Thoracic Electric Impedance Tomography Detects Lung Volume Changes in Amyotrophic Lateral Sclerosis
Funding: This work was supported by ALS Society of Saskatchewan.
ABSTRACT
Introduction/Aims
Spirometry is the conventional means to measure lung function in amyotrophic lateral sclerosis (ALS), but is dependent on patient effort and bulbar strength. We aimed to use electric impedance tomography (EIT), an emerging non-invasive imaging modality, to measure dynamic lung volume changes.
Methods
Twenty-one patients with ALS underwent sitting and supine spirometry for forced vital capacity (FVC), and sitting and supine EIT. There were 13 patients in the high FVC group (FVC ≥ 80% predicted) and 8 in the low FVC group (FVC < 80% predicted). Additional demographic and clinical data were collected from clinical records.
Results
Only the low FVC group had significant loss of lung volumes in the supine position (R 2 = 0.89 and p < 0.001). The supine volume loss measurement at 10 min correlated with sitting (r 2 = 0.47) and supine FVC (r 2 = 0.36), maximum inspiratory (r 2 = −0.44) and expiratory pressures (r 2 = 0.36) (MIP and MEP), and the ALS Functional Rating Scale-Revised (ALSFRS-R) dyspnea subscore (r 2 = 0.36).
Discussion
EIT is an emerging alternative to existing measures of lung function in ALS, but without need for patient effort or bulbar strength. Significant losses in lung volume are seen on supine compared to upright position in patients with respiratory dysfunction. Further study is needed to determine relationships to existing clinical measures.
1 Introduction
Regular respiratory monitoring is required in Amyotrophic Lateral Sclerosis and includes symptom review, sitting and/or supine spirometry with forced or slow vital capacity (FVC/SVC), peak cough flow (PCF), maximal inspiratory and expiratory pressures (MIP/MEP), sniff nasal pressures (SNIP), arterial or venous blood gases, overnight oximetry, and polysomnography [1]. Airway clearance strategies and non-invasive ventilation (NIV) have become standard of care, but the relationship of these maneuvers to alveolar recruitment in real time is unknown.
Electrical impedance tomography (EIT) is a commercially available, non-invasive imaging modality that tracks dynamic changes to regional lung volumes without ionizing radiation [2-8]. In recent animal [8], pediatric [2-4], and adult studies [5-7], EIT has been employed to evaluate the efficacy of recruitment maneuvers in critically ill patients with acute respiratory distress syndrome. In patients with neuromuscular disease (patients with ALS were excluded), EIT detected a sustained increase to ventilation to anterior lung regions following intermittent positive pressure breathing [9]. One small study of non-bulbar ALS patients and healthy volunteers found that EIT metrics correlated with FVC, and qualitative differences were found between the patients with ALS and healthy volunteers [10]. Small studies of patients with ALS have shown that there is moderate correlation between upright FVC and EIT metrics [11] with differences in EIT metrics between healthy controls and patient with ALS [12], and between EIT measures and supine SVC in eight participants [13]. Spirometry relies on upon patient effort and bulbar strength to generate an appropriate seal on the testing equipment; neither of which is required for EIT.
In this prospective cohort study, we hypothesized that the supine posture would cause lower lung volumes for those with low FVC (less than 80% predicted).
2 Methods
2.1 Patients
Persons with a diagnosis of ALS attending the multidisciplinary ALS clinic in Saskatchewan, Canada were consecutively invited to participate during their regularly scheduled visits. Inclusion criteria were a diagnosis of ALS, 18 years of age or older, capable of giving informed consent, and ability to provide reliable results with spirometry according to the opinion of a respiratory therapist (RT) and pulmonologist with experience and expertise in neuromuscular/ALS care. Informed consent was obtained from all participants. Demographic data was collected from the patient medical records and included age, weight, sex, site of onset, date of onset, months since onset, date of diagnosis, months since diagnosis, genetic testing (if performed), ALS Functional Rating Scale—Revised (ALSFRS-R) [14], King's Score [15], medications (riluzole, edaravone, sodium phenylbutyrate with tauroursodeoxycholic acid [PB-TUDCA]), support devices (feeding tubes, non-invasive ventilation, cough assist devices, and lung volume recruitment). Ethics approval was obtained from the Biomedical Research Ethics Board at the University of Saskatchewan.
2.2 Electrical Impedance Tomography
The appropriately sized elastic silicone belt was applied on the patients' thoraces while EIT calibration (Dräger Pulmovista 500, Drägerwerk AG and Co. KGaA, Lübeck, Germany) was conducted (Figure S1). For 5 min, baseline EIT was recorded in the sitting position, followed by a measurement of sitting FVC. The patients were then placed in a supine position, their FVC measurement repeated, and EIT further recorded for 10 min or until dyspnea was appreciated. At the conclusion, the patients were returned to a sitting position, and the EIT belt was removed.
2.3 Statistics
The primary variable was lung volume changes in the supine position over time. Patient characteristics were summarized using descriptive statistics. Differences of means and Chi squared statistics compared patients with low (< 80% predicted) and high baseline FVC (≥ 80% predicted) in terms of respiratory measurements and scores. A simple linear regression was calculated for lung volume changes based on time for these two groups. This was followed by calculating difference of means at every minute of measurement to determine potential step changes. Pearson's correlations were calculated between the lung volume changes at minute 10 and routine respiratory values or measurements. All analyzes were done using SPSS Statistics for Windows, version 24 (IBM, Armonk, NY). A p value < 0.05 was considered significant.
3 Results
Patient characteristics are summarized in Table 1. A total of 21 patients with ALS were enrolled in the study, with 13 patients in the high FVC group and 8 in the low FVC group. The two groups were similar in age, weight and sex, but had significant differences with the lower FVC group utilizing more frequent home NIV (50% vs. 8%; p = 0.03) and lung volume recruitment (50% vs. 0%; p < 0.001) support. There were also significant differences between the low and high FVC group (Table 2) with respect to ALSFRS-R respiratory subscore, dyspnea item, and MIP.
| Characteristic | FVC ≥ 80% predicted | FVC < 80% predicted |
|---|---|---|
| (n = 13) | (n = 8) | |
| Female, n (%) | 4 (31) | 2 (25) |
| Age, years a | 60.8 (14.3) | 58.1 (13.9) |
| Weight, kg a | 79.3 (28.2) | 80.1 (22.1) |
| Site of onset | ||
| Limb, n (%) | 11 (85) | 6 (75) |
| Bulbar, n (%) | 2 (15) | 2 (25) |
| Time since ALS onset, months a | 56.1 (94.9) | 39.5 (22.1) |
| Time since ALS diagnosis, months a | 13.8 (16.2) | 22.1 (23.9) |
| Positive genetic test, n (%) | 2 (15.4) | 1 (12.5) |
| King's Score b | 2 (1–3) | 3 (2.5–4) |
| ALSFRS-R 2 | 40 (33.5–45.5) | 27.5 (23–32.5) |
| Supportive measures | ||
|---|---|---|
| Medications, n (%) | ||
| Riluzole | 9 (69.2) | 8 (100) |
| Edaravone | 2 (1) | 0 |
| PB-TUDCA | 1 (7.7) | 2 (25.0) |
| Non-invasive respiratory support | ||
| CPAP, n (%) | 0 | 1 (12.5) |
| BiPAP, n (%) | 1 (7.7) | 3 (37.5) |
| Cough assist, n (%) | 1 (7.7) | 2 (25) |
| Lung volume recruitment, n (%) | 0 | 4 (50) |
| Tracheostomy | 0 | 0 |
| PEG Tube, n (%) | 1 (7.7) | 2 (25) |
- Abbreviations: ALSFRS-R—Amyotrophic Lateral Sclerosis Functional Rating Score—Revised; BiPAP—bilevel positive airway pressure; CPAP—continuous positive airway pressure; FVC—forced vital capacity; PB-TUDCA—sodium phenylbutyrate with tauroursodeoxycholic acid; PEG—percutaneous endoscopic gastrostomy.
- a Mean (standard deviation).
- b Median (interquartile range).
| Respiratory variables and measurements | FVC ≥ 80% | FVC < 80% | p |
|---|---|---|---|
| (n = 13) | (n = 8) | ||
| ALSFRS-R respiratory subscore a | 12 (8.5–12) | 8 (5–10) | 0.009 |
| Dyspnea item | 4 (3–4) | 1.5 (1–2) | 0.0002 |
| Orthopnea item | 4 (4–4) | 3.5 (1.5–4) | 0.16 |
| Respiratory insufficiency item | 4 (3.5–4) | 3 (2–4) | 0.13 |
| FVC, percentage predicted b | 98.1 (14.3) | 67.6 (10.0) | < 0.0001 |
| MIP, cm H2O b | −67.4 (23.7) | −46.4 (17.1) | 0.04 |
| MEP, cm H2O b | 71.5 (22.5) | 52.3 (19.5) | 0.06 |
| Peak cough flow, L/min b | 468 (221) | 390 (211) | 0.43 |
- Abbreviations: ALFRS-R—Revised amyotrophic lateral sclerosis functional rating scale; FVC—forced vital capacity; MEP—maximal expiratory pressure; MIP—maximal inspiratory pressure.
- a Median (interquartile range).
- b Mean (standard deviation).
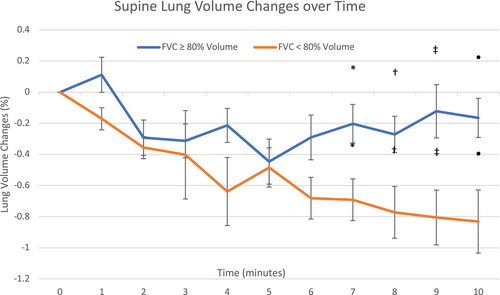
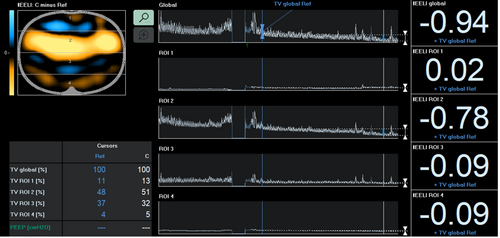
All patients tolerated 10 min of the supine EIT evaluation including those with low FVC, regardless of orthopnea subscore. The loss of lung volumes is depicted in Figure 1. A significant linear regression equation was only found in the low FVC group, with an R 2 = 0.89 and p < 0.001. A scatter plot and normal probably plot of residuals for regression of the standardized predicted value versus lung volume changes is depicted in Figures S2 and S3. There were also significant and progressive step losses of lung volume between the two groups at minute 7, 8, 9, and 10. The 10-min lung volume change had correlations with sitting FVC (r 2 = 0.46), supine FVC (r 2 = 0.36), ALSFRS score (r 2 = 0.56), ALSFRS-R dyspnea subscore (r 2 = 0.36), MIP (r 2 = −0.44) and MEP (r 2 = 0.32). Figure 2 depicts the EIT display of a patient with significant lung volume loss.
4 Discussion
Using EIT, the low FVC group (< 80% predicted) demonstrated significant and progressive loss of lung volumes during seven to 10 min of supine positioning compared to the high FVC group (80% or greater). The low FCV group's EIT volumes correlated with sitting and supine FVC, MIP, MEP, and the ALSFRS-R dyspnea item.
These data build upon what is already known from prior small studies; EIT metrics correlate with upright FVC with qualitative differences between patients with ALS and healthy volunteers [10-12]. A previous case series of 8 participants with ALS also demonstrated a correlation between supine FVC and supine EIT measurements at one time point [13]. In our study, lung volume parameters measured with continuous EIT demonstrated that this loss in volume occurred rapidly and progressively within 7 min.
We also evaluated correlations in EIT volumes with standard measurements of respiratory function beyond what is known from the literature for FVC/SVC in ALS. Since EIT lung volumes demonstrated correlations with many of the respiratory evaluations routinely conducted in ALS clinics for the low FVC group, future research may be beneficial to realize EIT's potential as an accurate and adjunct measure of respiratory function. Interestingly, there was a correlation between the EIT measures and the dyspnea item on ALSFRS-R, but not for the orthopnea item. This might be a consequence of a small sample size, and additional research is required to determine whether this is a consistent finding.
One patient in the high FVC group (84%) required NIV support for pre-existing sleep apnea. This same patient also exhibited the greatest loss of lung volume while supine compared to other participants. Additionally, four patients in the low FVC group were not prescribed home NIV. There is significant variability among clinics and health care providers as to the optimal time to initiate NIV. Accepted guidelines [1] suggest that using FVC alone is insufficient for decisions about NIV use, and other measures, such as supine FVC should be incorporated as needed. Volume loss on supine EIT could be considered as an alternative to supine FVC. Respiratory complications are the main cause of death for patients with ALS, due to diaphragmatic weakness, infection, and aspiration pneumonia. NIV slows the decline of vital capacity [16] and also improves lung compliance [17]. NIV not only increases survival [18], but improves quality of life, with improvements demonstrated in cognition, breathlessness, and energy [19, 20]. Finding optimal tools to evaluate respiratory function could translate into better access to these life-sustaining therapies.
There are many benefits of EIT when considering applications for clinical use. It is non-invasive, does not utilize ionizing radiation, and does not require bulbar strength or patient effort for accurate results. When bulbar dysfunction is severe, there can be significant issues obtaining accurate spirometry due to poor lip seal on the equipment. Sniff nasal pressure assessments are not reliant upon lip seal, but are less widely available in clinics, and at times, not well tolerated due to the discomfort of having a probe inserted into the nasal cavity. Spirometry accuracy is also subject to patient effort. The EIT belt is simple to apply, and results are available within minutes. The type of measurements obtained can be tailored to the population. For example, EIT can be utilized in both the upright and supine positions. This is important in the context of ALS; patients with very severe orthopnea would not be appropriate for supine EIT since they would not be able to lie supine for several minutes. Regardless, it is notable that all of our patients were able to tolerate the supine position for 10 min, even 3 patients who had very low supine FVC scores of < 50% predicted.
A limitation of this study is the relatively small number of participants. Our study population included more males than the usual ALS population. We limited participation in this study to those who could provide reproducible spirometry results, but there may be a role for future studies to evaluate the correlation between EIT and sniff nasal pressures, which is another measure of lung function that bypasses requirement for bulbar strength. A limitation of EIT is that the pictures are lower resolution (less precise level of detail) compared to other more common imaging modalities such as magnetic resonance imaging or computed tomography. However, higher resolution is not necessary for clinical uses such as ours in which determining regional lung volumes is the goal. In our study, EIT recorded lung volume changes at the macro level. Although it is capable of very precise measurements such as alveolar stability, these values are more suitable for patients who require conventional mechanical ventilation for whom optimal positive end expiratory pressures (PEEP) are unknown. Therefore, we were very careful not to attribute lung volume losses to derecruitment—although this was the most probable mechanism—but merely reported the volume changes we measured. As indicated, supine EIT would not be suitable for persons with severe orthopnea since they would not be able to tolerate the supine position, but measures could still be obtained from the upright position. The major limitation to EIT use in neuromuscular disease is its relative lack of availability since it is an emerging technology. EIT has already demonstrated important clinical utility in other settings such as the intensive care unit, where peak end expiratory pressures are titrated in complicated ventilated patients [2].
EIT was well tolerated and safe, and relevant volume measures were obtained rapidly. Pending further study, it might provide a useful adjunct to other pulmonary measures. If it could contribute to the diagnosis of early respiratory decline, particularly in the setting of bulbar dysfunction or limited patient effort, it might have meaningful clinical use. Our next research steps will include continued data collection of participants with ALS on NIV, and sequential EIT assessments to follow individual patient progression through disease course.
Author Contributions
Gregory Hansen: conceptualization, investigation, writing – original draft, methodology, writing – review and editing, validation, software, formal analysis, project administration, data curation, supervision. Adam Shaw: investigation, data curation, resources, writing – review and editing. Kala Bolt: investigation, writing – review and editing, data curation. Ryan Verity: writing – review and editing, project administration. Richard T. Nataraj: conceptualization, writing – review and editing. Kerri Lynn Schellenberg: conceptualization, investigation, funding acquisition, writing – original draft, methodology, writing – review and editing, formal analysis, project administration, data curation, supervision, resources.
Acknowledgments
ALS Society of Saskatchewan.
Ethics Statement
We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.