Complex reconstruction of the clavicle with a prefabricated medial femur condyle chimeric flap including a superficial circumflex iliac artery perforator flap: A case report
Abstract
The medial femur condyle (MFC) cortico-periosteal flap is a popular flap for bone reconstruction. The use of a chimeric version of this flap with a skin island has been described, but anatomical arterial variation can occur that prevent its harvest. Furthermore, the donor area of the skin paddle has been debated as poor because of the scarring in a visible area and because of the difficulty in obtaining pliable thin skin. We present a fabricated chimeric MFC cortico-periosteal flap joined with a superficial inferior epigastric perforator (SCIP) flap to reconstruct and augment a sclerotic and insufficient small clavicula with the skin paddle acting as a monitor and as a substitute for the overlying skin. A 52-year-old female patient had a history of multiple refractures of the right hypoplastic clavicle with a diameter of 7 mm, resulting in a sclerotic bone with a fibrotic scar. The reconstruction was done in one surgical session using a cortico-periosteal flap from the left medial condyle and a thin SCIP flap from the left groin. The area of the clavicle to be reconstructed was 3 cm, and the direct overlying skin (approximately 6 × 3 cm) was severely scarred and painful. The MFC flap was 5 × 4 cm, while the SCIP flap was 7 × 3.5 cm. The SCIP flap artery was anastomosed on the table end-to-side to the descending genicular (DG) artery of the MFC, and the vein was anastomosed end-to-end to a comitans vein of the DG artery. The flap fully survived after an initial congestion. At 12 months, we observed a satisfactory reconstruction of the clavicle with an enhanced diameter of 12 mm. The patient recovered full function of the shoulder with no pain. Using a fabricated chimeric flap composed of a medial femoral condyle and a superficial circumflex artery perforator flap may be an additional option for tailored reconstruction of complex osteo-cutaneous defect of clavicle.
1 INTRODUCTION
The reconstruction of complex or specific bone defects in the extremities might be challenging as it can include the need for simultaneous reconstruction of both the bone and the surrounding soft tissue, as well as the need to restore both blood flow and function to the affected area. One surgical option that has been developed to address these challenges is using chimeric flaps, which combine multiple tissue types to achieve the desired reconstructive goals. These flaps can be either pedicled or free, depending on the specific situation, and can be used to repair a wide variety of defects (Hallock, 1991, 2017).
The medial femur condyle (MFC) cortico-periosteal flap is a popular flap for bone reconstruction, and it is supplied by the descending genicular artery (DGA) or more rarely by the superior medial genicular artery (SMGA) (Del Pinal et al., 2007; Sakai et al., 1991). The use of a chimeric version of this flap with a skin island supplied by the saphenous branch (SB) has also been published (Gaggl et al., 2008; Hsu et al., 2018; Mehta et al., 2021; Pelzer et al., 2010), but anatomical variation can occur with the SB feeding the skin paddle being separated from the DGA or the main artery not having any consistent side branch in order to fabricate an osteo-cutaneous chimeric flap (Del Pinal et al., 2007). Furthermore, the donor area of the skin paddle of such a chimeric flap has been long debated as poor because of the usual bad scarring in a visible area and because of the difficulty in obtaining pliable thin skin (Acland et al., 1981; Karamursel & Celebioglu, 2006). The use of the MFC as a cortico periosteal flap for the reconstruction of the clavicle, is also been reported (Belyea et al., 2020; Fuchs et al., 2005).
We present a novel fabricated chimeric MFC cortico-periosteal flap combined with a superficial inferior epigastric perforator (SCIP) flap to reconstruct and augment a sclerotic and insufficient small clavicula that could not heal after multiple fractures, while also replacing the overlying skin. After revascularization of the flap, the skin acted as a monitor for the viability of the bone transfer.
According to the literature, there have been no reports of using a fabricated chimeric flap composed of a medial femoral condyle and a superficial circumflex artery perforator flap for reconstruction of the clavicle. In this communication, the authors aim to present this technique as an additional option for reconstructing complex osteo-cutaneous defects and as an alternative for tailored reconstruction.
2 CASE REPORT
A 52-year-old female patient otherwise healthy, sustained a fracture and then two refractures at the same location of the same right clavicula, the two refractures happening 1 year following fixation with a plate and shortly after removing the plates. The second refracture occurred just 7 days after plate removal, following a minor stress to the shoulder. Patient was then referred to our service.
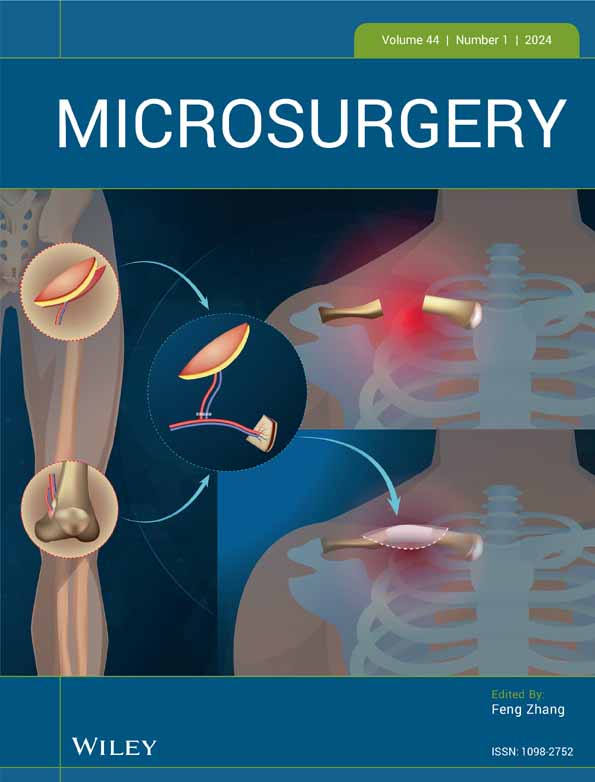
The preoperative CT scan demonstrated a sclerotic and hypoplastic clavicula with the smallest diameter of ca. 7 mm (normal reference 12 mm ± 1 mm). The patient exhibited an exceedingly thin and scarred skin, surpassing the visible scar boundary and primary visual inspection. Before the most recent re-fracture, the patient had already reported experiencing severe discomfort in the affected area, describing it as “unbearable discomfort” beneath the thin and scarred skin. In this case, the skin was resulting in localized discomfort, heightened sensitivity, and intolerance to cold. The scarring invaded the supraclavicular region to such an extent that the normal anatomy of the local vessels became questionable (Figure 1).
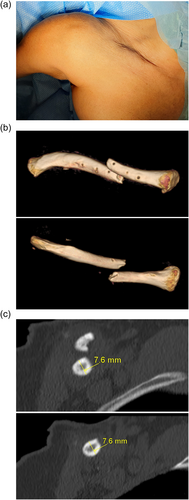
Our reconstruction was performed in one surgical time and divided into six steps. We excised the fibrotic scar and resected the clavicula bone stumps, which were extremely thin and sclerotic. We fixed the clavicula with an anterior six holes clavicula plate and five screws. We then prepared the thoraco-acromial artery and its vena comitans as donor vessels. The arteria transversa colli was not available. We harvested a cortico-periosteal flap from the left medial condyle of 5 × 4 cm: the feeding vessel was the DGA with a diameter of 2 mm, that appeared to be short and emerging from the superficial femoral very distally. As an important technical note, no other side branch was present between the emerging point of the DG artery from the superficial femoral artery and the first entry point into the medial femur condyle periosteum. The SA for a possible chimeric skin island, was separated from the DGA and emerged more proximally. We then harvested a 7 × 3.5 cm thin SCIP flap from the left groin based on the superficial branch with a pedicle of 5 cm. The diameter of the feeding artery at his section point was 1.2 mm. On the operating table, under the microscope, we created a lateral opening on the DG artery of the MFC flap and we anastomosed the SCIP artery to the artery of the MFC flap end to side. We then sutured the draining vein of the SCIP flap to one of the two comitans veins of the DG artery, end to end. The construct was then mounted in place: the cortico-periosteal part of the flap was loosely sutured around the clavicula creating a chamber and a free cancellous bone graft previously taken from the femur condyle, was inserted between the two clavicula stumps and between the periosteum flap and the clavicula. Then the skin paddle was sutured over the plate. The main pedicle (DGA) of the flap was then anastomosed end to end to the thoraco-acromial artery and its comitans vein (Figure 2).All anastomoses were performed with microsurgical technique under the operative microscope with 10.0 nylon. In the immediate postoperative time, the flap showed an initial congestion that resolved simply by further elevating the patient's thorax. The skin paddle then fully survived (Figure 3).


AT 12 months a CT scan demonstrated a completed reconstruction of the clavicula, with an enhanced diameter of 12 mm (Figure 4). The patient was satisfied with the functional result and had no deep or superficial pain. The patient did not request a plate removal but considered revision of the skin paddle for aesthetic reasons.
3 DISCUSSION
Chimeric or composite osteocutaneous flaps are often required to reconstruct composite defects including bone and the surrounding soft tissue, but also with the skin paddle of those flaps acting as “monitor” for the underlying vascularized reconstructed bone (Scaglioni et al., 2023).
We prefer the MFC as a vascularized bone reconstruction for limited bone defects as it has a minor donor site morbidity compared to Iliac crest and has a rate of success close to 100% (Guzzini et al., 2017). Some of the options available for chimeric flaps that include bone and skin, include the vascularized iliac crest, which has the disadvantage of having a short pedicle between the origin of the circumflex artery and the division between the skin vessel and the bone vessel. It has not been popularized as a periosteal flap only and the bone block might be more difficult to adapt to complex defects (Silva et al., 2018). The authors were concerned that, given the patient's small clavicle and general bone structure, utilizing a bone graft from the iliac crest might lead to an inadequate graft. Hence, the initial strategy was to acquire a sizable corticoperiosteal flap from the medial condyle of the femur and enhance it with cancellous graft to substantially augment the diameter of the reconstructed clavicle. On the other side and arguably, the fibula is mainly used for long bone consistent defects, and the skin that can be carried might be limited. Occasionally reports have shown that an osteocutaneous fibula is an option for clavicle reconstruction when a larger bone defect needs to be reconstructed (O'Neill et al., 2023).
The medial femur condyle (MFC) flap has been popularized as an alternative for microsurgical reconstruction of small and medium bone defects (Del Pinal et al., 2007; Sakai et al., 1991). Originally described as a periosteal flap, it has been used in the cortico-periosteal form for the reconstruction of long bones and successfully also for the clavicula (Belyea et al., 2020; Fuchs et al., 2005) and the scaphoid (Deng et al., 2020; Keating et al., 2021; Keller et al., 2020; Pet & Higgins, 2019). Its main advantages are the versatility and the possibility to customize the flap to irregular bones and the possibility to include cartilage as an osteochondral flap.
The medial (and the lateral) femur condyle can be harvested as a chimeric flap including skin, but the skin flap might be very bulky, and the lateral femur condyle has a very short and small feeding artery (Aribert et al., 2019; Gaggl et al., 2008; Hsu et al., 2018; Mehta et al., 2021; Pelzer et al., 2010). Furthermore, the skin of the thigh is not pliable, especially in Caucasians (Acland et al., 1981; Karamursel & Celebioglu, 2006). As it happened in our case, in the medial femur condyle, the feeding branch for the overlying skin, might be separated from the main vessel for the bone, therefore making impossible to harvest a conventional chimeric flap.
The superficial circumflex iliac artery perforator flap (SCIP) is a described option for upper limb reconstruction (Berner et al., 2020), and offers many advantages as the minor donor site morbidity and the possibility to customize it to many situations with its pliable skin and the possibility of thinning. The combination of these two flaps seemed to be successful and advantageous in our case for several reasons: it was possible to attach the SCIP flap artery to the DGA, at the most convenient location for our specific reconstruction configuration. The periosteal part of the flap could be harvested in abundant quantity, in order not only to reconstruct the clavicula, but also to enlarge its diameter. The skin provided by the SCIP flap was appropriately thinned to fit the contour of the skin of the clavicula, typically very thin. The SCIP flap acted with a dual role of monitor for the bony part of the flap and has a reconstructive tool for a retracted scar.
In the field of monitoring buried free flaps, numerous devices have been reported in the existing literature ranging from Dopplers to state of the art wireless implantable optical probes (Guo et al., 2022; Molitor et al., 2021a, 2021b). Among these devices, implantable Dopplers have gained significant popularity and may have been utilized in our specific case (Agha et al., 2014; Dunklebarger et al., 2022; Tabrizi et al., 2021). In our case skin replacement was required and we opted for the use of skin for both reconstructive purposes and for monitoring the deeper MFC. Nevertheless, it is important to note that implantable Dopplers, despite their relative widespread usage, are not without limitations as their low specificity, which can result in unnecessary revisions and potential vessel damage during removal. This last risk could have been particularly relevant when dealing with very small vessels like in our flap (Acland et al., 1981; Chang et al., 2016; Wax, 2014).
We find only quite not so similar cases in literature: a fabricated sequential flap with an anterolateral thigh flap and a medial femur condyle has been published for a complex case of wrist arthrodesis (Kurlander et al., 2019). On the other side, numerous cases of chimeric SCIP flap have been published but we could find only one case with a fabricated chimeric SCIP flap including the skin of the SCIP and a sartorius muscle (Yoshimatsu et al., 2017) for a skeletal reconstruction. With this case the authors further promote the use of “custom fabricated chimeric flaps” or “micro-engineered chimeric flaps,” which are created on the operating table using the best available tissue and donor sites for a specific reconstruction. This approach allows for multiple and unusual combinations of tissue transfer, tailored to the specific defect. This surgical approach of engineering flaps on the table, choosing the best donor site for a particular defect, has the potential to become a more common tool for the future reconstructive surgeon. The limitation is that there is currently no available mean to understand the boundaries in the size and numbers of different flaps that can be assembled to create the required reconstruction, depending on a single vessel and sometimes small vessel (Iorio et al., 2012; Silva et al., 2018). Using a fabricated chimeric flap composed of a medial femoral condyle and a superficial circumflex artery perforator flap may be an additional option for tailored reconstruction of complex osteo-cutaneous defect of clavicle.
CONFLICT OF INTEREST STATEMENT
None.
ACKNOWLEDGMENT
Open access funding provided by Universita della Svizzera italiana. We would like to extend our sincere gratitude to Dr. Christian Domenghini for his invaluable clinical insights that enhanced the quality of this report.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.