Do we really need two sessions?: The use of a structured interview as a trauma cue reactivity paradigm
Abstract
Objectives
Derived from classical conditioning theory and rooted in motivational mechanisms, cue reactivity paradigms (CRPs) are used in addictions research to measure participants' propensities for substance-relevant responses (e.g., craving) during exposure to substance-relevant cues (e.g., drug paraphernalia). CRPs are also useful in PTSD-addiction comorbidity research, allowing the study of affective and substance-relevant responses to trauma cues. However, studies using traditional CRPs are time-consuming with high attrition rates due to repeat testing. Thus, we sought to test whether a single session semi-structured trauma interview could serve as a CRP in terms of eliciting theorized cue exposure effects on craving and affect measures.
Method
Fifty regular cannabis users with trauma histories provided detailed descriptions of their most traumatic lifetime experience, and a neutral experience, according to an established interview protocol. Linear mixed models examined the effect of cue type (trauma vs. neutral) on affective and craving responses.
Results
As hypothesized, the trauma interview elicited significantly greater cannabis craving (and alcohol craving among the drinkers), and, greater negative affect among those with more severe PTSD symptoms, compared to the neutral interview.
Conclusion
Results suggest an established semi-structured interview may function effectively as a CRP for use in trauma and addictions research.
1 INTRODUCTION
Individuals with substance use disorder tend to experience both physiological (e.g., increased heart rate; Starcke et al., 2018) and psychological (e.g., increased substance craving; Romero-Sanchiz et al., 2022) reactions when exposed to substance-related cues. Cue-reactivity paradigms (CRPs) allow researchers to examine whether exposure to a particular cue or reminder elicits reactivity or a change in state (e.g., craving, affect, heart rate). Traditionally, CRPs have utilized drug-related stimuli as cues to understand how relapse might occur when individuals are exposed to situational antecedents of drug use (i.e., cues). CRPs are derived from classical conditioning theory (e.g., to study involuntary craving elicited by exposure to a substance use cue established through classical conditioning; Sayette et al., 2000) and operant conditioning theories (e.g., learning to associate substance use with reward or relief; Verheul et al., 1999). Both learning theories suggest that, over time, repeated exposure to substance use-related cues can lead to the development of conditioned craving (Carter & Tiffany, 1999). Indeed, research has shown that exposure to substance use cues is associated with both increased craving (Coffey et al., 2006) and substance use behavior (Drobes, 2002) in substance-using samples.
In laboratory-based CRPs, participants are exposed to an audio and/or visual cue (e.g., an audio clip describing substance use imagery and/or a visual reminder such as drug paraphernalia), and their subjective (e.g., self-reported craving, self-reported negative affect [NA] and/or positive affect [PA]) and/or physiological responses (e.g., salivation, heart rate) are measured during or immediately following the cue exposure and compared to levels of the same variable during/following a neutral cue (e.g., toothbrush) and/or to their baseline (pre-cue exposure) levels.
CRPs have also been used to help understand why certain addictive disorder-mental health disorder comorbidities occur. For example, post-traumatic stress disorder (PTSD) shows high rates of comorbidity with substance use disorder (SUD; Walsh et al., 2014). Individuals with trauma histories generally, and PTSD particularly, may use substances as a means of coping with NA responses to trauma reminders (e.g., encounters with external trauma reminders or experiences of intrusive traumatic memories; Jacobsen et al., 2001). Theoretically, strong memory associations are likely to form between the trauma cue, substance use behavior, and relief consequences that may elicit conditioned craving and reinforce substance use when the individual reencounters trauma cues (Romero-Sanchiz et al., 2022). For example, an individual with PTSD might use cannabis when reminded of a past traumatic event to feel relief from the NA elicited by that reminder. Repeated cannabis use in such situations may lead to the development of conditioned cannabis craving (Sayette et al., 2000) upon exposure to trauma cues, as the user has been conditioned to associate trauma cues with aversive NA (Stasiewicz & Maisto, 1993) and cannabis use with relief of the NA (Romero-Sanchiz et al., 2022).
Consistent with this theory, lab-based research has demonstrated a general pattern of greater self-reported NA and substance craving during exposure to trauma cues (compared to neutral cues or pre-exposure levels) across populations of trauma-exposed substance users (see review by DeGrace et al., 2022). Moreover, research has shown that drinkers with PTSD (vs. no PTSD) experience greater conditioned alcohol craving following trauma cue exposure (Read et al., 2017). Similarly, Romero-Sanchiz et al. (2022) found that PTSD symptom severity was positively associated with relief cannabis craving and NA responses to trauma versus control cues in cannabis users with trauma histories. However, as described by Nosen et al. (2012), cue reactivity research has yet to firmly establish if an increase in/greater NA during trauma cue exposure (compared to pre-exposure levels or neutral cue exposure) is accompanied by a decrease in/lesser PA, or more ambivalent (e.g., high NA and PA) responses. Taken together, these findings using traditional CRP methods suggest that NA responses and conditioned substance craving to trauma cues may be greater among those trauma exposed individuals with greater PTSD symptomatology; this provides a possible mechanism to help explain high rates of PTSD-SUD comorbidity (Walsh et al., 2014).
Trauma CRP cues are often chosen to be specific to the participant's own trauma history (e.g., Romero-Sanchiz et al., 2022) as such personalized cues have been shown to elicit greater cue reactivity compared to standardized, non-personalized cues (Conklin et al., 2010). While protocols have varied somewhat across studies (Vujanovic et al., 2018; Witteman et al., 2015), a two-session format is typically used. In a first lab-based session, a semi-structured interview developed by Sinha and Tuit (2012) to study the role of stress in addiction is used to obtain personalized details about a traumatic and a neutral event; these interviews are then used to develop standardized imagery cues for the script-driven imagery used in the second CRP session. The protocol for eliciting vivid imagery in the first session's interviews is based on Lang's (1979) theory of emotional imagery and is considered the gold standard in cue reactivity research (Coffey et al., 2002). These interviews are audio-recorded and later summarized into short and detailed standardized retellings of the events (also guided by the Sinha & Tuit (2012) protocol), which are then recorded and played for the participant in a the second CRP session where cue reactivity effects are studied.
While this two-session CRP protocol is valid and well-established in the trauma and addictions field (see review by DeGrace et al., 2022), high attrition rates (i.e., participants failing to return for the cue exposure session after the initial interview) are difficult to avoid (e.g., Coffey et al., 2006). This is especially important to consider in the context of trauma-exposed substance users with PTSD, as one symptom of PTSD is avoidance of trauma reminders (American Psychiatric Association [APA], 2013). Results may be less generalizable if our studies only reflect the experiences of those who are more likely to return to the second (CRP testing) session (e.g., less avoidant individuals). Additionally, obtaining results in a single session would minimize the overall distress to the participant. Moreover, the time and resources needed to run CRP studies in this traditional manner are demanding of both participant and researcher. Thus, a less demanding protocol would be a welcome methodological addition to the field, particularly when working with trauma-exposed individuals and those with PTSD.
Thus, this study served as a proof-of-concept to determine whether semi-structured interviews (Sinha & Tuit, 2012) alone could serve as an effective CRP. Specifically, we conducted an initial test of the construct validity of the semi-structured interviews as a form of CRP in terms of their ability to elicit theorized reactivity responses. Behavioral theory predicts that CRPs should elicit certain conditioned responses acquired through learning (Drummond, 2000; Reynolds & Monti, 2013). Thus, we reasoned that if the semi-structured interviews were valid as a CRP, they would elicit similar reactivity on response indices (i.e., substance craving, NA, PA) elicited by traditional CRP methodologies (see review by DeGrace et al., 2022). Such findings could provide researchers with a feasible means of conducting CRP studies with avoidant individuals without compromising their validity. Moreover, the use of the standardized Sinha and Tuit (2012) protocol for undertaking the interviews, which is published and readily accessible to researchers around the world, would allow for cue exposure replicability across future studies. Indeed, while interviews have been used as cues in some CRP studies (e.g., McGuire et al., 2018), the protocols for such interviews are often not described, which can create difficulties with replicability. We hypothesized that a semi-structured trauma interview, administered according to the protocol developed by Sinha and Tuit (2012), would elicit greater cannabis craving (H1), greater NA (H2), and lesser PA (H3) than a semi-structured neutral interview administered using the same protocol in a sample of individuals with trauma histories who use cannabis, and that the above effects would be stronger among participants with more severe PTSD symptoms (H4). Additionally, for the subset of participants who were drinkers, we expected that the trauma interview would elicit greater alcohol craving than the neutral interview (H5) demonstrating generalizability of the utility of the interview-based CRP across substances.
2 METHOD
2.1 Participants
Fifty1 participants (34% male; M [SD] age = 37.8 [10.02] years) living in the Halifax Regional Municipality in the Canadian province of Nova Scotia were recruited to participate in an in-person study investigating the relationship between past trauma exposure and cannabis use. Participants were recruited via posters, Veterans associations, clinics including an Operational Stress Injury (OSI) clinic, and on social media (e.g., Facebook). Participants were required to meet the following inclusion/exclusion criteria to be eligible: aged between 19 and 65 years; and no current diagnosis of a serious and persistent mental illness (i.e., bipolar disorder, schizophrenia, or other psychotic disorder). Participants were also required to report having been exposed to at least one lifetime traumatic event on the Life Events Checklist (LEC; Gray et al., 2004) and to report current regular cannabis use (at least 1 g per week for the last month; as in Gabrys & Porath, 2019). Sample characteristics, including substance use, can be found in Table 1.
| Demographic and clinical characteristics | N (%)/Mean (SD) | |
|---|---|---|
| Age (in years) | 37.8 (10.02) | |
| Sex | Male | 17 (34%) |
| Female | 33 (66%) | |
| Military status | Previous or current military | 10 (20%) |
| Civilian | 40 (80%) | |
| Cannabis use disorder status | None | 15 (30%) |
| Mild | 12 (24%) | |
| Moderate | 6 (12%) | |
| Severe | 17 (34%) | |
| Cannabis use disorder symptom severity | 3.72 (2.84) | |
| Past month PTSD | Present | 29 (58%) |
| Absent | 21 (42%) | |
| PTSD symptom severity | 10.52 (4.88) | |
| Primary trauma type | Interpersonal | 41 (82%) |
| Intrapersonal | 9 (18%) | |
| Past month substance use | Alcohol | 37 (74%) |
| Nicotine/Tobacco | 20 (40%) | |
| Hallucinogens | 2 (4%) | |
| Prescription stimulants | 5 (10%) | |
| Opiates | 1 (2%) | |
| Sedatives | 8 (16%) | |
| Prescribed psychiatric medication | Yes | 35 (70%) |
| No | 15 (30%) | |
- Note: Cannabis use disorder status and symptom count: Structured Clinical Interview for DSM-5 (SCID-5; First et al., 2015); Past month PTSD and PTSD symptom severity: Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2018); Trauma type: Life Events Checklist (LEC; Gray et al., 2004). Gender corresponded with sex in 98% of cases; thus, only sex is reported.
2.2 Measures: Eligibility
Trauma Exposure. The Life Events Checklist (LEC; Gray et al., 2004) was administered during a telephone eligibility screening. The LEC is a 17-item measure used to assess criterion A of a PTSD diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5; APA, 2013). If participants indicated they had been exposed to more than one lifetime trauma, they were instructed to focus on their most distressing lifetime trauma when answering questionnaires about the trauma, and in the semi-structured trauma interview.
2.3 Measures: Predictor
Semi-Structured Interviews. Both the neutral and trauma interviews were conducted following the protocol by Sinha and Tuit (2012) for creating detailed imagery-based scripts for use in stress and addiction research. Based on Lang's (1979) theory of emotional imagery, this protocol involves the “re-living” of the event through guided recall and imagery. To help elicit this imagery, the experimenter followed an interview guide (Sinha & Tuit, 2012) which provided sample probes to ensure that each participant was exposed to specific types of details about the event. However, as compared to a fully structured interview, the respondent was allowed to tell their story without substantial interruption and was only probed for details that they had not provided spontaneously during their event retelling. This semi-structured interview format allowed participants to become more immersed in details and tell their story naturally, with the prompts ensuring that all participants were exposed to similar details during the interview. Participants were asked to retell the event from their perspective and were probed for details throughout the interview to retrieve significant sensory aspects of the experience (e.g., the smell of smoke) as well as the participant's feelings and thoughts that occurred during the event (e.g., “I'm going to die”). These probed details focused on what the participant saw, heard, smelled, how they felt, which details stuck with them, and thoughts they were having at the time. Neutral events included those without substance use or stressful subject matter; researchers suggested describing an event that takes place during the participant's daily routine (e.g., morning routine, grocery shopping). These trauma and neutral interviews served as the CRP cues in the present study (i.e., the first within-subjects independent variable).
PTSD. PTSD symptom severity and the presence of current (past month) PTSD were assessed using the 20-item Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2018). We used continuous CAPS-5 scores (i.e., PTSD symptom count; possible range = 0–20) as a predictor of each cue reactivity outcome (i.e., the second within-subjects independent variable). Established CAPS-5 scoring rules (i.e., presence of at least one symptom for each of criteria B and C, and at least two symptoms for each of criteria D and E) were also used to determine the proportion of the sample meeting DSM-5 (APA, 2013) criteria for past-month PTSD for sample description purposes. The CAPS-5 possesses excellent interrater reliability, test-retest reliability, and high internal consistency (α = 0.88) (Weathers et al., 2018).
2.4 Measures: Outcomes
Cannabis Craving. The Marijuana Craving Questionnaire-Short Form (MCQ-SF; Heishman et al., 2009) is a 12-item (e.g., Smoking marijuana would be pleasant right now) measure of cannabis craving scaled from 1 (strongly disagree) to 7 (strongly agree) which assess the degree to which a participant is currently craving cannabis. The MCQ-SF has good convergent validity when compared to the original 47-item Marijuana Craving Questionnaire (Heishman et al., 2001). The MCQ-SF total score was used to assess cannabis craving—one of the main dependent variables in the current study (current study α = 0.93 and α = 0.94 for the neutral and trauma cues, respectively).
Alcohol Craving. A 0—100 Visual Analog Scale (VAS) was used as a single-item measure of alcohol craving, as in Coffey et al. (2006) and Vujanovic et al. (2018).
Affect. The Positive and Negative Affect Schedule-Short Form (PANAS-SF; Serafini et al., 2016) is a 20-item (10 NA items, 10 PA items) measure on which participants indicate the extent to which they are currently feeling NA-related (e.g., nervous, distressed) and PA-related (e.g., enthusiastic, proud) affective states on a scale from 1 (very slightly or not at all) to 5 (extremely). The PANAS-SF has good psychometric properties (i.e., excellent reliability (Crawford & Henry, 2004) and good convergent and discriminant validity (Serafini et al., 2016)). The PANAS-SF was used to assess NA (current study α = 0.90 and α = 0.81) and PA (current study α = 0.88 and α = 0.87) for the neutral and trauma cues, respectively.
2.5 Procedure
2.5.1 Screening
Individuals who expressed interest were contacted via telephone to assess their eligibility to participate. Respondents answered questions regarding demographic characteristics, the quantity and frequency of their cannabis use, and past trauma exposure (LEC-5; Gray et al., 2004) to ensure study eligibility. If eligible, they were booked for an in-person session. Participants were then sent a link to a virtual consent form and a battery of descriptive questionnaires.
2.5.2 Lab Session
A licensed psychiatrist and/or clinical psychologist was available on call during each lab session. Researchers interacting with participants were carefully trained and supervised. Participants were asked to abstain from cannabis, alcohol, and illicit drug use for 12 h, and caffeine for 2 h, prior to testing. At the beginning of the testing session, participants were screened verbally to ensure they had abstained from cannabis for 12 h prior to testing. Abstinence from all other substances was verified using a urine test and a breathalyzer. Participants were clinically assessed for PTSD symptoms with the CAPS-5 (Weathers et al., 2018). Then, their baseline affect, alcohol craving, and cannabis craving were assessed using the PANAS-SF (Serafini et al., 2016), alcohol craving VAS (Coffey et al., 2006), and the MCQ-SF (Heishman et al., 2009), respectively. Participants were then randomized to begin with either the neutral or trauma semi-structured interview, before completing the other interview (Sinha & Tuit, 2012). Immediately following each interview, participants completed the same measures of NA, PA, alcohol craving, and cannabis craving as at baseline, with instructions to respond according to how they were feeling during the interview.
2.5.3 Statistical Approach
A set of three linear mixed-effects models (R v. 4.2.1; lme4 package) was used to examine the effects of cue type (fixed effect; neutral vs. trauma) on cannabis craving (H1), NA (H2), and PA (H3) with the interactive effects of PTSD (H4) and on alcohol craving among drinkers (H5), respectively. Participants were inputted as a random effect to control for individual mean responses. We used the Nakagawa formula (Nakagawa & Schielzeth, 2013) and the Johnson (2014) expansion to calculate conditional and marginal R2 values (which served as a measure of effect size). Finally, a set of sensitivity analyses was conducted to ensure the effects persisted when covariates were controlled and when interactions were considered.
3 RESULTS
3.1 Sample characteristics
See Table 1 for a summary of demographic, clinical, and substance use characteristics of our sample. Bivariate correlations between outcome measures in each cue condition are shown in Table S1.
3.2 Hypothesis tests
See Table 2 for omnibus results of the main linear mixed-effects models.
| Estimate (b) | CI (95%) | p | |
|---|---|---|---|
| Outcome: Cannabis craving | Marginal R2 = 0.123/Conditional R2 = 0.936 | ||
| Condition (neutral = 0) | 0.94 | 0.48–1.40 | 0.001** |
| PTSD symptoms | 0.04 | −0.04 – 0.11 | 0.342 |
| Condition × PTSD symptoms | −0.00 | −0.04 – 0.04 | 0.952 |
| Outcome: Negative affect | Marginal R2 = 0.460/Conditional R2 = 0.922 | ||
| Condition (neutral = 0) | 5.71 | 2.24–9.19 | 0.002** |
| PTSD symptoms | 0.18 | −0.15 –0.50 | 0.289 |
| Condition × PTSD symptoms | 0.35 | 0.05–0.65 | 0.026* |
| Outcome: Positive affect | Marginal R2 = 0.175/Conditional R2 = 0.917 | ||
| Condition (neutral = 0) | −2.44 | −5.14–0.54 | 0.113 |
| PTSD symptoms | −0.59 | −0.95–0.23 | 0.002** |
| Condition × PTSD symptoms | 0.04 | −0.22–0.30 | 0.762 |
- *p < 0.05, **p < 0.01.
3.2.1 Cannabis craving
As hypothesized in H1, cannabis craving was significantly higher during the trauma than the neutral interview (t [99] = 4.01, p = 0.001, 95% CI [0.48–1.40]; see Figure 1). However, contrary to H4, there was no significant interaction between cue condition and PTSD symptom severity (t [99] = −0.60, 95% CI [−0.04–0.04]). Our model accounted for 12.3% of the variance (marginal R2) in cannabis craving scores (see Table 2).
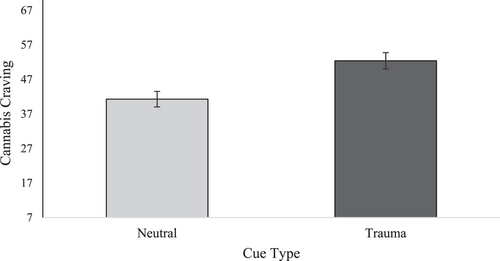
Average cannabis craving scores on the MCQ-SF across trauma versus neutral interview conditions. Error bars represent the standard error. MCQ-SF, Marijuana Craving Questionnaire—Short Form (Heishman et al., 2009).
3.2.2 Negative affect
As hypothesized in H2, NA scores were significantly higher during the trauma than the neutral interview (t [99] = 3.23, p = 0.002, 95% CI [2.24–9.18]; see Figure 2). Moreover, this main effect was qualified by the interactive effect of cue type and PTSD symptoms predicted in H4 (t [99] = 2.28, p = 0.027, 95% CI [0.05–0.65]) with the cue type effect stronger among those with higher PTSD symptom severity (see Figure 2). Our model accounted for 46.0% of the variance (marginal R2) in NA scores (see Table 2).
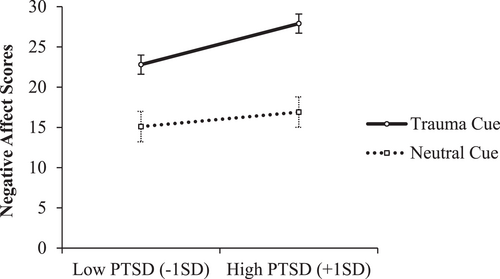
Interactive effect between PTSD and cue type (trauma vs. neutral) on negative affect. Error bars represent the standard error. Negative affect scores from the PANAS-SF, Positive and Negative Affect Schedule—Short Form (Serafini et al., 2016).
3.2.3 Positive affect
Contrary to H3 and H4, there was no main effect of cue type on PA (t [99] = −1.61, p = 0.11, 95% CI [−5.41–0.54]) and no interactive effect of cue type x PTSD symptoms ((t [99] = 0.30, p = 0.76, 95% CI [−0.22–0.30); however, a main effect of PTSD symptoms emerged (t [99] = −2.56, p = 0.013, 95% CI [−1.12–0.15] with lower PA among those with higher PTSD symptoms (see Figure 3). Our model accounted for 17.5% of the variance (marginal R2) in PA scores (see Table 2).
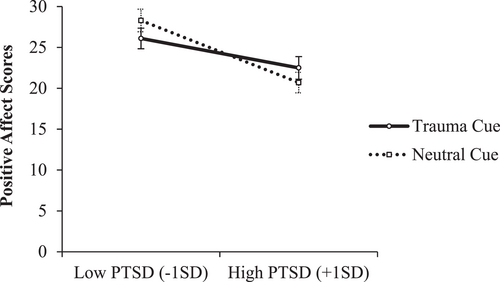
Interactive effect between PTSD and cue type (trauma vs. neutral) on positive affect. Error bars represent the standard error. Positive affect scores from the PANAS-SF, Positive and Negative Affect Schedule—Short Form (Serafini et al., 2016).
3.3 Sensitivity Analyses
First, we ran t-tests (and chi-square tests for categorical variables) to determine if sample characteristics, or baseline craving, NA, or PA differed by groups randomized to each order of cue presentation (trauma cue first (n = 29) versus neutral cue first (n = 21)). All tests were non-significant, suggesting there were no systematic differences in those randomized to the two cue presentation orders.
Second, we ran a supplementary linear mixed model (H5) examining the effect of cue type on alcohol craving to test if our results generalized beyond cannabis. We conducted this analysis only among those who reported being drinkers (n = 34) to avoid zero inflation and for conceptual reasons (as alcohol craving to trauma cues is only relevant among those participants who drink alcohol). The sample size of drinkers was too small to allow for a test of the interactive effects of cue type by PTSD symptoms, so we restricted this analysis to focus on cue type main effects. As hypothesized in H5, alcohol craving was significantly greater (M = 19.53) following the trauma cue (t [67] = 3.53, p = 0.001, 95% CI [4.32–15.62]) compared to the neutral cue (M = 9.56). The effect of our cue manipulation accounted for 4.00% of the variance (marginal R2) in our single-item index of alcohol craving.
Next, we re-ran our linear mixed models examining the effect of cue type on craving (H1) and affect (H2 & H3), with participants' baseline (pre-interview) levels of each respective outcome and the order of cue presentation controlled for. Cue order did not significantly predict NA or PA, nor cannabis craving. Moreover, in the case of all three outcome variables, baseline levels showed significant effects on the CRP outcome for cannabis craving (F [1, 47] = 166.47, p < 0.001), NA (F [1, 45] = 38.74, p < 0.001), and PA (F [1, 44.31] = 67.08, p < 0.001) with higher baseline levels predicting higher levels during the interview in each case. Nonetheless, a similar pattern of results emerged for our hypothesis tests as with our main analyses, even when these covariate effects were controlled. Specifically, cannabis craving (H1; t [99] = 3.95, p < 0.001, 95% CI [0.48–1.40]; Marginal R2 = 0.76) and NA (H2; t [99] = 3.07, p = 0.004, 95% CI [2.05–9.18]; Marginal R2 = 0.65) were significantly higher during the trauma (vs. neutral) interview. Additionally, our interaction between cue condition and PTSD symptoms for NA was retained (H4; t [99] = 2.21, p < 0.001, 95% CI [0.04–0.67]) despite the inclusion of these covariates. However, the main effect of PTSD symptoms for PA was no longer significant following inclusion of these covariates. The results of this set of sensitivity analyses generally supported the stability of our findings following control of potentially important covariates.
4 DISCUSSION
To begin to examine the construct validity of semi-structured interviews alone as a CRP among trauma-exposed current cannabis users, we conducted a proof-of-concept study measuring indices of cue reactivity commonly used in both the trauma and addictions literatures in response to both a trauma and neutral interview. Specifically, we measured self-reported cannabis craving, NA, and PA (and alcohol craving among the drinkers) using a semi-structured interview to elicit vivid imagery of the events of interest (Sinha & Tuit, 2012). Consistent with H1, H5, and H2, the trauma interview elicited significantly greater cannabis craving, alcohol craving (for the drinkers), and NA compared to the neutral interview. However, for NA, this main effect was qualified by the interactive effects of cue type and PTSD; consistent with H4, the cue condition effects on NA were stronger among those participants with more severe PTSD symptoms. Inconsistent with H3, there was no significant main effect of cue type on PA, and inconsistent with H4, no interaction of cue condition with PTSD symptoms on PA. Instead, a main effect of PTSD symptoms on PA emerged with those with more severe PTSD symptoms experiencing less positive affect than those with less severe PTSD symptoms regardless of interview type. Overall, the present results provide evidence of the construct validity for the use of the Sinha and Tuit (2012) interview protocol alone as a CRP (Reynolds & Monti, 2013) in that the trauma interview elicited greater substance craving and NA than the neutral interview.
These findings are consistent with prior research that utilized brief script-driven imagery audio cues (e.g., Rodriguez & Read, 2020), and a combination of audio and in vivo cues (e.g., Nosen et al., 2012) as CRP cues in populations of trauma-exposed substance users. Specifically, like studies that have utilized standardized script-driven audio and/or visual cues tested during a two-session protocol (see review by DeGrace et al., 2022), the single-session trauma interview used in the present study (Sinha & Tuit, 2012) provoked higher levels of cannabis craving and NA compared to the neutral interview. Moreover, the magnitude of effects was very similar in our study on our various outcomes to those obtained using a two-session protocol. For example, in a recent study, Berenz and colleagues (2021) measured craving during a combination of narrative imagery (neutral vs. trauma) and in vivo (water vs. alcohol) cue. The variance explained by their within-subjects narrative imagery cue type manipulation (Marginal R2 = 0.122) is comparable to the within-subjects interview cue type manipulation in the present study (Marginal R2 = 0.105) without the addition of PTSD to our model. Similarly, Nosen et al. (2012) reported the effects of a within-subjects narrative imagery cue (trauma vs. neutral) on PA and NA in combination with a neutral in vivo cue (i.e., water). Converted to R2, the proportions of variance in NA (R2 = 0.460) explained by their traditional CRP cue manipulation are similar to the proportions of variance in NA explained by the interview cue manipulation alone in our study (i.e., Marginal R2 = 0.391). Such results support the use of semi-structured interviews originally developed to elicit details for the later development of script-driven imagery as an appropriate cue to use themselves as a CRP.
To the authors' knowledge, this is the first proof-of-concept of a standardized interview method for cue exposure in trauma CRP studies. Indeed, while some prior work has utilized interviews as CRP cues (e.g., McGuire et al., 2018), standardization processes were not described. The present study provides evidence supporting a more feasible personalized CRP than the two sessions required for developing and administering personalized script-driven imagery, which would aid in reducing CRP study attrition (e.g., Coffey et al., 2006), particularly when studying avoidant populations like those with PTSD. Indeed, it is important to have a feasible protocol and representative samples in CRP research since this research has potentially important clinical implications. Specifically, CRPs can be used to study the antecedents of substance use and relapse, which may then inform the development and refinement of cue exposure treatments (Drummond, 2000).
There were some additional findings of note. Importantly, primary findings did not change in direction, significance, or magnitude when we controlled for order of cue presentation in sensitivity analyses, with the exception of losing significance of the main effect of PTSD symptoms on PA. Additionally, the effects of the interview cue manipulation were much stronger for NA than for PA, with respect to there being no main effect of cue type for PA and more variance accounted for in our NA model. Indeed, a pattern of ambivalence in PA responses to trauma cue exposure has been obtained in prior research using the gold standard brief personalized trauma versus neutral cues (e.g., Nosen et al., 2012) and suggests that the Sinha and Tuit (2012) trauma interview is primarily a NA induction. Finally, while we observed the expected interaction of cue type with PTSD symptoms for NA (H4), only cue type effects were evident for cannabis craving. The latter may have been due to our use of a total cannabis craving score rather than focusing on specific dimensions of craving that may be most reactive to trauma cue exposure in those with greater PTSD symptoms (Romero-Sanchiz et al., 2022).
While the findings of the present study are an important first step in validating the use of semi-structured standardized interviews following protocol by Sinha and Tuit (2012) in a single session, several methodological considerations should be noted. First, our sample was only comprised of individuals with trauma histories who use cannabis. While we did run a supplementary analysis on alcohol craving, these analyses were restricted to the subsample of drinkers and thus were underpowered for testing interactions with PTSD symptoms. Moreover, the sample was selected to be regular cannabis users, perhaps explaining the weaker effects of cue exposure for alcohol (vs. cannabis). Additionally, the single item nature of the alcohol craving measure compared to the multi-item cannabis craving measure may have introduced measurement error. Thus, we recommend further validation of our methodology a priori across other substance-using populations (e.g., alcohol, cocaine users) with multi-item craving measures, as traditional CRPs have been useful in studying this comorbidity in a variety of substance-using populations (Vujanovic et al., 2019). Second, our study assessed cannabis craving and affect. Future work should test the validity of this CRP method for other cue reactivity measures, such as cognitive reactions (e.g., attentional bias tasks) and physiological reactions (e.g., salivation). Third, the present findings are simply the first step in evaluating the validity of this CRP methodology. For example, reactivity elicited by the interviews was not directly compared to that elicited by gold standard methods (e.g., Coffey et al., 2006) within the same sample. Thus, convergent validity of the interviews has yet to be demonstrated; however, direct comparisons will always be confounded by potential order effects since the gold standard requires the interview to precede the briefer CRP session. Finally, while the proportion of variance in our outcomes explained by our manipulation was similar to that obtained in similar studies using traditional CRP methods (e.g., audio cues), we cannot assert full confidence that the interview achieves similar effects to other types of cue manipulations from these indirect comparisons alone. Future research should aim to quantify the magnitude of trauma cue-induced craving and affective responses across the literature to date to provide a more robust comparator for new CRP paradigms.
It is also important to note that our semi-structured interviews were not completely standardized. For example, because the interview protocol by Sinha and Tuit (2012) calls for the participant to tell their story in an uninterrupted fashion, interviews may vary in length and the degree of detail elicited. Furthermore, prompts from the researcher do not necessarily occur in a standardized order and not all prompts are required in every interview. Future research should compare the semi-structured interview to a more standardized version of the interview. Strict standardization might increase the magnitude of reactivity effects by ensuring imaginal exposure to all important sensory details. Alternatively, strict standardization might instead disrupt the flow of the interview, thus interrupting the participants' experience of reliving the event, possibly enough to dampen affective and/or craving responses to the cue. Moreover, in future, researchers may wish to establish the inter-rater reliability of this interview. Despite its limitations, the present study suggests that a single-session interview cue manipulation can elicit significant effects on cannabis craving, NA, and alcohol craving, the same effects that are obtained by procedures requiring at least two sessions (Berenz et al., 2021; Nosen et al., 2012).
ACKNOWLEDGMENTS
This work was supported through a Cannabis and Mental Health Catalyst Grant (Principal Investigator: SHS) from the Mental Health Commission of Canada and by a grant (Principal Investigator: SD) from the Nova Scotia Health Authority Research Fund. SD is supported by graduate studentships from the Chronic Pain Center of Excellence for Canadian Veterans' Capacity Building Initiative, the L’Oréal-UNESCO & France-Canada Research Fund for Women in Science Scholarship, and the Dalhousie Medical Research Foundation's MacQuarrie Neuroscience Research Graduate Studentship. TC was funded through a summer studentship from the Dalhousie University Department of Psychiatry Research Fund. PT is supported thru the Dr Paul Janssen Chair in Psychotic Disorders, Dalhousie University, Halifax, NS. SHS is supported through a Tier 1 Canada Research Chair in Addictions and Mental Health.
CONFLICT OF INTEREST STATEMENT
All authors note that they have no COIs to declare in relation to the work reported in this paper.
PREREGISTRATION
The protocol for this experiment was not preregistered in a public database prior to data collection.
REPORTING
We report how we determined our sample size, all data exclusions, all manipulations, and all measures in the study.
ETHICS STATEMENT
All measures and methods reported in this manuscript were approved by the Nova Scotia Health Research Ethics Board (ref #: 29820).
ENDNOTE
Open Research
DATA AVAILABILITY STATEMENT
The data, protocol, and REB approval for the present experiment is available via Open Science Framework (OSF): https://osf.io/t5uch/?view_only=3629e76e26614c0b943d25018c44cd18.