Early Infant Feeding and BMI Trajectories in the First 5 Years of Life
Abstract
Objective
This study examined the relative impact of breastfeeding duration and timing of solids introduction on BMI z score (BMIz) trajectory in early childhood.
Methods
This study conducted secondary analyses of data from the Melbourne Infant Feeding, Activity and Nutrition Trial (InFANT) Program (N = 542), a prospective cohort study with data collected at birth and 3, 9, 18, 42, and 60 months. Linear spline multilevel models were performed.
Results
Differential growth rates were observed from birth to 3 months and from 9 to 18 months by breastfeeding duration (≥ 6 vs. < 6 months) and timing of solids introduction (before vs. after 6 months). Children who were breastfed for ≥ 6 versus < 6 months had lower BMIz at all ages from 3 to 60 months. The difference remained after adjusting for child and maternal factors, and the adjusted mean differences in BMIz at 3, 9, 18, 42, and 60 months were −0.34, −0.44, −0.13, −0.19, and −0.23, respectively. Children who received solids before versus after 6 months of age had higher BMIz at 18 and 42 months, but adjustment for child and maternal factors attenuated these differences.
Conclusions
Longer breastfeeding duration was associated with lower BMIz to 5 years of age, providing further support for infant feeding guidelines to prolong breastfeeding duration for healthy growth.
Study Importance
What is already known?
- Longer breastfeeding duration may protect against subsequent obesity.
- Early introduction of solids may increase subsequent obesity risk.
- The relative impact of breastfeeding duration and the timing of solids introduction on obesity development in children remains unclear.
What does this study add?
- Breastfeeding duration and the timing of solids introduction are independently associated with BMIz trajectories from birth to 5 years.
- Breastfeeding duration ≥6 months is associated with lower BMIz as early as 3 months of age and this association remains evident until age 5 years.
- Children who introduced solids before versus after 6 months showed differences in period-specific growth rates, but no difference was found for BMIz at 5 years.
Introduction
The increasing prevalence of childhood overweight and obesity is a global health concern (1). Childhood obesity tracks through the life course and is associated with substantial health and psychosocial consequences later in adulthood (1). The 2017 World Health Organization Commission on Ending Childhood Obesity indicated that the progress in combating childhood obesity has been slow and inconsistent, highlighting the importance of identifying key areas for prevention (1). Contemporary research has highlighted that opportunities for obesity prevention may relate to the potential role of infant feeding on growth across early childhood (2). A growing body of evidence has suggested that breastfeeding protects against subsequent obesity (3). In addition, emerging evidence has indicated that early introduction of solid foods is associated with greater obesity risk (4). It is likely that early introduction of solids might interfere with breastfeeding intensity and lead to earlier breastfeeding termination (5). Whether there is an independent or interaction effect of breastfeeding duration and timing of solids introduction on obesity remains unclear (5).
Most existing evidence on the impact of early feeding on obesity has come from observational studies, and findings have been inconsistent, possibly because of large variations in study design (6, 7). Moreover, the majority of studies on this topic have examined how early infant feeding impacts later obesity outcomes at just one time point (8). Only a few studies have examined the relationship between infant feeding and subsequent BMI z score (BMIz) growth trajectories (9, 10). Studying growth trajectories is imperative to facilitate the understanding of critical windows during which the relationship emerges or the exposure is most predictive of the outcome (11). Such information can be valuable for guiding obesity prevention interventions and contributing to the evidence base for infant feeding guidelines. The Australian Infant Feeding Guidelines encourage exclusive breastfeeding until 6 months of age, continued breastfeeding until 1 year of age and beyond, and offering of solids at around 6 months of age (12). This study aimed to investigate the relative impact of breastfeeding duration and timing of solid foods introduction on BMIz trajectories across the first 5 years of life among a cohort of Australian young children.
Methods
Study design and participants
We conducted a secondary analysis of longitudinal data extracted from the Melbourne Infant Feeding, Activity and Nutrition Trial (InFANT) Program, a 15-month, parent-focused randomized controlled trial that aimed to reduce infant obesity risk behaviors from ages 3 to 18 months with additional follow-up until age 5 years to test the sustainability of intervention effects. The program was registered with Current Controlled Trials (identifier ISRCTN81847050). A total of 542 families participated in the study at baseline, when children were approximately 3 months old (T1), and they were followed up when the child’s mean age was around 9 (T2), 18 (T3), 42 (T4), and 60 months (T5). Detailed study protocol and follow-up outcomes were reported elsewhere (13-15).
Anthropometric measures
Parents reported children’s birth length and weight. Trained staff measured children’s length/height and weight at each time point from T1 to T5. Length/height was measured to the nearest 0.1 cm using a calibrated measuring mat or portable stadiometer. Weight (in light clothes) was measured to the nearest 10 g using calibrated digital scales. Length/height and weight were measured twice, and the average was used for analysis. BMIz was calculated using World Health Organization sex-specific growth charts (16).
Breastfeeding duration
The study collected information on any breastfeeding, including both feeding directly from the breast and bottle feeding of pumped breast milk. At 3, 9, and 18 months, parents were asked, “How long did you breastfeed your child?” and given three response options: “never breastfed,” “still breastfeeding,” and “stopped breastfeeding”; additionally, parents were asked an open question: “Age of the baby in months and in weeks when you stopped breastfeeding.” Breastfeeding duration was obtained by combining responses to all breastfeeding-related questions and was analyzed as a binary variable (< 6 and ≥ 6 months) in the primary analyses to allow assessment of the relative impact on BMIz trajectories with timing of solids introduction (before vs. after 6 months). Additional analyses by breastfeeding duration (< 3 vs. ≥ 3 months) were also conducted.
Timing of solids introduction
The timing of solids introduction was assessed using questions at 3 and 9 months. “Solids” are defined as foods of appropriate texture moving from pureed to lumpy to normal texture during a 6- to 12-month period, excluding water, fruit juice, and other fluids (12). At 3 months, mothers were asked, “Have you started to give your baby solids (foods other than milk)?” and given the response options “yes” or “no.” At both 3 and 9 months, parents were asked an open question: “How old was your baby in months and in weeks when you started giving them solids?” The timing of solids introduction was analyzed as a binary variable: child introduced to solids before 6 months of age (< 6 months) versus at or after 6 months of age (≥ 6 months). Six months was used as a cutoff informed by the Australian Infant Feeding Guidelines to delay introduction of solids until around age 6 months (12). A 4-month cutoff was considered but was not feasible because of a low number of children who had solids introduced before age 4 months (n = 18).
Covariates
Given that a range of child (sex, birth weight, and gestational age) and maternal (education, country of birth, and prepregnancy BMI status) factors has been associated with child growth and obesity (2, 17, 18), these factors were considered as covariates in the present analyses. Parents reported information on maternal country of birth, highest education level attained, height, prepregnancy weight, and gestational age through a self-administered questionnaire completed at baseline. Country of birth was classified as Australia or other. Highest level of maternal education attained was classified as either university level (university degree and higher) or preuniversity level (certificate, diploma, apprenticeship, and high school). Maternal prepregnancy BMI was calculated as weight in kilograms divided by height in meters squared and categorized into healthy weight (< 25.0) and overweight/obesity (≥ 25.0). Gestational age was reported in weeks.
Statistical analyses
Summarizing BMIz trajectory
A descriptive analysis was conducted first to describe characteristics of the study cohort. Linear spline multilevel models were used to model the BMIz trajectory from birth to 60 months. This method uses a series of linear splines connected at knot points to model the trajectory and allows assessment of linear associations between the outcome and risk factors within different time periods rather than an entire trajectory (19, 20). Within-subject correlations and unequal variances of repeated BMIz measures were mitigated through use of covariance structure, and inclusion of random intercepts and slopes allowed for individual variations in BMIz trajectory (9, 21-23). This method has been widely used to describe growth when there are large variations in growth trajectories over time (9, 21-23). Both fractional polynomial and Lowess curves were used to estimate the best-fitting curve for age and BMIz, from which we identified three knot points (3, 9, and 18 months) at which the direction or slope of growth changed; three knot points generated four splines (growth periods): 0 to 3 months, 3 to 9 months, 9 to 18 months, and 18 to 60 months. The basic model included repeated measures of BMIz as the dependent variable, four individual splines as fixed effects, four individual splines as level 1 random effects, and the parent group as a level 2 random effect with an unstructured covariance structure. Parent groups were included as a random effect to account for clustering. Parameters in the model were estimated through restricted maximum likelihood methods. The intercept and coefficient (slope) of each spline of the fixed part represented average BMIz at birth and growth rates for that growth period, respectively. Random effects described the individual deviation from the average intercept and slope (19). A comparison of the observed and estimated mean at each time point revealed good agreement (data not shown).
Association between infant feeding and BMIz trajectory
To explore the association of breastfeeding duration and timing of solids introduction in relation to BMIz trajectories, these infant feeding practices were initially analyzed as the principal fixed effects in separate models. The interactions between the principal fixed effects and splines were fitted, and the coefficients of the interaction represented the mean difference between the growth rates by breastfeeding duration (< 6 vs. ≥ 6 months) or timing of solids introduction (before vs. after 6 months) in a given growth period. Additional multivariable multilevel models (model 1) with adjustment for covariates were conducted. Although previous analyses have shown no difference in anthropometric measures between the intervention and the control arms of the InFANT study (14), intervention allocation was included as a covariate to adjust for the potential bias by intervention. Assessment of multicollinearity of all independent variables via pairwise correlations confirmed that variables were not highly correlated (r < 0.3), confirming that all variables could be included in the same model. Average BMIz trajectories by breastfeeding duration and timing of solids introduction were graphed by plotting the estimated means at each follow-up. Further analyses (model 2) were performed to test the relative effects of breastfeeding duration and timing of solids introduction on BMIz trajectory by including them simultaneously in the same model. To test the potential interaction effect between these two variables, their interaction term was also included as a predictor. Only significant interactions (P < 0.05) were included in the mutually adjusted model.
To assess the effects of missing covariates on the analysis, we conducted multiple imputation to impute missing covariates and repeated the main analysis using imputed data. Covariates were assumed to be missing at random. The proportion of missing covariates ranged from 2% to 9%. Given the mixture of continuous and categorical covariates, imputation by chained equation was used with 10 data sets created using the “mi impute chained” command in Stata software version 15.0. Linear and logistic regression was used to predict continuous and categorical variables, respectively. Results from individual data sets were combined to obtain final estimates using the “mi estimate” command. All analyses were conducted using Stata software version 15.0 (StataCorp LLC, College Station, Texas), with the significance level set at P < 0.05.
Results
Of 542 children at baseline, 492 children with ≥ 2 BMIz measures and complete data on breastfeeding duration and timing of solids introduction were included in the unadjusted analysis. We excluded 9 participants with missing data on covariates, resulting in a sample of 483 children included in the final adjusted analysis (Supporting Information Figure S1). Participant characteristics are shown in Table 1. The proportion of children who were breastfed for ≥ 6 months was 59.2%, and 64.6% had solids introduced before 6 months of age. Characteristics of those included versus excluded were similar, although the proportion of children breastfed for ≥ 6 months was slightly higher among those included versus excluded (Supporting Information Table S1).
| n | % or Mean (SD) | |
|---|---|---|
| Intervention group | ||
| Intervention | 271 | 50.0 |
| Control | 271 | 50.0 |
| Maternal education | ||
| University | 287 | 53.0 |
| Preuniversity | 243 | 44.8 |
| Missing | 12 | 2.2 |
| Maternal prepregnancy BMI | ||
| Healthy weight | 339 | 62.5 |
| Overweight/obesity | 186 | 34.3 |
| Missing | 17 | 3.1 |
| Maternal country of birth | ||
| Australia | 418 | 77.1 |
| Other | 111 | 20.5 |
| Missing | 13 | 2.4 |
| Gestational age | ||
| < 37 weeks | 59 | 10.9 |
| ≥ 37 weeks | 470 | 86.7 |
| Missing | 13 | 2.4 |
| Child sex | ||
| Boys | 255 | 52.6 |
| Girls | 257 | 47.4 |
| Any breastfeeding duration | ||
| < 6 months | 189 | 34.9 |
| ≥ 6 months | 321 | 59.2 |
| Missing | 32 | 5.9 |
| Timing of solids introduction | ||
| Before < 6 months | 350 | 64.6 |
| After ≥ 6 months | 142 | 26.2 |
| Missing | 49 | 9.2 |
| Mean child age at each time point, mo | ||
| T1 | 536 | 3.6 (1.1) |
| T2 | 519 | 9.2 (1.1) |
| T3 | 472 | 17.8 (1.5) |
| T4 | 361 | 43.3 (2.5) |
| T5 | 361 | 60.7 (1.6) |
| Mean BMIz at each time point | ||
| Birth | 515 | 0.001 (1.3) |
| T1 | 536 | −0.5 (1.0) |
| T2 | 518 | 0.2 (1.0) |
| T3 | 469 | 1.0 (0.9) |
| T4 | 361 | 0.8 (0.9) |
| T5 | 246 | 0.7 (0.9) |
| Birth weight | 523 | 3.4 (0.6) |
| Low (< 2.5 kg) | 37 | 6.8 |
| Normal (≥ 2.5 and < 4 kg) | 418 | 77.1 |
| High (≥ 4 kg) | 68 | 12.5 |
| Missing | 19 | 3.5 |
| Birth length, cm | 516 | 50.0 (2.7) |
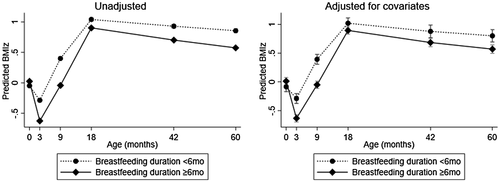
Average BMIz trajectory by breastfeeding duration
Table 2 presents the mean differences in birth BMIz and period-specific growth rates from birth to 60 months by breastfeeding duration. BMIz at birth was similar between children who were breastfed for ≥ 6 and < 6 months (P > 0.05). The average BMIz trajectory of children who were breastfed for < 6 months had an initial deceleration from birth to 3 months (−0.06 units/month), then an acceleration from both 3 to 9 months (+ 0.12 units/month) and 9 to 18 months (+ 0.08 units/month), followed by a deceleration from 18 to 60 months (−0.004 units/month) (Table 2). In contrast, the deceleration from birth to 3 months was more rapid (−0.12 units/month) (P = 0.002) and the acceleration from 9 to 18 months was faster (+ 0.03 units/month) among children who were breastfed for ≥ 6 months (P < 0.001) (unadjusted model; Table 2). No significant difference was found for growth rates between the two groups from 3 to 9 months and from 18 to 60 months (P > 0.05). The mean difference in growth rates of each period remained similar after adjustment for covariates (model 1; Table 2). Figure 1 shows the estimated average BMIz trajectory by breastfeeding duration group. Children who were breastfed for ≥ 6 months (solid lines) had lower mean BMIz at all ages between 3 and 60 months than those who were breastfed for < 6 months (dotted lines), and the mean differences were −0.34, −0.44, −0.14, −0.23, and −0.28 at 3, 9, 18, 42, and 60 months, respectively (P < 0.001) (unadjusted model; Figure 1). Adjustment for covariates slightly reduced the magnitude of the mean differences in BMIz between the two breastfeeding groups from 3 to 60 months (−0.34, −0.44, −0.13, −0.10, and −0.23 for 3, 9, 18, 42, and 60 months, respectively) (adjusted model; Figure 1). The model with missing data imputation revealed similar results (Supporting Information Table S2). Children with breastfeeding duration ≥ 3 months versus < 3 months had lower BMIz at 3 and 9 months, but no significant difference in BMIz at 18, 42, and 60 months was found (Supporting Information Figure S2).
| Breastfeeding duration < 6 months | Breastfeeding duration ≥ 6 vs. < 6 months | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted mean (95%CI) | Unadjusted model | Model 1 | Model 2 | |||||||
| Mean difference | 95% CI | P | Mean difference | 95% CI | P | Mean difference | 95% CI | P | ||
| Birth BMIz | −0.05 (−0.25 to 0.15) | 0.07 | −0.17 to 0.32 | 0.56 | 0.06 | −0.13 to 0.25 | 0.54 | 0.08 | −0.12 to 0.27 | 0.43 |
| Growth rate, mo | ||||||||||
| 0-3 | −0.06 (−0.12 to −0.02) | −0.12 | −0.20 to −0.04 | 0.002 | −0.13 | −0.21 to −0.05 | 0.001 | −0.14 | −0.22 to −0.06 | 0.001 |
| 3-9 | 0.12 (0.10 to 0.15) | −0.02 | −0.05 to 0.01 | 0.23 | −0.02 | −0.05 to 0.01 | 0.24 | −0.02 | −0.05 to 0.01 | 0.25 |
| 9-18 | 0.08 (0.06 to 0.09) | 0.03 | 0.02 to 0.05 | < 0.001 | 0.03 | 0.02 to 0.05 | < 0.001 | 0.035 | 0.02 to 0.05 | < 0.001 |
| 18-60 | −0.004 (−0.01 to −0.0002) | −0.003 | −0.01 to 0.001 | 0.17 | −0.003 | −0.01 to 0.001 | 0.15 | −0.004 | −0.01 to 0.001 | 0.12 |
- Model 1 adjusted for following covariates: child sex, birth weight, and gestational age; maternal country of birth, education, and prepregnancy BMI; and intervention group.
- Model 2 adjusted for covariates in model 1 and timing of solids introduction (≥ 6 vs. < 6 months).
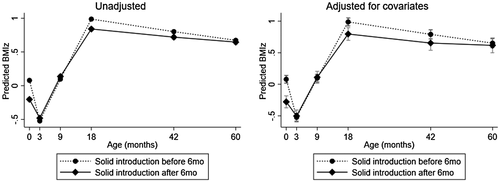
Average BMIz trajectory by timing of solids introduction.
The mean BMIz at birth for children who had solids introduced after 6 months of age was 0.28 units lower than that for children who had solids introduced before 6 months of age, but adjusting for covariates attenuated this difference (unadjusted model; Table 3). The deceleration in BMIz growth from birth to 3 months of children who had solids introduced after 6 months of age was less rapid (+ 0.09 units/month, P = 0.04) and the acceleration in BMIz growth from 9 to 18 months was slower (−0.02 units/month, P = 0.03) in comparison with those who had solids introduced before 6 months of age (unadjusted model; Table 3). The growth rates from 3 to 9 months and from 18 to 60 months were not significantly different between the two groups (P > 0.05). Controlling for covariates did not substantially change the growth rates in each period (model 1; Table 3). No significant difference in the mean BMIz was found between the two groups at both 3 and 9 months (P > 0.05). The mean BMIz of children who had solids introduced before 6 months of age was 0.15 and 0.08 units higher at 18 and 42 months, respectively, than that of children who had solids introduced after 6 months of age (P < 0.001) (unadjusted model; Figure 2). The mean BMIz of the two groups converged after 18 months, and no significant difference was found at 60 months (P > 0.05). Following adjustment for covariates, the mean differences in BMIz at 18 and 42 months were no longer statistically different (adjusted model, P > 0.05; Figure 2). Similar results were shown in the model with missing data imputation (Supporting Information Table S3).
| Solids introduction before 6 months | Solids introduction after 6 vs. before 6 months | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted mean (95%CI) | Unadjusted model | Model 1 | Model 2 | |||||||
| Mean difference | 95% CI | P | Mean difference | 95% CI | P | Mean difference | 95% CI | P | ||
| Birth BMIz | 0.08 (−0.07 to 0.22) | −0.28 | −0.54 to −0.02 | 0.03 | −0.17 | −0.38 to 0.03 | 0.10 | −0.20 | −0.38 to −0.02 | 0.08 |
| Growth rate, mo | ||||||||||
| 0-3 | −0.16 (−0.21 to −0.12) | 0.09 | 0.005 to 0.17 | 0.04 | 0.10 | 0.02 to 0.19 | 0.02 | 0.12 | 0.03 to 0.20 | 0.005 |
| 3-9 | 0.11 (0.1 to 0.13) | −0.0005 | −0.03 to 0.03 | 0.90 | −0.003 | −0.03 to 0.03 | 0.99 | −0.002 | −0.03 to 0.03 | 0.92 |
| 9-18 | 0.10 (0.09 to 0.11) | −0.02 | −0.04 to −0.002 | 0.03 | −0.02 | −0.04 to −0.001 | 0.03 | −0.02 | −0.04 to −0.005 | 0.01 |
| 18-60 | −0.01 (−0.01 to −0.0045) | 0.003 | −0.002 to 0.007 | 0.26 | 0.003 | −0.002 to 0.01 | 0.27 | 0.003 | −0.002 to 0.008 | 0.20 |
- Model 1 adjusted for following covariates: child sex, birth weight, and gestational age; maternal country of birth, education, and prepregnancy BMI; and intervention group.
- Model 2 adjusted for covariates in model 1 and breastfeeding duration (≥ 6 vs. < 6 months).
Relative effects of breastfeeding duration and timing of solids introduction on BMIz trajectory
There was no evidence of an interaction between breastfeeding duration and timing of solids introduction (P > 0.05). When breastfeeding duration and timing of solids introduction were mutually adjusted for in the same model, they both independently predicted significant mean differences in growth rates from 0 to 3 months and from 9 to 18 months (model 2; Tables 2 and 3). The mean differences in growth rates by breastfeeding duration were similar in models without versus with adjustment for timing of solids introduction (model 1 vs. model 2; Table 2). Results were similar with missing data imputation (Supporting Information Table S4). Children who were breastfed for ≥ 6 months (solid lines) had lower average BMIz from 3 to 60 months than those who were breastfed for < 6 months (dotted lines), irrespective of the timing of solids introduction (before or after 6 months) (Figure 3).

Discussion
In a cohort of Australian children, we found that breastfeeding duration and timing of solids introduction were both independently associated with BMIz trajectory from birth to 60 months. Differential growth rates from birth to 3 months and from 9 to 18 months by breastfeeding duration (≥ 6 vs. < 6 months) and timing of solids introduction (before vs. after 6 months) were revealed. Moreover, children with breastfeeding duration ≥ 6 months had consistently lower mean BMIz from 3 to 60 months than those with breastfeeding duration < 6 months, and this difference remained after adjustment for child and maternal factors. In contrast, children with breastfeeding duration ≥ 3 versus < 3 months did not show significant differences in BMIz from 18 to 60 months. For timing of solid foods introduction, children who had solids introduced before versus after 6 months of age showed higher mean BMIz at both 18 and 42 months, but this disappeared after adjustment for child and maternal factors.
This work expands on the small number of studies that have examined the association between breastfeeding duration and subsequent BMIz trajectories. Eny et al. (9) examined the influence of breastfeeding duration on BMIz trajectory from birth to 10 years in a cohort of Canadian children (N = 5,905). Consistent with our study findings, that study reported (with adjustment for child birth weight, maternal ethnicity, maternal BMI, and household income) that children with breastfeeding duration ≥ 6 months had smaller BMIz at 18, 36, and 72 months than those with breastfeeding duration < 6 months, with mean differences of −0.24, −0.12, and −0.19, respectively (9). Our study extends and supports these findings by the inclusion of data from 3 months of age. We found an early emergence of differential BMIz trajectories by breastfeeding duration group at 3 months of age. However, further information on exclusive breastfeeding and formula feeding is needed to understand the early difference of BMIz between breastfeeding duration groups in our cohort. Our finding that children with breastfeeding duration ≥ 6 months (compared with < 6 months) had a smaller mean BMIz at 60 months of age confirms a favorable long-lasting effect of longer breastfeeding duration on BMIz development. Similar findings were documented in a large Japanese cohort, in which children with breastfeeding duration ≥ 6 months had lower BMI at both 6 and 7 years of age than those with breastfeeding duration < 6 months (24). Likewise, Carling et al. (25) and Liu et al. (26) found that infants with longer breastfeeding duration were less likely to have rising weight gain trajectories during infancy. In contrast, contradictory findings were reported in the Promotion of Breastfeeding Intervention Trial (PROBIT) study, in that breastfeeding duration was not associated with improvement in BMI at 11.5 years of age (27). The low prevalence of any breastfeeding at 6 months (24%-36%) and obesity (5%) in that sample might contribute to the discrepant findings (27).
The underlying mechanism by which breastfeeding protects against obesity is unclear. The most prominent current hypothesis is that the slower growth of breastfed babies may mitigate obesity risk (28). Systematic reviews have suggested that rapid infant growth, defined as crossing one percentile line in the growth chart, is associated with two to three times higher risk of subsequent overweight or obesity (29, 30). Other hypotheses relate to the nutritional composition of breast milk (i.e., leptin and ghrelin), which may contribute to energy balance and body weight regulation via appetite control and endocrine pathways (31-33). Moreover, breast milk has lower protein content than infant formula. High protein intake during infancy has been associated with an increased risk of subsequent obesity (34, 35). Confounding effects by other obesity-related factors are also possible, with longer breastfeeding duration associated with high nutrition knowledge and maternal education, both of which are associated with lower obesity prevalence in high-income countries (33). Our study, however, found that adjustment for growth-related child and maternal factors, including maternal education, did not attenuate the associations, indicating that differential BMIz trajectories between breastfeeding duration groups were likely independent of these potential confounding factors.
Studies investigating the association between timing of solids introduction and subsequent BMI trajectories are limited. Our finding supports the conclusion from a 2015 systematic review that no clear association was found for the introduction of solids after 6 months of age with subsequent obesity (5). This review, however, suggests that there is some evidence linking the introduction of solids prior to 4 months of age with an elevated risk of childhood obesity (5). It is hypothesized that early introduction of solids may result in an increased intake of energy and protein during infancy that leads to weight gain (36). We were unable to examine 4 months as a cutoff because of the small number of children who had solids introduced before 4 months of age. It has to be noted that infant feeding guidelines to introduce solids at around 6 months of age are primarily driven by the prevention of infant nutrient deficiencies and food allergies (12).
This is one of the first studies to report an independent effect of breastfeeding duration and timing of solids introduction on subsequent BMIz trajectories. Garden et al. (37) used latent class growth models to identify distinct BMIz trajectory groups and assessed determinants of the identified BMIz trajectory groups in an Australian cohort (N = 370) (37). They found that neither breastfeeding duration nor timing of solids introduction was associated with BMI trajectory groups from birth to 11.5 years. The longer duration of follow-up in that study and the different study methodology may have contributed to the null findings. Other existing studies have examined the relationships of both breastfeeding and timing of solids introduction in relation to subsequent obesity outcomes at one point in time but have not examined relative effects. In a large cohort of US children (N = 8,030), breastfed infants were less likely to be affected by obesity at 24 months compared with formula-fed or mixed breastfed/formula-fed children, and the introduction of solids before 4 months of age had a higher risk of obesity at 24 months (38). In contrast, Ejlerskov et al. (39), in a Danish study of 233 children, found no associations between breastfeeding and timing of solids introduction and body composition at 3 years of age (39).
The current study has several strengths and limitations. The longitudinal design with repeated measures of BMIz enabled the use of linear multilevel spline models to construct longitudinal trajectories of BMIz, derive period-specific growth rates, and explore the determinants of BMIz trajectory. Given that infant feeding clusters with other prenatal and early-life factors that impact growth and obesity, a strength of this study was controlling for important confounders that relate to both infant feeding and childhood obesity, including child birth weight, maternal education, and maternal prepregnancy BMI. Study limitations include loss of follow-up and missing data. However, the use of multilevel models enabled the use of all available measurements, and missing data imputation revealed similar findings. We were unable to separate exclusive breastfeeding from any breastfeeding, and we did not collect information on timing of formula feeding. This information could be useful to better understand the observed early difference in BMIz trajectory between the breastfeeding duration groups. Studies with further exploration into varying breastfeeding duration lengths would be desirable to provide further insights into potential linear dose–response relationships. It is important to acknowledge that the observational nature of the study limits our ability to infer causal relationships, and other residual and unmeasured confounding is also possible. Maternal smoking, gestational weight gain, and history of diabetes, which have been shown to impact child BMIz, were not examined in the present study (18). One major limitation of the study is the lack of adjustment for intake of energy-dense and nutrient-poor foods, physical activity, sedentary behaviors, and sleep pattern in early childhood. These factors need to be carefully considered in future studies because they may be potential mediators of the association between infant feeding and growth trajectories (40).
Our findings could have important implications. The protective effects of any breastfeeding on BMIz extended to 5 years of age, and they were prominent in all children regardless of their birth weight, maternal education, or maternal BMI. These findings strongly endorse current policies, public health campaigns, and interventions that seek to promote and support any and extended breastfeeding. Our findings suggest that solids introduction before or after 6 months of age was less important in predicting BMIz differences in early childhood than breastfeeding duration. Future research may further explore the effects of solids type and quantity on BMIz development.
Conclusion
The present study showed that breastfeeding duration for 6 months or more was associated with lower BMIz across the first 5 years of life. The timing of solids introduction, whether before or after 6 months of age, showed no evidence of differences in BMIz at 5 years of age. The findings provide further support for infant feeding guidelines to promote breastfeeding of at least 6 months duration to promote healthy growth.
Acknowledgments
This secondary analysis of the InFANT Program differs from the previous analyses because the focus is not to evaluate intervention effects but to assess the effect of infant feeding on body weight development with the use of additional follow-up data at 3.5 and 5 years of age. The InFANT study protocol and outcome analyses have been published and cited in the present study. All individual participant deidentified data are available for sharing with researchers who provide a methodologically sound proposal. Proposals should be directed to [email protected], and a data access agreement will need to be signed before the release of data.





