Behavioral and Psychological Strategies of Long-Term Weight Loss Maintainers in a Widely Available Weight Management Program
Abstract
Objective
The study’s purpose was to use validated questionnaires to identify novel behavioral and psychological strategies among weight loss maintainers (WLMs) in a commercial weight management program.
Methods
Participants were 4,786 WLMs in WW (formerly Weight Watchers, New York, New York) who had maintained weight loss ≥ 9.1 kg (24.7 kg/23.8% weight loss on average) for 3.3 years and had a current mean BMI of 27.6 kg/m2. A control group of 528 weight-stable individuals with obesity had a mean BMI of 38.9 kg/m2 and weight change < 2.3 kg over the previous 5 years.
Results
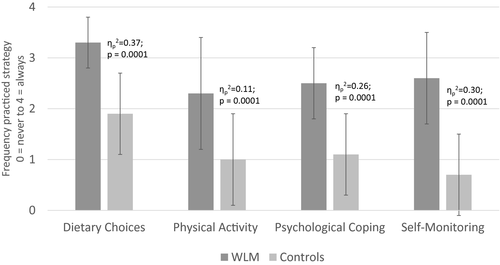
WLMs versus Controls practiced more frequent healthy dietary choices (3.3 vs. 1.9;  = 0.37), self-monitoring (2.6 vs. 0.7;
= 0.37), self-monitoring (2.6 vs. 0.7;  = 0.30), and psychological coping (2.5 vs. 1.1;
= 0.30), and psychological coping (2.5 vs. 1.1;  = 0.25) strategies. WLMs also reported more willingness to ignore food cravings (4.4 vs. 3.5;
= 0.25) strategies. WLMs also reported more willingness to ignore food cravings (4.4 vs. 3.5;  = 0.16) and had greater habit strength for healthy eating (5.3 vs. 3.2;
= 0.16) and had greater habit strength for healthy eating (5.3 vs. 3.2;  = 0.21). Standard canonical coefficients indicated that dietary (0.52), self-monitoring (0.40), and psychological (0.14) strategies as well as habit strength for healthy eating (0.15) contributed independently and most (49.5% of variance) to discriminating groups.
= 0.21). Standard canonical coefficients indicated that dietary (0.52), self-monitoring (0.40), and psychological (0.14) strategies as well as habit strength for healthy eating (0.15) contributed independently and most (49.5% of variance) to discriminating groups.
Conclusions
In a widely available weight management program, more frequent practice of healthy dietary, self-monitoring, and psychological coping strategies as well as development of greater habit strength for healthy eating differentiated long-term WLMs from weight-stable individuals with obesity.
Study Importance
What is already known?
- ► Few people are successful in long-term weight maintenance.
- ► Successful maintainers are charecterized by a lower-calorie diet, higher levels of physical activity, higher dietary restraint, and more frequent self-monitoring.
- ► In WW, long-term successful weight loss maintenance has not been studied.
What does this study add?
- In WW, compared with weight-stable individuals with obesity, successful weight loss maintainers: practiced more healthy dietary choices, self-monitoring, and psychological coping; reported greater habit strength for healthy eating, which was related to longer duration of maintenance and less perceived effort for maintenance; and demonstrated no difference in self-kindness, mindfulness, and acceptance strategies.
Introduction
Long-term successful weight control requires continued consumption of a lower-calorie diet, engagement in high levels of physical activity, and frequent self-monitoring of weight, eating, and activity (1, 2). The National Weight Control Registry (1, 2) and others (3-5) have comprehensively described these strategies. The frequency and intensity with which these behaviors are practiced have been consistently related to duration and magnitude of long-term successful weight control. Behavioral strategies identified among weight loss maintainers (WLMs) have informed clinical trial research and development of the behavioral treatment programs widely used today.
Despite these advances, several novel behavioral and psychological targets remain uninvestigated. Weight control strategies, such as keeping healthy foods in visible locations, setting daily goals, and “talking back” to negative thoughts, are numerous in standard behavioral weight management programs, but frequency and practice of these “micro” behaviors have not been investigated outside the clinical research setting and among WLMs (6). Similarly, acceptance and mindfulness-based approaches (7) and developing routines and habit strength (8) have received increasing attention in research, but the extent to which long-term WLMs outside of clinical research settings regularly employ and benefit from these strategies remains unknown. Understanding whether and how WLMs use these strategies compared with weight-stable individuals with obesity is important to informing programs designed to promote long-term weight loss maintenance in individuals with obesity outside of the research clinic setting.
Most (55%) WLMs in the National Weight Control Registry reported using “a formal program or professional assistance” to lose weight, but the habits of successful WLMs in commercial weight management programs have remained largely unexamined. About 10% to 15% of individuals seek weight loss through commercial weight management programs, and current clinical guidelines recommend commercial weight loss programs with documented efficacy (9). WW (formerly Weight Watchers, New York, New York) is a widely available, commercial behavioral weight management program that encourages healthy habits in the areas of food, activity, and mind-set that has demonstrated clinically significant average long-term weight loss (10-13). Identifying the strategies of individuals who succeed at long-term weight loss maintenance in programs such as WW is critical for developing effective treatments that promote successful weight loss maintenance in the millions of consumers whom commercial programs reach each year.
The purpose of this study was to use validated questionnaires to identify novel behavioral and psychological strategies among WLMs who lost weight in WW. Compared with weight-stable individuals with obesity, long-term WLMs in WW were expected to report greater practice of weight control strategies, including healthy diet (e.g., setting a calorie goal), self-monitoring (e.g., keeping a record of the type and amount of food), physical activity (e.g., keeping exercise clothes in sight), and psychological coping (e.g., challenging negative thoughts). WLMs were also expected to report greater habit strength and acceptance, mindfulness, and self-kindness strategies. Finally, WLMs were expected to report significantly greater quality of life as a result of their long-term weight loss.
Methods
Design
The WW Success Registry is a cross-sectional observational study of individuals who lost weight in the WW program and who were successful at long-term (≥ 1 year) maintenance of substantial weight loss. To distinguish the factors associated with successful maintenance of weight loss versus weight-stable obesity, a control group of weight-stable individuals with obesity was enrolled. Other control groups were considered, including individuals who had lost and regained weight (“weight regainers”). Prior research found that weight regainers and weight-stable individuals with obesity scored similarly on measures of behavioral strategies (14). Thus, only one control group was included in the current study.
Participants
Procedures were approved by the California Polytechnic State University (Cal Poly) Institutional Review Board, and all participants provided informed consent.
WLMs
To be eligible for enrollment, individuals were aged ≥ 18 years and they had maintained weight loss ≥ 20 lb (9.1 kg) from WW entry for ≥ 1 year. The criterion of 20 lb (9.1 kg) was selected to approximate a clinically significant 10% weight loss (9), assuming a starting weight of 200 lb (90 kg) among people entering WW and other weight loss programs (15). Use of an absolute weight loss value was also intended to simplify messaging for recruitment and eligibility screening, as used successfully in the National Weight Control Registry (1).
Weight-stable individuals with obesity
To be eligible for enrollment, individuals were aged ≥ 18 years, had BMI ≥ 30, and reported weight stability (± 5 lb) for ≥ 5 years prior to enrollment (14); weight loss attempts over the prior 5 years were not assessed. Individuals who reported being currently in WW were also excluded. After completion of the questionnaire, control participants were provided 1 month of the WW online program (WW Digital) free of charge.
Procedures
Prospective WLMs were recruited through an email sent by WW to members who had reported weight loss ≥ 20 lb in WW more than 1 year prior. Interested individuals were referred to the study website hosted by Cal Poly for online screening, consent, and enrollment. Eligibility was based on self-reported weight, height, weight change, and duration. Weight-stable individuals with obesity were recruited through local and national advertising channels, including Facebook, ResearchMatch.org, and Amazon Mechanical Turk, and via the Cal Poly Center for Health Research registry; consent and assessment procedures were the same in both groups.
Measures
All measures were administered online via RedCap (version 9.1.0; Vanderbilt University, Nashville, Tennessee) immediately after consent. All participants were asked for standard demographic information (age, education level, marital status), details about weight history (age of onset of overweight, maximum lifetime weight), and current weight and height. The validity of self-reported weight history has been established previously (16). Also, self-reported weights have been shown to correlate strongly with measured weights (17).
The Weight Control Strategies Scale (18) was used to measure weight control strategies, including healthy dietary choices (e.g., kept high-calorie foods out of sight, kept low-calorie foods accessible), self-monitoring (kept graph of weight, kept record of calories), physical activity (set exercise goals, had plan for exercise), and psychological coping (if I regained weight, I thought about past successes; if I had negative thoughts about weight loss progress, I tried to calm myself and stop that kind of thinking). Cronbach α coefficients for the total scale were shown to be > 0.79 in other research (18) and 0.94 in the current study. For WW participants, the questionnaire included reference to the WW SmartPoints system (e.g., “low-calorie food” became “low-calorie/low-point food”).
The Food Craving Acceptance and Action Questionnaire (FAAQ) (19) was administered to assess participants’ ability to experience uncomfortable internal experiences (e.g., thoughts, feelings, urges, cravings) versus attempting to change or control them; the scale was shown to have adequate internal consistency (α = 0.66) and validity (19). In the current sample, the FAAQ’s internal consistency was α = 0.57. Self-kindness and compassion were measured using the validated Self-Compassion Scale (20), which was shown to have high internal consistency (α = 0.94) in prior research (21) and the current sample (α = 0.87). The measure was designed to assess self-compassion as being kind and understanding toward oneself in instances of pain or failure (Self-Kindness subscale) rather than being harshly self-critical (Self-Judgment subscale); perceiving one’s experiences as part of the larger human experience (Common Humanity subscale) rather than seeing them as isolating (Isolation subscale); and holding painful thoughts and feelings in mindful awareness (Mindfulness subscale) rather than overidentifying with them (Over-Identified subscale).
Habit strength for physical activity and healthy eating was measured using the Self-Report Habit Index, which had high internal validity and reliability in prior studies (α’s ranging from 0.85 to 0.95) (22) and in the current sample (α = 0.96). This measure captures features of exercise and healthy eating as routine, frequent, and automatic (e.g., I do automatically, I do without having to consciously remember, I do without thinking). Routinization was measured using the Variety Scale (23). The psychometric and behavioral properties of this scale were reported as adequate (α = 0.74) (23) with two factors: Having Order and Routine in Life (α = 0.71) and Disliking Disruption (i.e., a tendency to respond negatively when life stresses threaten structure and routine; α = 0.63). In the current sample, the Cronbach α for the overall scale was 0.57. Also, dietary and exercise consistency was measured with single-item questions used in the National Weight Control Registry (24). Finally, quality of life was measured using the well validated Short Form (SF)-20 (α > 0.70), which measures overall health-related quality of life (25).
Statistical methods
Group differences in sociodemographic variables and characteristics of those who completed versus did not complete the questionnaire were analyzed by independent t tests and χ2 analyses. ANCOVA and linear and logistic regression models were used to examine differences between the WLMs and weight-stable individuals with obesity on dependent measures, adjusting for demographic factors of sex, income, age, race, education, lifetime maximum weight, and employment. Similar analyses explored group differences in individual items on the questionnaires.
Discriminant function analysis was used to determine the strategies that most discriminated WLMs from weight-stable individuals with obesity among the set of variables (subscale scores only, not individual items) that were found to differ between the two groups in the initial univariate analyses. The resulting standardized canonical coefficients represent the measure of association between the discriminant function (based on the linear combination of variables) and each predictor variable and they indicate the relative importance of each variable in distinguishing the two groups (similar to β weights in a multiple regression).
To guard against type I error due to multiple analyses, statistical significance was set to P < 0.01, and significance furthermore was interpreted only for group differences that resulted in ηp2 values > 0.15, representing at least a small effect size (26). Among WLMs, partial correlations were conducted to examine relationships among weight control strategies, habit strength, duration of weight loss maintenance, and quality of life, adjusting for the same covariates. SPSS Statistics software version 23.0.0 (IBM Corp., Armonk, New York) was used for all analyses.
Results
This study included a group of WLMs and a comparison group of weight-stable individuals with obesity. For the WW group, a total of 6,476 eligible individuals completed the consent form; of these, 4,786 (73.8%) participants who completed the weight control strategies questionnaire were included in this study. WLMs who completed versus did not complete the questionnaire were older (mean [SD]; 53.9 [12.6] vs. 52.0 [12.7] years; P = 0.0001), had a lower BMI at study entry (27.6 [5.4] vs. 28.1 [5.5] kg/m2; P = 0.002), were more likely to be White (94.5% vs. 54.1%; P = 0.0001), and were more likely to be married (74.7% vs. 68.4%; P = 0.0001), but they did not differ by sex, education, income, BMI at their WW start, duration of weight loss maintenance, or magnitude of weight loss from WW start. Among weight-stable individuals with obesity, 665 eligible individuals completed the consent form; of these, 528 (79.4%) participants completed the weight control strategies questionnaire and were included in this study. Comparison of completers versus noncompleters revealed that completers were more likely to be White (84.7% vs. 33.8%; P = 0.0001), but no other significant differences were observed. As shown in Tables 1 to 4, sample sizes varied across the measures. For the habits and routinization scales, the sample sizes among WW and controls were 3,676 and 429, respectively; for the self-compassion, acceptance, and quality of life scales, the sample sizes were 3,559 WW and 408 controls. Comparing those who completed the full versus partial questionnaire, completers were older (53.9 [12.0] vs. 52.7 [12.6] years; P = 0.0001) and more likely to be employed (75.3% vs. 24.7%; P = 0.0001), but they did not differ by group or any of the other demographic factors.
| WLM, N = 4,786 | Controls, N = 528 | P value | |
|---|---|---|---|
| Age, mean (SD), y | 53.4 (12) | 48.5 (13) | 0.0001 |
| Female, % | 91.9 | 80.4 | 0.0001 |
| Currently in WW, % | 88.8 | Not applicable | – |
| Lifetime maximum weight, mean (SD), kg | 105.3 (22.9) | 119.1 (26.5) | 0.0001 |
| Weight at start of WW, mean (SD), kg | 101.3 (21.2) | Not applicable | – |
| Current weight, mean (SD), kg | 76.9 (16.6) | 108.3 (21.6) | 0.0001 |
| Weight loss since WW start, mean (SD), kg | 24.7 (12.5) | – | – |
| Percentage weight loss since WW start, mean (SD), % | 23.8 (8.7) | – | – |
| Duration of 9.1-kg loss from WW start weight, mean (SD), y | 3.3 (3.3) | – | – |
| Weight lost from maximum weight, mean (SD), kg | 28.6 (15.0) | 10.5 (12.4) | 0.0001 |
| Current BMI, mean (SD), kg/m2 | 27.6 (5.4) | 38.9 (7.2) | 0.0001 |
| BMI categories | 0.0001 | ||
| Obesity, % | 22.5 | 100% | – |
| Overweight, % | 44.7 | 0 | – |
| Normal weight, % | 32.7 | 0 | – |
| Underweight, % | 0.0 | 0 | – |
| Income (total in family per year) | 0.0001 | ||
| < $25,000, % | 4.6 | 20.4 | – |
| $25,000-74,999, % | 30.5 | 48.3 | – |
| ≥ $75,000, % | 65.0 | 31.3 | – |
| Race/ethnicity | 0.0001 | ||
| White, % | 94.4 | 83.9 | – |
| Black, % | 2.8 | 12.7 | 0.0001 |
| Hispanic, % | 3.7 | 3.4 | 0.0001 |
| Employed, % | 66.1 | 72.0 | 0.01 |
| College education or more, % | 88.9 | 86.5 | 0.01 |
| Married, % | 73.5 | 50.9 | 0.29 |
| WLM, N = 4,786, mean (95% CI) | Controls, N = 528, mean (95% CI) | Group effecta | |
|---|---|---|---|
| Weight control strategies total (0 = never; 4 = always) | 2.7 (2.7-2.8) | 1.3 (1.2-1.3) |  = 0.373; P = 0.0001 = 0.373; P = 0.0001 |
| Dietary Choices subscale score | 3.3 (3.2-3.3) | 1.9 (1.9-2.0) |  = 0.356; P = 0.0001 = 0.356; P = 0.0001 |
| Individual items | |||
| I chose lower-calorie/lower-point foods to eat instead of higher-calorie options | 3.1 (3.1-3.2) | 1.6 (1.5-1.7) |  = 0.256; P = 0.0001 = 0.256; P = 0.0001 |
| I kept low-calorie/low-point foods accessible for a healthy snack | 3.4 (3.4-3.5) | 1.9 (1.8-2.0) |  = 0.239; P = 0.0001 = 0.239; P = 0.0001 |
| I had several servings of fruits/vegetables each day | 3.4 (3.4-3.4) | 1.9 (1.8-2.0) |  = 0.240; P = 0.0001 = 0.240; P = 0.0001 |
| I ate lower-fat meats | 3.2 (3.2-3.3) | 1.9 (1.8-2.0) |  = 0.220; P = 0.0001 = 0.220; P = 0.0001 |
| When eating dairy products (milk, yogurt, cheese), I chose low-calorie/low-point options. | 3.2 (3.2-3.3) | 1.6 (1.5-1.7) |  = 0.182; P = 0.0001 = 0.182; P = 0.0001 |
| I ate meats, fish, or vegetables that were baked, broiled, or grilled | 3.4 (3.3-3.4) | 2.2 (2.1-2.3) |  = 0.179; P = 0.0001 = 0.179; P = 0.0001 |
| I set a calorie goal for myself | 2.8 (2.8-2.8) | 0.9 (0.8-1.0) |  = 0.149; P = 0.0001 = 0.149; P = 0.0001 |
| Physical Activity Strategies subscale score | 2.3 (2.3-2.3) | 1.0 (0.9-1.1) |  = 0.11; P = 0.0001 = 0.11; P = 0.0001 |
| Psychological Coping subscale score | 2.5 (2.5-2.5) | 1.1 (1.1-1.2) |  = 0.26; P = 0.0001 = 0.26; P = 0.0001 |
| Individual items | |||
| If I regained weight, I thought about my past successes and reminded myself that I could get back on track | 3.2 (3.4-3.2) | 1.2 (1.1-1.3) |  = 0.25; P = 0.0001 = 0.25; P = 0.0001 |
| If I got off track with my eating or exercise, I encouraged myself by thinking positively | 2.9 (2.9-2.9) | 1.4 (1.3-1.5) |  = 0.18; P = 0.0001 = 0.18; P = 0.0001 |
| Self-Monitoring Strategies subscale score | 2.6 (2.6-2.6) | 0.7 (0.7-0.8) |  = 0.30; P = 0.0001 = 0.30; P = 0.0001 |
| Individual items | |||
| I kept a record of the type and amount of foods that I ate | 3.0 (3.0-3.0) | 0.7 (0.7-0.8) |  = 0.27; P = 0.0001 = 0.27; P = 0.0001 |
| I kept a record of the calories/points of foods I ate | 3.0 (3.0-3.0) | 0.6 (0.5-0.7) |  = 0.26; P = 0.0001 = 0.26; P = 0.0001 |
| I weighed and/or measured the foods I ate | 2.4 (2.4-2.4) | 0.4 (0.3-0.5) |  = 0.20; P = 0.0001 = 0.20; P = 0.0001 |
| I set a daily calorie/point goal for myself | 2.8 (2.8-2.8) | 0.9 (0.8-1.0) |  = 0.16; P = 0.0001 = 0.16; P = 0.0001 |
| Weekly or more frequent self-weighing, % | 94.3% | 46.0% | Odds ratio (95% CI) = 17.3 (13.5, 21.9)b |
- a
Group effect based on general linear model adjusting for age, race, employment, education, income, maximum lifetime weight, and sex. Means adjusted for these variables. To guard against type I error due to multiple analyses, statistical significance set to P < 0.01 and significance furthermore interpreted only for group differences that resulted in
 values > 0.15, representing at least a small effect size (26).
values > 0.15, representing at least a small effect size (26).
- b Logistic regression analysis adjusting for age, race, employment, education, income, maximum lifetime weight, and sex. Proportions are unadjusted.
| WLM, N = 3,676, mean (95% CI) | Controls, N = 429, mean (95% CI) | Group effecta | |
|---|---|---|---|
| Healthy eating habit strength (1 = strongly disagree; 7 = strongly agree) | 5.3 (5.2-5.3) | 3.2 (3.1-3.4) |  = 0.21; P = 0.0001 = 0.21; P = 0.0001 |
| Individual items | |||
| I do frequently | 6.1 (6.1-6.1) | 3.7 (3.6-3.8) |  = 0.30; P = 0.0001 = 0.30; P = 0.0001 |
| Belongs to my daily routine | 6.2 (6.1-6.2) | 4.1 (3.9-4.2) |  = 0.25; P = 0.0001 = 0.25; P = 0.0001 |
| I have been doing for a long time | 5.6 (5.5-5.6) | 3.2 (3.1-3.4) |  = 0.19; P = 0.0001 = 0.19; P = 0.0001 |
| I do automatically | 5.4 (5.3-5.5) | 3.2 (3.0-3.5) |  = 0.17; P = 0.0001 = 0.17; P = 0.0001 |
| Makes me feel weird if I do not do it | 5.4 (5.4-5.5) | 3.1 (3.0-3.3) |  = 0.18; P = 0.0001 = 0.18; P = 0.0001 |
| I start doing before I realize I am doing it | 5.3 (5.2-5.3) | 3.1 (3.0-3.3) |  = 0.15; P = 0.0001 = 0.15; P = 0.0001 |
| That’s typically me | 5.3 (5.2-5.3) | 3.2 (3.0-3.3) |  = 0.15; P = 0.0001 = 0.15; P = 0.0001 |
| Physical activity habit strength (1 = strongly disagree and 7 = strongly agree) | 4.4 (4.3-4.5) | 2.7 (2.5-2.9) |  = 0.08; P = 0.0001 = 0.08; P = 0.0001 |
| Individual item | |||
| I do frequently | 5.3 (5.2-5.4) | 3.0 (2.8-3.2) |  = 0.114; P = 0.0001 = 0.114; P = 0.0001 |
| Routinization/Variety Scale Overall (1 = very untrue; 5 = very true) | 3.3 (3.3-3.4) | 3.2 (3.1-3.2) |  = 0.005; P = 0.0001 = 0.005; P = 0.0001 |
| Extent Have Order and Routine in Daily Life subscale | 3.3 (3.3-3.4) | 3.2 (3.1-3.3) |  = 0.004; P = 0.0001 = 0.004; P = 0.0001 |
| Extent Dislike Disruption subscale | 2.8 (2.8-2.9) | 2.8 (2.7-2.9) |  = 0.0; P = 0.33 = 0.0; P = 0.33 |
- a
Group effect based on general linear model adjusting for age, race, employment, education, income, maximum lifetime weight, and sex. Means adjusted for these variables. To guard against type I error due to multiple analyses, statistical significance set to P < 0.01 and significance furthermore interpreted only for group differences that resulted in
 values > 0.15, representing at least a small effect size (26).
values > 0.15, representing at least a small effect size (26).
| WLM, N = 3,559, mean (95% CI) | Controls, N = 408, mean (95% CI) | Group effecta | |
|---|---|---|---|
| Self-compassion (subscale range: 2 = almost never; 10 = almost always) | |||
| Self-Kindness subscale | 6.5 (6.5-6.6) | 6.1 (5.9-6.3) |  = 0.005; P = 0.0001 = 0.005; P = 0.0001 |
| Self-Judgment subscale | 6.0 (5.9-6.0) | 5.6 (5.4-5.9) |  = 0.002; P = 0.004 = 0.002; P = 0.004 |
| Common Humanity subscale | 6.6 (6.6-6.7) | 6.1 (5.9-6.3) |  = 0.01 P = 0.004 = 0.01 P = 0.004 |
| Isolation subscale | 6.2 (6.1-6.2) | 5.6 (5.4-5.8) |  = 0.006; P = 0.0001 = 0.006; P = 0.0001 |
| Mindfulness subscale | 7.2 (7.-7.2) | 6.9 (6.8-7.1) |  = 0.002; P = 0.005 = 0.002; P = 0.005 |
| Over-Identified subscale | 5.9 (5.8-6.0) | 5.7 (5.4-5.9) |  = 0.001; P = 0.02 = 0.001; P = 0.02 |
| Food Craving Acceptance & Action (1 = very seldom; 3 = sometimes; 4 = frequently; and 6 = always) | |||
| Willingness subscale (willingness to ignore cravings) | 4.4 (4.4-4.5) | 3.5 (3.4-3.6) |  = 0.16; P = 0.0001 = 0.16; P = 0.0001 |
| Acceptance subscale (don’t try to control urges) | 3.2 (3.1-3.2) | 2.9 (2.8-3.1) |  = 0.003; P = 0.0001 = 0.003; P = 0.0001 |
| Quality of life | 77.7 (77.3-78.1) | 64.3 (63.2-65.4) |  = 0.14; P = 0.0001 = 0.14; P = 0.0001 |
| Effort to maintain current weight (1 = no effort; 7 = extreme effort) | 4.6 (4.5-4.6) | 3.5 (3.4-3.7) |  = 0.05; P = 0.0001 = 0.05; P = 0.0001 |
- a
Analyses and means adjusted for lifetime maximum weight, income, race (White vs. other), employment, education, age, and sex. To guard against type I error due to multiple analyses, statistical significance set to P < 0.01 and significance furthermore interpreted only for group differences that resulted in
 values > 0.15, representing at least a small effect size (26).
values > 0.15, representing at least a small effect size (26).
Demographic characteristics of study participants are displayed in Table 1. WLMs had lost on average 24.7 kg and maintained the minimum (9.1 kg) weight loss for 3.3 years. WLMs had an average BMI of 36.5 before their successful weight loss and a current BMI of 27.6. In contrast, weight-stable individuals with obesity had maintained a current average BMI of 38.9 for more than 5 years. Compared with WLMs, these participants were more likely to be more employed, less educated, nonwhite, male, younger, and with lower income (Table 1), which were adjusted for in subsequent analyses.
Univariate group differences in behavioral and psychological factors
Adjusting for group differences in demographic factors, WLMs and weight-stable individuals with obesity differed on several behavioral and psychological variables. Compared with weight-stable individuals with obesity, WLMs reported significantly greater practice of strategies to support healthy dietary choices, self-monitoring, and psychological coping (Table 2 and Figure 1). Exploring individual questions within these subscales, specific dietary strategies included choosing lower-calorie foods, keeping low-calorie/low-point foods accessible, and eating more servings of fruits and vegetables. Specific self-monitoring strategies included keeping a graph of weight, recording calories/points, and keeping a daily calorie/point goal. Psychological coping strategies included, if they regained weight, thoughts about past successes and, if they got off track, self-encouragement to think positively (Table 2). Group differences in physical activity strategies, while statistically significant, were below the prespecified 0.15 effect size threshold.
Examining habit strength, WLMs versus weight-stable individuals with obesity reported significantly greater habit strength scores for healthy eating (5.3 vs. 3.2 on 1-7 scale) (Table 3). Specific items that differed significantly between groups pertained to WLMs’ greater frequency and automaticity of healthy eating habits. Although WLMs reported statistically more habit strength for physical activity and also more structure and order in their lives compared with weight-stable individuals with obesity, the effect sizes were below the 0.15 threshold (Table 3).
Examining self-compassion and acceptance scores (Table 4), both groups reported “sometimes” to “frequent” practice of these strategies. WLMs versus weight-stable individuals with obesity reported greater willingness to ignore food cravings (4.4 vs. 3.5 on a 6-point scale; P = 0.0001;  = 0.16). While higher scores among WLMs were observed for many of the other acceptance and self-kindness domains (Table 4), effect sizes were small.
= 0.16). While higher scores among WLMs were observed for many of the other acceptance and self-kindness domains (Table 4), effect sizes were small.
Quality of life scores were significantly higher among WLMs than weight-stable individuals with obesity (Table 4). Moreover, WLMs versus weight-stable individuals reported exerting significantly more effort (4.6 vs. 3.5, respectively, on a scale of 1-7) to maintain their current body weight.
Multiple discriminant analysis of behavioral and psychological factors
Multiple discriminant analysis was conducted to determine, among subscale variables that differed between groups in univariate analyses, which ones most strongly discriminated WLMs from weight-stable individuals with obesity. Standardized canonical coefficients indicated that healthy dietary strategies (0.52), self-monitoring (0.40), psychological coping strategies (0.14), and habit strength for healthy eating (0.15) contributed independently and most (49.5% of variance; P = 0.0001) to discriminating the two groups.
Correlations with duration of weight loss, perceived effort, and quality of life
WLMs
Weight loss, magnitude of weight loss, duration of weight loss maintenance, perceived effort, and quality of life were explored in relation to practice of weight control strategies and habit strength among WLMs, adjusting for demographic covariates. WLMs with greater weight loss from WW start reported greater practice of strategies to support healthy dietary choices (r = 0.21; P = 0.0001), physical activity (r = 0.16; P = 0.0001), psychological coping (r = 0.21; P = 0.0001), and self-monitoring (r = 0.19; P = 0.0001), as well as greater habit strength for healthy eating (r = 0.23; P = 0.0001) and physical activity (r = 0.15; P = 0.0001). WLMs with a longer duration of weight loss maintenance reported greater habit strength for healthy eating (r = 0.05; P = 0.004), but duration was not related to habit strength for physical activity or practice of weight control strategies. WLMs with lower perceived effort to maintain their current body weight reported more frequent practice of healthy dietary choices (r = −0.06; P = 0.0001) and psychological coping strategies (r = −0.13; P = 0.0001), as well as greater habit strength for healthy eating (r = −0.18; P = 0.0001). Perceived effort was not related to self-monitoring or physical activity strategies. Finally, higher quality of life scores were related to more frequent practice of healthy dietary choices (r = 0.19; P = 0.0001), physical activity strategies (r = 0.28; P = 0.0001), self-monitoring (r = 0.16; P = 0.0001), and psychological coping strategies (r = 0.19; P = 0.0001), as well as greater habit strength for healthy eating (r = 0.17; P = 0.0001) and physical activity (r = 0.28; P = 0.0001).
Controls
Similar correlational analyses were conducted among controls to examine relationships between perceived effort, quality of life, practice of weight control strategies, and habit strength, adjusting for demographic factors. Higher quality of life scores were related to more frequent practice of physical activity (r = 0.15; P = 0.0004) and psychological coping (r = 0.16; P = 0.002) strategies as well as greater habit strength for physical activity (r = 0.20; P = 0.0001). Perceived effort was not related to habit strength or weight control strategies.
Discussion
This is the first study to use validated and standardized questionnaires to examine habit strength and the specific weight control behaviors and psychological coping approaches used by WLMs in a widely available commercial weight management program. WLMs reported more frequent engagement in several healthy dietary, self-monitoring, and psychological coping strategies and reported greater habit strength for healthy eating that differentiated them from weight-stable individuals with obesity. Future weight loss interventions may seek to emphasize these components in building effective weight loss maintenance programs.
Habit strength in healthy eating emerged as a defining characteristic among WLMs, suggesting greater frequency, repetition, and automaticity in healthy eating choices. Observational survey studies of convenience samples with measures of habit strength have found that stronger exercise and healthy eating (e.g., fruit intake) habits were related to less perceived effort to engage in these behaviors and greater persistence in engagement in these behaviors (27-29). In an experimental study, longer-term practice of specific eating or activity behaviors in the same context (e.g., exercise after breakfast) was found to produce automaticity (30), allowing the behaviors to occur with less reported intentional effort (30, 31). The more complex the behavior, the longer it appears to take to develop habit automaticity (27, 30, 31). Similarly, in the current study, WLMs who maintained their weight the longest reported the greatest habit strength, and greater habit strength for healthy eating was related to less perceived effort to maintain their reduced body weight. In the National Weight Control Registry, the chance of longer-term success was found to increase in participants who had kept their weight off for 2 years or more, and the most successful registry members reported that it became easier to maintain a weight loss over time (32). Over time, healthy eating behaviors may become progressively easier, requiring less intentional effort. Future research is needed to replicate these findings and include other measures of automaticity (e.g., implicit association test).
Prior research from the National Weight Control Registry and the German and Portuguese Weight Control Registries of general populations has reported several global strategies associated with weight loss maintenance, including consuming a low-calorie diet, having high dietary restraint, self-monitoring (33), and engaging in high physical activity (1, 4, 33). The current study’s results complement these findings, providing specific eating, monitoring, and psychological coping strategies that may be integrated into future treatments to support long-term maintenance. The key behaviors (among the 54 items assessed in our measure) that emerged as greater among WLMs than controls included keeping low-calorie foods accessible, setting daily calorie goals, daily recording of calories, and measuring foods. Specific psychological coping strategies included “thinking about past successes” and “remaining positive in the face of weight regain.” These strategies may be emphasized in future intervention trial research.
Compared with weight-stable individuals with obesity, WLMs reported greater self-kindness and practice of mindfulness and acceptance strategies and they had particularly higher scores on the “willingness to ignore cravings” subscale; however, these strategies overall did not emerge as strong group discriminators. Both groups reported that, on average, they “sometimes” used the mindfulness and acceptance strategies. Clinical trial research using the same FAAQ questionnaire in the current study showed that acceptance and mindfulness approaches enhanced weight loss maintenance when practiced “frequently” to “almost always” (7). While the content of WW has changed over the years, WW has continued to emphasize balanced nutrition, self-monitoring of points (i.e., simplified system of calories), and behavioral strategies that include problem solving, stimulus control, and goal setting. Mind-set techniques, including self-compassion and mindfulness, were added to the curriculum in 2015. It is possible that greater emphasis of mindfulness and acceptance strategies in WW could have increased practice among WLMs compared with weight-stable individuals with obesity. Also, the internal validity of the FAAQ (α = 0.57) was lower in the current study than in published validation studies (19), and thus the questionnaire might not have adequately measured the constructs as desired. Findings overall suggested that other strategies were more important in distinguishing WLMs from weight-stable individuals with obesity.
Successful weight loss is associated with a variety of benefits, including increased quality of life (16). This study is novel in suggesting that specific weight control strategies and habit strength were related to improved overall quality of life. In both groups, higher quality of life was related to greater habit strength and practice of physical activity strategies and more psychological coping strategies. Additionally, among WLMs, higher quality of life was related to greater practice of self-monitoring and dietary strategies and greater habit strength for healthy eating. Improved quality of life may serve as a motivator for continued weight loss maintenance, and it has been shown in other studies to modestly predict participants’ ability to maintain long-term weight loss (34).
This study’s strengths include novel evaluation of WLMs from a widely used commercial weight loss program and use of validated questionnaires. The study included nearly 5,000 WLMs as well as a comparison group. To avoid type I error, P values were adjusted and effect sizes were used to guide data interpretation. The cross-sectional, two-group study was designed to be hypothesis generating and to help inform future avenues of research. However, causality cannot be inferred. The study did not evaluate prospective changes in weight status over time. Thus, whether the reported behavioral and psychological factors led to successful weight maintenance is unknown. Also, WLMs and weight-stable individuals with obesity were self-selected, and the groups differed on several demographic factors, including age, sex, income, education, and employment. While the analyses were adjusted for these factors, the observed behavioral and psychological differences could have been due to other unmeasured factors. Generalizability of these findings to other commercial programs or the general population of WLMs, and in particular to more socioeconomically and ethnically diverse populations, remains unknown.
Lifestyle interventions typically include an armament of strategies to help promote successful weight control. The practical implications of the current study’s findings are to highlight some key strategies that most characterized successful WLMs in a large, commercial weight management program: keeping low-calorie foods accessible, setting daily intake goals, recording daily intake, measuring foods, thinking about past successes, and remaining positive in the face of weight regain. More frequent practice of these dietary, self-monitoring, and psychological coping strategies and development of greater habit strength differentiated long-term WLMs from weight-stable individuals with obesity. Future research should consider emphasizing these components in development of effective weight maintenance programs.
Acknowledgments
We thank all the participants in the WW Success Registry as well as Rena R. Wing, PhD, and James O. Hill, PhD, for creating the National Weight Control Registry that inspired the proposed work.





