Knowledge, attitudes and practices concerning catheter-associated urinary tract infection amongst healthcare workers: a mixed methods systematic review
Abstract
Aim
To evaluate healthcare workers' knowledge, attitudes and practices level of prevention and management of catheter-associated urinary tract infection.
Design
A mixed-methods systematic review.
Methods
Searches were conducted in CINAHL, Cochrane Library, EMBASE, Medline, PubMed and Web of Science databases. Limited literatures published in English before 20 June 2021. Data were analysed and synthesized using thematic analysis by two authors.
Results
Thirty-four articles were included. Healthcare workers' unbalanced varied knowledge level, positive attitudes, undesirable practices of catheter-associated urinary tract infection's prevention and control were identified. Barriers of healthcare workers' knowledge, attitudes and practices level of infection prevention included heavy workload, understaffing, physician variability in indwelling urinary catheter (IUC) practice by diagnosis, nursing variability in IUC placement technique, poor relationship and nurse's poor documentation. Leadership, better education, teamwork, technique training and information technology support, advocacy for nurse-driven protocol and IUC removal reminder were considered as facilitators.
1 INTRODUCTION
Catheter-associated urinary tract infection is the urinary system infection that occurs in 48 hours after indwelling or removing the urinary catheter. The CDC (Centers for Disease Control and Prevention) updated CAUTI criteria in 2018. Patient must meet (1), (2) and (3): (1) Patient had an indwelling urinary catheter that had been in place for more than two consecutive days in an inpatient location on the date of event. (2) Patient has at least one of the following signs or symptoms: fever (>38.0°C), suprapubic tenderness, costovertebral angle pain or tenderness, urinary urgency, urinary frequency and dysuria. (3) Patient has a urine culture with no more than two species of organisms identified, at least one of which is a bacterium of ≥105 CFU/ml. CAUTI is one of the most common nosocomial infections (Saint et al., 2016). As a common adverse event amongst inpatients with indwelling urinary catheters, it can prolong length of stay and increase costs, or even cause urosepsis at worst, which is cannot be overlooked (Cathy, 2019).
The KAP model (knowledge-attitude-practice, KAP) is the most commonly model to explain how personal knowledge and attitudes affect their healthy behaviour. It was proposed by Mayo in the 1960s. “Knowledge” means the understanding and cognition of relevant knowledge. “Attitude” means the correct belief. “Practice” means the behaviour. There is a dialectical relationship between these three elements: knowledge is the basis of behaviour change; attitude is the driving force of behaviour change (Liu & Bao, 2004). Only when people sublimate knowledge into faith, can they take a positive attitude to change their behaviour. Therefore, healthcare workers (HCWs) with good knowledge, attitudes and practices are essential to CAUTI's prevention and control. Based on this theory, it is essential to identify the HCWs' knowledge, attitudes and practices level of prevention and management of catheter-associated urinary tract infection from previous studies, providing basis for the development of healthcare worker-related education projects.
2 BACKGROUND
CAUTI has been considered as a common adverse event amongst inpatients with indwelling urinary catheters (Cathy, 2019). The United States of America identified the CAUTI rate as one of the top ten safety goals for patients in 2017 (Gould et al., 2017). With the prolongation of catheterization time, the incidence of bacteriuria is close to 100% in 30 days after catheterization, then 1%–4% of bacteriuria will evolve into urosepsis (Li et al., 2019), it prolongs the length of stay, increases costs and mortality. Besides, prophylactic antibiotic treatment is a conventional prevention treatment method of CAUTI. Some studies indicated that about 52% of patients with catheter-associated asymptomatic bacteriuria (CA-ABU) were treated with inappropriate antibiotics (Khawcharoenporn et al., 2011). It causes continually increasing of the burdens of antimicrobial stewardship.
HCWs play a pivotal role in putting infection prevent and control measures into effect. A study showed that if guidelines are strictly followed, 69% of infections can be avoided (Septimus & Moody, 2016). Only when HCWs sublimate bountiful knowledge of CAUTI into belief, can they take a positive attitude to improve their practice on prevention and management of CAUTI. Especially, the nurses who are important participants in infection prevention, they have more responsibility in maintaining patient care and treatment. It will lead to the increase in the opportunity of bacteria colonization and the spread of infection if they are lack of relevant knowledge and normative behaviour practice. (Carter et al., 2016).
The World Health Organization declared that education and training of healthcare workers is a core of infection prevention (WHO, 2017). It has been proved that taking healthcare professional's education into CAUTI prevention programmes contributes to reducing catheterization time (Lo et al., 2014). To meet demands of CAUTI's prevention and management, education and training of healthcare workers on catheterization indication, catheter insertion and care, early removal of urinary catheter is vital. But several research about healthcare worker's educational intervention paying close attention to the outcome of CAUTI rates rather than variation of HCWs' knowledge, attitude and practices level. (Blondal et al., 2016). In addition, there is a lack of relevant summative articles about knowledge, attitude and practices of healthcare workers in CAUTI. Therefore, to give basis for targeted infection prevention (TIP) studies of CAUTI, it is necessary and significant to evaluate the level of healthcare workers' knowledge, attitudes and practices.
2.1 Aims
- What is the knowledge, attitudes and practices level of CAUTI amongst healthcare workers?
- What are the barriers and facilitators of healthcare workers' prevention and control for CAUTI?
3 THE REVIEW
3.1 Design
We used descriptive analysis methods to make quantitative analysis and used a results-based mixed-methods synthesis design – thematic analysis to make quantitative and qualitative study's data synthesis (Noyes et al., 2019). The protocol for this systematic review was registered at PROSPERO (CRD42021274574). This review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (Liberati et al., 2009).
3.2 Search methods
Six databases: CINAHL, Cochrane Library, EMBASE, Medline, PubMed and Web of Science were included in the search. Searched relevant literatures published in English before 20 June 2021. Medical subject headings (MeSH) and keywords for ‘urinary tract infections’ or ‘catheter-associated urinary tract infection’, ‘nurses’ or ‘health personnel’, ‘health knowledge, attitudes, practice’ were combined to form the search terms (Table 1). Boolean operators AND, OR and NOT (if applicable in a database) were applied to broaden or limit search scope. Hand searching of list of references, citation tracking was for finding more extra articles.
| Block 1 | Block 2 | Block 3 |
|---|---|---|
| Urinary tract infection | Nurs* | Knowledge* |
| Urinary-tract-infection* | Nursing Personnel* | Perception* |
| Catheter-associated urinary tract infection* | Registered Nurse* | Attitude* |
| CAUTI | Nursing staff, hospital | Opinion* |
| Urinary Catheter* | Health Personnel* | Practice* |
| Ureteral Catheter* | Healthcare Provider* | Health Knowledge, Attitudes, Practice [MeSH Terms] |
| Urethral Catheter* | Healthcare Provider* | Knowledge [MeSH Terms] |
| Foley* | Healthcare Worker* | Perception [MeSH Terms] |
| Indwelling urinary catheter* | Healthcare Professional* | Attitude [MeSH Terms] |
| Urinary Catheterization | Physician* | Attitude to health [MeSH Terms] |
| Ureteral Catheterization | Nurses [MeSH Terms] | Nursing Faculty Practice [MeSH Terms] |
| Urethral Catheterization | Health Personnel [MeSH Terms] | Professional Practice [MeSH Terms] |
| Foley Catheterization | Physicians [MeSH Terms] | |
| Urinary tract infection [MeSH Terms] | ||
| Urinary Catheter [MeSH Terms] | ||
| Urinary Catheterization [MeSH Terms] |
The inclusion criteria were as follows: (i) population: Registered Nurses, licensed practical nurses, bedside nurses, nurse aides, nurse manager, attending physicians, resident physicians, healthcare assistants and other allied healthcare professionals (case manager, mid-levels such as nurse practitioners and physician assistants). (ii) interest of phenomenon or intervention: evaluated healthcare worker's knowledge, attitude and practice of CAUTI (about management of urinary catheter or compliance situation of CAUTI guidelines), CAUTI's intervention strategy (about prevention or control intervention). (iii) outcomes: HCW's knowledge, attitude and practice level of CAUTI. (iv) setting: in hospitals or nursing homes. (v) study/design: quantitative, qualitative or mixed-methods study.
The exclusion criteria were as follows: (i) Population: interns without qualifications. (ii) conference papers, policies, letters, editorials, case studies, position statements or systematic reviews. (iii) the full text is not visible.
3.3 Search outcome
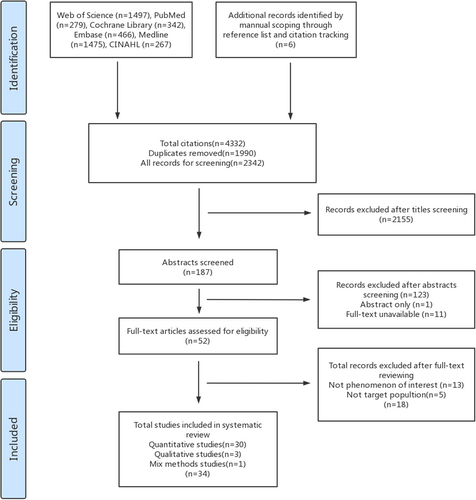
Referring to the Preferred Reporting Items for Systematic review Protocol (PRISMA-P). Two authors were responsible for literature screening, when disagreement occurs, analysed and decided by another author. A total of 4,332 were identified in initially retrieval. Of these, 1990 duplicates were removed using software of ENDNOTE. After titles and abstract were screened, there were still 64 articles left. Since one study was abstract only, 11 studies were not visible in full text, 52 articles were eligible for full-text review. As 13 studies did not give the phenomenon of interest, five studies failed to meet the criteria for the target population, 34 articles were finally included in our research. PRISMA flow chart see Figure 1.
3.4 Quality appraisal
The Mixed Methods Appraisal Tool (MMAT) was applied by two authors to independently assess the methodological quality of included studies (Table 2) (Hong et al., 2018). The divergences were solved by discussion. Despite Hong et al. (Hong et al., 2018) suggested that it was more informative to reporting complete findings than to calculating quality score, they added that a score can be better used for narrative section. Therefore, we adopted Martin et al (Martin et al., 2020) scoring method to making quality score of all included studies. Assigned a value: yes = 1; no or cannot tell = 0 and divided studies into low (score ≤3) or high level (score >3). Based on recommendation of Hong et al. (Hong et al., 2018), it is not enough to judge which aspects of studies are problematic by a single score and even it might hide serious defects of studies. Therefore, we did not excluded articles according to the study's methodological quality score.
| Author/Year | Study design | MMAT criteria for qualitative studies | ||||
|---|---|---|---|---|---|---|
| 1.1 | 1.2 | 1.3 | 1.4 | 1.5 | ||
| B H Roe (1989) | Qualitative study | Y | Y | Y | Y | Y |
| Jane, 1997 | Qualitative study | Y | Y | Y | Y | Y |
| Mary R.Mulcare et al. (2015) | Qualitative study | Y | Y | Y | Y | Y |
| 3.1 | 3.2 | 3.3 | 3.4 | 3.5 | ||
| Mohamad G.Fakih et al. (2013) | Retrospective analysis | N | N | Y | N | Y |
| Brenda Shaver et al. (2018) | Prospective cohort study | N | N | Y | N | Y |
| Sonali D. Advani et al. (2019) | Retrospective chart review | Y | Y | N | Y | Y |
| Monina Hernandez et al. (2019) | Non-randomized controlled trials | Y | N | Y | N | Y |
| 4.1 | 4.2 | 4.3 | 4.4 | 4.5 | ||
| Tracey J. Siegel (2006) | Cross-sectional study | Y | N | Y | Y | Y |
| Asteria LM Ndomba et al. (2008) | Cross-sectional study | Y | Y | C | Y | Y |
| Weerakoon & Lawrentschuk, 2010 | Cross-sectional study | C | N | C | Y | Y |
| Dimitri M.Drekonja et al. (2010) | Cross-sectional study | Y | Y | C | N | Y |
| Dimitri M.Drekonja et al. (2010) | Cross-sectional study | Y | N | C | N | Y |
| Lona Mody et al. (2010) | Cross-sectional study | N | C | Y | Y | Y |
| Ana Montoya et al. (2013) | Cross-sectional study | Y | N | C | Y | Y |
| Fernández-Ruiz et al. (2013) | Cross-sectional study | Y | N | Y | Y | Y |
| Shuko Maeda et al. (2013) | Cross-sectional study | Y | Y | Y | Y | Y |
| MARK LISTER F. Opina & Oducado, (2014) | Cross-sectional study | Y | C | N | Y | N |
| Kartik Viswanathan et al. (2015) | Cross-sectional study | Y | N | Y | N | Y |
| Manisha et al. (2015) | Cross-sectional study | N | N | Y | Y | Y |
| Yildiz Kose et al. (2016) | Cross-sectional study | Y | Y | C | Y | Y |
| Karen Jones et al. (2016) | Cross-sectional study | Y | C | N | C | Y |
| Shah et al. (2017) | Cross-sectional study | Y | Y | N | Y | Y |
| Kulbay & Tammelin, 2018 | Cross-sectional study | N | Y | Y | Y | Y |
| MC Cutinho et al. (2018) | Cross-sectional study | N | Y | N | Y | Y |
| Tenzin Dawa et al. (2019) | Cross-sectional study | Y | N | Y | N | Y |
| Salha Salem Algarni et al. (2019) | Cross-sectional study | Y | Y | Y | Y | Y |
| Andrea Niederhauser et al. (2019) | Cross-sectional study | Y | N | Y | N | Y |
| Sanniya Khan Ghauri et al. (2019) | Cross-sectional study | Y | N | Y | N | Y |
| Kelly Thomas (2020) | Cross-sectional study | Y | Y | N | N | Y |
| Andrea Niederhauser et al. (2020) | Cross-sectional study | Y | N | Y | N | Y |
| Anns M. Benny et al. (2020) | Cross-sectional study | Y | Y | Y | Y | N |
| Ivy Mong BNSc et al. (2021) | Cross-sectional study | Y | N | Y | Y | Y |
| Balu et al. (2021) | Cross-sectional study | Y | Y | Y | N | Y |
| 5.1 | 5.2 | 5.3 | 5.4 | 5.5 | ||
| Brian T Conner, (2013) | Mixed method study | Y | Y | Y | Y | Y |
- Note: C = Cannot tell, means that the paper does not report appropriate information to answer ‘Yes’ or ‘No’.
3.5 Data extraction
Two authors are responsible for data extraction. They designed a data extraction table which contains the following variables: (i) authors, year and country of study, (ii) methodology, (iii) population, (iv) instruments, (v) focus point and (vi) key findings. Each study is arranged in chronological order (Table 3). Disagreements were solved by discussion of two authors or consultation of third author.
| Author/Year/Country | Methodology | Population | Instruments | Focus point | Key findings |
|---|---|---|---|---|---|
| B H Roe (1989)/England | Qualitative, | N = 106 nurses | Semi-structured interview | Investigated the information given by 106 hospital and district nurses to patients who are to use an indwelling urethral catheter in the community, and their careers. |
· The information given for catheter care was not comprehensive nor consistent and differed according to the nurse's location of work. · This nursing practice implicated a need for further education of nurses about catheter care. |
| Jane, 1997/England | Qualitative, | N = 12 first-level registered nurses | Unstructured interviews | First, what care do nurses give with the aim of preventing catheter-associated NUTIs; secondly, what improvements in practice would further prevent catheter-associated NUTIs; thirdly, what do nurses see as constraints to the prevention of catheter-associated NUTIs? |
· Two broad themes: nursing practice and procedures included the need for risk assessment of patients and the need for rationale for practice; resources plus additional findings. · Nurses stated that their practice differed because of a lack of time to give care and to update themselves. · The consequences of understaffing were that junior and temporary staff (whose competence in preventing NUTIs was questioned) worked unsupervised. · Those interviewed identified feelings of powerlessness in effecting preventative measures and identified not only the role of medical staff in influencing NUTIs but also their inconsistent approach to care. |
| Tracey J. Siegel (2006)/USA | Quantitative, survey method | N = 82 nurses | The Catheter Anchoring Survey (CAS), based on experts' discussion and literature review, having content validity. |
To determine if registered nurses employed at an acute care facility perceived the anchoring of IUCs as necessary. |
· Ninety-eight per cent of the registered nursing staff agreed that they anchored catheters, that IUCs should be stabilized, but this perception did not concur with current practice. · Ninety-nine per cent of participants disagreed that a physician order was needed to stabilize IUC. |
| Asteria LM Ndomba et al. (2008)/Tanzania | Quantitative, survey and observational method | N = 135 nurses | A structured questionnaire, based on experts' discussion and literature review. Unspecified validity and reliability. | To investigate nurses' knowledge and clinical practice about care of patients with IUC in preventing nosocomial infections. |
· The nurses' overall knowledge was good: it was found that 110 of 135 nurses (81.5%) had good knowledge and the remaining 25 nurses (18.5%) had poor knowledge. · Many nurses' answers about the 18 questions were also answered unsatisfactorily. The weakest areas (<60% adequate answers) were how and where to attach the collection bags (Q3and Q4), emptying of urine bag (Q9), securing of the IUC to the thigh (Q11, Q12), and cleaning after bowel opening (Q13). · There was a discrepancy between knowledge and clinical practice: appropriate securing of the IUC, hand washing before and after meatal cleaning and bag emptying, asking patients how they felt once the IUC was in place, monitoring of fluid intake charts and the bag not resting on the floor. · Hand washing prior to care for patients with IUC was poor due to lack of water and soap. |
| Weerakoon & Lawrentschuk, 2010 | Quantitative, survey method |
N = 315 87 doctors and 228 nurses |
A self-administered questionnaire. Unspecified validity and reliability. | Assess the attitudes of doctors and nurses to infection control, occupational health and safety issues, and environmental waste. |
· Doctors and nurses were concerned about infection control, occupational health and safety issues, and environmental waste. Incidents involving spillage of urine and/or blood often go unreported. · There were no differences between nurses and doctors having specialist training in urology or experience (p > 0.05). |
| Dimitri M.Drekonja et al. (2010)/American | Quantitative, survey method |
N = 635 licensed physicians |
An Internet-based questionnaire. Unspecified validity and reliability. | Assessment of physicians' knowledge and attitudes about catheters. |
· Overall, respondents exhibited good knowledge about indications for catheterization. · Most respondents reported awareness of the changed reimbursement policy for CAUTI; fully one-third indicated that because of this change, they now removed catheters earlier than previously. · The responses from primary care physicians and surgeons differed significantly in terms of indications for catheterization, methods to prevent CAUTI, and the impact of the policy change on their practice patterns. |
| Dimitri M.Drekonja et al. (2010)/American | Quantitative, survey method |
N = 370 registered nurses |
A Internet-based questionnaire. Unspecified validity and reliability. | To assess the current state of RN's knowledge and attitudes abouturinary catheters. |
· Nurses perceived early catheter removal as the most effective intervention to prevent CAUTI (mean score, 4.5; range 1–5). · Most interventions for preventing CAUTI were rated favourably. · Most respondents reported no institutional guidance aboutcatheterization. · Although the surveyed Minnesota RNs demonstrated high-level awareness of the utility of early Foley catheter removal for preventing CAUTI, other aspects of their catheter-related knowledge were concerning. |
| Lona Mody et al. (2010)/American | Quantitative, survey method | N = 356 nurses (registered professional nurse (RN) and licensed practical nurse (LPN)) and nurse aides | A self-administered anonymous questionnaire, based on national recommendations, guidelines and first pilot tested amongst eight nurses. | To evaluate HCWs' knowledge and awareness of recommended practices pertaining to urinary catheter care. |
· They were less aware of research-proven recommendations of not disconnecting the catheter from its bag (59% nurses, 30% aides, p < .001), not routinely irrigating the catheter (48% nurses, 8% aides, p < .001), and hand hygiene after casual contact (60% nurses, 69% aides, p = .07). · HCWs were also unaware of recommendations aboutalcohol-based hand rub (27% nurses and 32% aides with correct responses, p = .38). · Significant discrepancies remain between research-proven recommendations pertaining to urinary catheter care and HCWs' knowledge. |
| Ana Montoya et al. (2013)/USA | Quantitative, survey method | N = 356 nurses and nurse aides | A self-administered anonymous questionnaire, based on national guidelines. Unspecified validity and reliability. | To evaluate the following: (1) whether NH health care workers (HCWs) are aware of their facility's HH and UC care policies and (2) whether awareness of facility policy pertaining to HH and UC leads to appropriate HH and UC care. |
· Overall, a majority of respondents (>93%) reported wearing gloves and practicing HH before and after manipulation of a UC. · Most of the respondents (94%) were aware of the HH policy at their facility. Furthermore, 85% of respondents were aware of an indwelling catheter policy, 82% of an intermittent catheterization policy. · Confusion about appropriate HH after casual patient contact persists, with approximately 40% of respondents answering incorrectly. · Confusion also persists about alcohol-based hand gel use as a method of appropriate HH, with less than 32% answering correctly. This reflects a relative delay in acceptance of alcohol hand rub in NHs. |
| Fernández-Ruiz et al. (2013/Spain | Quantitative, survey method | N = 55 physicians | A self-administered questionnaire, based on pilot. Unspecified validity and reliability. | Tested physicians' knowledge of the appropriate indications for UC and management of NUTI. |
· The median per centage of correct responses was 62.5%. · The questions for which the highest rates of correct responses were obtained the risk factors for UC-related NUTI (94.5%) and the appropriateness of UC for urine output monitoring in uncooperative patients (96.4%). · The questions for which the lowest per centage of correct answers were obtained the daily risk of NUTI in patients with UC (45.5%), the inappropriateness of UC for convenience of care in patients with impaired mobility (49.1%), and the therapeutic approach to UC-related NUTI (50.9%). · There was a physician order for UC in 47.8% of patient charts, whereas its indication was explicitly documented in only 41.3% of cases. Most attending physicians were aware that their patients had a catheter in place (95.7%), and knew the initial indication for UC (93.5%) and its duration (82.6%); Twelve of them (26.1%) were inappropriately catheterized. |
| Shuko Maeda et al. (2013)/Japan | Quantitative, survey method | N = 30, nurses |
A questionnaire based on books and guidelines. Items was confirmed in a pretest conducted by four nurses. Unspecified validity and reliability. |
Assess the status of long-term indwelling urinary catheter users' management. |
· A high per centage of visiting nurses implemented all the items of observation, practice, guidance and cooperation in catheter management. · Experience of difficulty was most frequent for catheter insertion (51·7%), followed by obtaining catheter replacement supplies (42·3%) and bladder irrigation (31·6%). · The frequency of cooperation was highest with physicians (100%), followed by care managers (82·1%), day care service personnel (73·7%). · Difficulty was experienced by visiting nurses when cooperating with physicians (40%), visiting home care personnel (25%), day care service personnel (14·3%). |
| Mohamad G.Fakih et al. (2013)/American |
Quantitative, intervention: a nurse-driven intervention to remove unnecessary urinary catheters; establishing institution-based guidelines for urinary catheter placement in ED physician education. Survey method. |
N = 257, bedside nurses, case managers, and nurse managers |
An anonymous questionnaire. Unspecified validity and reliability. | Assess the perception of bedside nurses about who they consider responsible for evaluation of urinary catheter er necessity in non-ICUs. |
· Of bedside nurses responding to the questionnaire, 222 of 227 (97.8%) identified themselves as responsible or as sharing the responsibility for catheter necessity evaluation. · 223 of 229 (97.4%) were confident in their knowledge, and 166 of 222 (74.8%) viewed physicians as receptive to their requests for catheter removal >70% of the time. |
| Brian T Conner, (2013)/USA | Mix methods, survey method and focus groups |
Survey: N = 36 Focus groups:N = 11 |
The EBP Questionnaire (EBPQ), the Cronbach α was 0.87 and internal reliability for the subscales ranged from 0.79 to 0.91. The Adoption of the Early Catheter Discontinuation Protocol Questionnaire (AECDPQ), the Cronbach α ranging from 0.89 to 0.71. |
|
Quantitative study: · The results of the EBPQ responses indicate that having the opportunity to learn about and implement the nurse-driven protocol was a factor in the intervention group nurses' perceptions of their practice and attitudes related to EBP. · The preintervention mean scores for the total EBPQ and the 3 subscales were moderate. Qualitative study: · The overarching theme to emerge from the focus group responses was that the nurses enthusiastically supported the nurse-driven protocol intervention. · They agreed that the intervention was better than the routine procedure of waiting physician order or reminding them. · The participants agreed that the early catheter discontinuation protocol was advantageous for the patients and hospital. · The nurses placed high value on having the opportunity to learn about EBP and CAUTI. But several participants stated that they were unaware of the risks associated with catheter duration. · The majority of participants from both focus groups agreed that the nurse-driven protocol fit well with their ideas of nursing practice and was appropriate. |
| MARK LISTER F. Opina & Oducado, 2014/Philippines | Quantitative, survey method | N = 30 nurses | A researcher-made questionnaire. Unspecified validity and reliability. | To determine the knowledge and practices of nurses on infection control in the use of urethral catheters in a private hospital in Iloilo City. |
· In general, respondents had a very poor knowledge on infection control in the use of urethral catheters. The respondents were least knowledgeable about the different approaches to catheterization and specimen collecting methods followed by proper urethral catheter maintenance and lastly, on considerations and techniques for catheter insertion. · 70 per cent had low level of knowledge. 30 per cent of the nurses have average level of knowledge on infection control, there is still a huge number of nurses who are not aware about infection control on CAUTI prevention. · 66.7 per cent of the respondents had poor practices on infection control. 33.3 per cent of the nurses had good practices, there is still a huge number of nurses prone to making mistakes. · 77.8 per cent who had an average level of knowledge on infection control had poor infection control practices. 61.9 per cent of the respondents who had low level of knowledge had poor infection control practices. It can be seen that 66.7 per cent of all insertions were poorly performed. |
| Mary R.Mulcare et al. (2015)/American | Qualitative, focus groups | N = 38 ED physicians, midlevel providers, nurses | Semi-structured interview outline. | To describe ED providers' knowledge, attitudes, and practice patterns related to use of IUCs in older adult patients in ED settings. |
· Participants reported believing that IUCs are overutilized in ED settings, confirming that IUCs are infrequently removed once placed and often inserted for staff convenience. · Participants reported that current clinical decision-making about IUC placement varies widely. |
| Kartik Viswanathan et al. (2015)/American | Quantitative, survey method |
N = 129 Emergency nurses, attending physicians, mid-levels (nurse practitioners [NPs] and physician assistants [PAs]), and resident physicians. |
A self-administered questionnaire based on previously published instruments, literature review and experts' discussion. Items was confirmed in a pilot. Unspecified validity and reliability. |
To describe the knowledge, attitudes and practices of ED providers aboutplacement and management of IUCs. |
· Self-reported practices amongst participants surrounding IUC placement in specific clinical scenarios aligned with current standards of care and best practices in 40% of cases for nurses and 37% of cases for providers. · Practice varied widely between individual providers. · Their reported practice patterns showed inconsistencies with established guidelines. |
| Manisha et al. (2015)/Indian | Quantitative, survey method | N = 154, 49 doctors and 105 nurses. | A structured questionnaire based on guidelines. Unspecified validity and reliability. | Assess the knowledge of indication for catheterization and measures to prevent CAUTI. |
· Only 57% of the respondents could identify all the measures for prevention of CAUTI. · The knowledge aboutthe indication for catheterization though suboptimal was significantly better amongst the doctors as compared to nurses. |
| Yildiz Kose et al. (2016)/Turky | Quantitative, survey method | N = 382 nurses | A questionnaire. Unspecified validity and reliability. | To evaluate the level of knowledge of the nurses about the use of a urinary catheter to prevent urinary tract infections. |
· The level of knowledge of the nurses concerning the intervention during the catheter insertion, to prevent the urinary tract infections was adequate. · The nurses could not get enough scores from the questions of daily catheter and perineal care. · The nurses had inadequate scores about the emptying of the bag before transfer, the weekly changing of the drainage bag, not to separate it from the system whilst emptying it. · The nurses had insufficient information concerning the maintenance of the closed drainage system in catheter insertion, irrigation if the catheter is clogged, keeping the catheter below the level of bladder, maintenance of the closed system during taking cultures, with their mean scores below 4. |
| Karen Jones et al. (2016)/USA | Quantitative, survey method |
N = 394 nurses |
A 40-question questionnaire. Unspecified validity and reliability. |
Assessment of the nurse's education and knowledge related to how to properly obtain urine cultures and identify CAUTI in catheterized patients. |
· Of all respondents, 15.7% rated their knowledge on CAUTI identification as excellent, 38.1% rated their knowledge as above average, 43.1% rated their knowledge as average, and 3.0% rated their knowledge as below average. · Although 327 of 394 (83%) of all nurses surveyed reported that they never collect urine samples by draining directly from the drainage bag, only 58.4% reported to be fully compliant with that standard (230/394; p < .001). · The mean score for nurses was 4.78 ± 1.75 (out of 12 points). |
| Shah et al. (2017)/Pakistan |
Quantitative, survey method |
N = 70 nurses | A self-developed questionnaire. Unspecified validity and reliability. | To identify knowledge and practices of nurses aboutCAUTI control. |
· The mean knowledge of participants was 66%. the Mean practice was 56.43%. · The result was alarming to know that the nurses had low knowledge and poor practices about infection control in the use of urethral catheter. |
|
Brenda Shaver et al. (2018)/USA |
Quantitative, Intervention: Conducting a CAUTI education program: Foley Product Training and Simulation train-the-trainer sessions. Survey method |
N = 48 nurses | Survey questions. Unspecified validity and reliability. | Evaluating nursing knowledge and attitudes towards Foley catheter insertion and maintenance. |
· The mean postsurvey score was significantly higher (86.9 ± 8.3%) than the presurvey score (76.0 ± 12.3%) for the knowledge section of the survey. · There was no marked difference in participant attitude following the educational training, with mean presurvey and postsurvey scores of 91.3 ± 7.0% and 89.8 ± 5.3%, respectively. · After the course, participants were more confident in their clinical knowledge; however, perception aboutCAUTI prevention did not improve. |
| Kulbay & Tammelin, 2018/Sweden | Quantitative, survey method |
N = 518 nurses and assistant nurses |
A structured questionnaire. Based on pilot test. Unspecified validity and reliability. | To investigate nurses and assistant nurses' opinion and practice of urinary catheterization. |
· Amongst all nurses and all assistant nurses, 20.6% (64/311) and 41.4% (75/181) respectively said that they used a sterile technique when inserting a urinary catheter; Of all the nurses, 81.4% (253/311) said that the urinary catheter should be sterile when inserted. The corresponding figure for assistant nurses was 82.9% (150/181). · In all 287/492 (58.3%) persons said that they followed the hospital guideline. |
| MC Cutinho et al. (2018)/Indian | Quantitative, survey method |
N = 108 staff nurses |
A structured knowledge questionnaire. Unspecified validity and reliability. | Aimed at assessing the knowledge on practice of urinary catheter care and compliance to urinary catheter care guidelines by the nurses working at a tertiary care hospital. |
· 89(82.4%) had average knowledge and only 1(0.9%) had poor knowledge on practice of urinary catheter care. · Majority (82.4%) of the staff nurses had adequate knowledge but there was noncompliance to procedural steps of urinary catheter insertion, urine specimen collection, maintenance of urinary catheter. |
| Monina Hernandez et al. (2019)/New Zealand |
Quantitative, Intervention: a CAUTI education package on nurses' knowledge and indwelling catheter management practice Survey method |
N = 50 nurses |
A self-administered Daily Urinary Catheter Maintenance Checklist based on CDC evidence-based guidelines. Unspecified validity and reliability. |
Investigated the impact of a CAUTI education package on nurses' knowledge and indwelling catheter management practices. |
· Of the 175 checklists, only 101 (58%) indicated that hand hygiene had been performed by the nurses; 31% (n = 54) showed that all evidence-based practices in the bundle of care were performed and documented by the nurses. Only half of the number of checklists given evidence of hand hygiene performance during catheter management. · Nurses ensured that the catheter bag was below the bladder and off the floor at all times, there was no kinking of the catheter tubing, the collecting bag was emptied regularly, a closed-drainage system was maintained at all times. · The checklists indicated that nurses assessed the need for catheter removal and that standard precautions were used. Documentation showed that 157 out of 175 (90%) indwelling catheters were removed. Of these, 144 (82%) had the appropriate date of removal and nurse's signature. On examination, all 144 patients had their catheters removed in 24 hours of surgery. · Nurses' performance of the catheter insertion component shows that sterile equipment was used, sterile technique was observed. · The findings highlighted poor documentation of nursing care (non-adherence to documentation standards). |
| Tenzin Dawa et al. (2019)/USA | Quantitative, survey method | N = 64 rehabilitation nurses | 37 Likert-like survey questions based on literature review. Cronbach's alpha was 0.752–0.891. | To develop and examine the reliability of a survey to assess knowledge, attitudes, and behaviours (KAB) of rehabilitation nurses for preventing urinary tract infections in persons requiring intermittent catheterization. |
· The nurses scored a mean of 6.86 (SD = 0.2081) on attitude, 6.68 (SD = 0.2087) on knowledge, and 7.04 (SD = 0.2813) on behaviour. Nurses reported adequate knowledge and training. · The lowest ratings (0–5) were with the knowledge questions (Items 14,17, and 18) specific to the frequency and helpfulness of the Elsevier Clinical Skills standard and the adequacy of training on the online system, the attitude question (Item 5) about searching for evidence, and the behaviour questions about the use of dexterity · Twenty-eight per cent incorrectly identified the root cause of urinary tract infection, and 45% reported that other nurses always washed their hands. |
| Salha Salem Algarni et al. (2019)/Saudi Arabia Kingdom | Quantitative, survey method | N = 137 nurses | Knowledge and Practices Questionnaire based on experts' review. Cronbach's alpha value was 0.841. | To assess the level of nurses' knowledge and practices towards prevention of CAUTI. |
· More than half of nurses (62.77%) had low a level of knowledge. Whilst about one-third (36.50%) of nurses had average level of knowledge, and only 0.73% of nurses had high level of knowledge. Aboutthe levels of nurses' practices towards CAUTI prevention, 83.94% had a poor level of practices. Whilst 16.06% of nurses had a good level of practices. · More than half (56.9%) of nurses did not know that using alcohol hand sanitizer is comparable to hand washing in preventing CAUTI incidence. 56.9% did not know that routine use of antiseptic lubricants to decrease the risk of infection is not necessary for urinary catheter insertion. · More than half (55.7%) of nurses responds correctly to overall practices towards prevention of CAUTI. More than half of nurses (54.7%) had a good practice due to used sterile gloves when inserting a catheter, but a little more than one-third of nurses (45.3%) were not. · More than three quarters (75.9%) of nurses had good practices on implementing quality improvement strategies to reduce CAUTI. |
| Andrea Niederhauser et al. (2019)/Switzerland | Quantitative, survey method |
N = 1,579 medical staff members |
A 55-item standardized questionnaire based on previous survey research and literature review. Items were pretested on 42 physicians and nurses. Unspecified validity and reliability. | To evaluate changes in staff perspectives (KAP) towards indwelling urinary catheter (IUC) use after implementation of a 1-year quality improvement project. |
· The average number of answers to questions in nurses' knowledge score was 10.2, which was less than that in doctors (11.1). The average score of attitudes is higher than that of doctors (5.4 & 5.1). · Nurses mainly felt responsible for placing, maintaining and removing an IUC. Physicians perceived themselves to be mainly responsible for ordering catheter placement and removal at both time points. |
| Sonali D. Advani et al. (2019)/American | Quantitative, survey method | N = 604, 405 physicians and nurses from tertiary medical centre, 199 from community medical centres. | A modified previously validated 13-questions survey based on guidelines. | Assessment of CAUTI practice pattern and knowledge of urine culture. |
· Mean scores amongst physicians were higher than amongst nurses (7.77 vs 6.50; p < .05) · Our data reveal specific knowledge gaps amongst physicians and nurses related to ordering urine cultures in catheterized patients. · The majority of physicians and nurses in our health care system were unable to accurately identify indications for ordering urine cultures in catheterized patients. |
| Sanniya Khan Ghauri et al. (2019)/Pakistan | Quantitative, survey method |
N = 485 doctors and nurses |
An interviewer-administered questionnaire which was validated by two epidemiologists. Unspecified validity and reliability. |
To assess their knowledge of indications for urinary catheterization, measures to be taken to prevent CAUTI, and attitude abouturinary catheterization. |
· Overall, the knowledge of doctors was better than the nurses. · The nurses knew more about CAUTI preventive measures than the doctors. · There was reasonable knowledge and attitude amongst nurses and doctors. |
| Kelly Thomas (2020)/UK | Quantitative, survey method | N = 16 nurses | A 11-questions questionnaire. Unspecified validity and reliability. | Exploring primary and community care nurses' knowledge of catheter maintenance solutions. |
· Community nursing staff had variable degrees of knowledge of catheter maintenance solutions. · Of the 16 participants, only four had previous training on the use of catheter maintenance solutions, but all 16 participants felt that an update would benefit their future practice. · The question that produced the most varying responses concerned whose responsibility it was to review the use of the solutions. · There is a need for change in primary and community care aboutcatheter maintenance solutions, as they indicated a lack of knowledge on catheter maintenance solutions amongst staff nurses working in the community. |
| Anns M. Benny et al. (2020)/Indian | Quantitative, survey method | N = 235 staff nurses |
A 17-questionsstructured knowledge questionnaire which was validated by seven experts. The internal consistency was 0.76. |
Knowledge assessment |
· Majority of nurses 190 (80.85%) had average knowledge whereas, 28 (11.2%) had low knowledge, and few 17 (7.23%) nurses had high knowledge aboutCAUTI. · It was found that nurses' overall knowledge on prevention of CAUTI was average, with mean per centage knowledge score of 73.47%. |
| Andrea Niederhauser et al. (2020)/Switzerland | Quantitative, survey method |
N = 1,579 nurses and physicians |
A structured questionnaire based on literature review which pretested on 43 physicians and nurses. Unspecified validity and reliability. |
To determine variation in the perceptions of the current practices and culture aboutIUC use between nurses and physicians. |
· Most of the nurses felt responsible for placing, maintaining, and removing an IUC, whereas physicians perceived themselves to be responsible mainly for prescribing catheter placement and removal. There is a substantial overlap between the two professional groups in terms of who considers themselves responsible for each of the tasks. · Nurses given significantly higher mean ratings and had a more positive view about perception of current IUC practices and culture than physicians. |
| Balu et al. (2021)/Indian | Quantitative, survey method | N = 95 doctors, nurses and other allied health care professionals. | A validated structured questionnaire. | Knowledge, attitude and practice assessment |
· 28.4% (n = 27) of individuals had moderately adequate knowledge and 71.6% (n = 68) had adequate knowledge about CAUTI. Average mean knowledge of the study participants was 11.42 (SD = 1.534). · 4.2% (n = 4) had unfavourable attitude, 88.4% (n = 84) had moderately favourable attitude and 7.4% (n = 7) had favourable attitude towards CAUTI. · 4.2% (n = 4) of individuals had moderate practice, and 95.8% (n = 91) had adequate practice on prevention of CAUTI. |
| Ivy Mong BNSc et al. (2021)/Malaysia | Quantitative, survey method | N = 301 nurses |
A questionnaire based on literature review which validated by six experts. The content validity index was in (0.83–1.000), Cronbach's alpha was (0.83–0.85). |
Aimed to (i) assess nurses' current knowledge, attitude and practices concerning CAUTI prevention and (ii) identify the influences of knowledge and attitude on practice with CAUTI prevention in the Malaysian context. |
· Knowledge of CAUTI prevention was found to be good, as 69.1% (n = 208) of the nurses scored more than 80% in this domain with a mean score of 83.34 (SD = 7.19). · The mean score for attitude towards CAUTI prevention was 3.28 (SD = 0.33), and 80.1% (n = 241) of the nurses were found to have a positive attitude. · The mean score for perceived practice was 3.15 (SD = 0.30); 64.8% (n = 195) of the nurses were found to have good perceived practice of CAUTI prevention. · Knowledge was found to be positively correlated with attitude and perceived practice. |
3.6 Synthesis
Due to the difference between intervention measures and outcome indicators in included quantitative studies, there existed great clinical heterogeneity, so that we could not use meta-analysis to make quantitative evaluation. Therefore, we chose descriptive analysis methods to make quantitative analysis and used a results-based mixed-methods synthesis design – thematic analysis to make quantitative and qualitative study's data synthesis (Noyes et al., 2019). Steps are as follows: (i) thematic analysis of qualitative studies, (ii) thematic analysis of quantitative studies and (iii) assimilated analysis and synthesis of findings from both methods of studies. Detailed stages of thematic synthesis referred to other studies (Thomas & Harden, 2008): (1) the line-by-line coding of study's findings (using NVivo 11), (2) the classification and organization of these free codes into corresponding field to obtain descriptive themes and (3) the development of analytical themes.
3.7 Ethical considerations
There was no requirement for this review of Research Ethics Committee approval.
4 RESULTS
4.1 Study characteristics
Of the 34 included studies, most of them were quantitative studies (30 of 34), three were qualitative studies, only one was mixed-methods study. Of the 30 quantitative studies, 26 were descriptive studies, four described interventions. A total of 23 studies were only focussed on nurses, two were only focussed on doctors and the rest (n = 9) were focussed on all healthcare workers included doctors, nurses, nurse aides, case managers and other allied healthcare workers. Four quantitative studies that described interventions were focussed on CAUTI prevention educational program of nurses or nurse-driven multidisciplinary effort for early urinary catheter removal to promote nurse's knowledge, practices of CAUTI and to decrease rate of CAUTI. A total of 26 descriptive studies were mainly focussed on identifying healthcare worker's knowledge, attitude and practice level of CAUTI.
4.2 Methodological quality
The assessment of methodological quality of included studies was based on the Mixed Methods Appraisal Tool (Table 2). The complete quality assessment can be found in Appendix S3. All qualitative and mixed-method studies were high methodological quality. For three qualitative studies' data collection, two studies used unstructured interview and semi-structured interview, respectively, the rest used focus group. For four quantitative non-randomized studies, three of them did not clarify the confounders in the study design and analysis, even did not test their instruments as well. Of 26 quantitative descriptive studies, only 11 of them were high methodological quality, 12 studies did not explain whether their research tool have been tested or pretested or not and were unaware of their validity and reliability, seven studies did not give a clear justification of the sample frame, 15 studies did not explain why certain eligible individuals did not participate in the research.
4.3 Synthesis
We used a results-based mixed-methods synthesis design – thematic analysis to make qualitative and quantitative study's data synthesis. By means of thematic analysis of qualitative and quantitative studies, we obtained three descriptive themes. The barriers and facilitators of HCWs' prevention and management of CAUTI were summarized by assimilated analysis and synthesis of findings from both methods of studies.
4.3.1 Qualitative and quantitative synthesis
Unbalanced varied knowledge level of CAUTI
There was an imbalance in knowledge of healthcare workers amongst CAUTI's prevention. It was demonstrated that HCWs have adequate or average knowledge about CAUTI's common risk factors and prevention measures. For instance, in a survey conducted by Balu et al. (2021) (N = 95), 94.7% of the healthcare professionals identified high-risk groups of CAUTI include female gender and elderly population (Balu et al., 2021). In several descriptive studies (Ghauri et al., 2019; Ivy et al., 2021; Kulbay & Tammelin, 2018; Shaver et al., 2018), more than 90% of HCWs knew that common preventive measures for CAUTI, such as urinary catheters should be inserted only by personnel who are proficient in technique of aseptic insertion and should be inserted only when necessary and removed as soon as possible, hand washing should be done instantly before and after any manipulation of catheter site or apparatus.
However, there were also some weak parts of HCW's knowledge on catheter's indication and latest guidelines. A survey conducted by Ivy Mong BNSc et al. (2021) (N = 301) (Ivy et al., 2021) found that nearly one-third of nurses thought that urinary catheter is indicated for urine output monitoring in a mobile patient, only 26.1% of the nurses knew that nursing care of incontinent patients is not indication for placing catheter. A majority of nurses described that they gained information about CAUTI's prevention from their previous education but not from the hospital's organizational learning of latest guidelines. A cross-sectional study conducted by Shah et al., (2017) (N = 70), only 48.6% nurses knew standard guidelines. A study that surveyed 108 staff nurses, only 14(13%) expressed their awareness of evidence-based guidelines of CAUTI (Cutinho et al., 2018). Manisha et al. (2015) (N = 154) (Manisha et al., 2015) also found that more than half of the doctors did not know that some important indications such as patients with receiving large volume infusions or diuretics during surgery or with urethral stricture was both needed to place urinary catheter. In addition, some studies (Manisha et al., 2015; Montoya et al., 2013; Algarni et al., 2019; Opina & Oducado, 2014) reported that quite a few HCWs were not aware that guideline suggestion for using alcohol hand sanitizer has the same effect as hand washing. A considerable number of HCWs did not know that latest guideline indicated that meatal care with antiseptic solution was not suggested to preventing CAUTI (Balu et al., 2021). And the same problem was pointed out in another study (Opina & Oducado, 2014). Meanwhile, some doctors and nurses could not distinguish effective and ineffective measures of CAUTI. They expressed uncertainty or greater of it to included preventive measures, such as antimicrobial-coated catheters, antimicrobial drainage bag additives, bladder irrigation or twice daily meatal care (Manisha et al., 2015; Mody et al., 2010; Dimitri et al., 2010). Another study conducted by Sonali D. Advani et al. (2019) (N = 199) showed that the majority of physicians and nurses could not accurately identify indications for urine culture, especially those worked in community hospital were more likely to choose inappropriate indications and their mean knowledge scores were lower than those worked in tertiary care centre (Sonali et al., 2019). Besides, some studies reported that the doctors had better knowledge than the nurses (Sonali et al., 2019; Manisha et al., 2015; Ghauri et al., 2019).
Generally positive attitudes towards CAUTI prevention
Although a few HCWs still considered CAUTI is impossible to prevent, it could not be denied that the vast majority of the HCWs gave weight to CAUTI's prevention and control (Weerakoon & Lawrentschuk, 2010). In a survey conducted by Manisha et al. (2015) (N = 154), more than 88% of doctors and nurses believed that though CAUTI was a common problem, it was still possible to prevent it (Manisha et al., 2015). A qualitative study conducted by Mary et al. (2015) that interviewed 38 healthcare workers, all of them showed strongly willingness to apply a clinical protocol to guide and standardize their operating procedures of indwelling urinary catheter practice to better prevent retrograde urinary infection. Some nurses showed a willingness to apply nurse-driven program to remove foley catheters and they wanted to be more involved in urinary catheter decision-making process (Conner, 2013; Viswanathan et al., 2015). In addition, the healthcare workers also attached importance to any chance of learning about evidence-based practice (EBP) of CAUTI and felt enjoyable in learning process and became more confident to making changes in practice when they deeply understood EBP knowledge, so that they could standardize their practice and improve their care quality for patients with indwelling urinary catheters (Conner, 2013).
Some studies showed that nurses have more positive attitudes than doctors towards the prevention and control of CAUTI. In a qualitative study conducted by Mary R.Mulcare et al. (2015), all eight nurses amongst 38 healthcare workers that include attending physicians, residents and physician assistants expressed their desire for seeking catheter alternatives and hoped that a clinical protocol could bring cultural change so that CAUTI rates could be effectively controlled. In addition, a qualitative study (Jane, 1997) interviewed 12 registered nurses showed that they were willing to nursing students come to the wards, so that to promote the development of ongoing education, urging nurses to abide by professional principles such as aseptic technology.
However, some studies showed that several nurses also expressed their frustration and powerlessness of CAUTI's management. A qualitative study conducted by Mary R.Mulcare et al. (2015) found that nurses felt depressed that their opinion on patient care were not included in decision-making process of urinary catheters' practice. Another qualitative study conducted by Jane et al (Jane, 1997) found that there was a disharmony amongst the 12 nurses they interviewed. The junior and senior nurses questioned and satirized each other. It jeopardized legal and ethical duties that were given in United Kingdom Central Council's Code of Professional Conduct (1992b) and made junior nurses felt helpless about not being able to correct non-standard urinary care practice of senior nurses. Besides, in this study, nurses expressed their powerless that sometimes doctors seem to feel stroppy about them for removing catheters by their own, although they have done it as soon as possible. This phenomenon has always existed. In addition, they described that the nurse–patient relationship has changed into ‘nurse-client’ mode. In this mode, clients are always right. For instance, after they suggested the alternatives of urinary catheter, patients still required for indwelling urinary catheter. So that they could only make recommendation for patients cautiously rather than patients cooperate with them to accomplish the treatment tasks. As a result, made it difficult for nurses to carry out their work smoothly and to fully play patient advocates role. The above phenomenon showed that the disharmony relationship between doctor-nurse–patient have caused negative effects on nurses' attitudes towards CAUTI's prevention and management.
Undesirable practices on CAUTI's prevention and management
There was a problem that the HCW's practice did not always conform to the CAUTI guidelines, such as (i) hand hygiene, Of the 175 checklists, only 38 had partially completed performance of evidence-based practices of the hand hygiene (Hernandez et al., 2019). Of 108 staff nurses, 40% of them did not wash hand before catheter insertion (Cutinho et al., 2018) and it was indicated in other study as well (Opina & Oducado, 2014), (ii) inappropriate use of urinary catheter, amongst 129 self-reported practices of HCPs, only 40% of nurses and 37% of other staffs had met current normal practices of urinary catheter placement (Viswanathan et al., 2015). Out of 380 cases, only 41.3% of cases documented explicitly urinary catheter's indication in patient chart and 26.1% of cases had inappropriate indication for urinary catheters (Fernández-Ruiz et al., 2013), (iii) non-standard sterile technique during urinary catheter insertion, amongst 311 nurses and 181 assistant nurses, only 20.6% and 41.4% of them used sterile technique when inserting urinary catheter (Kulbay & Tammelin, 2018). Amongst 137 nurses, more than 45.3% of nurses did not use sterile gloves when inserting a catheter (Algarni et al., 2019). (iv) non-standard nursing documentation (Hernandez et al., 2019). In some studies, the medical staff also expressed that many important standard measures were not applied in their practice and when they had a question, they usually asked the senior nurses, rather than searched or used evidence-based measures. (Andrea et al. 2020; Dawa et al., 2019; Hernandez et al., 2019).
However, the HCWs also had relatively adequate practice on routine urinary catheter care. The most common practices followed by healthcare staff were (i) fixation of urinary catheter (Balu et al., 2021; Ivy et al., 2021; Siegel, 2006), (ii) maintenance of foley drainage bags were below the level of the bladder (Cutinho et al., 2018; Hernandez et al., 2019; Ndomba et al., 2008; Opina & Oducado, 2014), (iii) avoidance of urinary catheter's kinking or twisting (Algarni et al., 2019; Hernandez et al., 2019; Opina & Oducado, 2014) and (iv) observation of urine volume and characteristics of urine (Algarni et al., 2019; Maeda et al., 2013).
4.3.2 Assimilated synthesis
After all qualitative and quantitative studies reviewed, the barriers and facilitators of HCWs' prevention and management of CAUTI were summarized. The barriers were heavy workload, understaffing, lack of knowledge and supervision, nurses' poor documentation, etc. The facilitators were leadership's effects, better education, teamwork, information technology support, advocacy for nurse-driven protocol, etc. (See Table 4).
| Barriers | Facilitators |
|---|---|
| Heavy workload (Ivy et al., 2021) | Leadership (Andrea Niederhauser et al. 2020; Andrea et al., 2019; Fakih et al., 2013) |
| Understaffing (Jane, 1997) | Positive attitude (Dawa et al., 2019; Ivy et al., 2021; Andrea et al., 2019) |
| Lack of supervision (Jane, 1997) | Betterr education (Anns et al., 2020; Manisha et al., 2015; Ndomba et al., 2008; Kelly, 2020; Niederhauser et al., 2019; Drekonja et al., 2009; Viswanathan et al., 2015; Dawa et al., 2019; Shaver et al., 2018; Hernandez et al., 2019) |
| Lack of attention to guidelines (Andrea Niederhauser et al. 2020;Ivy et al., 2021) | Teamwork (Andrea Niederhauser et al. 2020; Andrea et al., 2019; Viswanathan et al., 2015; Dawa et al., 2019; Shaver et al., 2018; Hernandez et al., 2019; Mary et al., 2015) |
| Lack of knowledge (Kose et al., 2016; Opina & Oducado, 2014; Shah et al., 2017) | Technique training and information technology support (Balu et al., 2021; Ivy et al., 2021; Mary et al., 2015; Shaver et al., 2018) |
| Physician variability in IUC practice by diagnosis (Mary et al., 2015) | Advocacy for nurse-driven protocol (Andrea Niederhauser et al. 2020; Conner, 2013) |
| Nursing variability in IUC placement technique (Mary et al., 2015) | Use of IUC removal reminder (Balu et al., 2021; Manisha et al., 2015; Dimitri et al., 2010; Ghauri et al., 2019; Drekonja et al., 2010; Algarni et al., 2019; Conner, 2013) |
| Nurses' poor documentation (Hernandez et al., 2019; Mary et al., 2015; Viswanathan et al., 2015) | |
| Nurses' time and patients' schedules (Dawa et al., 2019) | |
| Poor relationship (Jane, 1997; Mary et al., 2015) |
5 DISCUSSION
The discussions include results of synthesis, methodological quality and limitation. Discussions of assimilated synthesis will be included in each section of discussion rather than be described independently.
5.1 Synthesis
5.1.1 Unbalanced varied knowledge level of CAUTI
The healthcare workers had average or even adequate knowledge about CAUTI's common risk factors and prevention measures. This may be related to most of them have received ongoing medical or nursing education for basic about theoretical knowledge (Anns et al., 2020). However, their knowledge of indwelling urinary catheter indications and latest guidelines were inaccurate and incomplete. The main reason for it, is still education. The hospital normally organizes healthcare workers to learn basic knowledge of CAUTI's prevention, such as risk factors for CAUTI and it conventional prevention measures, but ignored some important indwelling catheter indication and latest guidelines of routine catheter care which were medical staffs mostly need to learn and to improve. Education as the main promotive tool can be tailored to address gaps in knowledge and standardize practices of HCWs (Anns et al., 2020; Shaver et al., 2018).
Amongst healthcare workers, doctors' knowledge of CAUTI's prevention and control better than the nurses on the whole (Sonali et al., 2019; Manisha et al., 2015; Ghauri et al., 2019), because in some countries and areas, the academic requirement of doctors is higher than the nurses. Those HCWs worked in community hospital were more likely to choose inappropriate indications. Their mean knowledge scores were lower than those worked in tertiary care centre (Sonali et al., 2019). This may be related to different characteristic of two types of institution. The tertiary care centres are general medical institutions, and they usually decide whether to keep an indwelling urinary catheter according to patients' symptom. But community hospitals are mainly responsible for community healthcare work or transitional care work, received patients who need urinary catheter care. No matter what types of institution that healthcare workers come from, there is a need for the institutions to give periodic course of latest evidence-based guidelines according to HCWS' needs and times. Specifically, for the doctors, the emphasis of education should be put on indications for indwelling urinary catheters to improve their catheterization prescribing practices and to reduce unnecessary insertion of urinary catheters (Fernández-Ruiz et al., 2013). And it is equally important to educate nurses about the indications of catheter placement since they can timely remind doctors to remove catheters as soon as possible. For nurses, the education weight should be given to hand hygiene and basic care of IUC, because nurses interact closely with patients and spend more time in catheter care by the bed than do doctors, so that they bear more responsibility for the details of infection prevention and management. Above all, HCWs should be educated for evidence-based searching methods for getting evidence, since their practices should not be guided by habit and experience.
5.1.2 Generally positive attitudes towards CAUTI prevention
The healthcare workers generally had positive attitudes towards CAUTI prevention. They showed strongly willingness to learn evidence-based standard protocol and to apply it to correct their daily practice. But the nurse staffs expressed their frustration and powerlessness due to one of the toughest barriers for efficient infection prevention that was disharmony in doctor-nurse–patient relationship.
For doctor-nurse discordant relationship, before starting infection prevention work, they should have a common understanding of CAUTI objectives that they would like to pursue, then reaching an agreement about their respective roles and responsibilities, establishing mutual trust and efficient cooperative relations between each other (Andrea et al. 2020). For nurse–patient tense relationship, nurses should be equipped with solid theoretical knowledge and professional practical ability to convince the patients, using it to solve patients' problem. Meanwhile, doctors act as regulators, need to communicate with patients for cooperating with nurses' care. It is equally important to educate patient and their caregivers to respect and coordinate with healthcare workers. Besides, nursing leadership should focus on striving for more empowerment chances for nurses, motivating nurses' enthusiasm and confidence. Then, gradually establish a doctor-nurse–patient relationship of mutual trust, develop and consolidate a collaborative nature, lay the foundation for efficient infection prevention work.
5.1.3 Undesirable practices on CAUTI's prevention and management
The healthcare workers' practices on CAUTI's prevention and management were undesirable in general. They had relatively adequate practice on routine urinary catheter care, since those were about basic knowledge. However, they failed to fully conform to the CAUTI guidelines, such as hand hygiene, use of urinary catheters, compliance of aseptic technique, standard documentation. Standard documentation might be one of the easiest parts to be ignored. It includes indications for catheter insertion, date and time of catheter insertion, individual who inserted catheter, and catheter removal's date and time, etc. which are parts of quality improvement program of CAUTI's prevention guideline (Gould et al., 2017). It is a nurses' legal responsibility and a valuable resource of information which gives evidence for nursing care process, facilitates audits for nursing care and communication between medical staffs. The poor quality of documentations may cause interdisciplinary team which includes epidemiologists, infection control experts, nursing leadership, etc. fail to recognize patients' indwelling urinary catheter, consequently, make the delay of early removal of IUC, increase the risk of CAUTI (Viswanathan et al., 2015). Therefore, it cannot be ignored that promote the nurses' practices of standard documentation.
Above undesirable practices could be attributed into healthcare workers' poor knowledge of it. But other factors cannot be ignored, such as understaffing and lack of supervision. When undermanned situation exists, there was no time and energy for healthcare workers to strictly follow every step of guidelines. And even having sufficient medical personnel, it could not work efficiently without supervision of leadership.
It is a crucial point for clinical leaders to play a leading and supervisory role in prevention and management of CAUTI. In the context of CAUTI's management, clinical leaders should actively assume the main responsibility of education, training and supervision (Andrea et al., 2019). With the continuous updating of evidence-based guidelines, it is crucial for leadership to conduct targeted learning of CAUTI's knowledge regularly, to collect feedbacks of healthcare personnel, to carry out routine assessment and to strengthen supervision of their compliance of the latest clinical criteria. Besides, nursing leadership should popularize a new mode that combining electronic information technology with nurse-driven of urinary catheter's care and removal tool to improve nursing documentation quality.
5.2 Methodological quality
Overall, all qualitative and mixed-method studies had high methodological quality. But amongst the quantitative studies, the quality of non-randomized studies and descriptive studies were unsatisfactory. According to standards of MMAT, their common defect was participants representative of the target population, as many of them did not describe the reason for eligible individuals' absent and did not describe any attempts to achieve enough sample of target population. For non-randomized studies, another non-standard point was that they did not take the confounders into the design and analysis. Using some methods such as stratification, regression, matching, standardization and inverse probability weighting to control confounders is crucial to preventing confounding bias if there are confounders exist. For descriptive studies in our included research, a prominent point was the validity and reliability of their assessment instruments. Nearly half of descriptive studies that identified healthcare workers' KAP level of CAUTI ignored pretest or verify the validity and reliability of instruments. It directly caused poor psychometric quality of research instruments and inaccurate results. Thus, our review emphasizes that there is a need to construct a specialized, reliable instrument to evaluate healthcare workers KAP level of CAUTI. Researchers normally described the inclusion and exclusion standard of target population and sampling strategy, but ignored some indispensable details which affect paper's methodological quality. For instance, quite a few studies did not give a clear justification of the sample frame and did not explain the absent of certain eligible individuals in research. It can make paper more rigorous and convincing if added.
5.3 Limitations
There are several limitations of our study. Due to search conditions were partly limited to English language and published articles, it may have not retrieved all primary previously researches. Besides, since heterogeneity such as diversities in measuring tools, it was hard to make a meaningful data comparison between the knowledge, attitudes and practices statistical level of medical staff for CAUTI. In addition, to ensure as comprehensive as possible results, we did not exclude low methodological quality studies. Therefore, the validity of results in this review was affected by the methodological quality of included studies, which varied greatly.
6 CONCLUSION
As far as we know, this systematic review is the first attempt to explore knowledge, attitudes and practices level concerning catheter-associated urinary tract infection amongst healthcare workers. We also summarized several barriers and facilitators of CAUTI prevention. According to results and discussions, we drew the conclusion that healthcare workers' knowledge and practices of CAUTI's prevention and management need further optimization and their attitudes towards CAUTI prevention were generally positive. But the doctor-nurse–patient disharmony relationship had a negative effect on nurses' attitudes towards CAUTI's prevention. To improve above situation, future solutions should focus on strengthening education for latest guidelines, developing collaborative culture in doctor-nurse–patient relationship for infection prevention and motivating clinical leaders' initiative of education, supervision and more empowerment chances for nurses.
ACKNOWLEDGEMENTS
Thanks to all authors for their contributions to the design, methodological quality assessment, data extraction and synthesis of this study. Aoli and Weixi carried out screening articles, Baojie and Rui assessed methodological quality of included studies. Weixi and Jing carried out data extraction. All authors analysed and synthesized data. Aoli mainly drafted the article, Yu revised the article. All authors examined and approved final version of this review.
FUNDING INFORMATION
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
ETHICS STATEMENT
Not applicable.