BMI and Cause-Specific Hospital Admissions and Costs: The UK Biobank Cohort Study
Abstract
Objective
To estimate the effect of BMI on cause-specific hospital admissions and costs in men and women is not well understood, and this study’s aim is to address this.
Methods
For 451,320 men and women aged 40 years or older recruited into the UK Biobank, followed up for 6 years on average, this study estimated annual rates and costs (at 2016 UK prices) of hospital admissions, overall and by diagnostic category (using International Classification of Diseases, Tenth Revision chapters), in relation to BMI.
Results
Among those who were never smokers, a 2-kg/m2 higher BMI (above 20 kg/m2) was associated with a 6.2% (99% CI: 5.3% to 7.2%) higher admission rate and an 8.6% (99% CI: 7.3% to 10.0%) higher annual cost in men and with a 5.7% (99% CI: 4.9% to 6.6%) higher admission rate and an 8.4% (99% CI: 7.5% to 9.3%) higher annual cost in women. Higher BMI was associated with higher admission rates and costs for many types of health conditions, particularly for endocrine, skin, and musculoskeletal disorders in both men and women and for circulatory diseases in men.
Conclusions
BMI beyond healthy weight is strongly associated with higher annual rates of hospital admission and higher costs in both men and women across a wide range of health conditions.
Study Importance
What is already known?
- ► Excess weight is associated with increased mortality, morbidity, and health care use.
- ► In women aged 50 years and older in the UK, musculoskeletal conditions are the largest single contributor to excess weight–related hospital costs.
- ► How associations between excess weight and cause-specific hospital admissions and costs differ in men and women is not well understood.
What does this study add?
- ► Higher BMI is associated with a higher rate of hospital admissions and higher annual hospital costs in both men and women overall and for many health conditions.
- ► In the UK, among people aged 40 to 79 years, around 16% of annual hospital costs in men and 19% in women are attributable to excess weight, with more than half incurred in people with BMI ≤ 35 kg/m2.
- ► Musculoskeletal conditions, particularly knee replacement due to osteoarthritis, account for about 40% of the costs attributable to excess weight in both men and women.
How might these results change the direction of research?
- ► These results could inform evaluations of interventions to reduce overweight and obesity and inform the decisions of health care policy makers, planners, and commissioners.
Introduction
The prevalence of overweight and obesity is a major public health concern in many countries ((1, 2)). Excess weight is associated with an increased risk of several chronic diseases, including coronary heart disease, stroke, type 2 diabetes, osteoarthritis, certain cancers, obstructive sleep apnea, and asthma, as well as increased mortality ((3-5)). In the United Kingdom (UK), more than 60% of adults now have overweight or obesity, and excess weight is estimated to account for 9% to 10% of disability-adjusted life years in the country ((6)).
Excess weight is also associated with higher hospital admission rates and costs ((7, 8)). Most studies have been based on data from US populations, and although there is some evidence that the associations between BMI and health care costs are stronger in middle-aged populations than in older populations, there is mixed evidence of differences by sex ((8)). Few of these studies have reported on the contributions of different conditions to health care costs attributable to excess weight, but among those that have, cardiovascular and musculoskeletal conditions were the largest contributors ((9-11)). It is, however, unclear how well these results translate to the UK, given the large differences in health care delivery and finance.
Few large studies have reported associations in UK populations ((8)). The largest UK study reported that, among 1 million middle-aged and older women, excess weight was associated with a substantially higher number of hospital admissions and substantially higher costs, overall and for a wide range of conditions, but this study presented no data from men or younger adults ((12)). Hospital costs were also found to be higher in people with a higher BMI among 500,000 men and women aged 40 years or older in the UK Biobank, but the authors did not assess the associations by population strata or for different health conditions ((13)).
Here, we use the UK Biobank, linked to routinely collected hospital data, to further examine cause-specific hospital admission rates and costs in relation to BMI; compare associations between men and women, by age, by smoking history, and across treated conditions; and project these findings to the wider UK population.
Methods
Study participants and data linkage
The study population was drawn from the UK Biobank, a prospective cohort of 500,000 adults from across England, Scotland, and Wales, aged 40 to 69 years at recruitment in 2006 to 2010. At recruitment, participants completed a detailed questionnaire and underwent physical measurements to provide data on demographic, behavioral, and physical characteristics. This included anthropometric and impedance measures, such as height and weight, from which BMI (in kilograms per meter squared) was calculated.
UK Biobank participants were linked to National Health Service (NHS) central registers for information on death and cancer registrations and to country-specific hospital admission records (Hospital Episode Statistics, Scottish Morbidity Records, and the Patient Episode Database for Wales) for information on inpatient and day-case admissions up to March 31, 2015. Linkage was performed by NHS number, postcode, sex, and age.
Costing hospital care
Hospital admission records provide data that include start and end dates (of constituent episodes), International Classification of Diseases, Tenth Revision (ICD-10) diagnostic codes, and Office for Population Censuses and Statistics Classification of Surgical Operations and Procedures, Fourth Revision procedural codes. Each episode of inpatient or day-case care (regular day or night admissions were excluded because of differences across data sources) was attached to one core health care resource group (HRG) and any number of additional unbundled HRGs, representing high-cost components of care. HRGs include clinically similar admissions requiring similar resources ((14, 15)). Costs at 2016 UK prices were then attached to the HRGs using NHS Reference Costs for 2015 to 2016, which provide the average cost of treating patients within a given HRG across different settings in England ((16)). Hospital episodes were deemed to be part of the same admission if they had overlapping durations.
Categorizing health conditions
To enable the breakdown of hospital costs and admissions by treated condition, the primary diagnosis of each admission was allocated to an ICD-10 chapter ((17)). ICD-10 chapters with relatively few admissions were combined into an “other” category (ICD-10 chapters 1, 5, 8, 15-17, and 20-22). Fractures (ICD-10 codes S02, S12, S22, S32, S42, S52, S62, S72, S82, S92, and T02) were extracted from ICD-10 chapter 19, with the remainder included in the “other” category. ICD-10 chapters representing neoplasms (chapter 2) and diseases or disorders of the circulatory (chapter 9), musculoskeletal (chapter 13), and genitourinary (chapter 14) systems were further subdivided into clinically distinct groups on the basis of primary diagnoses. Patients with osteoarthritis undergoing knee or hip replacement procedures were identified on the basis of ICD-10 and OPCS-4 code combinations specified by the National Joint Registry ((18)).
Statistical analysis
Participants were excluded from analysis if they had missing data on height and/or weight. Because of the small proportions of missing data, we also excluded participants with missing data on any explanatory variables, except for physical activity and education (see below). Participants with evidence of previous cancer, chronic obstructive pulmonary disease, or renal failure at recruitment were excluded because of concerns about reverse causality by preexisting disease. Exclusions were based on self-reported data in the UK Biobank and, for cancer, the presence of ICD-10 codes C00 to C97 (except C44, for nonmelanoma skin cancer) in the central cancer registry prior to recruitment. The first 2 years of follow-up after recruitment were also excluded for all participants to limit the potential impact of preexisting illness and residual confounding ((5)). All other UK Biobank participants contributed outcome data until the earliest of death, emigration, or the end of follow-up (March 31, 2015).
Annual hospital admissions and costs were analyzed with a generalized linear model with a log-link function and Poisson variance in relation to BMI as a categorical variable (in bands of <18.5, 18.5-19.9, 20-22.4, 22.5-24.9, 25-27.4, 27.5-29.9, 30-34.9, 35-39.9 and ≥40 kg/m2) and per 2-kg/m2 difference in BMI for BMIs > 20 kg/m2. Models were estimated separately in men and women, and according to smoking status (never a smoker, current smoker, or former smoker), with further adjustment for age group at the start of the annual period (<50, 50-54, 55-60, 60-64, or ≥65 years), ethnicity (white or nonwhite), region of recruitment (Scotland, Wales, or one of eight regions of England), cohort-specific fifths of the Townsend socioeconomic deprivation index ((19)), alcohol intake at recruitment (never or on special occasions, monthly to ≤2 times per week, or ≥3 times per week), highest educational qualification (no qualifications, secondary qualifications, or tertiary qualifications), frequency of vigorous physical activity (zero times per week, one to two times per week, and three to seven times per week), calendar year of follow-up, and the proportion of the annual period for which data were observed (some periods are not fully observed, e.g., because follow-up ended in the middle of an annual period). For analyses of current or former smokers, further adjustment was made for smoking history (current or former). For education and physical activity variables (2%-5% of data missing), missing values were assigned to a separate category. Cluster-robust SEs were estimated to account for lack of independence between admissions for a given individual across observation years. Standardized estimates of the mean annual admission rates and costs for each BMI category were derived using recycled predictions. SEs for these standardized estimates were generated from 1,000 bootstrap replicates.
Models were estimated for total annual admissions and costs and also by category of health condition, separately for men and women and by smoking status. For total annual costs, we also estimated these models in subgroups of participants defined by age (<60 or ≥60 years), country of recruitment (England, Scotland, or Wales), alcohol use (never, infrequently, or weekly), frequency of vigorous physical activity (never, one to two times per week, or three to seven times per week), by thirds of deprivation, and by highest educational qualification (no qualifications, secondary qualifications, or tertiary qualifications).
Sensitivity analyses estimated total annual costs with the following modifications to the model or inclusion/exclusion criteria: including all participants and all years of follow-up data (i.e., no exclusions); excluding those who reported being in poor health or who had a BMI > 50 kg/m2; and, using a two-part model for annual costs, with the first part, a logistic regression model, predicting whether any costs were incurred in the annual period (i.e., the patient was admitted to hospital) and the second part, a generalized linear model with gamma variance and log-link, modelling the number of costs conditional on any costs being incurred. This model explicitly accounts for the large proportion of observations with zero costs (i.e., no admissions in the annual period).
Hospital costs attributable to excess weight (BMI ≥ 25 kg/m2) were projected for all men and women aged 40 to 79 years in the UK, overall and for each diagnostic category. Differences in standardized mean costs between each overweight and obesity BMI category and BMI of 20 to <25 kg/m2 were calculated and then multiplied by the number of men and women aged 40 to 79 years in the UK in the respective BMI categories, by smoking status. The population distribution was estimated by applying the distribution of measured BMIs among men and women aged 40 to 79 years by smoking status in the Health Surveys for England from 2014 to 2016 ((20)) to the total population for the UK in 2016 ((21)).
All analyses were performed with R version 3.4.3 (R Foundation, Vienna, Austria) and Stata Software version 14.2 (College Station, Texas).
Patient and public involvement
This study was conducted using the UK Biobank resource. Details of patient and public involvement in the UK Biobank are available online (http://www.ukbiobank.ac.uk/about-biobank-uk/). No patients were involved in setting the research question or the outcome measures or in developing plans for recruitment, design, or implementation of this study. No patients were involved in the interpretation or write-up of results. There are no plans to disseminate the results of the research specifically to study participants, but the UK Biobank disseminates key findings from projects on its website.
Results
From the original cohort of 502,613 participants (273,452 women and 229,161 men), we excluded 3,105 (<1%) with missing data on height or weight, 3,565 (<1%) with missing data on other model covariates, 34,905 (7%) with preexisting cancer, 7,341 (2%) with preexisting chronic obstructive pulmonary disease, 717 (<1%) with renal failure, and 1,660 (<1%) who did not contribute data beyond 2 years after recruitment (Supporting Information Figure S1). The remaining 451,320 participants (243,366 women and 207,954 men) were followed up for an average of 4.2 years (4.2 women and 4.1 men), during which time they had 558,132 hospital admissions (290,648 women and 267,484 men) (Table 1). Among women, 37% had overweight (BMI 25 to <30 kg/m2) and a further 23% had obesity (BMI ≥ 30 kg/m2), whereas 50% of men had overweight and 25% had obesity. When compared with adults with healthy weight, men and women with obesity were less likely to be current drinkers, less likely to be in good/fair health, and more likely to be socially deprived or, for women but not men, a current or former smoker. Women were less likely to have ever smoked than men, and smoking rates were particularly high in men at lower BMIs.
| BMI at recruitment, kg/m2 | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <18.5 | 18.5-19.9 | 20-22.4 | 22.5-24.9 | 25-27.4 | 27.5-29.9 | 30-34.9 | 35-39.9 | ≥40 | ||||
| Women | ||||||||||||
| Number of participants | 1,782 | 6,506 | 33,292 | 55,706 | 52,208 | 37,081 | 37,831 | 13,176 | 5,784 | 243,366 | ||
| Mean BMI, kg/m2 | 17.7 | 19.4 | 21.4 | 23.8 | 26.2 | 28.7 | 32.1 | 37.0 | 43.9 | 27.0 | ||
| Mean age at recruitment, y (SD) | 54.9 (8.2) | 53.8 (8.2) | 54.3 (8.2) | 55.6 (8.0) | 56.6 (7.9) | 57.1 (7.9) | 56.8 (7.8) | 56.2 (7.8) | 55.0 (7.8) | 56.0 (8.0) | ||
| Deprivation in study population (%) | ||||||||||||
| Least deprived third | 33.5 | 33.4 | 36.2 | 37.1 | 35.2 | 32.7 | 29.4 | 25.7 | 20.5 | 33.6 | ||
| Most deprived third | 35.8 | 33.4 | 29.3 | 28.3 | 30.3 | 32.7 | 37.5 | 44.0 | 50.8 | 32.5 | ||
| Highest educational qualification (%) | ||||||||||||
| None | 10.2 | 8.5 | 9.9 | 13.0 | 16.5 | 19.5 | 21.0 | 21.8 | 20.6 | 16.1 | ||
| Secondary | 42.1 | 45.2 | 47.2 | 49.9 | 51.7 | 51.8 | 52.1 | 53.2 | 55.3 | 50.7 | ||
| Tertiary | 45.3 | 44.7 | 41.5 | 35.5 | 30.1 | 26.9 | 24.8 | 22.9 | 21.8 | 31.5 | ||
| Missing | 2.4 | 1.5 | 1.4 | 1.6 | 1.7 | 1.8 | 2.0 | 2.1 | 2.3 | 1.7 | ||
| Frequency of vigorous physical activity (%) | ||||||||||||
| 0 times/wk | 38.0 | 34.7 | 31.5 | 32.5 | 36.4 | 39.5 | 43.5 | 48.5 | 54.0 | 37.4 | ||
| 1-2 times/wk | 27.2 | 30.2 | 31.7 | 31.8 | 30.1 | 27.8 | 25.8 | 23.0 | 19.6 | 29.0 | ||
| 3-7 times/wk | 29.5 | 31.3 | 33.3 | 31.5 | 28.4 | 26.1 | 22.8 | 19.5 | 16.5 | 27.9 | ||
| Missing | 5.3 | 3.8 | 3.5 | 4.2 | 5.2 | 6.6 | 7.9 | 9.1 | 9.9 | 5.6 | ||
| Smoking status (%) | ||||||||||||
| Never | 64.3 | 65.4 | 63.0 | 61.2 | 60.0 | 58.6 | 59.5 | 59.0 | 58.5 | 60.5 | ||
| Former | 20.9 | 23.6 | 27.6 | 30.3 | 31.5 | 32.9 | 32.3 | 33.4 | 33.2 | 30.9 | ||
| Current | 14.9 | 11.0 | 9.4 | 8.5 | 8.5 | 8.5 | 8.2 | 7.7 | 8.2 | 8.6 | ||
| Current alcohol drinker (%) | 68.7 | 77.8 | 81.4 | 81.6 | 78.3 | 74.6 | 69.1 | 61.1 | 52.5 | 75.9 | ||
| Good/fair health (%) | 78.7 | 85.1 | 87.7 | 86.4 | 82.3 | 76.6 | 66.9 | 54.7 | 40.5 | 78.3 | ||
| Person years of follow-up a | 7,373 | 26,993 | 138,151 | 231,840 | 217,169 | 154,569 | 157,131 | 54,636 | 24,067 | 1,011,932 | ||
| Total number of admissions a | 1,821 | 6,097 | 30,409 | 56,242 | 60,502 | 47,655 | 53,922 | 22,339 | 11,661 | 290,648 | ||
| Men | ||||||||||||
| Number of participants | 425 | 1,604 | 12,483 | 37,923 | 56,308 | 46,790 | 40,696 | 9,023 | 2,702 | 207,954 | ||
| Mean BMI, kg/m2 | 17.7 | 19.4 | 21.6 | 23.9 | 26.3 | 28.7 | 31.9 | 36.9 | 43.6 | 27.8 | ||
| Mean age at recruitment, y (SD) | 54.7 (8.1) | 55.0 (8.5) | 55.5 (8.4) | 56.0 (8.3) | 56.5 (8.2) | 56.7 (8.2) | 56.7 (8.0) | 56.4 (7.9) | 55.3 (7.6) | 56.4 (8.2) | ||
| Deprivation tertile in study population (%) | ||||||||||||
| Least deprived third | 18.8 | 24.7 | 31.7 | 35.9 | 36.1 | 34.8 | 31.5 | 26.6 | 21.6 | 33.9 | ||
| Most deprived third | 59.3 | 47.9 | 37.2 | 31.3 | 30.3 | 31.6 | 35.4 | 41.8 | 49.9 | 33.1 | ||
| Highest educational qualification (%) | ||||||||||||
| None | 21.6 | 15.6 | 11.6 | 12.4 | 14.7 | 17.4 | 20.4 | 22.7 | 23.5 | 16.3 | ||
| Secondary | 41.4 | 41.2 | 40.4 | 43.7 | 47.0 | 49.8 | 51.4 | 51.8 | 53.7 | 47.7 | ||
| Tertiary | 34.6 | 41.0 | 46.3 | 42.2 | 36.6 | 31.0 | 26.2 | 23.4 | 21.1 | 34.2 | ||
| Missing | 2.4 | 2.1 | 1.8 | 1.7 | 1.7 | 1.8 | 2.0 | 2.2 | 1.7 | 1.8 | ||
| Frequency of vigorous physical activity (%) | ||||||||||||
| 0 times/wk | 42.1 | 34.1 | 28.4 | 26.8 | 28.8 | 32.2 | 37.1 | 44.1 | 51.7 | 31.8 | ||
| 1-2 times/wk | 21.9 | 24.8 | 28.7 | 29.9 | 30.4 | 28.2 | 26.4 | 22.6 | 19.9 | 28.4 | ||
| 3-7 times/wk | 27.1 | 34.5 | 39.2 | 39.9 | 37.2 | 35.2 | 31.1 | 26.9 | 20.9 | 35.5 | ||
| Missing | 8.9 | 6.6 | 3.7 | 3.4 | 3.6 | 4.4 | 5.4 | 6.5 | 7.5 | 4.3 | ||
| Smoking status (%) | ||||||||||||
| Never | 44.7 | 52.7 | 56.7 | 55.8 | 51.6 | 47.8 | 44.2 | 43.0 | 44.7 | 49.9 | ||
| Former | 16.2 | 18.6 | 25.6 | 31.2 | 36.8 | 40.7 | 44.5 | 45.8 | 44.1 | 37.8 | ||
| Current | 39.1 | 28.6 | 17.7 | 13.0 | 11.6 | 11.5 | 11.3 | 11.2 | 11.2 | 12.3 | ||
| Current alcohol drinker (%) | 76.7 | 76.7 | 84.4 | 87.5 | 88.5 | 87.6 | 85.5 | 81.8 | 73.3 | 86.7 | ||
| Good/fair health | 62.2 | 72.0 | 80.8 | 83.0 | 80.2 | 73.9 | 61.7 | 46.0 | 29.2 | 73.5 | ||
| Person years of follow-up a | 1,720 | 6,580 | 51,687 | 157,509 | 233,448 | 193,972 | 168,381 | 37,361 | 11,130 | 861,791 | ||
| Total number of admissions a | 558 | 2,014 | 13,519 | 40,210 | 67,384 | 61,197 | 61,488 | 15,771 | 5,343 | 267,484 | ||
- a Excluding the first 2 years of follow-up.
Annual rates of hospital admissions and costs tended to be higher at all levels of BMI in men compared with women, particularly among current or former smokers. However, percentage differences in cost compared with those at healthy weight tended to be lower in men than women (Table 2, Figure 1; Supporting Information Table S1). Among those who had never smoked, rates of hospital admissions rose steadily from 214 admissions per 1,000 person years (99% CI: 200 to 227) at an average annual cost of £326 per person (99% CI: £304 to £348) among women with BMIs from 20 to 22.5 kg/m2 to 392 admissions per 1,000 person years (99% CI: 358 to 427) at an average annual cost of £779 per person (99% CI: £695 to £862) among women with BMIs in excess of 40 kg/m2. Among men who had never smoked, rates of hospital admissions rose from 212 per 1,000 person years (99% CI: 191 to 232) at a cost of £367 per person (99% CI: £328 to £407) among those with a BMI from 20 to 22.5 kg/m2 to 376 admissions per 1,000 person years (99% CI: 326 to 427) at an average cost of £805 per person (99% CI: £641 to £969) among those with BMIs in excess of 40 kg/m2. A 2-kg/m2 higher BMI (above 20 kg/m2) was associated with increases in the admission rate of 6.2% (99% CI: 5.3% to 7.2%) and 5.7% (99% CI: 4.9% to 6.6%) and increases in annual costs of 8.6% (99% CI: 7.3% to 10.0%) and 8.4% (99% CI: 7.5% to 9.3%) in never-smoking men and women, respectively. In both men and women, annual admission rates and costs were substantially elevated in underweight participants (BMI <18.5 kg/m2), but CI were very wide.
| BMI, kg/m2 | Never smoked | Current or former smokers | ||
|---|---|---|---|---|
| Mean annual cost, £ (99% CI) | Mean excess cost, % (99% CI) | Mean annual cost, £ (99% CI) | Mean excess cost, % (99% CI) | |
| Women | ||||
| <18.5 | 408 (272 to 543) | 25.0 (−10.9 to 75.2) | 447 (281 to 613) | 1.2 (−31.0 to 48.5) |
| 18.5-19.9 | 315 (271 to 359) | −3.3 (−16.6 to 12.1) | 493 (410 to 576) | 11.7 (−6.9 to 34.1) |
| 20-22.4 | 326 (304 to 348) | reference | 441 (407 to 476) | reference |
| 22.5-24.9 | 361 (342 to 380) | 10.6 (2.3 to 19.7) | 458 (430 to 485) | 3.7 (−5.5 to 13.6) |
| 25-27.4 | 375 (356 to 394) | 15.0 (6.3 to 24.3) | 518 (486 to 550) | 17.3 (7.0 to 28.6) |
| 27.5-29.9 | 430 (405 to 456) | 31.9 (21.5 to 43.1) | 540 (506 to 574) | 22.4 (11.2 to 34.7) |
| 30-34.9 | 498 (472 to 525) | 52.8 (41.1 to 65.4) | 598 (564 to 633) | 35.5 (23.7 to 48.5) |
| 35-39.9 | 616 (566 to 665) | 88.8 (70.6 to 108.9) | 720 (653 to 787) | 63.2 (45.4 to 83.1) |
| ≥40 | 779 (695 to 862) | 138.8 (110.8 to 170.5) | 891 (791 to 991) | 101.9 (76.2 to 131.3) |
| Trend a | — | 8.4 (7.5, 9.3) | — | 6.6 (5.6, 7.5) |
| Men | ||||
| <18.5 | 439 (140 to 738) | 19.4 (−36.0 to 123.0) | 1,283 (654 to 1,912) | 102.7 (24.3 to 230.5) |
| 18.5-19.9 | 342 (218 to 466) | −7.0 (−34.7 to 32.6) | 744 (558 to 929) | 17.5 (−10.8 to 54.7) |
| 20-22.4 | 367 (328 to 407) | reference | 633 (563 to 703) | reference |
| 22.5-24.9 | 374 (347 to 401) | 1.9 (−10.0 to 15.4) | 553 (513 to 593) | −12.6 (−22.8 to −1.1) |
| 25-27.4 | 397 (374 to 421) | 8.2 (−3.7 to 21.5) | 604 (570 to 637) | −4.6 (−15.0 to 7.0) |
| 27.5-29.9 | 441 (414 to 469) | 20.2 (6.8 to 35.2) | 627 (593 to 660) | −1.0 (−11.7 to 10.9) |
| 30-34.9 | 541 (506 to 575) | 47.1 (30.3 to 66.1) | 735 (695 to 775) | 16.1 (3.6 to 30.1) |
| 35-39.9 | 650 (568 to 732) | 76.9 (50.8 to 107.6) | 888 (807 to 968) | 40.3 (22.4 to 60.7) |
| ≥40 | 805 (641 to 969) | 119.1 (74.4 to 175.2) | 1,091 (921 to 1,262) | 72.4 (43.3 to 107.5) |
| Trend a | — | 8.6 (7.3,10.0) | — | 6.7 (5.5, 7.8) |
- Relative effects adjusted for age, ethnicity, region of recruitment, socioeconomic status, alcohol intake, education, physical activity, calendar year, proportion of annual period for which data were observed, and, when applicable, smoking status. Absolute values standardized according to these characteristics among UK Biobank participants contributing data to analysis.
- a Percentage difference in outcomes for each 2-kg/m2 higher BM above 20 kg/m2.
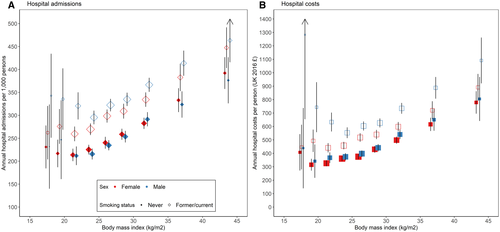
Annual admissions and costs were higher at all levels of BMI for both men and women who were current or former smokers compared with those who had never smoked. Among women with a history of smoking, annual admissions and costs were also lowest at a BMI of 20 to <22.5 kg/m2. However, relative increases in annual admissions and costs with higher BMI were smaller than in those who had never smoked. For instance, among women, a 2-kg/m2 higher BMI (above 20 kg/m2) was associated with 8.4% (99% CI: 7.5% to 9.3%) higher annual costs in those who had never smoked versus 6.6% (99% CI: 5.6% to 7.5%) in current or former smokers. Among men with a history of smoking, annual admissions and costs were lowest in those with a BMI of 22.5 to <25 kg/m2 and were not elevated among men with overweight. A 2-kg/m2 higher BMI (above 20 kg/m2) was associated with 8.6% (99% CI: 7.3% to 10.0%) higher annual costs in those who had never smoked versus 6.7% (99% CI: 5.5% to 7.8%) in current or former smokers.
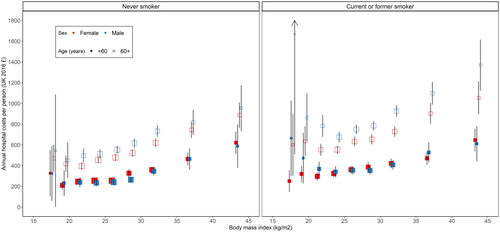
Annual hospital admissions and costs were higher in older individuals (age >60 vs. ≤60 years) at all levels of BMI and greater at higher BMIs beyond healthy weight in both age groups (Figure 2; Supporting Information Tables S2-S3). In both men and women, the percentage increase in rates of admission and costs tended to be lower in older adults, and there was statistical evidence of heterogeneity by age in differences in annual costs per unit increase in BMI among adults who had never smoked (Supporting Information Figures S2-S3). There was no evidence of heterogeneity in estimates of percentage differences in annual costs by country of recruitment, frequency of alcohol use, or tertile of deprivation, regardless of smoking history or sex.
Associations between BMI and annual costs were similar when excluding individuals with BMIs of 50 kg/m2 or greater or when using a two-part log-gamma generalized linear model for estimation (Supporting Information Table S4). Associations between BMI and annual costs were marginally lower among women who had never smoked when including all individuals, regardless of disease history at recruitment and data from all years of follow-up. Among women, but not men, who self-reported their health as poor, associations between higher levels of BMI and annual costs were weaker. Among both men and women who had never smoked, there was no association between having underweight and having elevated hospital costs in those reporting their health as good or fair.
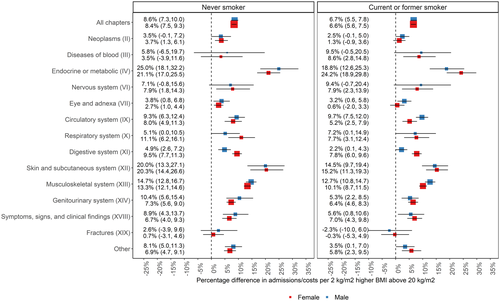
The annual hospital admission rates and costs were greater at higher BMIs in most categories of health conditions, with estimates being similar in men and women (Figure 3). The largest differences by sex were for diseases of the digestive system (ICD-10 chapter 11) and, for those who had never smoked only, respiratory conditions (ICD-10 chapter 10), for which associations were stronger in women than in men. The strongest increases in annual costs per 2-kg/m2 higher BMI (above 20 kg/m2) were for endocrine, metabolic, and nutritional disorders (ICD-10 chapter 4), musculoskeletal conditions (ICD-10 chapter 13), diseases of the circulatory system (ICD-10 chapter 9), and diseases of the skin and subcutaneous tissue (ICD-10 chapter 12), largely due to elevated rates of cellulitis.
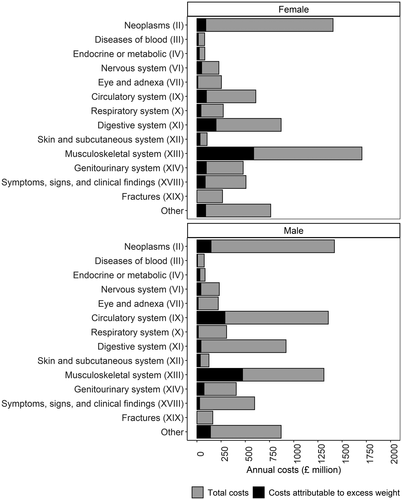
Per person estimates of annual admissions and costs were projected to all 15.2 million women and 14.5 million men aged 40 to 79 years in the UK in 2016 (Supporting Information Table S5). Total annual hospital admission costs for this age group were estimated to be £7.6 billion in women and £8.1 billion in men, of which £1.4 billion (or 18.7%; 99% CI: 16.4% to 20.9%) in women and £1.3 billion (or 16.3%; 99% CI: 13.3% to 19.3%) in men was attributable to excess weight (Supporting Information Table S6, Supporting Information Figure S4). The proportion of costs attributable to excess weight was higher at a higher BMI in both men and women, with over half of costs in people with BMIs of 40 kg/m2 or higher attributed to their weight. However, at the population level, 56% and 65% of all excess weight–attributable costs in women and men, respectively, were incurred in those with BMIs < 35 kg/m2.
Musculoskeletal conditions were the biggest contributors to total excess weight–attributable costs in both men and women, accounting for 41.3% (99% CI: 36.5% to 46.1%) and 35.5% (99% CI: 29.2% to 41.8%) of the total hospital admission costs in women and men, respectively (Figure 4; Supporting Information Table S7). Treatments for osteoarthritis accounted for 79% of total excess weight–attributable costs for musculoskeletal conditions in women and accounted for 82% in men, with knee replacement surgery due to osteoarthritis alone accounting for 39% of these attributable costs in women and 38% in men (Supporting Information Table S8). Circulatory-system conditions accounted for 6.9% (99% CI: 3.6% to 10.2%) of total excess weight–attributable costs in women and 21.8% (99% CI: 15.4% to 28.2%) in men. In men, 61% of these excess costs were due to coronary heart disease. Diseases of the digestive system accounted for 14.0% (99% CI: 11.1% to 16.8%) of all excess weight–attributable costs in women (of which 65% related to diseases of the gallbladder, biliary tract, and pancreas) and accounted for 3.2% (99% CI: 0.0% to 7.3%) in men. Neoplasms accounted for 6.5% (99% CI: 1.0% to 12.0%) of total excess weight–attributable costs in women (of which 68% related to cancers of the breast) and accounted for 11.0% (99% CI: 3.4% to 18.7%) in men (of which 55% related to cancers of the digestive system).
Discussion
Statement of principal findings
In a large cohort of middle-aged and older adults in the UK, we found that annual rates of hospital admissions and annual costs were elevated in men and women who had overweight or obesity, overall and for many categories of treated health conditions. There were 5.7% and 6.2% higher admission rates and 8.4% and 8.6% higher costs per 2-kg/m2 higher BMI (beyond 20 kg/m2) for women and men, respectively, who had never smoked. The strongest associations with annual costs were observed for endocrine (including diabetes), skin, and musculoskeletal disorders in both men and women and for circulatory conditions in men. We estimated that 19% of annual hospital costs in women aged 40 to 79 years and 16% in men could be attributed to excess weight, with treatments for osteoarthritis and diseases of the heart and digestive system contributing most to these excess costs.
Comparison with other studies
These associations between BMI and annual costs are broadly consistent with other large and high-quality studies from the UK and elsewhere ((8, 11-13, 22)). Based on the same cohort, Dixon et al. ((13)) reported that a 2-kg/m2 higher BMI was associated with an approximately 5.9% higher cost across the entire BMI range. Similarly, using data on over 1 million women aged 55 to 79 years in England, Kent et al. ((12)) reported that every additional 2 kg/m2 above 20 kg/m2 was associated with 7.7% higher costs, which compares with 8.4% higher costs in the present study. These small differences are likely to reflect the exclusion of adults by smoking history and the slightly younger population in the present study, with weaker associations observed between BMI and hospital admissions and costs among current or former smokers and among older adults.
We observed some differences in associations between BMI and hospital admissions and costs by sex, age, and smoking history. For BMIs above 20 kg/m2, the average difference in admissions and costs per additional unit of BMI was similar in men and women. Relative increases in hospital admissions and costs were smaller in current or former smokers compared with those who had never smoked and in older versus younger adults. A systematic literature review of individual-participant data studies reported stronger associations of obesity with total health care costs in women compared with men and in middle-aged versus older adults ((8)). Few large studies have compared the relationship between BMI and hospital costs by sex and age or separately in those who have never smoked versus current or former smokers. Korda et al. ((11)) reported rates of hospital admissions and costs by BMI by age and sex groups using data on 225,000 adults aged 45 years or older from Australia. They reported comparable associations between BMI and annual hospital admissions and costs in men and women aged 45 years or older in Australia. Consistent with our findings, they also reported stronger associations in adults aged 45 to 64 years than in adults aged 65 to 79 years. More generally, the differences in associations by age and smoking status, reported in the present study, are consistent with associations reported between BMI and mortality and may be a consequence of reverse causality due to higher rates of morbidities in smokers and older adults or may result from the higher background risk of events across all BMI categories ((5)). Differences by age group may also result from changes to body composition in older adults, who tend to have less fat-free mass ((23)).
We estimated that 19% of the annual hospital costs of women and 16% of the annual hospital costs of men aged 40 to 79 years in the UK were attributable to excess weight. In the somewhat older Million Women Study population, aged 55 to 79 years, it was projected that 16% of the annual hospital costs of women were attributable to excess weight ((12)), a difference consistent with the stronger associations between BMI and annual costs in younger adults. Among adults aged 45 years or older in Australia, Korda et al. ((11)) reported that 17% of annual costs were attributable to excess weight.
The composition of total excess weight–attributable costs by categories of health conditions in this study was also similar to that reported in the Million Women Study ((12)), with musculoskeletal conditions accounting for around 35% to 40% of the total attributable costs, largely reflecting knee replacements for adults with osteoarthritis. Circulatory-system disorders were the second largest contributor to excess weight–attributable costs in men, accounting for about 22% of the total, albeit they accounted for only 7% in women. Previous studies using data from the US workforce have reported that musculoskeletal and circulatory conditions each contribute between 20% to 30% to total excess weight–attributable costs ((9, 10)).
Strengths and weaknesses of the study
The approach to defining diagnostic categories using ICD-10 chapters based on the ICD-10 codes of the primary diagnosis at admission follows closely the approach taken to describe hospital activity and spending by NHS England ((24)), which increases its value to health care planners and commissioners. However, with this method, the full contribution of underlying health conditions, like type 2 diabetes, is not fully reflected, because admissions caused by diabetes will often be ascribed to the actual complication treated (e.g., myocardial infarction).
Around 5% of people invited to participate in the UK Biobank study did so, and those who participated were less likely to have obesity, to smoke, to be socioeconomically deprived, to drink alcohol regularly, or to have existing medical conditions than the general population, and they experienced a lower rate of mortality ((25)). Absolute costs are likely to be lower than in the comparable general population, thereby potentially limiting the generalizability of the findings to the wider UK population. However, these results go further than previous research in that they apply to a population of both sexes and to a broader age range. UK Biobank also estimated BMI from measured rather than self-reported height and weight, which was used in the Million Women Study.
Our findings are based on observational data, and although we sought to minimize bias by excluding individuals with health conditions that could affect weight at recruitment and early years of follow-up, as well as stratifying by smoking history ((5)), residual biases and confounding in the associations may remain. The use of the associations reported in the present study in comparative evaluations of, for example, cost-effectiveness of weight-reducing interventions, will benefit from further corroboration of causality from, for example, intervention effects on health outcomes. Future work could consider use of information on genetic variation in BMI as an instrument to investigate further the causal effects of BMI on hospital admissions and costs. Wehby et al. ((26)), for example, reported that greater genetic predisposition to obesity was associated with higher annual Medicare expenditure, reporting that a 1-SD higher polygenic risk score (corresponding to a 2.5-kg/m2 higher BMI) was associated with 15% higher mean annual hospital costs, more than twice the association reported in the present study.
Conclusion
In this large prospective cohort study of adult men and women in the UK, we reported robust evidence of graded associations between higher BMI and higher hospital admission rates and costs, overall and for a large range of health conditions. These results could inform evaluations of the impacts on hospital costs of interventions to reduce overweight and obesity and could inform the decisions of health care policy makers, planners, and commissioners.
Funding agencies
BM and SK are supported by the Oxford National Institute for Health Research (NIHR) Biomedical Research Centre (BRC). BRC funded access to the UK Biobank data. The views expressed are those of the authors and not necessarily those of the NHS, NIHR, or the Department of Health. BC is supported by a Nuffield Department of Population Health Senior Research Fellowship. The University of Oxford Medical Research Council (MRC) Population Health Research Unit is funded through a strategic partnership between the MRC and the University of Oxford. The funders had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Disclosure
The authors declared no conflicts of interest.
Author contributions
All authors were involved in the design of the study and interpretation of the findings. SK and RO undertook the data analysis and drafted the manuscript.





