Waist Circumference Change is Associated with Blood Pressure Change Independent of BMI Change
Abstract
Objective
This study aimed to understand how an increase in abdominal adiposity relative to overall adiposity is associated with blood pressure (BP) change.
Methods
A sex-stratified mixed linear model was used to examine the association (95% CI) between annual changes in waist circumference (WC) and systolic blood pressure and diastolic blood pressure, estimated from two to eight repeated measures across the 1993-2015 China Health and Nutrition Survey, among 5,742 men and 5,972 women (18-66 years) with no history of antihypertension medication use.
Results
The association between annual WC change and BP change remained statistically significant but was attenuated after controlling for annual BMI change, regardless of baseline abdominal obesity or overweight status. Each 10-cm annual WC gain in men and women was associated with a 0.98-mm Hg (95% CI: 0.61-1.35) and a 0.97-mm Hg (95% CI: 0.62-1.32) annual increase in systolic blood pressure and a 1.13-mm Hg (95% CI: 0.87-1.38) and a 0.74-mm Hg (95% CI: 0.51-0.97) annual increase in diastolic blood pressure, respectively, independent of annual BMI change.
Conclusions
WC gain may elevate BP even in the absence of BMI gain. BP management that addresses only BMI gain could overlook individuals at risk of elevated BP who have increased WC but not BMI.
Study Importance
What is already known?
- Elevated blood pressure is a leading global health risk, especially in China, where the absolute burden of elevated blood pressure is the largest worldwide.
- There is limited research on whether waist circumference gain disproportionate to BMI gain is related to changes in blood pressure.
What does this study add?
- With 22 years of follow-up, this study adds to the evidence that waist circumference is positively associated with blood pressure, independent of increases in BMI, in Chinese adults.
- This study provides a longer period of follow-up, a more diverse population, and a more robust set of confounders, including diet and physical activity, than previous studies in China.
Introduction
Measures of overall and abdominal obesity (i.e., BMI and waist circumference [WC]) have increased substantially in Western and Asian adult populations over the past decades, with more increases in WC than expected from change in BMI alone (1-3). In particular, the largest disproportional increases in WC relative to BMI occurred in Mexico and China, compared with the US and England (1), indicating that these populations have experienced an excess accumulation of abdominal adiposity. Because WC is a stronger predictor for cardiometabolic risk factors, including elevated blood pressure (BP), than BMI in Chinese adults and in meta-analyses of multiethnic studies (4, 5), the disproportionate increase in WC relative to BMI may contribute to adverse BP change.
Several studies have investigated the relationship between WC change and incidence of elevated BP in Chinese adults (6-9), yet few have examined the association between WC change and BP change. It is more informative to quantify the estimated BP change than the elevated BP risk associated with WC change because systolic blood pressure (SBP) and diastolic blood pressure (DBP) are strongly and positively associated with cardiovascular diseases and vascular and overall deaths with no apparent threshold (10, 11). In a meta-analysis of 1 million adults from 61 prospective observational studies, including Chinese adults, each 20-mm Hg increase in SBP or 10-mm Hg increase in DBP doubled the death rates of stroke, heart disease, and other vascular causes at ages 40 to 49 years (10). Additionally, it is largely unknown how WC gain disproportionate to BMI gain is related to BP change, particularly in Asian populations (1, 3). Whereas the pathogenesis of weight-induced BP elevation is through the activation of the sympathetic nervous system (12), the mechanisms linking WC to elevated BP were shown to involve the accumulation of abdominal visceral adipose tissue (13). The increase in WC may contribute to BP change independent of BMI gain. However, few epidemiological studies have examined this independent relationship between changes in WC and BP.
Therefore, we aimed to quantify the association of WC change with changes in SBP and DBP independent of concurrent BMI changes within individuals. We used longitudinal data from eight visits in the population-based China Health and Nutrition Survey (CHNS) representing rural and urban communities in nine provinces from 1993 to 2015. The CHNS data provide rich sociodemographic, health behavior, and health status data, allowing us to account for a wide range of confounders. Whereas the prevalence of elevated BP increased from 13% in 1991 to 28% in 2009, diagnosis and treatment among individuals with elevated BP remained below 50% (14). Thus, despite high prevalence of elevated BP in CHNS adults, the prevalence of hypertension diagnosis and treatment are low, allowing us to study the natural history of BP change without the effects of medication.
Methods
CHNS
The CHNS is a longitudinal study that was started in 1989, with subsequent surveys every 2 to 4 years for a total of 10 rounds of surveys until 2015. The primary CHNS surveys took place in nine provinces in China, using a multistage, random-cluster design, with three additional megacities included in 2011 and three additional provinces included in 2015, giving a total sample of about 7,200 households with more than 30,000 participants. The CHNS was designed to capture urban-rural differences in selected provinces and megacities, and it is not nationally representative. Survey procedures have been described in more detail elsewhere (15). The study met the standards for the ethical treatment of participants, and it was approved by the institutional review boards of the University of North Carolina at Chapel Hill; the China-Japan Friendship Hospital, Ministry of Health of the People’s Republic of China; and the National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention.
Outcome measures
BP was measured three times using standard mercury sphygmomanometers, with a 30-second interval between cuff inflation, on the right arm after 10 minutes of seated rest by experienced physicians, who had completed a 7-day training session and passed a comprehensive test for the reliability of BP measurement. The average of the three BP measures was used in analyses. High BP was defined as SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg (16). We estimated annualized changes in SBP and DBP per year by dividing the changes in SBP and DBP between surveys by the number of years between surveys, assuming constant changes in SBP and DBP per year.
Primary exposure
WC was measured to the nearest 0.1 cm at midway between the lowest rib and iliac crest using nonelastic tape. We estimated annual WC change by dividing the WC change between surveys by the number of years between surveys, assuming a constant change in WC per year. Abdominal obesity was defined as WC ≥ 85 cm in men and WC ≥ 80 cm in women using the Chinese cut point (17).
Covariates
Weight was measured to the nearest 0.1 kg in light clothing using calibrated beam scales. Height was measured without shoes to the nearest 0.1 cm using portable stadiometers. BMI was calculated as weight in kilograms divided by height in meters squared. We estimated annual BMI change by dividing BMI change between surveys by the number of years between surveys, assuming a constant BMI change per year. We used a single category of BMI ≥ 24 kg/m2 to define overweight and obesity, according to the Chinese cut point (17).
Energy intake and sodium intake were estimated based on three consecutive 24-hour dietary recalls and household food inventories using a Chinese food composition table (18). Energy intake was validated by doubly labeled water (r2 = 0.56 for men; r2 = 0.60 for women) (19), and sodium intake was validated by urinary sodium excretions using 24-hour urine samples (correlation coefficients: 0.58; P = 0.005) (20). We used year-specific tertiles of total physical activity, estimated from self-reported 7-day recalls of occupational, transportation, domestic, and leisure activities, to define low, medium, and high activity level. Based on self-reports, we categorized individuals as smokers if they smoked cigarettes during the baseline or follow-up survey periods, and we categorized alcohol consumers as those who drank alcohol during the year prior to the baseline or follow-up surveys.
We dichotomized educational attainment to below high school versus high school or above. Household income was measured by detailed reports of all income activities of all household members. We defined low-, medium-, and high-income levels using year-specific tertiles of per capita household income. We generated a household asset score with a maximum of seven points that represented whether any household member owned the following items: a color TV, refrigerator, microwave oven, electrical cooking pot, air conditioner, electric fan, and camera. We used year-specific tertiles of a validated community-level, multidimensional, 12-component urbanization index (21), derived from household and community surveys, to define low, medium, and high urbanization.
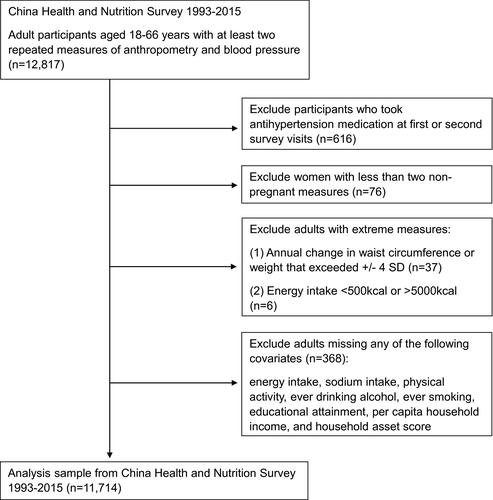
Study population
Individuals eligible for the current analysis were adults aged 18 to 66 years who participated in at least two primary CHNS surveys from 1993 to 2015 (1993, 1997, 2000, 2004, 2006, 2009, 2011, and 2015) with repeated anthropometric and BP measurements (n = 12,817; Figure 1). We excluded adults aged 66 years and older to minimize potential effects of weight loss due to sarcopenia (age-related loss of skeletal muscle mass) (22). We then excluded measures of participants after the first report of antihypertension medication use (n = 616), as well as measures of women who were pregnant during surveys (n = 76) to ensure that changes in WC and weight captured weight and waist gain, not pregnancy changes. We excluded high outliers of annual changes in WC (mean [4 SDs]: 0.50 [10.14] cm) and BMI (mean [4 SDs]: 0.11 [2.47] kg/m2) because these changes might indicate data errors and unmeasured conditions such as injury and disease, which resulted in an additional exclusion of 37 individuals. We further excluded individuals who reported implausible energy intake, estimated by three consecutive 24-hour diet recalls and household inventories (< 500 kcal or > 5,000 kcal; n = 6), and individuals missing any of the following covariates at baseline (n = 368): educational attainment, energy intake, sodium intake, physical activity, alcohol intake, smoking, per capita household income, and household asset score. The final analysis sample had 11,714 adults, with a total of 33,523 observations for change measures.
Statistical analyses
We presented continuous variables as means (SD) and categorical variables as proportions. We compared the characteristics of men and women at the first entry to the survey using t tests for continuous variables and χ2 tests for categorical variables. We used linear mixed models with a random intercept for the individual to estimate the average years between change measures and annual changes in WC, BMI, SBP, and DBP stratified by sex.
We used sex-stratified linear mixed models to estimate the associations between annual changes in WC and SBP and DBP to allow both fixed and random effects, adjusting for the above covariates (baseline age, WC, BMI, height, SBP or DBP, energy intake, sodium intake, smoking, alcohol drinking, physical activity, educational attainment, per capital household income, household asset score, urbanization index, province, and survey year) in model 1 and additionally including annual change in BMI in model 2. We annualized changes in WC, SBP, and DBP and adjusted for baseline age in the model to account for age-related changes in WC and BP (23, 24). We added random intercepts for the community, household, and individual to account for repeated measures within communities, households, and individuals. To consider the potential that the relationship between WC and BP varied by baseline WC and/or BMI levels, we tested for their interaction terms in models 1 and 2. We assessed significance for these interaction terms at a 10% level of significance (P < 0.10). It was decided a priori that if these interactions were not statistically significant, they would be dropped from the final analysis model.
To test whether transition in abdominal obesity was associated with BP change, we categorized transitions in abdominal obesity between surveys to the following groups: maintained normal WC (normal WC at baseline and follow-up), which was the referent group; incident abdominal obesity (normal WC at baseline and abdominal obesity at follow-up); reversed abdominal obesity (abdominal obesity at baseline and normal WC at follow-up); and persistent abdominal obesity (abdominal obesity at baseline and follow-up). We used the same linear mixed models (Models 1 and 2) to examine the association of these transitions in abdominal obesity with annual changes in SBP and DBP, with additional control for years between surveys because transitions in abdominal obesity were more likely to occur during longer follow-ups.
We conducted all statistical analyses using Stata software version 14 (StataCorp, College Station, Texas). All statistical tests were two-tailed and were assessed at a 5% level of significance (P < 0.05) for main effects, with the exception of the 10% level of significance for interaction (P < 0.10).
Sensitivity analysis
To assess the sensitivity of the associations between changes in WC and SBP and DBP to long periods of follow-up (22-year maximum) due to missed interim visits, we excluded changes estimated from more than a 10-year interval (675 observations).
Results
Compared with men, women were slightly older, resided in more urbanized areas, and had lower WC, height, SBP, DBP, energy intake, sodium intake, and proportions of high school completers but higher BMI, household asset scores, numbers of survey visits, and proportions with abdominal obesity and overweight (Table 1). There were considerably more men (13.25%) with untreated high BP than women (7.62%). Whereas 72.64% and 79.12% of men were smokers (smoked cigarettes during survey periods) and alcohol consumers (consumed alcohol during the past years of surveys), respectively, only 4.69% and 17.30% of women were smokers and alcohol consumers, respectively. The mean WC, BMI, SBP, and DBP increased across surveys for men and women (Table 2), with an average of 3.80 and 3.57 years between change measures in men and women, respectively.
| Men (n = 5,742) | Women (n = 5,972) | P valueb | |
|---|---|---|---|
| Age, mean (SD), y | 37.28 (11.96) | 37.86 (11.21) | 0.007 |
| SBP, mean (SD), mm Hg | 116.66 (13.34) | 111.74 (14.25) | < 0.001 |
| DBP, mean (SD), mm Hg | 76.99 (9.68) | 73.65 (9.77) | < 0.001 |
| High BP, % c | 13.25 | 7.62 | < 0.001 |
| WC, mean (SD), cm | 78.76 (9.49) | 75.58 (8.79) | < 0.001 |
| Abdominal obesity, % d | 25.88 | 30.31 | < 0.001 |
| BMI, mean (SD) | 22.20 (2.90) | 22.33 (3.06) | 0.024 |
| Overweight, % d | 24.12 | 26.61 | 0.002 |
| Height, mean (SD), cm | 167.03 (6.43) | 156.15 (5.96) | < 0.001 |
| Energy intake, mean (SD), kcal | 2,517.95 (660.38) | 2,171.15 (596.17) | < 0.001 |
| Sodium intake, mean (SD), mg | 5,841.75 (2,988.59) | 5,506.80 (2,809.43) | < 0.001 |
| Physical activity, % e | < 0.001 | ||
| Low | 34.55 | 30.46 | … |
| Medium | 34.45 | 32.80 | … |
| High | 31.00 | 36.74 | … |
| Alcohol consumer, % f | 79.12 | 17.30 | < 0.001 |
| Smoker, % g | 72.64 | 4.69 | < 0.001 |
| Completed high school education, % | 28.07 | 22.04 | < 0.001 |
| Per capita household income, % h | 0.241 | ||
| Low | 31.96 | 33.37 | … |
| Medium | 34.26 | 33.22 | … |
| High | 33.79 | 33.41 | … |
| Household asset score, mean (SD) i | 2.46 (1.82) | 2.60 (1.85) | < 0.001 |
| Urbanization, % j | 0.079 | ||
| Low | 33.42 | 31.80 | … |
| Medium | 32.29 | 32.12 | … |
| High | 34.29 | 36.09 | … |
| Year of study entry, % | < 0.001 | ||
| 1993 | 39.62 | 39.77 | … |
| 1997 | 22.24 | 18.85 | … |
| 2000 | 12.68 | 12.98 | … |
| 2004 | 9.58 | 10.85 | … |
| 2006 | 4.65 | 4.76 | … |
| 2009 | 8.36 | 8.82 | … |
| 2011 | 2.87 | 3.97 | … |
| Number of survey visits, mean (SD) | 2.84 (1.72) | 2.98 (1.83) | < 0.001 |
- a First study visit may be study baseline (1993) or first visit after 1993 for participants who entered survey over course of follow-up. Latest year for first survey entry was 2011 because all eligible participants had at least two survey visits. Year of entry varies because of household-based design affected by family formation, childbirth, and replacement enrollment using identical sampling techniques.
- b t test and χ2 test used to compare continuous and categorical variables, respectively, between men and women.
- c High BP defined as SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg (16).
- d According to Chinese cutoff point (17), abdominal obesity defined as WC ≥ 85 cm in men and WC ≥ 80 cm in women, and overweight or obesity defined as BMI ≥ 24.
- e Physical activity in metabolic equivalent of task per week was categorized into year-specific tertiles to represent low, medium, and high levels of physical activity.
- f Participants who consumed alcohol during the past year of surveys.
- g Participants who smoked cigarettes during surveys.
- h Per capita household income categorized into year-specific tertiles to represent low, medium, and high levels of income.
- i Asset score ranged from 0 to 7, with each asset (color TV, refrigerator, microwave oven, electrical cooking pot, air conditioner, electric fan, and camera) worth 1 point.
- j Urbanization index, a 12-component scale that includes population density, economic activity, transportation infrastructure, sanitation, etc., to define and distinguish urbanicity, was categorized into year-specific tertiles to represent low, medium, and high levels of urbanization (21).
| Men (16,037 observations)b | Women (17,486 observations)b | |
|---|---|---|
| Years between change measures | 3.80 (3.77-3.84) | 3.57 (3.54-3.60) |
| Annual change in WC, cm | 0.53 (0.50-0.57) | 0.47 (0.44-0.51) |
| Annual change in BMI | 0.12 (0.11-0.12) | 0.10 (0.09-0.11) |
| Annual change in SBP, mm Hg | 0.72 (0.64-0.80) | 0.81 (0.73-0.88) |
| Annual change in DBP, mm Hg | 0.37 (0.31-0.42) | 0.35 (0.29-0.40) |
- a Estimated using sex-stratified linear mixed models with random intercept for individual to account for repeated measures.
- b Number of observations for changes measured.
There was no evidence (P > 0.10) for any interaction of annual change in WC with baseline abdominal obesity status or overweight status, and thus these interactions were not included in the analysis. The associations between annual WC change and annual SBP and DBP changes were not different by baseline abdominal obesity status and overweight status (Supporting Information Tables S1-S2). Annual change in WC was significantly associated with annual change in SBP and DBP without accounting for concurrent BMI change (Table 3). Each 10-cm increase in WC per year was associated with a 2.06-mm Hg (95% CI: 1.73-2.39) increase in SBP and a 1.74-mm Hg (95% CI: 1.51-1.97) increase in DBP per year in men. In women, each 10-cm increase in WC per year was associated with a 1.69-mm Hg (95% CI: 1.37-2.01) increase in SBP and a 1.20-mm Hg (95% CI: 0.99-1.42) increase in DBP per year. When holding annual BMI change constant, the association between annual changes in WC and SBP and DBP was attenuated but remained statistically significant (Table 3). Among men, each 10-cm increase in WC per year was associated with a 0.98-mm Hg (95% CI: 0.61-1.35) increase in SBP and a 1.13-mm Hg (95% CI: 0.87-1.38) increase in DBP per year, independent of annual increase in BMI. Among women, each 10-cm increase in WC per year was associated with a 0.97-mm Hg (95% CI: 0.62-1.32) increase in SBP and a 0.74-mm Hg (95% CI: 0.51-0.97) increase in DBP per year, independent of annual increase in BMI.
| Observations for change measures | Annual change in SBP | Annual change in DBP | |||
|---|---|---|---|---|---|
| Model 1b | Model 2c | Model 1b | Model 2c | ||
| Men | 16,037 | 2.06 (1.73-2.39) | 0.98 (0.61-1.35) | 1.74 (1.51-1.97) | 1.13 (0.87-1.38) |
| Women | 17,486 | 1.69 (1.37-2.01) | 0.97 (0.62-1.32) | 1.20 (0.99-1.42) | 0.74 (0.51-0.97) |
- a Annual changes in SBP, DBP, WC, and BMI estimated from repeated measures.
- b Adjusted for age, WC, BMI, height, SBP or DBP, energy intake, sodium intake, physical activity, ever completed a high school education, ever smoked or drank alcohol during survey year, urbanization level, income level, household asset score, province, and survey year at baseline measure for change calculation.
- c Adjusted for variables in model 1 as well as for annual change in BMI.
Transition in abdominal obesity status between surveys was significantly associated with annual SBP and DBP changes (Table 4). Compared with participants who maintained normal WC, participants who had incident and persistent abdominal obesity had increased SBP and DBP. Compared with maintenance of normal WC between surveys, incident abdominal obesity between surveys was associated with a 0.84-mm Hg (95% CI: 0.63-1.05) and a 0.62-mm Hg (95% CI: 0.42-0.83) greater annual change in SBP in men and women, respectively, and with a 0.71-mm Hg (95% CI: 0.56-0.86) and a 0.55-mm Hg (95% CI: 0.41-0.69) greater annual change in DBP in men and women, respectively. After holding annual BMI change constant, annual changes in SBP and DBP associated with abdominal obesity at follow-up decreased but remained statistically significant (Table 4). Compared with maintenance of normal WC between surveys, incident abdominal obesity between surveys was associated with a 0.43-mm Hg (95% CI: 0.21-0.65) and a 0.37-mm Hg (95% CI: 0.16-0.58) greater annual SBP change in men and women, respectively, and with a 0.45-mm Hg (95% CI: 0.30-0.60) and a 0.39-mm Hg (95% CI: 0.25-0.53) annual DBP change in men and women, respectively, holding annual BMI change constant.
| Transition in abdominal obesity status | Observations for change measures (%) | Annual change in SBP | Annual change in DBP | ||
|---|---|---|---|---|---|
| Model 1c | Model 2d | Model 1c | Model 2d | ||
| Men | |||||
| Maintained normal WC | 8,238 (51.37) | Reference | Reference | Reference | Reference |
| Incident abdominal obesity | 2,469 (15.40) | 0.84 (0.63 to 1.05) | 0.43 (0.21 to 0.65) | 0.71 (0.56 to 0.86) | 0.45 (0.30 to 0.60) |
| Reversed abdominal obesity | 1,192 (7.43) | −0.14 (−0.47 to 0.19) | −0.01 (−0.34 to 0.32) | −0.07 (−0.30 to 0.16) | 0.01 (−0.22 to 0.23) |
| Persistent abdominal obesity | 4,138 (25.80) | 0.58 (0.29 to 0.87) | 0.20 (−0.09 to 0.50) | 0.52 (0.31 to 0.72) | 0.28 (0.07 to 0.48) |
| Women | |||||
| Maintained normal WC | 7,729 (44.20) | Reference | Reference | Reference | Reference |
| Incident abdominal obesity | 2,778 (15.89) | 0.62 (0.42 to 0.83) | 0.37 (0.16 to 0.58) | 0.55 (0.41 to 0.69) | 0.39 (0.25 to 0.53) |
| Reversed abdominal obesity | 1,472 (8.42) | −0.02 (−0.33 to 0.28) | 0.05 (−0.26 to 0.35) | −0.01 (−0.21 to 0.20) | 0.04 (−0.16 to 0.24) |
| Persistent abdominal obesity | 5,507 (31.49) | 0.83 (0.55 to 1.11) | 0.58 (0.30 to 0.86) | 0.62 (0.44 to 0.81) | 0.46 (0.28 to 0.65) |
- a Abdominal obesity defined as WC ≥ 85 cm in men and WC ≥ 80 cm in women, according to Chinese cutoff point (17). Maintained normal WC defined as normal WC at baseline and at follow-up. Incident abdominal obesity defined as normal WC at baseline and abdominal obesity at follow-up. Reversed abdominal obesity defined as abdominal obesity at baseline and normal WC at follow-up. Persistent abdominal obesity defined as abdominal obesity at baseline and at follow-up.
- b Annual changes in SBP, DBP, WC, and BMI estimated from repeated measures.
- c Adjusted for age, WC, BMI, height, SBP or DBP, energy intake, sodium intake, physical activity, ever completed a high school education, ever smoked or drank alcohol during survey year, urbanization level, income level, household asset score, province, and survey year at baseline measure for change calculation, as well as for years between surveys.
- d Adjusted for variables in model 1 as well as for annual change in BMI between surveys.
In the sensitivity analysis, we tested whether our results were sensitive to long intervals between follow-ups due to missed interim visits. Compared with our findings using the full sample, the effect estimates of associations of annual WC change (Supporting Information Table S3) and transitions in abdominal obesity (Supporting Information Table S4) with annual SBP and DBP changes varied within a magnitude of 0.03 mm Hg when we excluded changes estimated from measures with more than a 10-year interval (675 observations).
Discussion
Consistent with global trends (25-29), the mean WC, BMI, SBP, and DBP increased between surveys from 1993 to 2015 among men and women aged 18 to 66 years in the CHNS who had not taken antihypertension medication. We found positive associations between annual changes in WC and SBP and DBP in Chinese men and women, independent of the concurrent annual BMI change and regardless of baseline abdominal obesity status and overweight status. We also found that incident and persistent abdominal obesity between surveys were associated with larger annual increases in SBP and DBP compared with maintenance of normal WC between surveys, independent of annual BMI change.
Whereas prior studies examining the association between WC change and incident hypertension among Asian adults have not considered baseline hypertension or high-normal BP at follow-up (6-9), the CHNS includes a large proportion of individuals without hypertension and/or treatment for hypertension (14, 30). Thus, we were able to quantify the natural history of BP change associated with WC change without the nuisance of treatment effects and regardless of hypertension threshold. This is a critical contribution because a prospective meta-analysis of 1 million adults, including Chinese adults, found a steep dose-response relationship between SBP and DBP and vascular and overall mortality (10). Although our findings for annual SBP and DBP increases (0.74-1.13 mm Hg) per 10-cm annual WC gain independent of annual BMI change were modest, a small population-wide BP shift could have substantial impacts on risk of cardiovascular diseases (11). In the Atherosclerosis Risk in Communities Study, a 1-mm Hg SBP reduction was associated with 20.3 and 13.3 fewer heart failure events per 100,000 person-years in African American and white patients, respectively (11). Because WC is a simple marker for abdominal subcutaneous and visceral fat (13, 31), our results suggest that an accumulation of abdominal fat may elevate SBP and DBP in Chinese adults, even in the absence of BMI gain and even in individuals without abdominal obesity or overweight.
Our findings show a strong association between WC gain and BP increase and are consistent with those of previous studies in Chinese populations (6-9). A prospective study conducted among rural adults older than 18 years from of age Luoyang, China, found that regardless of baseline abdominal obesity status, greater 6-year hypertension risk was associated with > 5% WC gain relative to within 2.5% WC change and was associated with abdominal obesity at follow-up versus normal WC at baseline and follow-up (8). However, this study did not examine whether this association was independent of concurrent BMI gain (8). It is important to understand this independent association because disproportionate increases in WC and weight have been widely observed in Asian and Western populations (1-3). To our knowledge, only two studies of southern Chinese adults have accounted for the concurrent BMI gain correlated with WC gain (6, 7, 9). Luo et al. (6, 9) found that the positive association between 2-year WC change and incident hypertension was independent of 2-year BMI change and was stronger than the association between 2-year BMI change and incident hypertension among adults aged 35 to 74 years from Jiangsu Province. Chuang et al. (7) reported that WC change was associated with BP and hypertension incidence at the 10-year follow-up, independent of BMI change, among nondiabetic adults older than 30 years of age from the island of Quemoy. Nevertheless, these studies used data from small parts of southern regions (6, 7, 9), which may not be generalizable to Chinese adults in other regions with diverse cultures and environments. Our study used the population-based CHNS and provides a broader picture of the diverse Chinese population than these smaller studies. In addition, these smaller studies did not address potential confounding from energy intake, sodium intake, and physical activity (6, 7, 9), whereas we accounted for these potential lifestyle confounders using three consecutive high-quality 24-hour diet recalls and a 7-day physical activity recall, respectively.
The strengths of our study include the large population-based study cohort, the longitudinal design, multiple follow-up visits over 22 years, and low treatment for elevated BP, which allowed us to examine the association between longitudinal changes in WC and BP in the diverse Chinese adult population. Additionally, we had rich data on health behavior and sociodemographic information and high-quality WC, BMI, and BP data measured by trained examiners at each survey visit; thus, we were able to examine the relationship between well-measured changes in WC and BP after controlling for a comprehensive set of confounders.
Our study is not without limitations. A potential limitation of our study is the wide range of follow-up periods from 2 to 22 years because the association between short- and long-term changes in WC and BP may be different and the assumption of constant rates of WC, BMI, and BP changes may be more likely to be violated in long intervals between follow-ups. Nonetheless, our sensitivity analyses, which excluded estimates over long follow-ups (≥ 10 years), suggest that our results are not sensitive to the length of survey intervals (Supporting Information Tables S3-S4). Lastly, we may not have enough statistical power to detect interactions of WC change with baseline abdominal obesity and overweight status. However, our stratified results for the association between WC change and BP change (Supporting Information Tables S1-S2) show no evidence for effect-measure modification by baseline abdominal obesity or overweight status.
In conclusion, our findings add to the evidence that WC gain is associated with BP increase, independent of BMI gain and regardless of baseline abdominal obesity and overweight status, in Chinese adults. Our unique study quantifies the association between WC change and BP change among a population-based Chinese adult cohort with low treatment for elevated BP, with comprehensive control for confounding. Given that WC provides an inexpensive and simple method to estimate abdominal fat distribution in various settings (13), WC should be monitored as an independent risk factor for elevated BP in health surveillance. Our findings suggest that BP management strategies aimed at addressing only overall overweight or obesity may overlook individuals at risk of elevated BP who gained WC but not BMI.
Acknowledgments
We are grateful to the participants of the CHNS.





