Fat mass is a predictor of incident foot pain
Disclosure: There are no conflicts of interest to disclose.
Author Contributions: All authors were involved in drafting this article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr Wluka had full access to all of the data in this study and took responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design: Butterworth, Menz, Urquhart, Cicuttini, Wluka, Strauss, Proietto, Dixon, and Jones were involved in study conception and design.
Acquisition of data: Butterworth, Urquhart, Cicuttini, Wluka, Strauss, and Proietto were involved in data acquisition.
Analysis and interpretation of data: Butterworth, Wluka, Urquhart, Cicuttini, Menz, Strauss, Jones, Proietto, and Landorf were involved in data analysis and interpretation.
Abstract
Objective
Foot pain is a common complaint in adults. Increased BMI and fat mass have been linked only to foot pain prevalence. Therefore, a longitudinal study to examine the relationship between body composition and incident foot pain over 3 years was conducted.
Design and Methods
Sixty-one community dwelling participants from a previous study of musculoskeletal health, who did not have foot pain at study inception in 2008, were invited to take part in this follow-up study in 2011. Current foot pain was determined using the Manchester Foot Pain and Disability Index, and body composition was measured using dual X-ray absorptiometry at study baseline.
Results
Of the 51 respondents (84% response rate, 37 females and 14 males), there were 11 who developed foot pain. BMI ranged from underweight to morbidly obese (17-44 kg/m2), mean 27.0 ± 6.0 kg/m2. Incident foot pain was positively associated with both fat mass (odds ratio [OR] 1.11, 95% confidence interval [CI] 1.03-1.20) and fat-mass index (OR 1.28, 95% CI 1.04-1.57) in multivariate analysis.
Conclusions
Fat mass is a predictor of incident foot pain. This study supports the notion that incident foot pain in overweight individuals is associated with fat mass rather than body mass alone.
Introduction
A recent systematic review (1) of 31 population-based studies, ranging in sample sizes from 96 to 42,826 and involving 75,505 participants, found that 24% of adults over the age of 45 suffered with frequent foot pain. A wide range of prevalence estimates were reported across studies, ranging from 0.2% for specific nail pain among middle-aged men and women to 64% for any foot pain in elderly females. Foot pain is known to have a significant and independent detrimental impact on balance and gait (2, 3), activities of daily living (4, 5), and overall health-related quality of life (6, 7). Furthermore, a substantial number of people with foot disorders consider them serious enough to seek treatment; a recent study in 2010 found that foot problems account for 8% of all musculoskeletal consultations with medical practitioners in the UK (8).
The study of foot pain in epidemiological research has been limited by an appropriate and validated assessment tool (9) until Garrow et al. (10) developed and validated the Manchester Foot Pain and Disability Index (MFPDI). An important advantage of the MFPDI is that it attempts to measure disabling foot pain, so may be used to identify a more severely affected subgroup of people with foot pain (6).
Recent studies have reported that overweight and obese adults are more likely to have foot pain than those of normal weight (11, 12). Foot pain is also common in obese adolescents; one study reported foot pain as the second most common musculoskeletal symptom, second only to back pain (13). A recent study (14) has demonstrated an association between foot pain and increased fat mass, rather than increased body mass alone. The systemic metabolic and inflammatory mediators produced by adipose tissue may cause detrimental changes to the connective tissues that are essential for anatomic foot integrity, thus promoting foot pain (15). Consequently, to understand the association between obesity and foot pain, it is important to examine the relationship of measures of body composition, including fat and fat-free mass, as well as weight and BMI, with foot pain.
Despite the link between fat mass and foot pain, this relationship has not been explored in longitudinal studies; two recent studies (11, 18) have assessed the temporal relationship between BMI and foot pain, without accounting for measures of fat and fat-free mass. Therefore, the aim of this study was to examine the relationship between specific body composition measures and incident foot pain, in a population recruited to study the effect of weight and body composition, over a 3-year period, using the MFPDI.
Methods and Procedures
Study population
Participants (n = 61) who did not have foot pain (according to the MFPDI) at baseline (in 2008) were eligible for the current study. These participants were invited to complete the MFPDI 3 years later. Of these, 51 (84%) completed the follow-up study, including 37 women (73%). Seven participants declined to participate and three were unable to be contacted by the researchers.
Initial recruitment was through the local media and public, private, and community weight loss clinics. Participants were initially recruited to participate in a study of the relationship between obesity and musculoskeletal disease. The aim of the baseline cross-sectional research was to examine the relationship between body composition and foot pain, in a population ranging from healthy to obese. Subjects were excluded if there was a history of any arthropathy diagnosed by a medical practitioner, prior surgical intervention to the knee including arthroscopy, previous significant knee injury requiring non-weight bearing therapy or requiring prescribed analgesia, malignancy, or contraindication to magnetic resonance imaging. This study was approved by the Alfred Health Human Ethics Committee and the Monash University Human Research Ethics Committee. Informed consent was obtained from all participants.
Data collection
Study participants completed a questionnaire that included information on their demographics and characteristics. The MFPDI was used to document disabling foot pain at baseline (2008) and follow-up (2011). The MFPDI has undergone several psychometric evaluations (6, 9, 19, 20) and has been used to determine the prevalence of disabling foot pain in population-based studies (6, 21, 22). The MFPDI consists of 19 items that are preceded with the phrase, “because of pain in my feet,” formalized under four categories: functional limitation (10 items), pain intensity (5 items), personal appearance (2 items), and difficulties with work or leisure activities (2 items). Each item is documented as being present “none of the time" (0 points), “on some days" (1 point), or “on most/everyday" (2 points); subsequently, scores on the MFPDI range between 0 and 38, with higher scores denoting more disabling pain. Using the original definition of foot pain as described by Garrow et al. (10), participants with a score of ≥1 from 19 items were defined as having disabling foot pain.
Measures of obesity taken at the time of the baseline MFPDI were used in the current analysis. Body composition was analyzed by two experienced radiographers using dual-energy X-ray absorptiometry (DXA) and operating system version 9 (GE Lunar Prodigy, GE Lunar Corp., Madison, WI). The machine has a weight limit of approximately 160 kg. Weight was measured to the nearest 0.1 kg using DXA (shoes, socks, and bulky clothing were removed). Height at baseline was measured to the nearest 0.1 cm (shoes and socks were removed) using a stadiometer. From these data, BMI was calculated and reported in kg/m2. Short-term coefficients of variation, assessed in 15 normal young adults, were 1.2% for total body fat mass and 0.4% for total body lean tissue mass (14, 23). Based on the DXA data, fat-mass index (FMI) and fat-free mass index (FFMI) were calculated as follows: FMI = fat mass/height2 and FFMI = fat-free mass/height2, where fat-free mass = lean tissue mass + bone mineral content.
The mental component summary (MCS) of the Short Form 36 (SF-36), measured at baseline, was used to examine psychological health and well-being. The SF-36 is a self-reported measure, used to assess health-related quality of life. Low MCS scores indicate psychological distress and social and role disability, due to emotional problems. High MCS scores indicate a positive effect, absence of psychological distress, and limitations in social and role activities due to emotional problems (14, 24).
Statistical analysis
All continuous data were initially checked for distribution and found to be normally distributed. Independent-samples t-tests and χ2 tests were used to assess differences in body composition in those without foot pain at baseline or follow-up (“no pain") and those without foot pain at baseline but with foot pain at follow-up (“incident pain"). Binary logistic regression was used to assess the relationship between incident foot pain and measures of body composition. The multivariate analyses were adjusted for age, gender, and the MCS and were repeated in women only. In order to distinguish between body composition measures (fat mass, fat-free mass, FMI, and FFMI) as predictors of foot pain, appropriate adjustments were made in the multivariate analysis. P values less than 0.05 (two-tailed) were regarded as statistically significant. All analyses were performed using the SPSS statistical package (standard version 18.0).
Results
Fifty-one (84%) of 61 eligible participants, with no foot pain at baseline, completed this study. Of the 51 participants (mean ± SD, age 49.2 ± 8.1 years), who at baseline ranged from underweight to morbidly obese (range 17-44 kg/m2), 37 (73%), were women. The 10 participants who were lost to follow-up were all female, of younger age (41.2 ± 10.4 vs. 49.2 ± 8.1, P < 0.001), and had a higher mean BMI (36.2 ± 10.5 vs. 27.0 ± 6.0, P < 0.001) and total fat mass (45.2 ± 19.3 vs. 26.1 ± 13.3, P < 0.001) than those who completed the follow-up study. There were 11 participants who developed foot pain, and characteristics of participants with and without incident foot pain are shown in Table 1.
| No foot pain (n = 40) | Incident foot pain (n = 11) | P valuea | |
|---|---|---|---|
| Age, years | 49.5 ± 7.9 | 48.3 ± 9.6 | 0.68 |
| Gender, no. of women, % | 28 (70) | 9 (82) | 0.44b |
| MCS | 47.9 ± 13.2 | 51.8 ± 7.3 | 0.35 |
| PCS | 55.0 ± 5.3 | 51.5 ± 7.2 | 0.08 |
| BMI, kg/m2 | 26.3 ± 5.4 | 29.6 ± 7.9 | 0.12 |
| Total fat mass, kg | 24.3 ± 11.9 | 32.4 ± 16.9 | 0.08 |
| Total fat-free mass, kg | 49.4 ± 10.5 | 46.6 ± 6.7 | 0.42 |
| FMI | 8.7 ± 4.2 | 12.1 ± 6.4 | 0.04 |
| FFMI | 17.5 ± 2.4 | 17.3 ± 2.3 | 0.81 |
- Values are the mean ± SD unless otherwise indicated.
- FMI, fat-mass index; FFMI, fat-free mass index; MCS, mental component summary of the SF-36.
- a P calculated for difference between subjects with and without foot pain using independent-samples t-test unless otherwise indicated.
- b P calculated for difference between subjects with and without foot pain using χ2 test.
When those with and without incident foot pain were compared (Table 1), those with foot pain had a significantly higher FMI (P = 0.04) than those without foot pain. There was a tendency toward those with incident pain having higher baseline BMI (P = 0.12) and fat mass (P = 0.08).
When examining the relationship among BMI, body composition, and incident foot pain (Table 2), BMI was not a significant predictor of incident foot pain in univariate (odds ratio [OR] 1.09, 95% confidence interval [CI] 0.98-1.20) or multivariate analysis (OR 1.12, 95% CI 0.99-1.26). In the univariate analysis, neither fat mass nor FMI were shown to be positive predictors of incident foot pain. However, total fat mass (OR 1.11, 95% CI 1.03-1.20) and FMI (OR 1.28, 95% CI 1.04-1.57) were both shown to be positive predictors of incident foot pain in the multivariate analysis, adjusted for age, gender, and either total fat-free mass or FFMI, as appropriate. In contrast, in both the univariate and multivariate analyses adjusted for age, gender, and either fat mass or FMI, as appropriate, there were no significant associations among fat-free mass, FFMI, and incident foot pain (Figure 1). Similar results were found when only women were examined and when the MCS was included as a covariate.
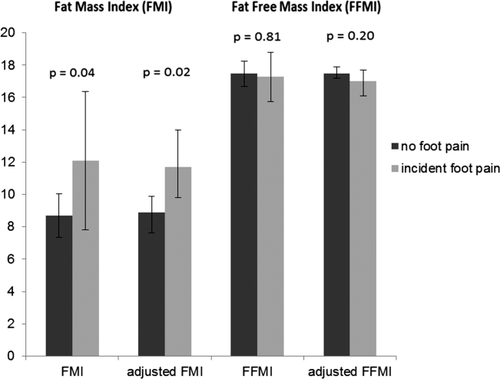
No pain versus incident foot pain: the mean FMI and FFMI using estimated marginal means; adjusted FMI: adjusted for age, gender, MCS, and FFMI; adjusted FFMI: adjusted for age, gender, MCS, and FMI; error bars represent 95% CI.
| No pain versus incident pain | ||||
|---|---|---|---|---|
| Univariate OR (95% CI) | P value | Multivariate OR (95% CI) | P value | |
| BMI | 1.09 (0.98-1.20) | 0.13 | 1.12 (0.99-1.26) | 0.07a |
| Total fat mass | 1.04 (0.99-1.10) | 0.09 | 1.11 (1.03-1.20) | 0.01b |
| Total fat-free mass | 0.97 (0.90-1.04) | 0.41 | 0.81 (0.65-1.00) | 0.05c |
| FMI | 1.14 (0.99-1.30) | 0.05 | 1.28 (1.04-1.57) | 0.02d |
| FFMI | 0.97 (0.72-1.29) | 0.80 | 0.68 (0.38-1.23) | 0.20e |
| Age | 0.98 (0.90-1.06) | 0.60 | – | |
| Gender | 1.93 (0.36-10.30) | 0.44 | – | |
| MCS | 1.04 (096-1.11) | 0.35 | – | |
- OR, odds ratio; 95% CI, 95% confidence interval.
- FMI, fat-mass index; FFMI, fat-free mass index; MCS, mental component summary of the SF-36.
- a Adjusted for age, gender, and MCS.
- b Adjusted for age, gender, MCS, and total fat-free mass.
- c Adjusted for age, gender, MCS, and fat mass.
- d Adjusted for age, gender, MCS, and FFMI.
- e Adjusted for age, gender, MCS, and FMI.
Discussion
This study has shown that fat mass, not fat-free mass, is an independent predictor of incident foot pain in a community-based population. Confirmation of the relationship among increased BMI, body composition, and the prevalence of foot pain has been recently published in a systematic review (12) and a cross-sectional study (14). Two recent longitudinal studies (11, 18) have examined the relationship between BMI and foot pain; however, these findings are the first longitudinal data examining the relationship between specific body composition measures and incident foot pain.
The results we have presented in this study suggest that fat mass may be a stronger predictor than BMI. While BMI remained non-significant in the multivariate analysis, it may have achieved significance with a larger study population. From these results, it appears that by analyzing fat and fat-free mass, rather than BMI alone, a more definitive conclusion may be drawn on the effect of specific body composition measures and the development of foot pain. Considering that fat mass and FMI are significant predictors of incident foot pain, independent of fat-free mass, the mechanisms underlying the onset of foot pain in an overweight population may be related to systemic metabolic processes rather than mechanical forces acting on foot structures. As fat-free mass and FFMI were not significantly associated with foot pain, this theory is further strengthened. The results from a recent cross-sectional study (14) from this same cohort also showed fat mass as a predictor of the prevalence of foot pain.
There are a number of biomechanical mechanisms that may contribute to the link between obesity and foot pain, including changes in structure and function of the foot (25) and increased plantar pressures (28). However, metabolic factors may also play a role, and there are a number of possibilities by which adipose tissue may influence incident foot pain. Adipose tissue is recognized as being a highly metabolically active endocrine organ (31, 32), as it produces hormones such as leptin, estrogen, resistin, and cytokines such as tumor necrosis factor-alpha and interleukin-6. Current evidence suggests that the accumulation of adipose tissue around the abdomen is more metabolically active and more closely related to an elevated risk of cardiac disease and diabetes (31, 32). Conversely, there is evidence to suggest that a more peripheral distribution of adipose tissue may have a protective effect for these diseases (32). Regardless, previous studies have shown the involvement of pro-inflammatory cytokines in the development and progression of chronic pain (33, 34). Moreover, recent studies have shown that foot and ankle tendinopathy is associated with abdominal obesity, dyslipidemia, hypertension, and insulin resistance (16, 17).
Disabling foot pain in this study was defined as current foot pain and/or pain in the last month with at least one item recorded “on some days" assessed using the MFPDI, which was previously validated by Garrow et al. (10) for this purpose in a population of similar age. Additional definitions of disabling foot pain, using the MFPDI, have been proposed (9, 19). Roddy et al. (19) suggest that, for foot pain and disability to be present, participants are required to record at least one item on the MFPDI as occurring “on most days or everyday.” Importantly, this method was validated for use in an older cohort (6), and, therefore, we considered the definition described originally by Garrow et al. to be more appropriate for our study. Moreover, as this study utilized baseline data from a previous study at the same institution (14), using the Garrow definition allowed us to analyze and draw conclusions with longitudinal rather than cross-sectional analysis. However, as our study utilized baseline data for the follow-up analysis, changes in weight and body composition over this timeframe could not be accounted for in our final analysis. A further limitation of this study was the small proportion of males compared to females, with few having incident foot pain. Our sample size also limited the number of variables we could use in our regression model. Despite this, we were able to detect significant relationships among fat mass, FMI, and foot pain. The follow-up in this study was excellent (84%), with those lost to follow-up having a higher degree of obesity and fat mass than those who completed this study, which would tend to bias our results toward the null.
There were additional strengths to this study: the inclusion of participants encompassing a broad spectrum of BMI, from underweight through to morbidly obese, strengthens the generalizability of our results to the broader population. The adjustment of confounders in our analysis was a strength; in particular, gender as a potential confounder has been reported with regard to pain perception (35) and obesity (36). Results of our analysis were similar when the analysis was limited to women only and also when we adjusted the multivariate analysis for the physical component summary of the SF-36 (data not presented). Adjustment for the MCS of the SF-36 was considered important, as mental health problems have been linked to both obesity and foot disorders (18, 37).
A substantial strength was that the measurement of both foot pain and body composition was made using established and validated measurement tools. Moreover, the longitudinal design of this study allowed us to examine the temporal relationship between fat mass and foot pain. Our study demonstrated that, in addition to fat mass being positively associated with incident foot pain, a similar association was also seen between FMI and foot pain but not fat-free mass or FFMI, which further supports the notion that being overweight impacts foot pain through a more systemic rather than biomechanical effect and that this is independent of height. Nonetheless, we cannot rule out the potential contribution of biomechanical mechanisms, as we did not assess foot structure and function in this study. It is likely in this population therefore that incident foot pain may be attributed to a combination of increased mechanical loading on the foot and systemic inflammatory effects of increased adiposity.
This study demonstrated that incident foot pain was related to an increased baseline fat mass. This provides stronger evidence for the role of fat, via metabolic mechanisms, in the development of incident foot pain. Therefore, it is likely that reducing adipose tissue mass with weight loss, exercise and counseling methods where necessary (37), may result in a reduced risk of incident foot pain. Consequently, weight loss and lifestyle changes may be important approaches to preventing foot pain and disability (38, 39).
Fat mass, not fat-free mass, is a predictor of incident foot pain. This study supports the notion that incident foot pain in overweight individuals is associated with fat mass rather than body mass alone.
Acknowledgments
The authors would like to acknowledge Judy Hankin and Alice Noone for recruitment of study subjects. The authors would also like to give a special thank you to all of the study participants who made this study possible.