ASL lexicon and reporting recommendations: A consensus report from the ISMRM Open Science Initiative for Perfusion Imaging (OSIPI)
Abstract
The 2015 consensus statement published by the International Society for Magnetic Resonance in Medicine (ISMRM) Perfusion Study Group and the European Cooperation in Science and Technology ( COST) Action ASL in Dementia aimed to encourage the implementation of robust arterial spin labeling (ASL) perfusion MRI for clinical applications and promote consistency across scanner types, sites, and studies. Subsequently, the recommended 3D pseudo-continuous ASL sequence has been implemented by most major MRI manufacturers. However, ASL remains a rapidly and widely developing field, leading inevitably to further divergence of the technique and its associated terminology, which could cause confusion and hamper research reproducibility.
On behalf of the ISMRM Perfusion Study Group, and as part of the ISMRM Open Science Initiative for Perfusion Imaging (OSIPI), the ASL Lexicon Task Force has been working on the development of an ASL Lexicon and Reporting Recommendations for perfusion imaging and analysis, aiming to (1) develop standardized, consensus nomenclature and terminology for the broad range of ASL imaging techniques and parameters, as well as for the physiological constants required for quantitative analysis; and (2) provide a community-endorsed recommendation of the imaging parameters that we encourage authors to include when describing ASL methods in scientific reports/papers.
In this paper, the sequences and parameters in (pseudo-)continuous ASL, pulsed ASL, velocity-selective ASL, and multi-timepoint ASL for brain perfusion imaging are included. However, the content of the lexicon is not intended to be limited to these techniques, and this paper provides the foundation for a growing online inventory that will be extended by the community as further methods and improvements are developed and established.
1 INTRODUCTION
Following the consensus statement for the recommended implementation of arterial spin labeling (ASL) perfusion MRI for clinical application in the brain1 by the Perfusion Study Group (SG) of the International Society for Magnetic Resonance in Medicine (ISMRM) and the European Consortium for ASL in Dementia (European Cooperation in Science and Technology (COST) Action BM1103) in 2014 (referred to hereafter as the ASL White Paper), standardized ASL perfusion imaging sequences have now been implemented by the majority of MRI manufacturers. Recommended acquisition protocols and the increased availability of ASL imaging sequences have encouraged the use of ASL in clinical applications.2 However, ASL remains a rapidly and widely developing field, both in terms of improving the accuracy and precision of cerebral blood flow (CBF) quantification via advances in pulse sequence and post-processing methods, and providing other output derivatives in addition to CBF (e.g., arterial transit time). These advances have greatly expanded the scope of ASL but also bring further divergence of the technique, particularly in the terminology used, which can lead to confusion and hamper interoperability. In addition, motivated by the noninvasive nature of ASL, there is an increased number of large cohort studies that adopt ASL perfusion imaging, such as the Alzheimer's Disease Neuroimaging Initiative (http://adni.loni.usc.edu/adni-3/) and some branches of the Human Connectome Project,3 in which data are acquired from multiple sites using different MRI scanners. To maximize the usefulness of these data, guidelines for consistent reporting of image acquisition parameters are essential.
As part of the ISMRM Open Science Initiative for Perfusion Imaging (ISMRM OSIPI, referred to hereafter as OSIPI), an initiative and activity of the ISMRM Perfusion SG, the ASL Lexicon Task Force has been working on the development of an ASL Lexicon and Reporting Recommendation for Perfusion Imaging and Analysis. The purpose of the ASL lexicon is to develop standardized nomenclature and terminology for the broad range of ASL imaging techniques and parameters, as well as for the physiological constants required for quantitative analysis. However, this ASL lexicon does not provide recommended standard ASL implementations and optimal parameter values, which is the remit of the other parallel recommendations/guidelines, and the readers are directed to those, such as the ASL White Paper, for a standard ASL implementation and processing approach, and its recent extensions for up-to-date summaries of more specific ASL techniques and developments (see the following subsection “1.1 Previous efforts on ASL standardization relevant to the development of ASL Lexicon and Reporting Recommendation”). Instead, ASL lexicon aims to provide harmonization across documentation, reports, and publications by standardizing the terminology and parameter definitions, which is beyond the scope of the ASL White Paper and the others. In addition, the developed ASL lexicon is intended to form a common, community-endorsed recommendation for reporting of ASL perfusion imaging, providing a list describing which parameters in acquisition protocols should be reported by investigators and how, aiming to improve the interoperability and comparability of reported studies.
- A lexicon for researchers/developers of ASL sequences and analysis tools to conform to the community-based consensus recommendation in order to avoid misunderstandings caused by diverse terminologies and inconsistent definitions.
- A reporting guideline for researchers using ASL sequences and analysis tools to find how their ASL studies and results should be documented and reported, which should make their studies more widely understandable and reproducible.
Within the OSIPI framework, an overarching aim of this paper is to enable researchers and developers to use openly available datasets (e.g., data repositories) without ambiguity relating to the acquisition parameters used.
1.1 Previous efforts on ASL standardization relevant to the development of ASL Lexicon and Reporting Recommendation
- A consensus statement of recommended implementations of ASL perfusion imaging for clinical applications (ASL White Paper1), published by an expert group of members of the ISMRM Perfusion SG and the European Consortium for ASL in Dementia (COST Action BM1103).
- Brain Image Data Structure (BIDS) extension for ASL4 (referred to as ASL-BIDS in this paper): A community effort to standardize how to organize and share neuroimaging datasets, which was extended to include ASL in 2021 (https://bids-specification.readthedocs.io/en/stable/04-modality-specific-files/01-magnetic-resonance-imaging-data.html#arterial-spin-labeling-perfusion-data).
- Technical recommendations for renal ASL5 from an international group of experts working under the framework of “Magnetic Resonance Imaging Biomarkers for Chronic Kidney Diseases (PARENCHIMA)”, funded by the EU COST Action CA16103 (referred to here as PARENCHIMA renal ASL).
- A series of extensions to the ASL White Paper (referred to as the ASL Gray Papers in this paper) on the following topics:
- “Velocity-Selective Arterial Spin Labeling Perfusion MRI: A Review of the State of the Art and Recommendations for Clinical Implementation.”6
- “Recent Technical Developments in ASL: A Review of the State of the Art.”7
- “Current State and Guidance on Arterial Spin Labeling Perfusion MRI in Clinical Neuroimaging.”2
- “Update on State-of-the-Art for Arterial Spin Labeling (ASL) Human Perfusion Imaging Outside of the Brain.”8
- Quantitative Cerebral Perfusion MRI Using Multi-Timepoint Arterial Spin Labeling: Recommendations and Clinical Applications (preprint9).
1.2 Development process of ASL Lexicon and reporting recommendation
The ASL Lexicon task force consists of 11 Perfusion SG members with diverse expertise in ASL imaging, who attended the launch events of OSIPI during and after the annual ISMRM meeting in 2019 and expressed their interest to contribute. The developmental process of the ASL Lexicon and Reporting Recommendation was as follows:
- Required: essential for meaningful interpretation of the ASL data and for quantitative analysis. These must be included in an ASL publication in order for its data set to be ‘OSIPI-compliant’.
- Recommended: parameters that are useful for interpretation of the ASL data and could explain specific characteristics or systematic differences between data sets. Authors are encouraged to include as many of these as possible in ASL publications.
Stage 2 (June 2021–July 2021): A separate and independent expert panel provided feedback and comments on the stage 1 draft. These experts were involved with the development of the ASL Gray Papers (please see the previous subsection “1.1 Previous efforts on ASL standardization relevant to the development of ASL Lexicon and Reporting Recommendation”). Based on their feedback, an updated stage 2 draft was generated.
Stage 3 (June 2021–October 2021): A manufacturer survey was carried out with the major MRI scanner manufacturers (in alphabetical order: Canon Medical Systems Corporation, Tochigi, Japan, FUJIFILM Healthcare, Tokyo, Japan, GE Healthcare, Waukesha, WI, Philips Healthcare, Best, The Netherlands, and Siemens Healthcare, Erlangen, Germany) to identify any potential conflicts or incompatible terminologies and definitions with their current ASL product implementation. In addition, information was requested relating to if/how the acquisition parameters listed in the reporting recommendation can be obtained via the graphical user interface (GUI) of the commercial MRI scanners.
- Yes, I think Required/Recommended is the appropriate category for parameter xxx.
- No, the parameter xxx should be in another category (i.e., Recommended for Required/Required for Recommended).
- No, we should remove the parameter xxx from the recommendation.
- I am not familiar with this parameter.
On November 19, 2021, a virtual Q&A session was held with ISMRM Perfusion SG members in which the concept of this initiative was explained and any queries were addressed.
Stage 5 (February 2022–April 2022): A total of 38 responses to the survey were collected and are summarized in Figures S1–S3, which are available online. Based on those responses, the reporting recommendation was finalized and is provided in section 3: Reporting Recommendation. United Imaging Healthcare (Shanghai) also joined the manufacturer survey, and the summary of the survey responses from all six MRI manufacturers is provided in Figures S4 and S5, showing how the acquisition parameters listed in the Reporting Recommendation can be obtained via the commercial MRI scanner GUIs. It was found that, when thespecific sequence/technique is implemented as a product, all corresponding parameters in the Required category were either displayed in the GUI or available on request from the manufacturers. In the Recommended category, however, several parameters are not available for some manufacturers. Therefore, the recommendation level remains that we only “encourage” authors to include as many of the recommended parameters as possible in ASL publications. After all feedback/comments were addressed, the ASL Lexicon was divided into two groups: (a) techniques and their parameters that are widely used and mature enough to be standardized, which are mostly covered by the ASL White Paper and some (but not all) of the ASL Gray Papers; and (b) advanced and emerging techniques and their parameters. Only the former (i.e. [a]) is included in this paper, to avoid premature standardization of emerging techniques in a published paper. The final draft of this paper was shared with the ISMRM Perfusion SG members for endorsement.
May 2022–future: The online version of the ASL Lexicon and Reporting Recommendation will be managed and updated by the community as further methods and improvements are developed.
2 ASL LEXICON
The ASL lexicon organizes comprehensive lists of terminology and definitions for ASL imaging techniques and acquisition parameters, as well as physiological constants and parameters required in quantitative analysis. As explained in subsection 1.2 (stage 5), this paper contains only techniques and parameters that are widely used and mature enough to be standardized, that is: (pseudo-)continuous ASL ((P)CASL), pulsed ASL (PASL), velocity-selective ASL (VSASL), and multi-timepoint ASL for brain perfusion imaging. Other more advanced and emerging techniques (e.g., vessel-selective ASL, MR fingerprinting ASL, ASL angiography, modified ASL labeling methods that measure other physiological parameters [e.g., water extraction fraction], and corresponding image processing) and ASL applications in the body will be listed on the online version of ASL lexicon that is available at https://osipi.ismrm.org/task-forces/tf4-1/, with a view to standardization in future work.
2.1 General definition of ASL
- ASL: Any MRI technique in which contrast is generated by manipulation of the arterial blood magnetization using RF pulses prior to image acquisition, with the aim of isolating flow signal for angiography/perfusion imaging.
- Labeling pulse: RF pulse, or train of RF pulses, intended to change the magnetization state of blood in order to differentiate it from stationary tissue. In general, labeling pulses can be spatially selective, targeting the blood outside the imaging volume (upstream), or velocity-/acceleration-selective, targeting blood without special selectivity (i.e., including blood flowing within the imaging volume) according to its velocity or acceleration.
- Control pulse: RF pulse, or train of RF pulses, intended to match the static tissue magnetization transfer (MT), diffusion, eddy currents, or any other side effects of the labeling pulse, while causing minimal perturbation to arterial blood.
- Labeled image: The image acquired after preparation by a labeling pulse.
- Control image: The image acquired after preparation by a control pulse.
- Delay time: The time interval between the labeling and the image readout that allows the labeled arterial blood bolus to reach the tissue of interest. In general, it is called the post-labeling delay (PLD) in (P)CASL and inversion time (TI) in PASL. In VSASL, both TI and PLD are used to define different temporal parameters. See subsection 2.3, Parameters in ASL labeling method, Table 5, and Figures 1-3 below for more details.
- Single PLD/TI: ASL protocol in which images are acquired with a single delay time.
- Multiple PLD/TI: ASL protocol in which images are acquired with multiple (more than one) delay times.
- Background suppression (also often abbreviated as BS): The strategy for reduction of static tissue signal intensity using a train of RF pulses applied prior to image readout. The aim of background suppression is to improve SNR of the ASL image by reducing signal fluctuations in the labeled and control images. There are many background suppression schemes available, involving saturation and inversion pulses.
- Saturation: The saturation of the imaging volume is performed just before and/or after the labeling and control pulses to set its longitudinal magnetization to zero and thereby eliminate any label/control MT or slice profile mismatches. Water suppression enhanced through T1 effects (WET) pulses10 are commonly used.11
- Vascular suppression (also known as vascular crushing): The reduction of signal present in larger arterial vessels at the time of imaging. Generally, it is achieved by applying vascular crusher gradients after the excitation pulse, which selectively dephases signal based on the velocity profile of the spins in the direction of the gradient.12-14 In VSASL, vascular suppression is achieved using velocity selective saturation pulses.6
- M0 image (also known as proton density image): The additional calibration image required for blood flow quantification, used to estimate the fully relaxed magnetization (M0) of blood (M0b) and tissue (M0t), which are necessary to calculate perfusion from ASL images (see subsection 2.6 and Table 8). M0 image is commonly obtained as a proton density image by turning off all preparation pulses before acquisition while using a relatively long TR. When background suppression pulses are not applied, the average (mean) control image can be used as the M0 image by correcting for T1 relaxation.
2.2 ASL labeling methods
This subsection focuses on the name of the techniques and their notations and descriptions with regard to ASL labeling methods. In general, ASL labeling methods are divided into three labeling types: (P)CASL, PASL, and VSASL. In addition to these labeling methods, this subsection also covers the techniques/sequences for multi-timepoint ASL.
2.2.1 (Pseudo-) continuous ASL ((P)CASL)
CASL15-17 and PCASL18 are general terms for the ASL labeling methods in which labeling is performed by applying RF pulses for long duration (typically 1–3 s) in combination with a magnetic field gradient. Flowing blood spins are inverted as they flow through a thin labeling plane by means of flow-driven adiabatic inversion.19 In the ASL White Paper, PCASL is the recommended ASL labeling method for clinical use due to its high SNR efficiency compared to PASL.1 Several techniques related to (P)CASL are listed in Table 1.
| Name | Notation | Description |
|---|---|---|
| Continuous ASL15-17 | CASL | A single, continuous-wave, RF pulse applied over a long period, typically 1–3 s, in combination with a constant magnetic field gradient. Arterial blood is continuously inverted as it flows through a specified labeling plane by means of flow-driven adiabatic inversion.19 |
| Pseudo-continuous ASL18 | PCASL | Similar to CASL, labeling occurs over a long period, typically 1.5–2 s, and inverts flowing arterial blood. In PCASL, however, a train of short RF pulses applied at a rate of approximately 1 per ms replaces the single, continuous pulse of CASL. For the control scan, phase modulation of the RF pulse train is applied such that MT effects are identical to the labeling scan, but the arterial blood magnetization is unperturbed. Note that the mechanism of arterial blood inversion is equivalent for CASL and PCASL and, consequently, the quantification model is the same. |
| Balanced PCASL | bPCASL | PCASL implementation that uses the same gradient waveform for the label and control pulses. |
| Unbalanced PCASL | ubPCASL | PCASL implementation that uses different gradient waveforms for the label and control pulses, so that the Gav becomes zero for the control. If optimized, improved robustness to off-resonance effects at the labeling plane can be achieved compared to bPCASL.20 |
| Separate RF labeling coils21, 22 | Using separate, dedicated RF transmission coils (i.e., in addition to the RF transmit coils for imaging) positioned over the artery/arteries of interest, to reduce power deposition and avoid MT effects in the perfused organ. | |
| Flow-encoding arterial spin tagging13 | FEAST | A technique based on (P)CASL that acquires a pair of ASL subtraction images with and without crusher gradients for vascular suppression. The ATT is calculated using the ratio between (P)CASL images with and without vascular suppression. |
- Abbreviation: ASL, arterial spin labeling; ATT, arterial transit time; Gav, average gradient; MT, magnetization transfer.
2.2.2 Pulsed ASL (PASL)
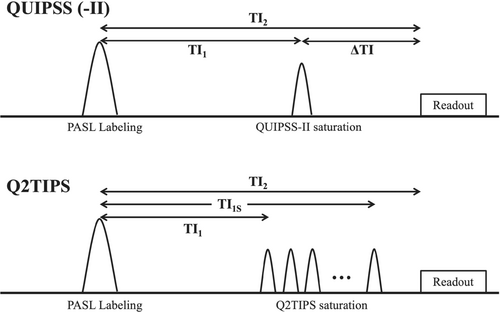
PASL23-25 is a general term for the ASL labeling method in which the labeling is performed by applying a single (or a limited number of) short RF pulse(s) that instantaneously invert the blood magnetization. In general, PASL labeling methods are grouped into two types: (i)asymmetric PASL, in which a spatially selective RF slab (typically 10–20 ms) labels the spins outside of the imaging volume on the upstream side (i.e., neck for imaging of brain), for example, Echo-planar imaging and signal targeting with alternating radiofrequency (EPISTAR)26; and (ii) symmetric PASL, in which the label is performed by a nonselective global inversion pulse (e.g., Flow-sensitive alternating inversion recovery (FAIR)24) and spins outside of theimagingvolume are labeled, regardless of whether they are upstream or downstream, symmetrically. In PASL, the bolus duration of labeled blood is unknown a priori and depends on the labeling slab thickness and blood flow velocity. To achieve accurate quantification of CBF with a single TI acquisition, a bolus cutoff technique, such as quantitative imaging of perfusion using a single subtraction II (QUIPPS-II)27 and QUIPPS-II with thin-slice TI1 periodic saturation (Q2TIPS),28 is applied to define the bolus duration. Figure 1 shows schematic sequence diagrams of QUIPSS-II and Q2TIPS. Several labeling methods related to PASL are listed in Table 2.
| Name | Notation | Description |
|---|---|---|
| Pulsed ASL | PASL | A general term for ASL methods with a single (or a limited number of) short RF pulse(s) (typically 10–20 ms) applied to “instantaneously” invert a slab of arterial blood magnetization. |
| Echo-planar imaging and signal targeting with alternating radiofrequency26 | EPISTAR, (also known as STAR for non-EPI readout) | A variation of PASL in which the label is performed by a slab-selective adiabatic inversion pulse applied proximal to the imaging volume/slices. In the original multi-slice implementation, the control preparation was achieved by applying slab-selective RF pulses over the same region as the label, with total power matched to the labeling inversion pulse (to generate the same MT effects across the imaging volume) but which resulted in minimal perturbation of the arterial blood magnetization, for example, two consecutive inversion pulses with half power. In the product implementation by Philips Healthcare, however, the control preparation is achieved by mirroring the frequency modulation for the second part of the adiabatic pulse.29 |
| Flow-sensitive alternating inversion recovery24 | FAIR | A variation of PASL in which the label is performed by a non–slice-selective global inversion pulse, whereas the control image is obtained using a slice-selective inversion pulse applied to the imaging slab. Because of this symmetric nature, FAIR allows the inflow of the labeled blood from both sides of the imaging volume. |
| Proximal inversion with control for off-resonance effects30 | PICORE | A variation of PASL, in which the label is the same as in EPISTAR, whereas the control image is obtained using an off-resonance inversion pulse that is applied with the same frequency offset as the label but without a slab-selective gradient. |
| Double inversions with proximal labeling of both tag and control images31 | DIPLOMA | A variation of PASL designed to reduce the residual MT mismatch between the label and control images observed in EPISTAR and PICORE. In both label and control, two consecutive adiabatic inversion pulses are applied; in the labeling preparation, application of an off-resonance inversion pulse (similar to the one applied in PICORE for control preparation) is followed by a slab-selective inversion pulse. In the control preparation, two slab-selective inversion pulses are applied. |
| Transfer-insensitive labeling technique32 | TILT | A variation of PASL in which labeling is achieved by two successive 90° RF pulses. For the control, the phase of the second pulse is shifted by 180°, thereby yielding no net effect on blood water magnetization. |
| Bolus cutoff technique | In PASL, the bolus duration (see Table 5 for the definition) of labeled blood is unknown a priori and depends on the labeling slab thickness and blood flow velocity. To achieve accurate quantification of CBF with a single TI acquisition, several techniques have been proposed to define the bolus duration, as described below. | |
| Quantitative imaging of perfusion using a single subtraction27 | QUIPSS | QUIPSS aims to eliminate arterial transit time effects in PASL, to enable reliable quantification of CBF with a single TI acquisition. This is achieved by applying a saturation RF pulse to the imaging volume at a time TI1 after labeling, when TI1 is greater than the arterial transit time, followed by image acquisition at time TI. N.B. this approach has not been widely adopted due to the prevalence of intravascular signal in the ASL difference images. |
| Quantitative imaging of perfusion using a single subtraction II28 | QUIPSS-II | QUIPSS-II aims to control the bolus duration in PASL and allow reliable quantification of CBF when using PASL with a single TI. This is achieved by applying a saturation RF slab to the area in which the labeling RF slab is applied, thereby cutting off the “tail” of the labeled bolus. See “Bolus duration” in Table 5 for the definition. |
| QUIPPS II with thin-slice TI1 periodic saturation28 | Q2TIPS | Modified version of QUIPSS-II, aiming to improve the saturation efficiency by replacing the QUIPSS-II saturation pulse with multiple thin RF saturation pulses applied at the distal edge of the labeling slab. |
| QUIPSS II with window-sliding saturationsequence33 | Q2WISE | A hybrid technique between Q2TIPS and QUIPSS II. In Q2WISE, saturation is achieved by using two thin saturation pulses and one thick slab saturation pulse to reduce the RF power deposition. |
| Wedge-shaped PASL34 | WS-PASL | A variation of PASL in which a wedge-shaped adiabatic inversion pulse is used to directly control the bolus duration in different vessels based on the flow velocity. |
| Attenuating the static signal in arterial spin tagging35 | ASSIST | FAIR ASL approach with multiple inversion pulses during the TI to suppress static tissue signal (first implementation of background suppression with ASL). |
- Abbreviation: CBF, cerebral blood flow; MT, magnetization transfer; TI, inversion time.
| Name | Notation | Description |
|---|---|---|
| Velocity-selective ASL6, 36 | VSASL | A general term for ASL techniques in which the magnetization is labeled by saturation or inversion based on its velocity. See Figure 2 for a general schematic diagram. In the original implementation, the saturation of flowing blood signal is achieved using a DRHS/T37 or BIR-838 pulse train in combination with velocity-encoding gradients. Control images are acquired without velocity-encoding gradients. |
| Fourier-transform–based velocity-selective saturation ASL39, 40 | FT-VSS ASL | A variation of VSASL in which the magnetization within a certain velocity band is saturated by a train of composite pulses incorporating velocity-sensitive bipolar gradients and refocusing 180° pulses. In contrast to the above-mentioned original implementation of VSASL, in FT-VSS-ASL, the static magnetization is saturated while preserving the magnetization flowing above the velocity threshold. In the control image acquisition, all magnetization is saturated. |
| Fourier-transform– based velocity-selective inversion ASL37 | FT-VSI ASL | Analogous to the FT-VSS ASL method described above, FT-VSI ASL uses composite velocity-selective inversion pulses to invert both flowing and static tissue magnetization (label) or only the static tissue magnetization (control). SNR is improved compared with saturation-based VSASL. |
| Multi-module velocity-selective ASL41 | mm-VSASL | A strategy to measure ASL signal with multiple VS labeling modules to increase labeling bolus duration and reduce T1 relaxation of the ASL signal. This method provides improved SNR compared to conventional single-module VSASL with VS saturation. |
| Acceleration-selective ASL42 | AccASL | An extension of VSASL that labels (saturates) based on the acceleration/deceleration of blood spins rather than their velocity. Because arterial blood exhibits stronger acceleration/deceleration, it labels predominantly arterial (as opposed to venous) blood. AccASL includes both CBF and CBV weighting. |
- Abbreviation: BIR-8, B1-insensitive rotation-8; CBF, cerebral blood flow; CBV, celebral blood volume; DRHS/T, double-refocused hyperbolic secant/tangent.
2.2.3 Velocity-selective ASL (VSASL)
VSASL6, 36 is a general term for the ASL labeling method in which the magnetization is labeled by saturation or inversion based on its velocity. See Figure 2 for a general schematic diagram. In the original implementation, the saturation of flowing blood signal is achieved using a double-refocused hyperbolic secant/tangent (DRHS/T)37 or B1-insensitive rotation-8 (BIR-8)38 pulse train in combination with velocity-encoding gradients in subsequent implementations. Control images are acquired without velocity-encoding gradients. Several variant approaches in VSASL are listed in Table 3. Detailed descriptions of the VSASL technique and recommendations for clinical application can be found in the recent ASL Gray Paper.6
2.2.4 Multi-timepoint ASL
Multi-timepoint ASL43-46 is a general term for ASLtechniques in which data are acquired repeatedly with several time parameters (delay time, and/or labelingduration for PCASL) to observe the kinetic ASL signal. These approaches are often called multi-delay ASL, particularly when only the delay time is varied. Multi-phase ASL is also sometimes used as a synonym of multi-delay ASL; however, this should not be confused with the PCASL approach that uses a range of RF phase offsets in the PCASL pulse train to reduce the sensitivity of the CBF estimation to B0 inhomogeneity.47 Table 4 shows several approaches to achieve multi-timepoint ASL. Detailed descriptions and recommendations for the use of multi-timepoint ASL can be found in the relevant recent ASL Gray Paper.9
| Name | Notation | Description |
|---|---|---|
| Multi-timepoint ASL | A general term for ASL techniques in which ASL data are acquired repeatedly with varied time parameters (delay time, and/or labeling duration for PCASL) to observe the kinetic ASL signal. Also often called multi-delay ASL, particularly when only the delay time is varied. | |
| Multi-timepoint sequential ASL44, 48 | Multi-time point ASL acquisition that acquires images with multiple timepoints as successive single-TI/PLD scans, as opposed to LL-ASL or time-encoded PCASL. | |
| Look–Locker ASL49 | LL-ASL | ASL acquisitions in which several images are acquired at multiple time points after a single labeling module. Readouts with low flip angle are used to reduce saturation of the labeled blood by the first readouts. |
| Quantitative STAR labeling of arterial regions12 | QUASAR | PASL-based sequence that consists of several Look–Locker readouts: (i) with and without vascular suppression to obtain local arterial input function; (ii) two different readout flip angles. A Q2TIPS-like saturation is used to define the bolus duration. This sequence allows measurement of the local AIF and quantification of CBF by deconvolution. |
| Reduced resolution transit delay prescan50 | A fast multi-timepoint ASL implementation that is specifically used to acquire low spatial resolution arterial transit time maps. Typically used as an ancillary scan to enhance the quantification accuracy of a standard-resolution single-PLD ASL acquisition. | |
| Time-encoded PCASL (also commonly referred to as Hadamard-encoded)51 | te-PCASL | Segmenting the PCASL labeling/control module into varying control and label sub-periods according to an encoding matrix. This improves the temporal efficiency of multi-timepoint ASL; that is, it reduces the number of acquisitions required for a multi-PLD data set. The most typical implementation is Hadamard encoding. Modifications include, for example, Walsh-ordering.52 |
- Abbreviation: AIF, arterial input function; PLD, post-labeling delay; TI, inversion time.
2.3 Parameters in ASL labeling method
The parameters related to ASL labeling methods are provided in Table 5. In general, the names and definitions of parameters comply with the ASL White Paper,1 as well as ASL-BIDS4; otherwise, the difference is provided in the description. In general, for timing parameters there is no preference between the use of “ms” and “s.” In ASL-BIDS, however, the values in JSON sidecars are entered without specifying the units; therefore, the use of correct units, as specified in the ASL-BIDS definition, should be strictly followed.
| Name | Notation | Unit | Description |
|---|---|---|---|
| Labeling duration | LD; alsoknownas τ | ms or s | For CASL/PCASL. Duration of the constant CASL labeling RF or PCASL labeling pulse train (see Figure 3). |
| Bolus duration | BD | ms or s | For PASL. Temporal width of the labeled bolus. For QUIPSS-II/Q2TIPS, this is defined as the time from the labeling pulse to the center of the first saturation pulse (and is equal to TI1, see below). If QUIPSS-II/Q2TIPS saturation is not used, this parameter is not known a priori but is determined by the arterial blood velocity and inversion slab thickness, or the RF transmit coil length for FAIR. |
| Post-labeling delay | PLD | ms or s | For CASL/PCASL. Time from the end of the labeling pulse to the center of the imaging excitation pulse (see Figure 3). In a 2D multi-slice acquisition, the PLD is defined by the time of the first slice acquisition; however, it is important to note that the effective PLD for each slice is different and is determined by the PLD and the interslice time (see Table 6). |
| Inversion time | TI | ms or s | For general PASL. Time from the center of the labeling pulse to the center of the imaging excitation pulse. In 2D multi-slice acquisition, this relates to the first acquired slice. ASL-BIDS uses the term post-labeling delay for this parameter in PASL. |
| Inflow time | ms or s | In some post-processing tools (e.g., FSL), inflow time is used to define the time from the start of labeling to the center of the imaging excitation pulse. For PASL, it is equivalent to inversion time. For PCASL, however, inflow time will be equivalent to PLD + LD. | |
| TI1 | ms or s | For QUIPSS (-II)/Q2TIPS. Time from the center of the labeling pulse to the center of the bolus saturation pulse (QUIPSS [-II]) or center of the first saturation pulse (Q2TIPS) (see Figure 1). BIDS uses the term BolusCutOffDelayTime (1). | |
| TI2 | ms or s | For QUIPSS (-II)/Q2TIPS. Time from the center of the labeling pulse to the center of the excitation pulse of the image acquisition. This value is equivalent to TI of the conventional (non–QUIPSS-II/Q2TIPS) PASL (see Figure 1). | |
| ΔTI | ms or s | For QUIPSS (-II), defined as TI2–TI1 (see Figure 1). | |
| TI1 stop | TI1s | ms or s | For Q2TIPS. Time from the center of the labeling pulse to the center of the last bolus saturation pulse (see Figure 1). BIDS uses the term BolusCutOffDelayTime (2). |
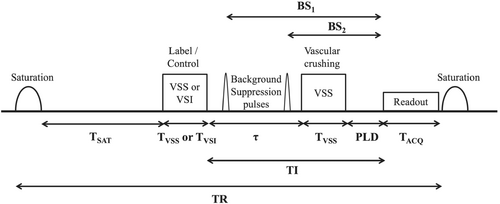
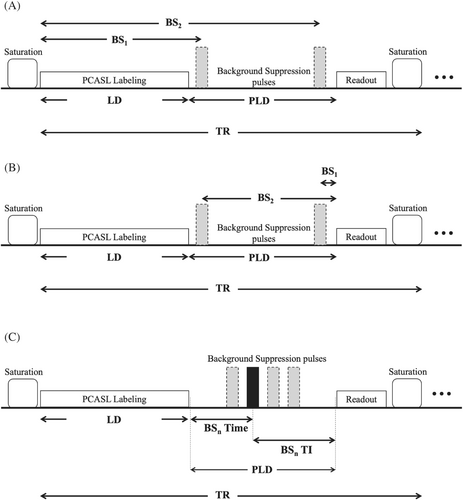
| Background suppression (pulse) timing | BS1 to BSn | ms or s | The timing parameters for the background suppression RF pulses. Currently, there are three different definitions for these timings implemented in commercial scanners (please see Figure 3): (A) time from the center of either the labeling pulse (for PASL) or the first labeling pulse (PCASL) to the center of the Nth background suppression pulse; (B) time from the center of the Nth background suppression to the center of the first readout excitation pulse; and (C) BSn time from the center of the last PCASL labeling pulse to the center of the Nth BS pulse, and BSn TI from the center of the Nth BS pulse to the center of the first excitation pulse. |
| Vascular crusher gradient strength | Venc | cm/s | Crusher gradients have an amplitude sufficient to cause a 180° phase shift for blood moving with a velocity of Venc in the direction of the gradients. |
| B | s/mm2 | Crusher gradients are equivalent to diffusion-weighting gradients with this b value.53 | |
| Labeling plane | Plane at which flowing blood is labeled in (P)CASL. | ||
| Fixed labeling plane means the labeling plane is parallel to the image slice orientation and angulation with a specified distance relative to the lowest slice. | |||
| Free labeling plane means the labeling plane can be moved and angulated independently from the image volume. | |||
| Labeling plane offset/distance | mm | For PCASL. This is the distance between the center of the imaging volume and the center of the labeling plane. | |
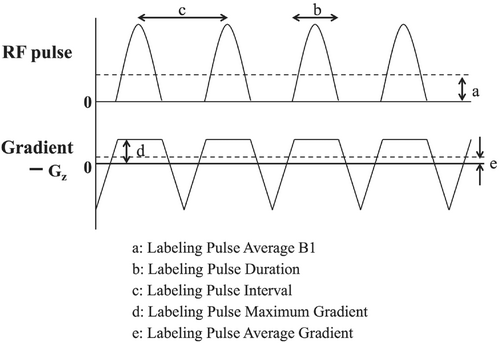
| Labeling pulse average gradient | Gav | mT/m | For PCASL. The non-zero mean gradient applied concurrently with the RF labeling pulses, which combines to produce flow-driven adiabatic inversion (see Figure 4). |
| Labeling pulse maximum gradient | Gmax | mT/m | For PCASL. The amplitude of the slice-selection gradient applied during the labeling pulses in the PCASL labeling pulse train (see Figure 4). |
| Labeling pulse average B1 | B1av | μT | For (P)CASL. The average B1-field strength of the RF labeling pulses over the entire pulse train (see Figure 4). |
| Labeling pulse flip angle | degree (°) | For PCASL. The flip angle of a single labeling pulse in the pCASL labeling pulse train. | |
| Labeling pulse interval | ms | For PCASL. The interval between the centers of two successive PCASL labeling pulses (see Figure 4). | |
| Labeling pulse duration | ms | For PCASL. The duration of each PCASL labeling pulse (see Figure 4). | |
| PCASL control type | For PCASL. Type of the gradient scheme used in pCASL control condition: either balanced or unbalanced. | ||
| Balanced: Identical Gav (non-zero) for label and control. | |||
| Unbalanced: Gav in label is nonzero but zero in control (refocusing gradient lobes are increased in amplitude such that the mean gradient is zero). | |||
| Labeling slab | For PASL, the volume over which the labeling RF pulse is applied. | ||
| Labeling slab thickness | mm | For PASL. The nominal thickness of the labeling slab. | |
| Labeling slab gap | mm | For PASL, this is the nominal gap between the leading edge of the labeling slab and the closest edge of the imaging volume. | |
| Cutoff velocity | Vcut | In VSASL, spins moving above a chosen velocity, referred to as the cutoff velocity (Vcut), is labeled. Vcut determines how deep into the arterial tree the blood is labeled. |
- Abbreviation: BIDS, Brain Image Data Structure; FSL, FMRIB software library.
In ASL perfusion imaging, the application of background suppression is recommended. It should be noted that, currently, there are three different ways in which the background suppression pulse timings are defined by six major MRI manufacturers (Canon, Fujifilm, GE, Philips, Siemens, and United Imaging; in alphabetical order), which are shown in Figure 3.
2.4 Readout sequences and parameters
In this subsection, the basic readout sequences and parameters that appeared in the ASL White Paper1 are listed (see Table 6). More advanced readout strategies can be found in the advanced ASL Gray Paper.7
| Name | Notation | Unit | Description |
|---|---|---|---|
| Echo-planar imaging | EPI | A 2D rapid imaging technique in which an excitation pulse is followed by acquisition of multiple k-space lines by switching the readout gradient polarity rapidly and applying phase-encoding blips. In single-shot EPI, all k-space lines are collected after a single excitation pulse, making it robust to motion. | |
| Gradient and spin echo | GRASE | Rapid imaging technique in which the excitation pulse is followed by several refocusing pulses (similar to fast/turbo spin echo), and after each refocusing pulse, a series of gradient echoes are collected by rapidly switching the readout gradient polarity (similar to EPI). The use of refocusing RF pulses prolongs the lifetime of the transverse magnetization compared to EPI. Typically acquired as a multi-shot 3D acquisition in ASL applications. | |
| Stack-of-spirals RARE or FSE | SoS | Non-Cartesian 3D fast spin-echo (also known as turbo spin-echo, or RARE) acquisition technique, in which the readout is performed using a spiral trajectory to efficiently sample kx-ky, with each spin echo being assigned to a different kz partition. Typically acquired as a multi-shot 3D acquisition in ASL applications. | |
| Segmented 3D sequence | 3D acquisition scheme (e.g., 3D GRASE or SoS) in which k-space is acquired over multiple TRs to keep each individual readout to a reasonable duration. It should be noted that, as compared to the single-shot sequence, this approach is more sensitive to motion. Also known as multi-shot 3D sequences. | ||
| Number of segments/shots | Nseg | In a segmented 3D sequence, this is the number of acquisition repeats required to sample the full k-space data set. | |
| Repetition time | TR | ms | The time from the beginning of a labeling/control pulse to the beginning of the next control/labeling pulse. Note that, when a readout sequence with multiple excitation pulses (e.g., balanced SSFP) is used, this TR is different to the TR of the readout sequence. RepetitionTimePreparation is used in BIDS to differentiate this from RepetitionTimeExcitation. |
| Total acquired pair | The number of paired labeled and control images acquired for improving SNR (averaging) in single-delay ASL, or for fitting in multi-time point ASL. Note that, if online averaging is performed, this number will be greater than the number of reconstructed image pairs; in the extreme, the latter may be a single image pair, representing the average over all acquisitions. | ||
| NB for te-PCASL, images are not acquired in label-control pairs; therefore, in this situation it is appropriate to specify the number of repeats of the full encoding matrix. | |||
| Interslice time | ms | For a 2D multi-slice acquisition scheme, the time between the excitation pulses of successive slices. This is needed in order to calculate the effective PLD/TI for each slice, which is required for accurate quantification. |
- Abbreviation: RARE, rapid acquisition with relaxation enhancement. SSFP, steady state free precession
2.5 Derived parameters
Table 7 provides a list of the derivative parameters of standard ASL, namely that commonly appear in the perfusion imaging using single PLD. In general, the names and definitions of parameters comply with the ASL White Paper,1 as well as ASL-BIDS4; otherwise, the difference is provided in the description.
| Name | Notation | Unit | Description |
|---|---|---|---|
| ASL difference image | ΔM | Arbitrary unit | Image obtained by subtracting the labeled image from the control image, which subtracts out the static tissue signal and consequently shows the perfusion-weighted signal produced by ASL preparation. |
| Also known as DeltaM | |||
| Also known as Perfusion weighted image | |||
| Normalized perfusion weighted image | ΔM/M0 | % | ASL difference image normalized by the M0, with a unit in %. |
| Cerebral blood flow | CBF | mL/100 g/min | Quantity of blood (mL) reaching 100 g of brain tissue per unit of time (min). |
| Arterial transit time | ATT | ms | Time between when blood is labeled and when it first arrives in the imaging voxel/slice. |
| BAT | |||
| Note that ATT, AAT, and BAT are dependent on the positioning of the labeling plane/slab relative to the imaging volume, and are therefore not generally comparable across studies. | |||
| Also known as bolus arrival time | |||
| AAT | |||
| Also known as Arterial arrival time | |||
| Partial volume54, 55 | PV | The typical voxel size of ASL perfusion image is much larger than the cortical thickness, and individual voxels are likely to contain a mixture of GM, WM, and CSF, which is known as the PV effect. | |
| Tissue partial volume | PGM, PWM | Fraction (0–1) | Partial volume of different tissue types (GM, WM, CSF) as a fraction of the total voxel volume. |
| Also known as fractional tissue volume | |||
| Tissue specific perfusion | CBFGM, CBFWM | Perfusion of specific tissue types within a voxel, estimated either by (a) including only voxels with a tissue probability value higher than a stated threshold, or (b) explicitly correcting for the partial volume effects of GM/WM/CSF within voxels. |
- Abbreviation: AAT, Arterial arrival time; BAT, bolus arrival time; CSF, cerebrospinal fluid; GM, gray matter; ; WM, white matter.
2.6 Ancillary parameters for quantification
This subsection focuses on the name, notations, and descriptions of the physiological constants andancillary parameters used in ASL quantification, including equations for quantification.
2.6.1 One-compartment model for single-PLD
The general kinetic model is used to derive the CBF quantification equations below. Several assumptions need to be fulfilled to ensure its validity—for example, delivery of the entire bolus to the tissue and that label relaxation is governed by blood T1 during the entire measurement. This is the basic quantification model recommended by the ASL White Paper.1 A list of the parameters used in these equations is provided in Table 8.
| Name | Notation | Unit | Description |
|---|---|---|---|
| T1 relaxation time of blood | T1b | ms | The longitudinal relaxation time of arterial blood |
| Also known as blood T1 | |||
| Equilibrium magnetization of blood | M0b | Arbitrary unit | Fully relaxed longitudinal magnetization of arterial blood, which is required to scale the subtracted ASL signal and obtain absolute CBF units. In the ASL White paper, it is recommended to estimate M0b from a voxel-by-voxel M0t measured by an M0 image. The blood–brain partition coefficient λ scales M0t to M0b. |
| Also known as M0 of blood | |||
| Equilibrium magnetization of tissue | M0t | Arbitrary unit | Fully relaxed longitudinal magnetization of tissue. This value might be different in different organs or tissue types within an organ. |
| Also known as M0 of tissue | |||
| Blood–brain partition coefficient | λ | mL/g | The ratio between blood and tissue water concentration at equilibrium in mL of blood, per g of tissue. When used in ASL quantification, instantaneous equilibrium between tissue and veins is assumed |
| Labeling efficiency | α | Fraction (0–1) | Combines the inversion efficiency of the labeling pulse itself and the loss of label caused by background suppression (dependent on the number and type of BS pulses). A value of 1 corresponds to full inversion of blood magnetization. |
3 REPORTING RECOMMENDATION
- Required: essential for meaningful interpretation of the ASL data and for quantitative analysis. These must be included for describing ASL methods in reports/articles in order for its data set to be OSIPI-compliant.
- Recommended: parameters that are useful for interpretation of the ASL data and could explain specific characteristics or systematic differences between data sets. Authors are encouraged to include as many of these as possible in ASL publications.
| Name | Abbreviation | Style | Condition |
|---|---|---|---|
| Required parameters: General | |||
| Arterial spin labeling type | PASL, (P)CASL, Velocity-selective, etc. | ||
| Background suppression | BS | Yes/No | |
| Method for M0b estimation | The description of how M0b is estimated, e.g., how M0 image is acquired, or any special method to estimate M0b directly. | When CBF estimation is performed | |
| Total acquired pairs | The number of paired labeled and control images, before online averaging is performed (if applicable) | ||
| Acquisition voxel size | Value in mm | ||
| Required parameters: (P)CASL | |||
| Labeling duration | LD or τ | Value in ms or s | When (P)CASL is used |
| Post-labeling delay | PLD | Value in ms or s | When (P)CASL is used |
| Required parameters: PASL | |||
| Inversion time/inflow time | TI | Value in ms or s | When PASL is used |
| Bolus cutoff techniques | Name of technique, or None | When PASL is used | |
| TI1 | Value in ms or s | When QUIPSS-II or Q2TIPS are used | |
| TI2 | Value in ms or s | When QUIPSS-II or Q2TIPS are used | |
| TI1s | Value in ms or s | When Q2TIPS is used | |
| Recommended parameters: General | |||
| Number of background suppression pulse | Value | If BS is used and details are available to the user | |
| Background suppression (pulse) timing | BS1 to BSn or BS time/TI | Value in ms | If BS is used and details are available to the user |
| Background suppression timing definition | Description of how timing is defined. See “Background suppression (pulse) timing” in Table 5, or Figure 3. | If BS is used and details are available to the user | |
| Labeling location description | Description of the labeling plane/slab location (other factor than offset/gap), such as the planning of the labeling plane/slab with respect to the imaging slices | ||
| Shim volume | Description of shim volume used, e.g., imaging volume only, both imaging volume and labeling region, labeling region during labeling pulse and imaging volume during acquisition, or other (please specify) | ||
| Vascular crushing | Venc | Value in cm/s | When vascular crushing is performed. Ideally, both Venc and b should be specified |
| b | Value in s/mm2 | ||
| Recommended parameters: (P)CASL | |||
| PCASL control type | Balanced or unbalanced | When PCASL is used | |
| CASL type | If a separate coil is used for labeling | When CASL is used | |
| Labeling plane offset/distance | Value in mm | ||
| Labeling pulse average gradient | Gav | Value in mT/m | When details are available to the user |
| Labeling pulse maximum gradient | Gmax | Value in mT/m | When details are available to the user |
| Labeling pulse average B1 | B1av | Value in μT | When details are available to the user |
| Labeling pulse flip angle | Value in degree (°) | When details are available to the user | |
| Labeling pulse interval | Value in ms | When details are available to the user | |
| Labeling pulse duration | Value in ms | When details are available to the user | |
| Recommended parameters: PASL | |||
| PASL type | EPISTAR, FAIR, PICORE, etc. | ||
| Labeling slab thickness | Value in mm | ||
| Labeling slab gap | Value in mm | ||
4 SUMMARY AND CONCLUSION
On behalf of the ISMRM Perfusion SG, this paper is intended to form a community-endorsed lexicon and recommendation for reporting of ASL perfusion imaging, detailing which parameters in acquisition protocols and analysis should be reported and how, with the aim of improving the reproducibility and consistency of the reported studies. In the future, this lexicon could also be used to improve the Digital Imaging and Communicationsin Medicine (DICOM) standard for the purposes of communicating raw images and parametric maps of ASL perfusion MRI.
ACKNOWLEDGMENTS
The authors would like to thank the expert panel members (in alphabetical order): Michael Chappell (University of Nottingham), Jia Guo (University of California Riverside), Luis Hernandez-Garcia (University of Michigan), Thomas Okell (University of Oxford), Qin Qin (Johns Hopkins University), Eric Wong (University of California San Diego), Joseph Woods (University of Oxford), for their feedback—and the following representatives of MRI manufacturers in aphabetical order): Valentin Prevost (Canon Medical Systems Corporation), Takashi Tsuneki (FUJIFILM Healthcare), David Shin, Marc Lebel and Suchandrima Banerjee (GE Healthcare), Kim van de Ven (Philips Healthcare), Josef Pfeuffer and Marta Vidorreta (Siemens Healthcare), Jun Xie (United Imaging Healthcare). The authors also thank the ISMRM Perfusion SG members, especially those who responded to the online survey and poll, as well as those who provided feedback during the public presentation. We also thank the ISMRM Publication Committee for reviewing the work and coordinating the ISMRM Board of Trustees approval process.
CONFLICT OF INTEREST STATEMENT
One of our co-author, Manuel Taso, has started to work for Siemens Medical Solutions USA, after the submission of our manuscript in March.
FUNDING INFORMATION
y.s. is supported by the Royal Academy of Engineering Research Fellowship scheme (RF/201920/19/236) and core funding from the Wellcome Trust (203139/Z/16/Z). d.l.t. is supported by the University College London Hospitals (UCLH) National Institute for Health and Care Research (NIHR) Biomedical Research Centre and the Wellcome Trust (Centre award 539208). s.d. is supported by National Institutes of Health (NIH) (grants R03 AG063213 and R01 NS111115). m.f-s. is supported by the Spanish Ministry of Science, Innovation and Universities (grants PI18/00084 and PI21/00578). t.l. is supported by the German Research Foundation (DFG) (grant LI-3030/2-1). h.j.m.m.m. is supported by the Dutch Heart Foundation (03-004-2020-T049); the Eurostars-2 joint programme with co-funding from the European Union Horizon 2020 research and innovation programme (grant ASPIRE E!113701), provided by the Netherlands Enterprise Agency (RVO); and the EU Joint Program for Neurodegenerative Disease Research, provided by the Netherlands Organization for Health Research and Development and Alzheimer Nederland (DEBBIE) (JPND2020-568-106).
Open Research
DATA AVAILABILITY STATEMENT
The online full version of the ASL Lexicon and Reporting Recommendation is available on the OSIPI website (https://osipi.ismrm.org/task-forces/tf4-1/). LaTex equations used in this manuscript are provided together with their source code on the OSIPI website as well. Material can be freely reused in publications and educational material.