Association of nursing hours with cognitive function, balance, and dependency level of stroke patients
Abstract
Aims
To examine the association of nursing hours given to patients with stroke with clinical characteristics to predict the nursing care needs.
Design
Twenty-four-hour observational study
Methods
Nursing hours per patient day (NHPPD) of 171 stroke patients were measured by 146 nursing personnel who worked on the day of the observation. Cognitive function, balance ability and dependency level were assessed using the Korean version of the Mini-Mental State Examination (K-MMSE), the Korean version of the Berg Balance Scale (K-BBS) and the Korean version of the Modified Barthel Index (K-MBI), respectively.
Results
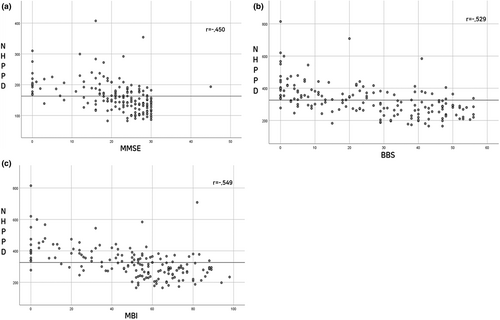
The NHPPD were moderately correlated with K-MMSE (r = −.450), K-BBS (r = −.529) and K-MBI (r = −.549). The worse the cognitive function, balance ability and dependency level, the more were the nursing hours given to the patients. Therefore, these factors can be considered to be factors that predict nursing care needs for patients with stroke.
Impact Statement
- The worse the cognitive function, balance ability and dependency level, the more were the nursing hours given to the patients with stroke.
- Cognitive function, balance and dependency level should be considered factors that measure nursing care needs of patients with stroke.
- These factors could give the basis for determining the adequate nursing staff levels for rehabilitation patients with stroke.
1 INTRODUCTION
The number of hospitalized patients worldwide continues to increase due to an increasingly aging population, the prevalence of chronic diseases and easy access to healthcare services (Kang et al., 2020). With the increased frequency and duration of patient hospitalization, the burden on nursing care has also increased (Grady, 2011). In elderly patients, more than half of the frequently observed illnesses are musculoskeletal and neurological in nature, which significantly increases the demand for rehabilitation nursing care (Health Insurance Review and Assessment Service & National Health Insurance Service., 2020). Stroke is the third most common cause of disability, and the incidence of stroke increases with age (Feigin et al., 2014). With the increased incidence of stroke, the global burden of stroke is also high, as extended hospitalization and life-long healthcare are needed. Stroke has a significant impact on the global economy as it accounts for approximately 34% of the global total healthcare expenditure (Rochmah et al., 2021). If patients with stroke are given rehabilitation and sufficient nursing care, the patient outcomes will improve faster, reducing national medical expenses.
For the treatment of rehabilitation patients, adequate nursing staff needs to be assigned to give sufficient nursing care. Some studies showed that nurses' workload is associated with patient safety in terms of the higher staffing level the hospital has, the less patient adverse events occur (Aiken et al., 2014; Kang et al., 2016). Inadequate nurse staffing causes problems such as increased patient safety events, poor patient outcomes and decreased patient and nurse satisfaction (Aiken et al., 2010; Griffiths et al., 2016). Thus, increasing nursing staff and resources can be a potential strategy for improving patient outcomes and promoting patients (Liu et al., 2018). To determine the appropriate nurse staffing level, it is necessary to be aware of the required nursing hours based on patient characteristics.
Currently, many countries recommend appropriate nurse staffing levels according to shift type, ward type or hospital type (Van den Heede et al., 2020). This is because the required nursing activities and nursing hours vary depending on the characteristics of the patients in the wards. Functional recovery can be achieved through a continuous process of rehabilitation therapy. Inpatient nursing services play an important role in ensuring the exact amount and frequency of rehabilitation therapy given to each patient and need to be given with sufficient nursing care (Pryor, 2012).
2 BACKGROUND
Most patients with stroke face cognitive and physical impairments, and rehabilitative hospitalization is required (Cho & Lee, 2012). Rehabilitation wards specialize in helping these patients with various diseases or disabilities return to their daily lives (Accreditation, 2010). In particular, most patients with stroke require specialized and professional rehabilitation, unlike patients in acute wards (Kang & Park, 2016). Patients in rehabilitation wards show poor self-care in the prevention of accidents and poor daily activities when they have cognitive impairments, thus requiring continuous supervision over 24 hr (Park et al., 2011). Falls are common in hospitals (Weil, 2015); therefore, it is necessary for nurses working with rehabilitation patients to be aware of their characteristics.
Most patients with acute stroke experience cognitive decline. The incidence of cognitive impairment after the onset of stroke has been found to be 23.1% and 42.3% of patients with stroke (Oh et al., 2018). Previous studies have revealed that cognitive impairment is commonly observed in patients with stroke, who make up the majority of patients in rehabilitation wards, and that cognitive function affects patient outcomes and nursing care needs (Casafont et al., 2020). Cognitive dysfunction is a factor that affects patients' self-care performance, including medication, diet and symptom management, which consequently affects their level of functional recovery (Heckman et al., 2007).
Additionally, stroke is accompanied by decreased balance, loss of independence and a decline in activities of daily living (ADLs) (Eng et al., 2008; Winstein et al., 2016). Balance functions are essential for independence in daily activities, mobility, ambulation and general health maintenance for the rehabilitation of patients (Chang et al., 2021). Stroke, one of the most common causes of impaired ambulatory and balance functions, affects patients' ADLs (Dehghani et al., 2019). Moreover, impairments in ambulation and balance frequently result in proneness to loss of equilibrium, which causes unexpected falls and fall-related injuries (Marchese et al., 2003). Nurses need to pay more attention to patient care because patients with stroke are at a higher risk of recurrent falls and fall-related injuries (Tilson et al., 2012).
Performing ADLs after a stroke, including eating, grooming and bathing, is very important for both the patient and the caregiver (Jeong et al., 2018). Many stroke survivors experience persistent difficulties with daily tasks as a direct consequence. This can further reduce physical activity and lead to undesirable events. Loss of independence due to a decline in ADLs leads to fear of falling and reduced physical activity, which can have a greater negative impact on patient outcomes (Friedman et al., 2002). In other words, as ADLs decline, nursing care needs increase, negatively affecting patient outcomes and burdening caregivers.
Cognitive impairment, balance ability and dependency level are the main characteristics that affect functional recovery in patients with chronic stroke (Cho & Lee, 2012). A previous study showed that cognitive impaired and functionally dependent patients used more resources such as nursing care time and medical costs (Sköldunger et al., 2019). If these characteristics of patients are related to the actual nursing hours, they can be the indicators that predict nursing care needs. Also, measuring required nursing hours according to patient characteristics and maintaining adequate nursing staffing are essential to improve patient outcomes. Therefore, cognitive function, balance ability and dependency level can be important indicators of patient outcomes and nursing care needs in patients with stroke.
The present study aims to investigate the actual nursing hours given to patients and its correlation with patient characteristics such as cognitive and balance function and ADLs to predict the nursing care needs of patients with stroke.
3 METHODS
3.1 Study design
A cross-sectional observational study was conducted employing the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) procedure (Cevallos et al., 2014).
3.2 Participants
One-hundred seventy-one patients with stroke and 146 nursing personnel (50 registered nurses, 23 nurse assistants and 73 rehabilitation support staff composed of care workers) who worked for the patients on the day of observation from rehabilitation wards of six different hospitals in five cities of South Korea selected through convenience sampling agreed to participate in this study.
The G-power 3.1.9 software (Heinrich-Heine-University Dusseldorf, Dusseldorf, Germany) was used to estimate the sample size. To calculate the sample size, the probability of alpha error and power were set at 0.05 and 0.9, respectively, with a medium effect size of f2 = 0.15 (F test, linear multiple regression: fixed model, number of predictors = 6) based on Cohen (Cohen, 1988). A sample size of 123 participants was required.
3.3 Measures
3.3.1 Nursing hours per patient day
Nursing hours per patient day (NHPPD) were measured through a “time and motion” study, which involved the continuous observation of nursing activities and hours by a third party by following the nursing personnel over a specified period. The NHPPD were observed using a list of nursing activities used by the National Health Service of the United Kingdom: direct care, indirect care, associate work and unproductive time (Table 1) (Hurst, 2008). Direct nursing activities were measured by tracking the time spent by the nursing personnel on each patient. For indirect and associate work activities, where matching with patients was ambiguous, with the exception of “meals and drinks”, the working hours were divided by the number of patients assigned to the relevant nursing personnel during the working hours and allocated as nursing hours. Unproductive time was excluded from the analysis since it was not spent on patient care. The time spent by the nursing personnel for the day per patient was measured.
| Nursing activity | ||
|---|---|---|
| Direct care | 14 | Vital signs/blood glucose/weight, etc., medication, communicating, nursing procedures, specimen, medical procedures, teaching, elimination, escorting/admitting/discharging, movement, nutrition, hygiene, assisting doctors, assisting others |
| Indirect care | 5 | Charting, reporting, communicating with staff, communicating with relatives, teaching |
| Associate work | 8 | Clerical, communication, supplies, cleaning, meals and drinks, errands, meetings, supervising |
| Unproductive time | 4 | Personal time, unoccupied, breaks, studying |
3.3.2 Activities of daily living
The Korean version of the Modified Barthel Index (K-MBI) was used to assess ADLs in patients with stroke (Choi, 2022). A total of 10 items describing ADLs and mobility were scored to measure the degree of assistance required by an individual. Two items (bathing and personal hygiene) were ranged from 0 to 5 scores, six items (feeding, toilet use, dressing, stair climbing, bladder and bowel control) were ranged from 0 to 10 scores, and two items (chair/bed transfer and ambulation) were ranged from 0 to 15 scores (Hong et al., 2017). A score of 91 or more indicated “slight dependency”, 61–90 indicated “moderate dependency”, 21–60 showed “severe dependency” and 20 or less indicated “total dependency” (Jung et al., 2007). The K-MBI has been reported that is valid for the patient with stroke and has excellent reliability of 0.94, with a range of discriminative index of 0.78–0.91 (Choi et al., 2012).
3.3.3 Balance
The Korean version of the Berg Balance Scale (K-BBS), generally considered the gold standard in assessing balance impairment, especially for patients with stroke (Berg et al., 1992), was used to evaluate each patient's ability in static and dynamic balancing during the tasks. It consists of 14 items that were scored from 0 meaning unstable to 4 meaning stable (Song et al., 2017). The total score was out of 56, with 41–56 indicating “good balance”, 21–40 representing “acceptable balance impairment” and a score below 20 representing “balance impairment” (Berg et al., 1995). The K-BBS has excellent intra-rater reliability of 0.98 and inter-rater reliability of 0.97 (Kim et al., 2021).
3.3.4 Cognitive impairment
Cognitive impairment was examined using the Korean Mini-Mental State Exam (K-MMSE), which has been widely applied in clinical and research settings (Kang et al., 1997). It was originally developed to screen for dementia, but several studies have also reported acceptable Mini-Mental State Exam (MMSE) validity in screening for cognitive impairment and predicting functional outcomes in patients with stroke (Bour et al., 2010). There are 30 questions that consist of the ability of orientation, memory, attention and calculation, language function, understanding and judgement (Kim et al., 2017). A score of 24 or above suggested “normal cognition”, 18–23 indicated “mild cognitive impairment” and 0–17 indicated “severe cognitive impairment” (Lee et al., 2002). The K-MMSE has excellent intra-rater reliability of 0.99 (Jeong et al., 2014).
3.4 Data collection
Data were collected from May to September 2020. The NHPPD of 171 stroke patients given by 146 nursing personnel who worked on the day of the observation were measured by 67 third-party observers. The details of the observed nursing hours included the shift, bed number of the patient, recorder, nursing activity, its start and end time and others. The NHPPD was measured in minutes, as third-party observers followed the nursing personnel working on the day of the observation. For the accurate classification of nursing activities and measurement of NHPPD, observers were off-duty nursing personnel working at the hospital where the observation was conducted.
The K-MMSE, K-BBS and K-MBI were obtained from the medical records of each patient, and experienced physical therapists and occupational therapists conducted all assessments within 5 days before the day of the observation of NHPPD.
3.5 Data analysis
The 24 observed nursing hours were extracted as NHPPD by nursing activities. Since “unproductive time” is irrelevant to the acuity and nursing care needs of patients, it was excluded from the data analysis. Data were analysed using SPSS for Windows (version 23.0, IBM Corp.). Data were calculated as means and standard deviations (SDs) for quantitative variables and as frequencies and percentages for categorical variables. A one-way anova test was performed to compare the NHPPD according to patient clinical characteristics, such as K-MBI, K-BBS and K-MMSE. Pearson's correlation was conducted to determine the relationship between the NHPPD and the clinical characteristics of the patients. Multiple regression analysis was conducted to determine the factors influencing NHPPD after adjusting for sex, age and days after diagnosis. The level of significance was set at α = 0.05.
3.6 Ethical considerations
The study was conducted in accordance with the guidelines of the Declaration of Helsinki, and all procedures and protocols for this study were approved by the Institutional Review Board of Gachon University (IRB No. 1044396-202,004-HR-075-03). The aims of the study and the means of data collection were explained, and all subjects signed an informed consent form before participating in the study. To protect personal information, investigators were unable to identify patients.
4 RESULTS
4.1 General characteristics of patients
The average age of the patients in this study was 67.6 years, and 63.2% were female. The mean number of days after diagnosis was 222 days. The mean ± SD of K-MMSE score was 20.6 ± 9.0, K-BBS was 25.8 ± 18.2, and K-MBI was 49.2 ± 25.8. About the nursing hours, the mean ± SD of NHPPD of direct care, indirect care, associate work and total hours were 183.4 ± 78.6, 68.1 ± 17.0, 69.5 ± 21.0 and 321.0 ± 88.1 min, respectively. The general characteristics of the patients and NHPPD are described in Table 2.
| N (%) | Mean ± SD | |
|---|---|---|
| Sex | ||
| Male | 63 (36.8) | |
| Female | 108 (63.2%) | |
| Age | 67.6 ± 13.4 | |
| Onset | 266.0 ± 178.9 | |
| K-MMSE | ||
| Total score | 20.6 ± 9.0 | |
| Severe cognitive impairment | 46 (26.9) | |
| Mild cognitive impairment | 44 (25.7) | |
| Normal | 81 (47.4) | |
| K-BBS | ||
| Total score | 25.8 ± 18.2 | |
| Good balance | 70 (40.9) | |
| Acceptable balance | 53 (31.0) | |
| Balance impairment | 48 (28.1) | |
| K-MBI | ||
| Total score | 49.2 ± 25.8 | |
| Total dependency | 30 (17.5) | |
| Severe dependency | 78 (45.6) | |
| Moderate dependency | 61 (35.7) | |
| Slight dependency | 2 (1.2) | |
| NHPPD (min) | ||
| Direct care | 183.4 ± 78.6 | |
| Indirect care | 68.1 ± 17.0 | |
| Associate work | 69.5 ± 21.0 | |
| Total nursing hours | 321.0 ± 88.1 | |
- Abbreviations: K-MBI, Korean version of Modified Barthel Index; K-BBS, Korean version of Berg Balance Scale; K-MMSE, Korean version of Mini-Mental State Examination; NHPPD, Nursing hours per patient day.
4.2 Difference in mean NHPPD according to clinical characteristics of patients
The NHPPD differed significantly depending on the patients' cognitive, balance and physical disability functions (Table 3). It was found to be the highest for the group with the greatest severity on the K-MMSE, K-BBS and K-MBI, with statistically significant differences (p < .001).
| K-MMSE | Severe cognitive impairmenta (n = 46) | Mild cognitive impairmentb (n = 44) | Normalc (n = 81) | p * |
|---|---|---|---|---|
| Direct care | 232.3 ± 85.4 | 196.6 ± 78.1 | 148.4 ± 55.2 | <.001(c<b<a) |
| Indirect care | 76.6 ± 20.0 | 65.2 ± 14.4 | 64.8 ± 147.7 | <.001(b, c<a) |
| Associate work | 79.1 ± 29.2 | 72.9 ± 18.6 | 62.2 ± 12.7 | <.001(c<a, b) |
| Total | 388.0 ± 87.5 | 334.8 ± 81.3 | 275.4 ± 62.1 | <.001(c<b<a) |
| K-BBS | Balance impairmenta (n = 70) | Acceptable balanceb (n = 53) | Good balancec (n = 48) | p * |
| Direct care | 220.6 ± 78.5 | 167.4 ± 67.5 | 146.8 ± 67.7 | <.001(b, c<a) |
| Indirect care | 73.2 ± 19.2 | 62.2 ± 13.8 | 67.1 ± 14.5 | <.001(b<a) |
| Associate work | 77.7 ± 27.2 | 62.7 ± 13.1 | 65.0 ± 12.3 | .002(b, c<a) |
| Total | 371.5 ± 83.5 | 292.3 ± 74.5 | 278.9 ± 72.0 | <.001(b, c<a) |
| K-MBI | Total dependencya (n = 30) | Severe dependencyb (n = 78) | Moderate & slight dependencyc (n = 63) | p * |
| Direct care | 251.1 ± 91.1 | 195.8 ± 68.9 | 195.8 ± 68.9 | <.001(c<b<a) |
| Indirect care | 84.4 ± 19.6 | 62.4 ± 14.0 | 67.3 ± 14.0 | <.001(b, c<a) |
| Associate work | 82.8 ± 35.4 | 68.6 ± 16.9 | 64.3 ± 12.5 | <.001(b, c<a) |
| Total | 418.3 ± 84.8 | 326.8 ± 76.0 | 267.3 ± 56.6 | <.001(c<b<a) |
- Abbreviations: K-MBI, Korean version of Modified Barthel Index; K-BBS, Korean version of Berg Balance Scale; K-MMSE, Korean version of Mini-Mental State Examination;
- * One-way anova with Scheffe's post-hoc test.
4.3 Correlations between NHPPD and clinical characteristics of patients
The NHPPD had a significant negative correlation with all the clinical characteristics of the patients in this study. The K-MMSE (r = −.450, p < .001), K-BBS (r = −.529, p < .001) and K-MBI (r = −.549, p < .001) were negatively correlated with NHPPD (Figure 1).
4.4 Association between NHPPD and clinical characteristics of patients
In the univariate analysis, K-MMSE, K-BBS and K-MBI affected the NHPPD (p < .001). After adjusting for participants' age, sex and days after diagnosis onset, a significant regression equation was found (p < .001), with an adjusted R2 of .325. Predicted NHPPD decreased by 1.89 min for each K-MMSE score (p = .045), 1.37 for each K-BBS score (p = .024) and 0.94 min for each K-MBI score (p = .049) (Table 4).
| Crude | Adjusted | |||||||
|---|---|---|---|---|---|---|---|---|
| Ba | SE | βb | p | Ba | SE | βb | p | |
| Constant | 453.467 | 46.070 | <.001 | |||||
| Age | .147 | 0.486 | 0.020 | .762 | ||||
| Sex (male) | −12.760 | 13.077 | −0.062 | .331 | ||||
| Onset | 0.011 | 0.035 | 0.020 | .759 | ||||
| K-MMSE | −5.074 | 0.646 | −0.518 | <.001 | −1.886 | 0.936 | −0.170 | .045 |
| K-BBS | −2.674 | 0.312 | −0.551 | <.001 | −1.369 | 0.600 | −0.249 | .024 |
| K-MBI | −2.065 | 0.209 | −0.605 | <.001 | −0.940 | 0.478 | −0.245 | .049 |
| F(p) | 14.703 (<.001) | |||||||
| Adjusted R2 | .325 | |||||||
- Abbreviations: SE, standard error; K-MBI, Korean version of Modified Barthel Index; K-BBS, Korean version of Berg Balance Scale; K-MMSE, Korean version of Mini-Mental State Examination.
- a Unstandardized coefficient beta.
- b Standardized coefficients beta.
5 DISCUSSION
This study aimed to assess the association between the clinical characteristics of stroke patients and nursing hours given to predict the nursing care needs. The average number of nursing hours given to patients with stroke per day was found to be 321.0 ± 88.1 min, and the results of our study showed that higher number of nursing hours are required for giving care to patients who show higher severity on the K-MMSE, K-BBS and K-MBI.
To our knowledge, this is the first and only study to measure the actual nursing hours spent on patients with stroke through a 24-hrr observation and predict the nursing care needs of patients by measuring characteristics such as cognitive function, balance ability and dependency level.
Cognitive function is one of the factors that can be used to measure the nursing care needs of stroke rehabilitation patients. Patients with stroke with severe cognitive impairment required an average of 388.0 ± 87.5 min of NHPPD from nursing personnel, and they were also given more direct or indirect nursing care hours than patients with mild cognitive impairment and no cognitive impairment. Moreover, with a one-point decrease in the MMSE score, the predicted NHPPD decreased by 1.89 min, which had a greater impact than K-BBS and K-MBI. This is because ADLs and complex problems arising from physical and mental difficulties reduced along with cognitive impairment.
Nursing personnel should make continuous efforts to reduce cognitive decline after stroke (Oh et al., 2018). The analysis of the NHPPD according to the severity of cognitive function and the regression analysis showed that the cognitive function of patients affects NHPPD. The NHPPD is the most direct indicator of the nursing care needs of patients. In other words, in the case of cognitive impairment, nursing staff needs to help more with self-care, and rehabilitation takes more time, so the extent of a patient's cognitive decline is an important consideration in predicting patients' nursing care needs. Therefore, the patients' cognitive functioning should be considered while predicting nursing care needs and nurse staffing levels for rehabilitation patients.
The NHPPD differed depending upon the patient's balance ability. Balance was analysed as an influential factor in the NHPPD in regression analysis. Patients with stroke with balance impairment were given an average of 371.5 ± 83.5 min of nursing care, which is significantly greater than those who did not have balance impairment. Falling is one of the indicators of nursing-related performance, which leads to an increase in nursing hours, and this relationship has been continuously reported (Dall et al., 2009). When a fall occurs, it delays the patient's recovery and leads to other health problems (Dall et al., 2009); thus, nurses need to spend more time on patients at high risk of falls due to impaired balance functions. That is, in the case of patients with balance impairment, nursing staff must give extensive help which leads to increased nursing hours. Therefore, a patient's balance function must be considered in the acuity and nursing care needs of stroke rehabilitation patients.
The ADLs also need to be taken into account, since the higher the ADL dependency score, the worse the prognosis, the higher the demand and the higher the cost of care (Mlinac & Feng, 2016). Therefore, it is important to measure and evaluate the complex dependencies of the patients. In this study, a complex ADL dependency assessment using the K-MBI was analysed as a factor affecting NHPPD. Patients with total dependency required more nursing hours. The lower the K-MBI score, the higher were the nursing hours given to the patients. This is because when the patient is not able to perform daily activities independently, they rely on caregivers or mechanical devices, which require more nursing care and hours (Edemekong et al., 2017). Evaluation of ADL is, thus, essential in nursing assessment because nurses need to be the first to notice and respond to patients' functional deterioration, which determines the need for further rehabilitation or assistance (Edemekong et al., 2017).
Physical and psychosocial problems cause complicated nursing care demands (Rezaei-Shahsavarloo et al., 2021) and should be comprehensively assessed to predict the nursing care needs. As with the results of our study, it is necessary to evaluate the patient's nursing care needs by measuring cognitive function, balance function and ADL in combination and using them to determine the appropriate nursing staff arrangements. Maintaining proper nursing staffing levels will improve the patient outcomes and ensure nurses have the enthusiasm to give quality care (Vloothuis et al., 2016), which can shorten the length of hospital stay and allow patients to return to the community faster if caregivers are more actively involved in the rehabilitation process (Aiken et al., 2010; Griffiths et al., 2016). The results of this study indicate that the patient's cognitive function, balance ability and dependency level should be factored in while determining the nursing care of stroke rehabilitation patients, and more nursing personnel should be deployed to give sufficient quality nursing.
5.1 Limitations
Although this study is the first to investigate the relationship between clinical characteristics of patients with stroke and the nursing hours they require, it has some limitations. First, it is difficult to achieve representativeness with the inclusion of only six hospitals from one country in the sample. Second, only patients with stroke were included in this study, making it difficult to extend the conclusions drawn to other rehabilitation patients. Third, nursing hours were observed for only 24 hr, so the daily changes could not be observed. Further study should include various rehabilitation patients in the rehabilitation ward, and furthermore, if nursing hours can be directly observed for longer than 24 hr, it will be a fundamental study on the nursing staffing level for the rehabilitation ward.
6 CONCLUSIONS
This study analysed the association between clinical characteristics of patients with stroke and nursing hours given by nursing staff for rehabilitation patients. Nursing hours were affected by cognitive and balance functions and dependency levels. The worse the cognitive function, balance ability and dependency level, the more were the nursing hours given to the patients. Cognitive function, balance and dependency level should be considered as factors that measure the nursing care needs of stroke rehabilitation patients. Therefore, the results of this study can be useful in determining the nursing staffing levels for stroke rehabilitation patients.
RELEVANCE TO CLINICAL PRACTICE
The practical implications of our findings are that patients with poor cognitive function, balance ability and ADLs need more nursing hours, and more nursing personnel should be deployed to give sufficient quality nursing to take care of patients with these problems. The appropriate nurse staffing levels should be determined based on patient nursing care needs (Cho et al., 2020, 2017). Measuring required nursing hours is the most direct method of determining the degree of nursing activities required for patient care; however, in reality, it is difficult to measure the nursing hours given to patients. Since cognitive function, balance ability and dependency level have been found to be indicators that predict nursing hours, patients' nursing care needs can be evaluated indirectly using these factors. This could give the basis for determining the adequate nursing staff levels for stroke rehabilitation patients.
AUTHOR CONTRIBUTIONS
Study design: HL, SL; Data collection: HL, SL; Data analysis: HL, KL; Study supervision: SL; Manuscript writing: HL, KL; Critical revisions for important intellectual content: HL, KL, SL.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
ETHICAL STATEMENTS
The study was conducted in accordancewith the guidelines of the Declaration of Helsinki and was approved by theGachon University Institutional Review Board (IRB No. 1044396-202004-HR-075-03). Informed consentwas obtained after explaining the study objectives to the ward nurses andparticipating patients.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.