The ability of critical care nurses to identify pressure injury and incontinence-associated dermatitis: A multicentre cross-sectional survey
Abstract
Aim
To investigate the ability of critical care nurses to identify pressure injury and incontinence-associated dermatitis and analyse the possible influencing factors.
Design
Cross-sectional survey.
Methods
This study was conducted at 24 hospitals across 12 provinces in China. A self-made electronic questionnaire was used. Nurses identified and judged injuries according to the information provided.
Results
The average identification score for pressure injury and incontinence-associated dermatitis was 9.00 ± 3.51 points, and only 2.16% of nurses scored ≥16 points. The average correct identification rate for pressure injury and incontinence-associated dermatitis was 45%. The correct identification rate for stage 1 pressure injury was the highest, while those for stage 3, stage 4, deep tissue pressure injury and unstageable pressure injury were all lower than 50%; incontinence-associated dermatitis was also easily misjudged. Nurses' educational backgrounds, professional titles, job positions, hospital levels and learning frequency were the factors that affected their ability to identify pressure injury and incontinence-associated dermatitis.
1 INTRODUCTION
Pressure injury is one of the most frequently occurring adverse events in hospitals, and the incidence of pressure injury is an essential indicator of the quality of hospital care (European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance, 2019). The ICU is a high-risk department for pressure injury occurrence, and the prevalence and incidence rate of pressure injury in critically ill patients has been reported to be 11.5%–32.7% and 3.0%–39.3% respectively (Chaboyer et al., 2018); pressure injury results in a series of harms to patients, increases patients' pain, prolongs the hospital stay, increases medical costs and reduces quality of life (Labeau et al., 2021). Incontinence-associated dermatitis (IAD) is a type of irritant contact dermatitis (inflammation of the skin) found in patients with faecal and/or urinary incontinence (Proceedings of the Global IAD Expert Panel, 2015). It is the most common complication in patients with incontinence, with prevalence and incidence rates of 50%–95% and 10%–50%, respectively, among patients in the ICU (Campbell et al., 2016; Coyer & Campbell, 2018; Gray et al., 2012). Since the concept of IAD was put forward in 2005 and related documents were issued, IAD has received extensive attention in the international wound, ostomy and incontinence fields(Gray et al., 2012). Given that pressure injury and IAD both tend to occur on patients' buttocks and have relatively similar wound appearance, they can easily cause confusion in clinical identification (Beeckman et al., 2008; Defloor & Schoonhoven, 2004). Although scholars had summarized the relationship and difference between IAD and pressure injury, and clearly proposed ways to accurately identify and judge pressure injury and IAD (Black et al., 2011; Browning et al., 2018; Proceedings of the Global IAD Expert Panel, 2015), there is evidence that healthcare providers have difficulties distinguishing between superficial skin injuries and early-stage pressure injuries because of the very subtle differences (Francis, 2019). In addition, nurses have been found to demonstrate a low level of knowledge about IAD identification (Şahin et al., 2019; Zhang et al., 2021), as well as the classification of pressure injuries (Deng et al., 2014; Rodriguez-Calero et al., 2021).
Due to impaired cognition, reduced mobility, perfusion problems, hypoproteinaemia, poor tissue tolerance and incontinence, patients in the ICU have a much higher incidence of pressure injury and IAD than patients in general wards (Beeckman et al., 2014; Wang et al., 2018). Consequently, it is essential for critical care nurses to master the knowledge and skills of the classification system of pressure injury and differential diagnostic ability to provide more targeted management to promote recovery of the patients and avoid medical disputes (Francis, 2019; Gray et al., 2012). However, large-scale information about Chinese critical care nurses' ability to identify pressure injury and IAD is lacking. Therefore, it is worthwhile to explore nurses' ability to identify pressure injury and IAD as well as the possible influencing factors, as the findings may contribute to the development of more effective education and training strategies.
1.1 Aim of the study
This study aimed to assess nurses' ability to identify pressure injury and IAD and analyse the possible influencing factors.
1.2 Research questions
- What are the levels of nurses' ability to identify pressure injury and IAD?
- Are there any factors that influence nurses' ability to identify pressure injury and IAD?
2 METHODS
2.1 Research design
A cross-sectional descriptive design was used in this study.
2.2 Setting and sample
2.3 Instruments
In this study, an electronic questionnaire named “A survey of ICU nurses' ability to identify pressure injury and incontinence-associated dermatitis” was administered. The questionnaire was developed according to the international clinical best practice guidelines of pressure injury and IAD (European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance, 2019; Proceedings of the Global IAD Expert Panel, 2015) and was formed through group discussion by an expert group composed of six senior certified wound experts. The expert group members were all teachers from the Sino-German Wound Care Specialist Training School and had rich clinical, teaching and scientific research experience. A preliminary draft of the questionnaire was submitted to another four clinical wound experts for review, feedback and revision. After the measurement, the content validity of the scale was 0.92. The questionnaire included two parts: (1) basic information, including the hospital, department, age, gender, working years, educational background, professional title, job position, part-time or full-time engagement in wound care and frequency of learning wound-related knowledge; (2) differential diagnostic ability evaluation, including 20 questions (including 9 questions on pressure injury, 8 questions on IAD, 3 questions on pressure injury combined with IAD [pressure injury & IAD]), with each question consisting of one picture, a brief description of the location and palpation response (such as non-blanchable erythema), a brief description of the relevant medical history and answer options. According to the given information, the respondents judged the injury in the pictures as stage 1 pressure injury, stage 2 pressure injury, stage 3 pressure injury, stage 4 pressure injury, deep tissue pressure injury, unstageable pressure injury, IAD, pressure injury & IAD, or unable to judge. For each question, 1 point was awarded for the correct selection, and 0 point were awarded for an incorrect selection. The total score was 20 points; the higher the score was, the better the differential diagnostic ability.
2.4 Study procedures
Research data were collected from June 25 to July 23, 2020. The survey was conducted using an online electronic questionnaire posted on the online platform www.wjx.cn. Before the multicentre study, 30 critical care nurses were recruited for the pre-experiment to ensure that the questionnaire could be correctly understood and that the pictures could be clearly displayed. The time required to complete the questionnaire was also estimated. To guarantee the authenticity of the research results, the person in charge of the participating hospitals told the respondents that the survey was anonymous and did not violate any interests of the respondents. Therefore, the respondents did not communicate with each other or read relevant materials when filling out the questionnaire and completed the questionnaire independently. In addition, the order of questions in the electronic questionnaire was set using the random mode; that is the order of questions was randomly generated by the system for each respondent. The time to complete the questionnaire was reasonably limited to 25 min based on the presurvey. The respondents voluntarily participated the survey and were required to complete the electronic questionnaire within 5 day. The head nurse of the participating hospital reminded the participants to complete the questionnaire via an online message or text message on the third day.
2.5 Ethics
All respondents were informed of the study's purpose and significance before filling out the questionnaire. There was an informed consent form on the first page of the questionnaire, and the respondents clicked “confirm” to sign and voluntarily participate in this study. The respondents were informed that they had the right to withdraw from the study at any time without any adverse consequences. This study was approved by the Ethics Committee on Biomedical Research of our hospital (No. 2020-534).
2.6 Data analysis
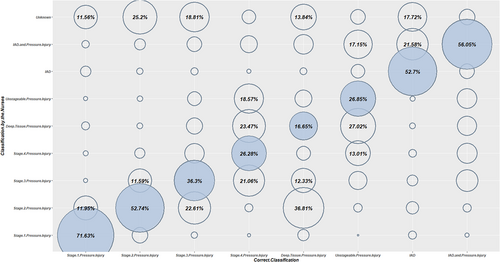
The Kolmogorov–Smirnov test was used to test whether the mean score of the correct answers had a normal distribution according to the demographic characteristics. Categorical variables were described as the frequency and proportion, and continuous variables were described as the mean and standard deviation. A bubble diagram was used to show the distribution relationship between the correct answer and the nurses' answers in the identification of different injuries. The demographic data and basic information of the nurses, such as gender, working years, educational background, professional title, job position, part-time or full-time engagement in wound care and the frequency of learning wound-related knowledge, were explored as factors that might affect nurses' identification ability, and multiple linear regression models were used for statistical analysis. All p values were two-sided, and those less than .05 were considered statistically significant. All data were analysed using R 4.0.2 software (for Windows) (source: https://www.r-project.org/).
3 RESULTS
3.1 Characteristics of the hospitals and ICU nurses
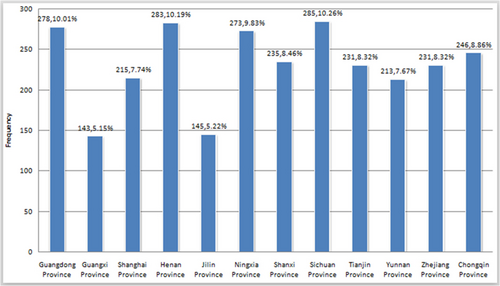
A total of 24 hospitals across 12 provinces participated in this study. The geographical distribution was as follows: four hospitals in East China, four hospitals in South China, two hospitals in North China, two hospitals in Central China, four hospitals in Northwest China, two hospitals in Northeast China and six hospitals in Southwest China. A total of 39 ICUs were involved, including 22 mixed ICUs, six surgical ICUs, two internal medicine ICUs, two neurological ICUs, two emergency ICUs, three respiratory ICUs and two extracardiac ICUs. A total of 2,778 nurses completed the survey as needed. The distribution of the included nurses from the 12 provinces is shown in Figure 1. The age of the included nurses ranged from 19–58, with an average of 30.27 ± 5.94. The working years of nurses ranged from 1–36 years, with an average of 7.99 ± 2.35 years. The nurses' basic information is shown in Table 1.
| Characteristics | N (%) | Mean identification score (M + SD) | Correct identification rate (%) |
|---|---|---|---|
| Gender | |||
| Male | 274 (9.86) | 9.19 ± 3.51 | 45.93 |
| Female | 2,504 (90.14) | 8.98 ± 3.52 | 44.90 |
| Age | |||
| ≤25 years old | 629 (22.64) | 8.30 ± 3.42 | 41.52 |
| 26–35 years old | 1,570 (56.52) | 8.99 ± 3.46 | 44.98 |
| ≥35 years old | 579 (20.84) | 9.77 ± 3.60 | 48.84 |
| Working years | |||
| ≤5 years | 1,212 (43.63) | 8.35 ± 3.44 | 41.74 |
| 6–10 years | 907 (32.65) | 9.17 ± 3.42 | 45.87 |
| >10 years | 659 (23.72) | 9.96 ± 3.53 | 49.80 |
| Education background | |||
| Secondary school | 64 (2.31) | 6.25 ± 3.16 | 31.25 |
| Junior college | 1,028 (37.00) | 8.02 ± 3.41 | 40.09 |
| Bachelor's | 1,657 (59.65) | 9.67 ± 3.39 | 48.34 |
| Master's | 29 (1.04) | 11.72 ± 2.67 | 58.62 |
| Professional title | |||
| Nurse | 904 (32.54) | 7.79 ± 3.38 | 38.96 |
| Senior nurse | 1,280 (46.08) | 9.15 ± 3.41 | 45.75 |
| Supervisor nurse and above | 594 (21.38) | 10.52 ± 3.28 | 52.58 |
| Job position | |||
| Staff nurse | 2,181 (78.50) | 8.63 ± 3.47 | 43.15 |
| Charge nurse | 336 (12.10) | 9.87 ± 3.60 | 49.18 |
| Head nurse or APN | 261 (9.40) | 11.01 ± 2.85 | 55.06 |
| Hospital level | |||
| Tertiary hospital | 1937 (69.73) | 9.82 ± 3.31 | 49.10 |
| Secondary hospital | 841 (30.27) | 7.11 ± 3.23 | 35.55 |
| Engagement in wound care | |||
| Yes | 341 (12.28) | 9.27 ± 3.76 | 46.33 |
| No | 2,437 (87.72) | 8.96 ± 3.48 | 44.81 |
| Frequency of learning wound-related knowledge every year | |||
| >5 time | 356 (12.81) | 9.48 ± 3.80 | 47.40 |
| 4–5 times | 1,570 (56.52) | 9.32 ± 3.42 | 46.61 |
| 2–3 times | 579 (20.84) | 8.73 ± 3.43 | 43.64 |
| ≤1 time | 273 (9.83) | 7.10 ± 3.16 | 35.51 |
- Abbreviation: APN, advanced practice nurse.
3.2 Nurses' ability to identify pressure injury and IAD
The identification scores of the critical care nurses for pressure injury and IAD ranged from 0–19 points (the total score was 20 points), with an average of 9.00 ± 3.51 points. Nearly 18% (493) of the nurses scored ≤5, 45.97% (1277) scored 6–10, 34.13% (948) scored 11–15 and 2.16% (60) scored 16–20. More information is shown in Table 1. The overall correct identification rate of wound pictures was 45% (25,002/55,560), and deep tissue pressure injury was most frequently classified incorrectly (Table 2). A total of 36.30% of stage 3 pressure injury pictures were classified correctly, and 22.61% were misjudged as stage 2. For stage 4 pressure injury pictures, 26.28% were classified correctly, and 21.06%, 23.47% and 18.57% were judged as stage 3, deep tissue damage and unstageable pressure injury respectively. Only 16.65% of deep tissue pressure injury pictures were classified correctly, and 36.81% were misjudged as stage 2. A total of 26.85% of unstageable pressure injury pictures were classified correctly, and 27.02% were misjudged as deep tissue damage. More information is shown in Figure 2.
| Injury type | Number of pictures | Number of identification attempts | Number of correct identifications | Correct rate (%) |
|---|---|---|---|---|
| Stage 1 pressure injury | 1 | 2,778 | 1990 | 71.63 |
| Stage 2 pressure injury | 1 | 2,778 | 1,465 | 52.74 |
| Stage 3 pressure injury | 2 | 5,556 | 2017 | 36.30 |
| Stage 4 pressure injury | 1 | 2,778 | 730 | 26.28 |
| Deep tissue pressure injury | 2 | 5,556 | 925 | 16.65 |
| Unstageable pressure injury | 2 | 5,556 | 1,492 | 26.85 |
| IAD | 8 | 22,224 | 11,712 | 52.70 |
| IAD & pressure injury | 3 | 8,334 | 4,671 | 56.05 |
| Total | 20 | 55,560 | 25,002 | 45.00 |
- Note: The correct identification rate of a certain type of wound = the number of correct identifications of a certain type of wound/the total number of identification attempts of this type of wound. The staging of pressure injury is based on the Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System (Edsberg et al., 2016; National Pressure Ulcer Advisory Panel, 2016).
3.3 Factors affecting nurses' ability to identify pressure injury and IAD
As shown in Table 3, the multivariate linear regression model showed that the educational backgrounds, professional titles, job positions, hospital levels and annual frequency of learning wound-related knowledge of critical care nurses were the factors that affected the ability of critical care nurses to identify pressure injury and IAD (p < .05).
| Item | Classification | Beta coefficient | Standard error | t | p Value | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|---|---|
| Gender | Male | – | – | – | – | ||
| Female | −0.25 | 0.201 | −1.245 | .213 | −0.644 | 0.144 | |
| Working years | ≤5 years | – | – | – | – | ||
| 6–10 years | 0.04 | 0.159 | 0.254 | .8 | −0.272 | 0.352 | |
| >10 years | −0.428 | 0.232 | −1.844 | .065 | −0.883 | 0.027 | |
| Education background | Secondary school | – | – | – | – | ||
| Junior college | 1.185 | 0.404 | 2.937 | .003 | 0.393 | 1.977 | |
| Bachelor's | 1.859 | 0.409 | 4.542 | <.001 | 1.057 | 2.661 | |
| Master's | 2.28 | 0.72 | 3.166 | .002 | 0.868 | 3.692 | |
| Professional title | Nurse | – | – | – | – | ||
| Senior nurse | 0.684 | 0.168 | 4.071 | <.001 | 0.355 | 1.013 | |
| Supervisor nurse and above | 1.643 | 0.266 | 6.173 | <.001 | 1.121 | 2.165 | |
| Job position | Staff nurse | – | – | – | – | ||
| Charge nurse | 0.352 | 0.217 | 1.609 | .108 | −0.074 | 0.778 | |
| Head nurse or APN | 1.171 | 0.242 | 4.839 | <.001 | 0.696 | 1.646 | |
| Hospital level | Tertiary hospital | – | – | – | – | ||
| Secondary hospital | −2.304 | 0.131 | −17.621 | <.001 | −2.561 | −2.047 | |
| Engagement in wound care | Yes | – | – | – | – | ||
| No | −0.048 | 0.186 | −0.258 | .796 | −0.413 | 0.317 | |
| Frequency of learning wound-related knowledge every year | >5 times | – | – | – | – | ||
| 4 ~ 5 times | −0.102 | 0.187 | −0.545 | .586 | −0.469 | 0.265 | |
| 2 ~ 3 times | −0.447 | 0.215 | −2.076 | .038 | −0.869 | −0.025 | |
| ≤1 time | −1.63 | 0.258 | −6.319 | <.001 | −2.136 | −1.124 |
- Note: Due to the obvious collinearity between age and working years, only working years was included in the analysis according to research needs. β*, standard regression coefficient. Regression model R2 = .325, adjusted R2 = .313, F = 132.538, p < .001.
4 DISCUSSION
To our knowledge, this is the first attempt to investigate the ability of critical care nurses to identify pressure injury and IAD within a large-scale multicentre survey in mainland China and to examine its possible influencing factors. Consistent with our hypothesis, the ability of critical care nurses to distinguish pressure injury and IAD was less than ideal, and some basic information of critical care nurses was identified to be crucial for their differential diagnostic ability, which provides an important guide for the development of more effective teaching strategies and thus for the improvement of the quality of care.
The results showed that nurses scored an average of 9.00 ± 3.51 points for the identification of pressure injury and IAD, the overall correct identification rate of pressure injury and IAD pictures was 45%, and only 36.29% of nurses had a correct identification rate ≥ 50%, which suggests that it is difficult for nurses to correctly differentiate between pressure injury and IAD. Lee et al. used the PUCS & IAD VDT to survey 602 nurses in South Korea and found that the average score of nurses in identifying pressure injury and IAD was 11.15 ± 4.90 points (the total score was 21 points) and that the nurses' identification ability was poor (Lee & Kim, 2016). A study of 1,217 nurses who attended a wound care conference revealed that only 44.5% of the pressure injuries and IAD pictures were classified correctly before educational intervention (Beeckman et al., 2010). Another study including 473 nurses also revealed that nurses had poor consistency in wound identification (Defloor et al., 2006). In mainland China, the term IAD was introduced relatively late, this type of skin problem was often referred to as perineal dermatitis or diaper rash, and less clinical attention was given to it. It was not until 2012 that the term IAD officially appeared in the literature in mainland China for the first time, and the relationship between IAD and pressure injury and the identification of the two attracted the attention of Chinese nurses (Wang & Duan, 2012). Therefore, the results of this study are similar to earlier studies in other countries that have focused on IAD.
Specifically, critical care nurses had the highest identification correct rate for stage 1 pressure injury (71.63%), while the correct identification rates of stage 3 pressure injury, stage 4 pressure injury, unstageable pressure injury and deep tissue pressure injury were low. This was consistent with a study in South Korea, which reported that nurses had a significantly lower identification correct rate for stage 3 pressure injury, unstageable pressure injury and deep tissue pressure injury (Lee & Kim, 2016). A more recent study conducted by Rodriguez-Calero found that stage 1 pressure injury achieved 85.60% agreement among nurses, while a substantially lower level of agreement was obtained for unstageable/deep tissue pressure injury (Rodriguez-Calero et al., 2021). However, some studies found that nurses had the worst correct identification rate for stage 1 and stage 3 pressure injuries (Beeckman et al., 2010). This discrepancy may be due to the pressure injury classification system used in Beeckman's study being an older version. Our results revealed that nurses tended to misjudge stage 3 as stage 2 pressure injury and stage 4 as stage 3 pressure injury, indicating that they were prone to inaccurately identifying the wound depth and characteristics, which was also supported by other studies (Beeckman et al., 2007; Defloor et al., 2006). In addition, nurses were likely to confuse stage 4 pressure injury, unstageable pressure injury and deep tissue pressure injury, which may be because nurses in some secondary hospitals have not fully understood the updated pressure injury classification system. This study also found that nurses tend to classify all intact or ruptured blisters as stage 2 pressure injuries, regardless of the colour of the wound bed. According to the updated pressure injury stages, epidermal separation revealing a dark wound bed or blood-filled blister should be considered deep tissue pressure injury (National Pressure Ulcer Advisory Panel, 2016), but ICU nurses tend to misdiagnose such injuries as stage 2 pressure injury. When IAD is serious, nurses tend to misjudge it as IAD combined with pressure injury or pressure injury, which means that once the skin affected by IAD is broken down, nurses' judgement will be easily confused.
Regarding the possible influencing factors of the ability of critical care nurses to distinguish pressure injury and IAD, our results revealed that higher educational level, higher professional title, higher job position and higher frequency of learning were associated with better differential diagnostic ability among nurses. Lee et al. also found that job position and frequency of learning wound-related knowledge were factors affecting nurses' identification ability (Lee et al., 2013). Highly educated nurses had better independent learning ability and strong acceptance ability, while nurses with higher professional titles and job positions might also have better clinical identification ability due to their longer working years and greater accumulation of clinical experience. Continuous updating of knowledge related to wounds, a higher learning frequency, higher exposure to new knowledge and strong acceptance ability might enable nurses to have better identification ability. Another important finding is that the identification ability of nurses in tertiary hospitals was better than that of nurses in secondary hospitals. In China, tertiary hospitals are the highest-level hospitals and are usually affiliated with universities. These hospitals often hold teaching activities and academic conferences, so nurses in tertiary hospitals update their knowledge more quickly, receive more training, and have greater opportunities to improve their abilities. However, this study also found that whether nurses were engaged in wound management was not an influencing factor. This might be related to the shortage of wound professionals in China; although some hospitals in China have arranged for nurses to take part-time jobs in wound management, these nurses do not receive professional training or continuously update their knowledge. Thus, there were few differences between these nurses and other nurses.
Preliminary studies suggest that education can address the difficulties in accurately determining the type of skin injuries and pressure injury stages (Beeckman et al., 2007; Ham et al., 2015). Based on this study's findings, it is necessary to carry out continuing education and adopt scientific teaching strategies to improve the ability of critical care nurses to identify pressure injury and IAD. Currently, training on pressure injury and IAD for nurses in mainland China focuses more on theoretical training. Even though there are pictures or case presentations in training, the evaluation is knowledge-based. Future education and training programs should change this mode and focus on clinical practice ability. Furthermore, the current model of continuing education is generally classroom-based, and nurses are often unable to attend due to their work demands, shift work, or resource constraints. If repeated learning is needed, it would be difficult to obtain the learning resources again, and the learning frequency would be significantly limited. Therefore, we should follow the development of informatization and release training with the help of a network platform (such as establishing a training tool similar to PUCLAS [Beeckman et al., 2007]), update the platform regularly and urge nurses to repeatedly study to reduce the gap between theoretical knowledge and clinical practice capabilities.
5 LIMITATIONS
Some limitations must be considered when interpreting these findings. First, in this study, 20 sets of pictures were used for nurses to make judgements, but pictures can only provide two-dimensional information, and the visibility of different tissue layers may be limited. Bedside evaluation can provide more clinical information on the evolution of wound or skin damage, which may be helpful to accurately interpret the aetiology or healing prognosis. Second, although we adopted some measures to avoid other interfering factors, such as nurses' mutual influence or the use of teaching materials, on the nurses' clinical identification ability, we could not fully guarantee that the nurses completed the questionnaires independently in accordance with our requirements. As a result, future research is warranted to verify the present results. Third, we evaluated the contribution of only some basic information to the nurses' clinical identification ability, and it would be interesting to further explore additional factors that can potentially improve nurses' knowledge, visual discrimination ability and clinical judgement, such as nurses' learning attitude and application of virtual simulation technology.
6 CONCLUSION
Our survey revealed that critical care nurses had a poor ability to identify pressure injury and IAD. Nurses' professional titles, education backgrounds, job positions, hospital levels and annual wound knowledge learning frequency affected their ability to identify wounds. The findings suggest that critical care nurses' ability to distinguish pressure injury from IAD urgently needs to be improved. The current study indicates the necessity and importance of providing continuous teaching and training for critical care nurses. Moreover, attention should be given to summarizing and emphasizing the confusion between the clinical judgement of pressure injury and IAD and bridging the gap between theoretical knowledge and clinical practice. Further exploration of other factors that might influence nurses' clinical identification ability for pressure injury and IAD is suggested.
AUTHOR CONTRIBUTIONS
HL contributed to the study conception, design and drafting of the manuscript. AD, MG, JM, XS, DH and XC contributed to the data collection. SJ contributed to data analysis. YT contributed to critical revisions of the manuscript and supervised the study.
- substantial contributions to conception and design, acquisition of data or analysis and interpretation of data;
- drafting the article or revising it critically for important intellectual content.
ACKNOWLEDGEMENT
The authors thank all the nurses and the hospitals who took part in the study.
FUNDING INFORMATION
This study is supported by Sichuan Science and Technology Program (No. 2019YFS0290).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICAL APPROVAL
This study was approved by the Ethics Committee on Biomedical Research of West China Hospital of Sichuan University (No. 2020-534).
INFORMED CONSENT
All respondents were informed of the study's purpose and significance before filling out the questionnaire. There was an informed consent form on the first page of the questionnaire, and the respondents clicked “confirm” to sign and voluntarily participate in this study. The respondents were informed that they had the right to withdraw from the study at any time without any adverse consequences.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.