) | |
| Unfavorable | 97 (16%) | 7 (4%) | |
| Other | 231 (37%) | 77 (46%) | |
| CNS statusb | 0.096 | ||
| CNS1-2 | 578 (94%) | 153 (91%) | |
| CNS3 | 36 (6%) | 16 (9%) | |
| Treatment protocol | <0.001 | ||
| NOPHO ALL-92 | 321 (52%) | 118 (70%) | |
| NOPHO ALL-2000 | 293 (48%) | 51 (30%) | |
| HSCT in CR1 | <0.001 | ||
| Yes | 107 (17%) | 3 (2%) | |
| No | 507 (83%) | 166 (98%) | |
| Survival (±SE) | |||
| 5-year EFS (%) | 68.5% ± 2.1 | 78.0% ± 3.2 | 0.017 |
| 10-year EFS (%) | 67.0% ± 2.1 | 76.6% ± 3.3 | |
| 5-year OS (%) | 82.8% ± 1.7 | 83.9% ± 2.8 | NS |
| 10-year OS (%) | 79.3% ± 1.9 | 83.9% ± 2.8 |
- a Favorable: t(12;21)(p12;q22), high hyperdiploidy with modal chromosomal number ≥50; Unfavorable: t(9;22)(q34;q11), MLL rearrangements (11q23), hypodiploidy (modal chromosomal number <45); Other: nonstratifying or nonspecific cytogenetic aberrations and missing values.
- b CNS1, no leukocytes in CSF; CNS2, 1–5 mononuclear cells/μl of CSF, CNS3, ≥5 mononuclear cells/μl of CSF.
- A total of 783 patients were treated in NOPHO ALL-92 or NOPHO ALL-2000 trials. Patients with induction failure or resistant disease have been excluded (N = 52). BCP, B-cell precursor.
Nonadherence to the irradiation recommendations was observed (Supplementary Table S1). Of the 52 CNS3-patients in remission at the end of induction, only 16 underwent CNS-RT, all being at least 5 years old. Thirteen of the 16 CNS3-patients received the dose prescribed in the protocol, whereas three patients were irradiated with a reduced dose. Eight patients in the prophylactic irradiation group received irradiation at a higher dose than indicated in the protocol. Three patients who underwent HSCT in CR1 had received CNS-RT, all CNS1-2. Among the 36 patients who were not irradiated, 16 were 5 years or older, of whom six underwent HSCT in CR1.
Due to the protocol stratification, the irradiated patients were older and had more often T-ALL compared with the nonirradiated patients. Among the T-ALL patients, 101 of 256 (39.5%) received CNS-RT compared with 63 of the 520 (12.1%) pre-B ALL patients. Both patients with unfavorable and favorable cytogenetics were more numerous in the nonirradiated group (Table 3). This could be explained by the higher proportion of patients with unfavorable cytogenetics who underwent HSCT in CR1 instead of CNS-RT and the higher proportion of T-ALL (normally without stratifying cytogenetic aberrations) in the irradiated group.
In total, 40 events were observed among the 169 irradiated patients (37 relapses, two DCR1, and one SMN) and 230 events (198 relapses, 25 DCR1s, and seven SMN) among the 614 nonirradiated patients (Supplementary Table S2). Relapses occurred in six (37.5%) of the 16 patients with CNS3 status at diagnosis who received CNS-RT compared with nine (25.0%) of the 36 patients with CNS3 who did not receive CNS-RT (P = 0.358). Among the nonirradiated patients who did not undergo HSCT in CR1 (n = 507), 183 events occurred (167 relapses, 15 DCR1, and one SMN).
The EFS at 10 years was significantly higher in irradiated (76.6 ± 3.3%) than in the nonirradiated (67.0 ± 2.1) patients (P = 0.017) (Table 3). Since there was a statistically significant difference in the distribution of baseline characteristics between the two groups, the data were analyzed with adjusted regression models. The first regression model estimated the unadjusted hazard ratio (HR) for CNS-RT (crude), the second model included age (model A), and the third model included multiple covariates (model B) (Table 4). The annual risk of an event decreased by 29% in nonirradiated patients (crude). When the patient received irradiation, the risk of events decreased by additional 42% (HR 0.58, P < 0.05) in the age- and multivariable-adjusted models. Taking into account both the baseline risk and the protective effect of CNS-RT plus other baseline factors in model B, the annual risk for any event was 12% (= 0.42 × 0.29) in the irradiated group but 29% in the nonirradiated group. Other independent risk factors in model B were hyperleukocytosis (WBC ≥100 × 109 l–1) at diagnosis (HR 1.56, P < 0.001) and treatment according to the ALL-92 protocol (HR 1.29, P < 0.05). In an alternative model (not shown) only including patients 5 years or older (n = 384), CNS-RT was the only statistically significant factor, reducing the risk of adverse events by 65% (P < 0.05).
| OS (HRs) | EFS (HRs) | |||||
|---|---|---|---|---|---|---|
| Crude | A | B | Crude | A | B | |
| Irradiation | ||||||
| Baseline change per year | 0.79*** | 0.80*** | 0.80*** | 0.71** | 0.71** | 0.71*** |
| Direct impact of CNS-RT | 0.75 | 0.69 | 0.69 | 0.59* | 0.58* | 0.58* |
| HSCT in CR1 | 1.37 | 1.23 | 1.05 | 1.05 | 1.03 | 0.92 |
| Age | ||||||
| 5–9 years | 1.64** | 1.60* | 1.14 | 1.19 | ||
| >10 years | 1.69** | 1.59* | 1.02 | 1.06 | ||
| WBC ≥100 × 109 l–1 | 1.46* | 1.56*** | ||||
| Cytogeneticsa | ||||||
| Favorable | 0.74 | 1.05 | ||||
| Unfavorable | 1.64* | 1.39 | ||||
| Other | 1.30 | 1.31 | ||||
| Immunophenotype | ||||||
| T-ALL | 1.07 | 0.92 | ||||
| CNS3 | 1.18 | 1.11 | ||||
| NOPHO ALL-92 | 1.52* | 1.29* | ||||
- a Favorable: t(12;21)(p12;q22), high hyperdiploidy with modal chromosomal number ≥50; Unfavorable: t(9;22)(q34;q11), MLL rearrangements (11q23), hypodiploidy (modal chromosomal number <45); Other: nonstratifying or nonspecific cytogenetic aberrations and missing values.
- *P < 0.05; **P < 0.01; ***P < 0.001.
In the competing-risks analysis where relapse was the event of interest and DCR1 and SMN were the competing events, the risk of relapses was considerably lower in the irradiated group (Table 5). We estimated the sub-HRs with three separate models, all showing reduced risk for relapse in patients undergoing CNS-RT. In the age-adjusted model (model A), the sub-HR was 0.42 (P < 0.001) and in model B, where adjustments were made for multiple baseline factors, the sub-HR was 0.47 (P < 0.01). WBC 100 × 109 l–1 or higher at diagnosis (HR 1.68, P < 0.01) and cytogenetics other than favorable or unfavorable (HR 1.67, P < 0.05) were independent risk factors for relapse.
| Relapse1 | Isolated BM relapse2 | CNS-involving relapse3 | Isolated CNS relapse4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Crude | A | B | Crude | A | B | Crude | A | B | Crude | A | B | |
| CNS-RT | 0.49** | 0.42*** | 0.47** | 0.42*** | 0.39*** | 0.50* | 0.46* | 0.39* | 0.34** | 0.40 | 0.23* | 0.12** |
| HSCT in CR1 | 1.02 | 0.94 | 0.82 | 1.08 | 1.01 | 0.92 | 0.55 | 0.50* | 0.40* | 0.43 | 0.30 | 0.15* |
| Age | ||||||||||||
| 5–9 years | 1.32 | 1.44 | 1.22 | 1.40 | 1.32 | 1.37 | 3.53* | 3.99* | ||||
| >10 years | 1.36 | 1.40 | 1.25 | 1.38 | 1.39 | 1.44 | 3.87* | 4.06* | ||||
| WBC ≥100 × 109 l–1 | 1.68** | 1.41 | 1.85 | 2.63 | ||||||||
| Cytogeneticsa | ||||||||||||
| Favorable | 1.41 | 1.61 | 1.46 | 1.10 | ||||||||
| Unfavorable | 1.50 | 1.67 | 0.91 | 1.90 | ||||||||
| Other | 1.67* | 1.89* | 1.99* | 2.04 | ||||||||
| T-ALL | 0.70 | 0.47** | 1.39 | 1.88 | ||||||||
| CNS3 | 1.10 | 1.01 | 1.62 | 7.09*** | ||||||||
| NOPHO ALL-92 | 0.74 | 0.67 | 1.02 | 2.04 | ||||||||
- *P < 0.05; **P < 0.01; ***P < 0.001.
- Competing events: 1DCR1 and SMN; 2DCR1, SMN, combined, and isolated extramedullary relapses; 3DCR1, SMN, and non-CNS-involving relapses; 4DCR1, SMN, combined, and isolated BM relapses.
- a Favorable: t(12;21)(p12;q22), high hyperdiploidy with modal chromosomal number ≥50; Unfavorable: t(9;22)(q34;q11), MLL rearrangements (11q23), hypodiploidy (modal chromosomal number <45); Other: nonstratifying or nonspecific cytogenetic aberrations and missing values.
The risk of isolated BM relapses, CNS-involving relapses and isolated CNS relapses were significantly lower in the irradiated group compared with that in the nonirradiated group, sub-HRs 0.50 (P < 0.05), 0.34 (P < 0.01), and 0.12 (P < 0.01), respectively (Table 4). We observed a decreased risk of CNS-involving relapses (HR 0.40, P < 0.05) and isolated CNS relapses (HR 0.15, P < 0.05) among patients who underwent HSCT in CR1. Involvement of the CNS was a very strong independent risk factor for isolated CNS relapse (HR 7.09, P < 0.001). The favorable effect of CNS-RT on relapse rate persisted even in separate analyses of pre-B and T-ALL patients.
3.3 The impact of irradiation on OS
The OS estimated with the Kaplan–Meier method was similar in high-risk ALL patients with or without CNS-RT (10 year OS 79.3 ± 1.9 vs. 83.9 ± 2.8, P = n.s.) (Table 3). In the multivariable Poisson regression analysis, the risk of death decreased by 20% every year in the nonirradiated group during the follow-up time (baseline) (Table 4). The risk of death decreased by additional 36% (HR 0.64, P = n.s.), in the adjusted models, in patients who received CNS-RT, but the survival advantage was not statistically significant. Independent factors for death were age 5–10 years (HR 1.60, P < 0.05), age 10 years or older (HR 1.59, P < 0.05), hyperleukocytosis (HR 1.46, P < 0.05), unfavorable cytogenetics (HR 1.64, P < 0.05), and ALL-92 protocol treatment (HR 1.52, P < 0.05).
4 DISCUSSION
In this population-based study, we show that, although CNS involvement at diagnosis does not decrease OS, it still remains as an independent risk factor for isolated CNS relapse in children with high-risk ALL patients treated with modern ALL therapy. However, due to the low number of CNS3 patients who underwent CNS-RT in our study, we were unable to answer the question whether CNS-RT is beneficial for CNS3 patients. Despite systemic high-dose therapy including MTX and cytarabine, intensive IT therapy, and even CNS-RT prescribed to a subgroup of children over 5 years of age in the NOPHO protocols, the cumulative incidence of isolated CNS relapse was as high as 47% in CNS3 patients compared with 10% in the remaining patients. However, as CNS3 status was not a threat to OS, this finding challenges the role of permanently damaging therapeutic modalities in CR1, including irradiation, in ALL patients of all ages.
We observed that CNS-RT has a clear therapeutic effect in ALL. Better EFS was mainly a result of a reduced incidence of relapse. Importantly, CNS-RT did not increase the rate of SMN and DCR1 compared with the nonirradiated patients, although the follow-up time may be too short for detecting all types of secondary tumors, such as basal cell carcinoma, meningioma, and glioblastoma.
Better EFS did not result in increased OS in irradiated patients stratified to high-risk-therapy by WBC, cytogenetics, CNS3, or poor response to therapy. These data are supported by other studies.19, 20 In NOPHO, these data have resulted in omission of irradiation for all patients in CR1, including CNS3, and CNS-RT is reserved for those with a CNS-involving relapse.13 Even in subgroups, such as T-ALL with hyperleukocytosis, who have a CNS relapse rate of up to 10–20%, 80% patients will avoid CNS-RT with this approach.
The methods to compensate for the effect of CNS-RT in the ALL therapy have been IT and systemic chemotherapy. Traditionally, NOPHO protocols have included a substantial number of high-dose MTX courses,21, 22 high-dose cytarabine, and intensive IT chemotherapy, as was the case in the ALL-92 and ALL-2000 protocols. A meta-analysis of 47 randomized trials showed that CNS-RT resulted in better protection against CNS-involving relapse but showed no EFS advantage as compared with IT therapy, given that the IT therapy comprised of sufficient number of injections.20 In comparison with IV high-dose MTX (at 0.5–8 g/m²), CNS-RT reduced the CNS relapse rate but had less effect on non-CNS relapse resulting in similar EFS rate.20 In contrast, IT triples are better for preventing CNS relapses, but protocols with IT MTX have lower frequency of systemic relapses.20 The optimal combination of IT and systemic chemotherapy is still an elusive target. New agents, including liposomal cytarabine,23 with long-acting IT effect may contribute to better protection against CNS relapses. Data are still pending whether new diagnostic methods more sensitive than cytospin, such as flow cytometry, may help in stratifying patients to more intensive CNS-directed therapy and result in better CNS control in the long run.
A meta-analysis covering 28 studies from late 1980s to 2004, reported that ALL survivors who had undergone CNS-RT consistently experienced significant deficits in intellectual functioning, academic achievement, and specific neurocognitive abilities compared with control groups.24 In addition to the impairment of the neurocognitive achievements, the multiple long-term late effects in endocrine function25 and increased risk of secondary brain tumors26, 27 have led many other ALL study groups to avoid prophylactic CNS-RT to the developing brain or even therapeutic CNS-RT in CNS3 patients as well.
Protocol adherence to the recommendation for CNS-RT was a problem in this study. The negative attitude toward irradiation among clinicians was obvious judging from the variation in the interpretation of the protocol irradiation guidelines. Not all patients eligible for CNS-RT received irradiation according to the protocol and, interestingly, some received CNS-RT, although it was not recommended in the protocol. We analyzed the cohort on “as-treated” basis taking into account competing events and time-dependent factors and adjusted for potential confounders in an attempt to estimate the actual effect of CNS-RT on outcome. We chose regression analyses instead of stratified survival analyses, since the groups were unbalanced and adjustments for baseline factors were therefore necessary. Our study is population-based with a long follow-up time, only few patients were lost to follow-up, and we performed thorough annual review and registration of the follow-up data, all which are the strengths of this study. In our study settings, the protocol violations and the respective design were hard to compensate for, but with our statistical approach and adapted exclusions, we attempted to make the most correct assumptions from our results. Since the majority of the patients irradiated were over 5 years of age, our results can be best adapted to this age group.
In conclusion, CNS-RT, either therapeutic or prophylactic, decreases the overall frequency of relapses in high-risk ALL patients, with particularly beneficial effect on the CNS protection against relapse. This result was achieved without an increase in treatment-related mortality or second malignancies. However, CNS-RT did not result in survival advantage. Thus, in the current Nordic ALL-2008 protocol, CNS-RT has been omitted for all patients.
ACKNOWLEDGMENTS
This study was financially supported by the Foundation for Pediatric Research (MT) and by the Swedish Childhood Cancer fund (TO and MH).
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.