A 9-year, bidirectional prospective analysis of depressive symptoms and adiposity: The African American Health Study
Funding agencies: This research was supported by National Institute on Aging grant R01 AG010436.
Disclosure: The authors declared no conflict of interest.
Author contributions: All authors were involved in writing the article and had final approval of the submitted version.
Abstract
Objective
Depression may be a predictor and consequence of obesity. However, available evidence for racial minorities has been inconsistent, and more prospective studies are needed. Thus, this study's objective was to examine whether depressive symptom severity is a predictor and/or consequence of total adiposity over a 9-year period in a representative sample of late middle-aged African-Americans.
Methods
A total of 410 participants (aged 49–65 years; baseline) in the prospective cohort African American Health study were examined. Depressive symptom severity was assessed with the Center for Epidemiologic Studies-Depression Scale (CES-D). Total body fat percent (BF%) and body mass index (BMI; kg/m2) were assessed. Structural equation models were tested.
Results
All model fit statistics, other than χ2, indicated good fit (RMSEA ≤ 0.058, SRMR ≤ 0.052, CFI ≥ 0.95). Baseline CES-D did not predict 9-year changes in BF% (β = −0.01, P = 0.78) or BMI (β = −0.01, P = 0.77). Baseline BF% (β = 0.05, P = 0.39) and BMI (β = 0.08, P = 0.095) did not predict 9-year change in CES-D.
Conclusions
Depressive symptom severity was not a predictor or consequence of excess total adiposity in late middle-aged African-American adults. Including a depression module in obesity prevention and treatment programs specifically designed for late middle-aged African-Americans may not have a beneficial effect on obesity outcomes.
Introduction
Depression and obesity are highly prevalent, disabling conditions (1, 2). Approximately, 17% of adults will suffer from major depressive disorder in their lifetime (3), and almost 36% of U.S. adults are obese (body mass index; BMI ≥ 30 kg/m2) (4). Both depression and obesity are associated with poorer psychosocial outcomes (5, 6) and elevated risk for chronic physical disease (7). Prospective evidence suggests that depression is a risk factor for obesity, with odds ratios (OR) ranging from 1.18 to 2.57 (8). Depression as a consequence of obesity has also been documented with obesity conferring greater risk of developing clinical depression (OR = 2.15) or elevated depressive symptoms (OR = 1.36; 8).
The depression-obesity relationship has been found for both genders (8, 9) and across multiple race/ethnicities, including Caucasians and African-Americans (10-13). However, evidence indicates that the relationship may be moderated by gender and race/ethnicity, such that stronger relationships exist for non-Hispanic white women compared with nonwhites (14-17). In a nationally representative adult sample, Gavin et al. (14) detected a depression by race by gender interaction, such that obesity was cross-sectionally associated with depression in non-Hispanic white women but not in African-American, Hispanic, or Asian women (14). Race/ethnicity moderation has also been observed in adolescents, such that depression was prospectively related to obesity and vice versa for non-Hispanic white female adolescents but not for African-American or Hispanic females (15).
To summarize, although the depression-obesity relationship appears to be strong and consistent among non-Hispanic white females, especially adolescents, the relationship among adult minorities is less understood, given that most studies have used predominantly white, female samples (14). Moreover, many studies with adequate representation of African-Americans (14) were cross-sectional and cannot determine the directionality of observed depression-obesity relationships. These limitations are important because African-American adults, especially women, have the highest rates of obesity in the U.S. (4; i.e., 50% of African-Americans vs. 34% of non-Hispanic whites and 39% of Hispanics). To address these limitations, the objective of this prospective study was to examine whether depressive symptom severity is a predictor and/or consequence of total adiposity indicators over 9 years in a representative sample of late middle-aged African-American adults. This aim was achieved by testing the following hypotheses:
Hypothesis #1
Greater baseline severity of depressive symptoms is associated with greater 9-year increases in adiposity, as indicated by body fat percent (BF%) or BMI.
Hypothesis #2
Greater baseline BF% or BMI is associated with greater 9-year increases in depressive symptom severity.
This study analyzed data from the African American Health (AAH) study (18), which contains measures of depressive symptoms, BF%, and BMI at baseline and at a 9-year follow-up.
Methods
Participants
AAH is a prospective, representative cohort study of 998 noninstitutionalized late middle-aged African-Americans (aged 49-65 years at baseline) living in the St. Louis metropolitan area (18). Two city catchment areas were sampled using a multistage cluster design. Inclusion criteria were: (1) self-reported black or African-American race, (2) birth date between 01/1936 and 12/1950, (3) score ≥ 16 on the standardized Mini-Mental Status Examination, and (4) written informed consent. Of the eligible persons, 76% (998 of 1,320) were enrolled in the study from 2000 to 2001 (baseline). Of these, 58% (n = 579) were reassessed in 2009-2010 (9-year follow-up). Only participants with complete data for depressive symptoms, BF%, BMI, age, and gender at baseline and 9-year follow-up were selected, yielding a final sample of 410 participants for the primary analyses (see Table 1). Participants with complete data did not differ in age (P = 0.47) or BMI (P = 0.39) but were more likely to be female (P = 0.016) and have lower Center for Epidemiologic Studies Depression Scale (CES-D) scores (P < 0.001) and higher BF% (P = 0.010) compared with those with incomplete data. The Institutional Review Board of Saint Louis University approved all procedures.
| Baseline | 9-year follow-up | |||
|---|---|---|---|---|
| Mean or N | SD or % | Mean or N | SD or % | |
| Demographic and medical factors (units/range) | ||||
| Age (years) | 56.2 | 4.4 | - | - |
| Women | 268 | 65.4 | - | - |
| Education (years) | 12.4 | 3.0 | ||
| Income | ||||
| $10,000 or less | 37 | 10.5 | ||
| $10,000-$25,000 | 95 | 26.9 | ||
| $25,000-$35,000 | 62 | 17.6 | ||
| $35,000-$50,000 | 68 | 19.3 | ||
| $50,000-$75,000 | 63 | 17.8 | ||
| $75,000 or greater | 28 | 7.9 | ||
| Hypertension | 201 | 56.9 | ||
| Cardiovascular diseasea | 48 | 13.6 | ||
| Diabetes | 59 | 16.7 | ||
| Cancer | 17 | 4.8 | ||
| Kidney disease | 5 | 1.4 | ||
| Basic ADLs (0-7) | 0.4 | 1.1 | ||
| Instrumental ADLs (0-8) | 0.4 | 1.2 | ||
| Lower body functional limitations (0-5) | 1.1 | 1.5 | ||
| Depressive symptoms (range) | ||||
| CES-D (0-33) | 5.0 | 5.5 | 5.1 | 5.4 |
| CES-D score ≥ 16 | 26 | 6.3 | 26 | 6.3 |
| Adiposity indicators (units) | ||||
| BF% | 36.9 | 10.2 | 36.2 | 10.3 |
| BMI (kg/m2) | 31.0 | 6.3 | 31.5 | 6.6 |
| Normal weight (BMI 18.5-24.9) | 66 | 16.1 | 56 | 13.7 |
| Overweight (BMI 25.0-29.9) | 123 | 30.3 | 126 | 30.7 |
| Obese (BMI ≥ 30) | 218 | 53.2 | 225 | 54.9 |
| 9-year change | ||||
| CES-D change | - | - | 0.0 | 5.1 |
| BF% change | - | - | −0.7 | 7.0 |
| BMI change | - | - | 0.5* | 3.5 |
- Note: ADL: activities of daily living; CES-D: Center for Epidemiologic Studies Depression Scale.
- a Participants with coronary artery disease, angina, stroke, or congestive heart failure were coded as having cardiovascular disease.
- *P < 0.05 for paired-samples t test comparing baseline scores to 9-year follow-up scores.
Measures
Depressive symptom assessment
Depressive symptoms were assessed at baseline and 9-year follow-up with the 11-item Center for Epidemiologic Studies Depression Scale (CES-D; 19). Participants indicate how often they experienced symptoms during the last week using a scale ranging from 0 (rarely or none of the time) to 3 (most or all of the time). Higher scores indicate greater depressive symptom severity, with scores ≥ 16 indicative of clinically-relevant depressive symptoms (19). The CES-D has good internal consistency and construct validity (19). Baseline Cronbach's alpha was 0.83 and follow-up alpha was 0.84. Missing values (≤ two items) were imputed using within-person mean substitution.
Adiposity assessment
Both BF% and measured BMI were assessed in-home at baseline and 9-year follow-up. BF% was measured using bioelectrical impedence analysis (BIA) using a Tanita portable, electronic impedance scale (Tanita Corporation of America; Arlington Heights, IL), which adjusted electronically for gender, height, and weight. Participants' measured BMI was calculated (kg/m2). BF% was also measured for a subset of 204 participants (20.4%) at baseline using dual X-ray absorptiometry (DEXA). DEXA, a gold standard measure of adiposity, was used to validate the BIA measures of BF% and BMI. Baseline BF% and BMI were strongly correlated with DEXA scores (rs = 0.82 and 0.69, respectively), and test-retest reliability (median interval 19 days) was 0.93 for BF% and 0.99 for BMI. Thus, BIA measures of BF% and BMI were deemed valid adiposity indicators. Obesity has been defined categorically (20); however, the current study used continuous BMI because this approach maximizes variability and because degree of adiposity has shown a linear relationship with increased health risk (21).
Demographic covariates
Given their potential associations with depression and obesity, self-reported age (years) and gender (male = 0, female = 1) were included in the primary analyses as potential confounders. An exploratory fully adjusted model was also conducted which included the following factors: education (years), objective income (total annual household income ranging from ≤ $10,000 to ≥ $75,000), the presence or absence of hypertension, cardiovascular disease, diabetes, cancer, and chronic kidney disease (as determined by asking if participants had ever been told by a physician that they had a particular disease), and physical disability/limitations [as assessed by standard measures of basic and instrumental activities of daily living and lower body functional tasks (22)].
Procedure
Participants received detailed, in-home baseline (average 2.5 h) and 9-year follow-up (2 h) evaluations conducted by professional interviewers. Two-thirds of the baseline interviewers were African-American, and all were African-American for the 9-year follow-up. Interviewers asked questions from a standardized protocol and set up the measuring tape and Tanita scale for assessing participants' height, weight, and BF%. During baseline, a random subsample (20%) of AAH participants completed additional assessments (e.g., DEXA testing) at a clinical testing center.
Data analyses
SEM was the chosen primary analytic strategy instead of multiple regression given the nature of our cross-lagged panel data (two primary variables measured at two time points; 23). The advantage of SEM is that it allows the simultaneous entry of multiple outcomes in one model while also adjusting for all predictors (24). Because our moderately sized sample met the minimum participant-to-parameter ratio for SEM analyses, data were screened to evaluate SEM assumptions (25), which were met. A cross-lagged panel analysis was conducted using latent variable path analysis in LISREL 8.8 and the advocated two-step approach (25). The chi-square (χ2) statistic, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), and comparative fit index (CFI) were examined. The χ2 statistic should be small and nonsignificant to indicate acceptable fit (25); however, this statistic is sensitive to sample size, with larger samples typically generating a significant χ2, regardless of fit (25). The RMSEA should be ≤ 0.06 (26). The SRMR should be ≤ .08, whereas CFI should be ≥ 0.95.
Two models were constructed. Model #1 included the CES-D score and BF% at baseline and 9-year follow-up, and baseline age and gender. Model #2 used BMI in place of BF%. All variables except the CES-D were modeled as latent variables with a single item-level indicator and errors set to zero. The CES-D score had 11 item-level indicators. The “I felt sad” item was used for scaling. For the measurement model, all variables were freed to correlate. The error variances of baseline and follow-up CES-D indicators were set to covary. In the structural model, follow-up CES-D and BF% or BMI were adjusted for their baseline scores, and their errors set to covary. Each baseline variable was connected to both follow-up variables.
The exploratory fully-adjusted models were identical to Models #1 and #2 except the following baseline variables were added: education, income, chronic physical diseases, and level of disability. Each variable was modeled as a latent variable with a single indicator except the disability factor, which had three indicators. These confounders were linked to follow-up CES-D and BF% or BMI variables. All models were also run using the total sample (N = 998) and employing the full information maximum likelihood (FIML) estimation procedure in order to account for missing data. The results of the FIML analyses did not differ from those in the sample of 410 with complete data (not shown).
To facilitate comparison with past studies employing categorical approaches (16), we also ran supplemental regression analyses with dichotomous variables for depression (0 = not depressed, 1 = depressed) and BMI (0 = not obese, 1 = obese) using the CES-D cut point of ≥16 or higher (19) and the BMI cut point of ≥30 kg/m2.
Results
Nine-year change in depressive symptom severity and adiposity
CES-D, BF%, and BMI scores at baseline and follow-up are shown in Table 1. Paired-samples t tests revealed that, at the group level, the CES-D, t(409) = −0.08, P = 0.94, and BF% scores, t(409) = 1.96, P = 0.051, did not significantly change over the 9-year follow-up interval, whereas BMI showed a small increase over time, t(409) = 2.85, P = 0.005). Although the average scores were relatively stable at the group level, the standard deviations of the change scores were substantial (SDCESD change = 5.1, SDBF% change = 7.0, SDBMI change = 3.5). The distribution of the change scores was also normal and varied widely across the sample (See Figure 1). Both the standard deviations and distribution of change scores indicate that there were substantial individual differences in 9-year changes in depressive symptom severity and adiposity despite the stability of scores at the group level.
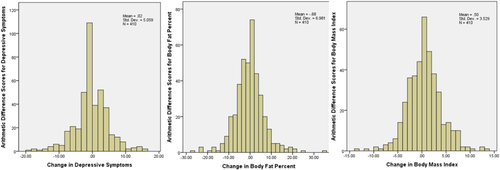
Distribution of change scores for depressive symptoms, BF%, and BMI. Change scores were calculated as arithmetic difference scores (follow-up score minus the baseline score). [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
BF% (Model #1)
The measurement model for Model #1 was specified as planned and showed adequate fit, as indicated by all the fit indices except the chi-square. Because a significant χ2 is very common in larger samples (25), the structural model was examined. The structural model fit statistics were identical to the measurement model's, and the individual structural paths were examined (see Figure 2). The structural path from baseline CES-D to 9-year BF% was not significant (β = −0.01, P = 0.78), indicating that baseline depressive symptom severity did not predict change in BF% over 9 years. The structural path from baseline BF% to 9-year CES-D was also not significant (β = 0.05, P = 0.39). These results show that baseline adiposity did not predict 9-year change in depressive symptom severity. Hence, neither Hypothesis 1 nor 2 was supported when BF% was examined. Baseline CES-D and BF% strongly predicted their corresponding follow-up scores (βs = 0.63 and 0.64, ps < 0.001). Baseline CES-D and BF% were not related (r = 0.05, P = 0.32), nor were follow-up CES-D and BF% (r = 0.04, P = 0.42). Greater 9-year increases in BF% was predicted by younger baseline age (β = −0.08, P = 0.01) and female gender (β = 0.21, P < 0.001). Age (β = 0.03, P = 0.48) and gender (β = 0.00, P = 0.98) were not predictors of CES-D change. Adding the additional demographic and medical covariates for the exploratory fully adjusted model did not change the results. Baseline CES-D did not predict 9-year BF% (β = −0.02, P = 0.60) or vice versa (β = 0.01, P = 0.86). Using dichotomized CES-D scores, baseline depression status did not predict 9-year changes in BF% (β = −0.02, P = 0.59).

Demographics-adjusted Model #1 for Hypotheses 1 and 2 using BF% over 9 years. Values for unidirectional arrows (structural paths) are standardized regression coefficients or factor loadings; values associated with bidirectional arrows are Pearson correlation coefficients. Black solid paths are significant (P < 0.05); gray dashed paths are not significant. Error terms and correlations with baseline age and sex are omitted for clarity.
BMI (Model #2)
Model #2 constructed with measured BMI had similar results (see Figure 3). Model #2 had good fit except for chi-square, so the structural paths were examined (Figure 3). The path from baseline CES-D to 9-year BMI was not significant (β = −0.01, P = 0.77). The path from baseline BMI to 9-year CES-D (β = 0.08, P = 0.095) was slightly stronger than in the BF% model but was still nonsignificant and weak. No correlations were detected between baseline (r = 0.02, P = 0.73) or follow-up (r = 0.03, P = 0.54) CES-D and BMI. These results also do not support Hypotheses 1 or 2, as they indicate that depressive symptoms did not predict 9-year change in BMI and that baseline BMI did not predict 9-year change in depressive symptoms. Baseline CES-D continued to predict its follow-up scores (β = 0.63, P < 0.001) with a similar magnitude as in Model #1. Baseline BMI was a strong predictor of its follow-up score (β = 0.84, P < 0.001). Younger baseline age (β = −0.08, P = 0.003) and female gender (β = 0.07, P = 0.014) predicted greater 9-year increases in BMI. Age (β = 0.03, P = 0.50) and gender (β = 0.01, P = 0.76) were not predictors of CES-D change. The exploratory fully adjusted model yielded similar results, as baseline CES-D did not predict 9-year BMI (β = 0.06, P = 0.13) or vice versa (β = 0.04, P = 0.45). When dichotomizing the CES-D and BMI scores, depression status did not predict changes in BMI (β = −0.01, P = 0.78) or vice versa (β = 0.019, P = 0.65).

Demographics-adjusted Model #2 for Hypotheses 1 and 2 using measured BMI over 9 years. Values for unidirectional arrows (structural paths) are standardized regression coefficients or factor loadings; values associated with bidirectional arrows are Pearson correlation coefficients. Black solid paths are significant (P < 0.05); gray dashed paths are not significant. Error terms and correlations with baseline age and sex are omitted for clarity.
Discussion
The hypothesis that greater baseline severity of depressive symptoms is associated with greater 9-year increases in total adiposity was not supported. Baseline CES-D scores did not significantly predict 9-year changes in BF% or BMI. When the reciprocal hypothesis was tested—that greater baseline total adiposity would be associated with greater 9-year increases in depressive symptom severity—it was also not supported. Baseline BF% and BMI did not predict 9-year changes in CES-D scores. Cross-sectional associations between depressive symptom severity and total adiposity indicators at baseline and follow-up were also nonsignificant. Taken together, our results suggest that depressive symptom severity is not a predictor or consequence of total adiposity among late middle-aged African-American adults. Our findings may have implications for the design of obesity and depression prevention and treatment programs specifically designed for this African-American age group.
The observed lack of depressive symptoms-adiposity relationships contrasts the results of five longitudinal studies in which greater depression at baseline predicted future obesity (11-13) and/or vice versa (9, 10) in samples of white and African-American individuals. When race/ethnicity interactions were tested, they were not detected (10-13). Although most studies had large numbers of African-Americans, none stratified by race and reported subgroup analyses. Because the majority of these prospective studies detecting depression-obesity relationships examined adolescent samples (10-13) or abdominal obesity (9, 16), their findings may not generalize to our late middle-aged sample (mean baseline age of 56 years) and our use of total body adiposity.
Our findings are consistent with several prospective studies detecting depression x race/ethnicity interactions. In a prospective investigation of 2,088 older adults, Vogelzangs et al. (16) found that baseline depression was associated with an increase in abdominal obesity for men and non-Hispanic white women, but not for African-American women. Similarly, in 2,547 adults, Vogelzangs et al. (17) found that visceral fat predicted depressive symptom onset in African-American and white men, but not African-American or white women. In 918 adolescent females (15), depression was prospectively related to obesity onset and vice versa for non-Hispanic whites but not for African-Americans or Hispanics. Thus, when prospective depression-total adiposity relationships are examined in African-Americans (especially middle-aged and older adults), associations are often not detected. Such findings may point not only to moderation effects by race/ethnicity but also by age/life stage and type of adiposity, possibilities that need further exploration. Our study not only adds to this literature it also has several strong methodological features typically missing in past studies, including (1) use of SEM that allowed for the simultaneous, prospective examination of both directions of the depression-obesity relationship, (2) two measured indicators of total adiposity, and (3) a lengthy, 9-year follow-up.
One key reason that depression was unrelated to adiposity in our sample may be that total body adiposity was examined instead of abdominal adiposity, and depression may be more strongly related to specific types or locations of adipose tissue (9, 16). A second reason is that the late middle-age life stage of our sample may not have encompassed the periods of greatest change in depression or adiposity (e.g., earlier adulthood; 27,28). Another possible explanation for why depression-adiposity relationships tend to be observed in non-Hispanic whites and adolescent African-Americans but not late middle-aged African-American adults is that the proposed mechanisms are not active among late middle-aged African-Americans. Depression has been said to promote obesity via biological pathways, such as hypothalamic-pituitary-adrenal axis dysregulation (29) and/or increased systemic inflammation (30) or via its impact on behaviors, such as emotional eating (31) and sedentary behavior (32; Figure 4, Panel A). However, depression may not lead to greater total adiposity in late middle-aged African-Americans because it may not promote systemic inflammation among adult African-Americans (33).
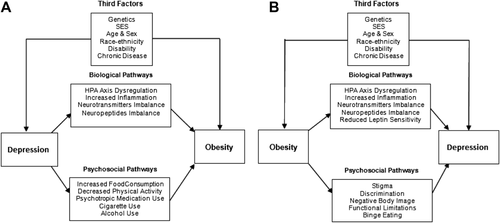
Biopsychosocial models of depression and obesity. (A) Depression as a predictor of obesity and the potential mechanisms. (B) Depression as a consequence of obesity and the potential mechanisms.
Regarding the opposite direction, obesity may lead to increases in depression via similar biological pathways (29), via leptin resistance (34), or via body image dissatisfaction (35) and stigma/discrimination (36) (Figure 4, Panel B). African-American adult women, however, have been shown to have less body dissatisfaction and a greater tolerance of larger body size than non-Hispanic white women (37). Compared with Caucasians, African-American men may prefer larger female body types and endorse more favorable characteristics of women with obesity (38). Thus, obesity may not have predicted increases in depressive symptom severity in our sample due to greater body shape/weight acceptance and satisfaction as well as less weight-related stigma/discrimination among African-American adults.
Although this study has several strengths, limitations should be acknowledged. First, no assessment of type or distribution of body fat was conducted, which may be important because some studies have found associations between depression and abdominal fat but not total adiposity (9, 16). Second, because our sample was comprised of late middle-aged African-American adults, future studies should test whether our findings generalize to African-Americans at earlier or later life stages, particularly adolescence, given that most of the conflicting evidence is for this age group. Third, many latent variables had only one single-item indicator (e.g., BF%), whereas others had multiple indicators (e.g., CES-D) but came from a single instrument. Using multiple indicators of latent factors is advocated, as it can provide a more reliable and valid assessment of the latent constructs (25). However, our obtaining similar results in models examining two different measures of adiposity mitigates this concern. Next, because participants with greater baseline depressive symptom severity were more likely to be lost to follow-up, this attrition may have restricted the range of CES-D scores. The general tendency of older African-Americans to report lower levels of depressive symptoms and to experience more chronic depression (39) could also have restricted the range of the baseline depression scores and the change scores in our sample, which may have contributed to our null results. However, reasonable variability in CES-D scores was observed at each time point as well as variability in the change scores (see Table 1). To improve the assessment of depression, future studies should assess depressive symptoms more frequently and also include diagnostic assessments. Lastly, although men were well-represented in the total sample (35%), the recommended sample size of ≥ 200 cases (25) was not met. This limitation is unfortunate, given evidence that the depression-obesity relationship has been found more consistently in women (e.g., 14). However, it should be noted that when the models were run in females only, CES-D was still not related to BF% or BMI in either direction (results not shown).
Altogether, the findings of this 9-year prospective cohort study suggest that depressive symptom severity may not be a predictor or consequence of total adiposity among late middle-aged African-Americans. Our findings highlight the importance of examining race/ethnicity, age/life stage, and type of adiposity as moderators of depression-obesity associations. Our results also emphasize the possible need for different conceptual models of obesity for non-Hispanic whites and African-Americans across the lifespan. If replicated, our findings suggest that including a depression module in obesity prevention and treatment programs specifically designed for late middle-aged African-Americans may not have a beneficial effect on obesity outcomes. Instead, resources should be used to target other factors that may play a role in obesity development/maintenance among African-Americans, such as perceptions of obesity-related health risk (40). Similarly, in depression prevention and treatment programs designed for late middle-aged African-Americans, our results raise the possibility that weight loss interventions may fail to have the desired influence on depression outcomes despite having many other health benefits. Replication in prospective studies that include well-powered race/ethnicity subgroup analyses, a wide age range, and measures of total and abdominal obesity is necessary before strong clinical conclusions can be drawn. Because African-Americans have among the highest rates of obesity of any racial/ethnic group in the nation and suffer significant health consequences from this condition (7), it is imperative that future studies identify strong predictors of obesity across the lifespan in this population, which can be targeted by culturally-sensitive and age-appropriate interventions.





