Plasma cell-free DNA methylome profiling in pre- and post-surgery oral cavity squamous cell carcinoma
Corresponding Author
Krupal B. Patel
Department of Head and Neck-Endocrine Oncology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Correspondence Krupal B. Patel, Moffitt Cancer Center, 12902 Magnolia Dr, Tampa, FL 33612.
Email: [email protected]
Xuefeng Wang, Moffitt Cancer Center, 12902 Magnolia Dr, MRC, Tampa, FL 33612.
Email: [email protected]
Search for more papers by this authorTapan A. Padhya
Otolaryngology–Head and Neck Surgery, University of South Florida Morsani College of Medicine, Tampa, USA
Search for more papers by this authorJinyong Huang
Department of Tumor Biology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorJuan C. Hernandez-Prera
Department of Pathology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorTingyi Li
Department of Biostatistics and Bioinformatics, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorChristine H. Chung
Department of Head and Neck-Endocrine Oncology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorLiang Wang
Department of Tumor Biology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorCorresponding Author
Xuefeng Wang
Department of Biostatistics and Bioinformatics, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Moffitt Cancer Center Immuno-Oncology Program, Tampa, Florida, USA
Correspondence Krupal B. Patel, Moffitt Cancer Center, 12902 Magnolia Dr, Tampa, FL 33612.
Email: [email protected]
Xuefeng Wang, Moffitt Cancer Center, 12902 Magnolia Dr, MRC, Tampa, FL 33612.
Email: [email protected]
Search for more papers by this authorCorresponding Author
Krupal B. Patel
Department of Head and Neck-Endocrine Oncology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Correspondence Krupal B. Patel, Moffitt Cancer Center, 12902 Magnolia Dr, Tampa, FL 33612.
Email: [email protected]
Xuefeng Wang, Moffitt Cancer Center, 12902 Magnolia Dr, MRC, Tampa, FL 33612.
Email: [email protected]
Search for more papers by this authorTapan A. Padhya
Otolaryngology–Head and Neck Surgery, University of South Florida Morsani College of Medicine, Tampa, USA
Search for more papers by this authorJinyong Huang
Department of Tumor Biology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorJuan C. Hernandez-Prera
Department of Pathology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorTingyi Li
Department of Biostatistics and Bioinformatics, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorChristine H. Chung
Department of Head and Neck-Endocrine Oncology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorLiang Wang
Department of Tumor Biology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Search for more papers by this authorCorresponding Author
Xuefeng Wang
Department of Biostatistics and Bioinformatics, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Moffitt Cancer Center Immuno-Oncology Program, Tampa, Florida, USA
Correspondence Krupal B. Patel, Moffitt Cancer Center, 12902 Magnolia Dr, Tampa, FL 33612.
Email: [email protected]
Xuefeng Wang, Moffitt Cancer Center, 12902 Magnolia Dr, MRC, Tampa, FL 33612.
Email: [email protected]
Search for more papers by this authorAbstract
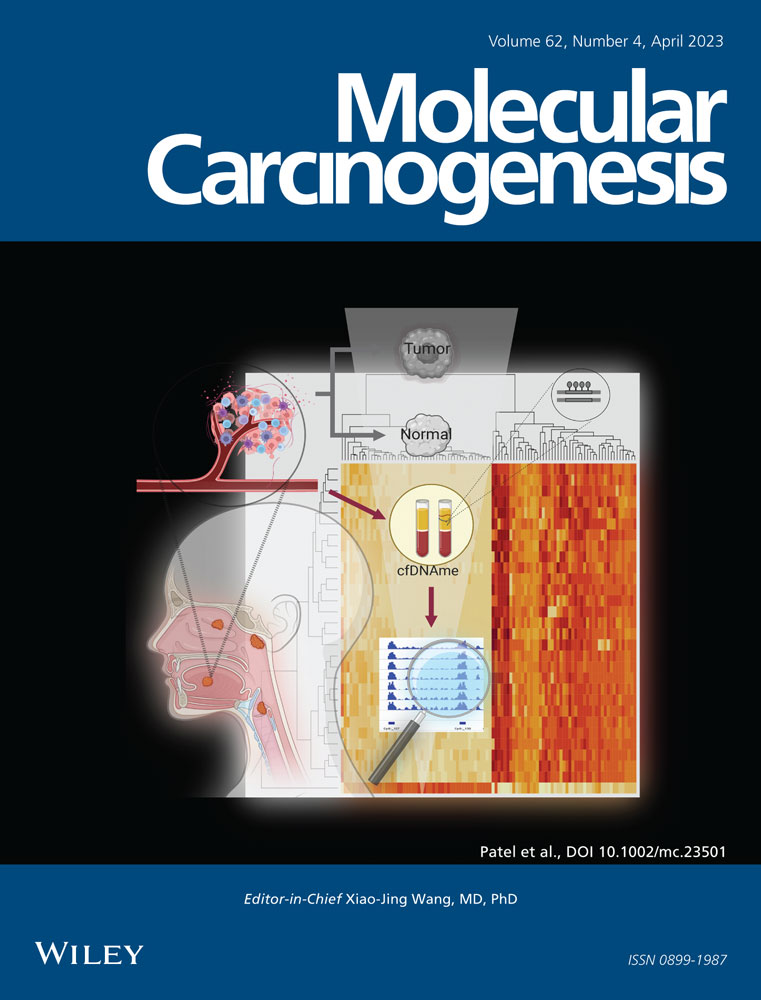
Head and neck squamous cell carcinoma (HNSCC), a highly heterogeneous disease that involves multiple anatomic sites, is a leading cause of cancer-related mortality worldwide. Although the utility of noninvasive biomarkers based on circulating cell-free DNA (cfDNA) methylation profiling has been widely recognized, limited studies have been reported so far regarding the dynamics of cfDNA methylome in oral cavity squamous cell carcinoma (OCSCC). It is hypothesized in this study that comparison of methylation profiles in pre- and postsurgery plasma samples will reveal OCSCC-specific prognostic and diagnostic biomarkers. As a strategy to further prioritize tumor-specific targets, top differential methylated regions (DMRs) were called by reanalyzing methylation data from paired tumor and normal tissue collected in the the cancer genome atlas head-neck squamous cell carcinoma (TCGA) head and neck cancer cohort. Matched plasma samples from eight patients with OCSCC were collected at Moffitt Cancer Center before and after surgical resection. Plasma-derived cfDNA was analyzed by cfMBD-seq, which is a high-sensitive methylation profiling assay. Differential methylation analysis was then performed based on the matched samples profiled. In the top 200 HNSCC-specific DMRs detected based on the TCGA data set, a total of 23 regions reached significance in the plasma-based DMR test. The top five validated DMR regions (ranked by the significance in the plasma study) are located in the promoter regions of genes PENK, NXPH1, ZIK1, TBXT, and CDO1, respectively. The genome-wide cfDNA DMR analysis further highlighted candidate biomarkers located in genes SFRP4, SOX1, IRF4, and PCDH17. The prognostic relevance of candidate genes was confirmed by survival analysis using the TCGA data. This study supports the utility of cfDNA-based methylome profiling as a promising noninvasive biomarker source for OCSCC and HNSCC.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Supporting Information
| Filename | Description |
|---|---|
| mc23501-sup-0001-Suppl_Figures.pdf933.1 KB | Supporting information. |
| mc23501-sup-0002-Suppl_Tables.xlsx164.8 KB | Supporting information. |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
- 1Klutstein M, Nejman D, Greenfield R, Cedar H. DNA methylation in cancer and aging. Cancer Res. 2016; 76: 3446-3450.
- 2Thierry AR, El Messaoudi S, Gahan PB, Anker P, Stroun M. Origins, structures, and functions of circulating DNA in oncology. Cancer Metastasis Rev. 2016; 35: 347-376.
- 3Diehl F, Schmidt K, Choti MA, et al. Circulating mutant DNA to assess tumor dynamics. Nature Med. 2008; 14: 985-990.
- 4Schwarzenbach H, Hoon DSB, Pantel K. Cell-free nucleic acids as biomarkers in cancer patients. Nat Rev Cancer. 2011; 11: 426-437.
- 5Jamal-Hanjani M, Wilson GA, Horswell S, et al. Detection of ubiquitous and heterogeneous mutations in cell-free DNA from patients with early-stage non-small-cell lung cancer. Ann Oncol. 2016; 27: 862-867.
- 6De Mattos-Arruda L, Weigelt B, Cortes J, et al. Capturing intra-tumor genetic heterogeneity by de novo mutation profiling of circulating cell-free tumor DNA: a proof-of-principle. Ann Oncol. 2014; 25: 1729-1735.
- 7Baylin SB, Esteller M, Rountree MR, Bachman KE, Schuebel K, Herman JG. Aberrant patterns of DNA methylation, chromatin formation and gene expression in cancer. Hum Mol Gen. 2001; 10: 687-692.
- 8Vrba L, Futscher BW. A suite of DNA methylation markers that can detect most common human cancers. Epigenetics. 2018; 13: 61-72.
- 9Constâncio V, Nunes SP, Henrique R, Jerónimo C. DNA methylation-based testing in liquid biopsies as detection and prognostic biomarkers for the four major cancer types. Cells. 2020; 9: 624.
- 10El Messaoudi S, Rolet F, Mouliere F, Thierry AR. Circulating cell free DNA: preanalytical considerations. Clin Chim Acta. 2013; 424: 222-230.
- 11Powrózek T, Krawczyk P, Kucharczyk T, Milanowski J. Septin 9 promoter region methylation in free circulating DNA-potential role in noninvasive diagnosis of lung cancer: preliminary report. Med Oncol. 2014; 31: 917.
- 12Song L, Yu H, Jia J, Li Y. A systematic review of the performance of the SEPT9 gene methylation assay in colorectal cancer screening, monitoring, diagnosis and prognosis. Cancer Biomarkers. 2017; 18: 425-432.
- 13Catarino R, Ferreira MM, Rodrigues H, et al. Quantification of free circulating tumor DNA as a diagnostic marker for breast cancer. DNA Cell Biol. 2008; 27: 415-421.
- 14Huang J, Soupir AC, Wang L. Cell-free DNA methylome profiling by MBD-seq with ultra-low input. Epigenetics. 2022; 17: 239-252.
- 15Lienhard M, Grimm C, Morkel M, Herwig R, Chavez L. MEDIPS: genome-wide differential coverage analysis of sequencing data derived from DNA enrichment experiments. Bioinformatics. 2014; 30: 284-286.
- 16Lienhard M, Grasse S, Rolff J, et al. QSEA—modelling of genome-wide DNA methylation from sequencing enrichment experiments. Nucleic Acids Res. 2017; 45:e44.
- 17Leon X, Quer M, Orus C, del Prado Venegas M, Lopez M. Distant metastases in head and neck cancer patients who achieved loco-regional control. Head Neck. 2000; 22: 680-686.
- 18Patel KB, Martin D, Zhao S, et al. Impact of age and comorbidity on survival among patients with oral cavity squamous cell carcinoma. Head Neck. 2021; 43(1): 268-277.
- 19Wang B, Zhang S, Yue K, Wang XD. The recurrence and survival of oral squamous cell carcinoma: a report of 275 cases. Chin J Cancer. 2013; 32: 614-618.
- 20Brands MT, Smeekens EAJ, Takes RP, et al. Time patterns of recurrence and second primary tumors in a large cohort of patients treated for oral cavity cancer. Cancer Med. 2019; 8: 5810-5819.
- 21Jeschke J, Bizet M, Desmedt C, et al. DNA methylation-based immune response signature improves patient diagnosis in multiple cancers. J Clin Invest. 2017; 127: 3090-3102.
- 22Carvalho L, Jeronimo C, Kim MM, et al. Evaluation of promoter hypermethylation detection in body fluids as a screening/diagnosis tool for head and neck squamous cell carcinoma. Clin Cancer Res. 2008; 14: 97-107.
- 23Mydlarz WK, Hennessey PT, Wang H, Carvalho AL, Califano JA. Serum biomarkers for detection of head and neck squamous cell carcinoma. Head Neck. 2016; 38: 9-14.
- 24Schröck A, Leisse A, de Vos L, et al. Free-circulating methylated DNA in blood for diagnosis, staging, prognosis, and monitoring of head and neck squamous cell carcinoma patients: an observational prospective cohort study. Clin Chem. 2017; 63: 1288-1296.
- 25Nakahara Y, Shintani S, Mihara M, Hino S, Hamakawa H. Detection of p16 promoter methylation in the serum of oral cancer patients. Int J Oral Maxillofac Surg. 2006; 35: 362-365.
- 26Sanchez-Cespedes M, Esteller M, Wu L, et al. Gene promoter hypermethylation in tumors and serum of head and neck cancer patients. Cancer Res. 2000; 60: 892-895.
- 27Danstrup CS, Marcussen M, Pedersen IS, Jacobsen H, Dybkær K, Gaihede M. DNA methylation biomarkers in peripheral blood of patients with head and neck squamous cell carcinomas. A systematic review. PLoS One. 2020; 15:e0244101.
- 28Ha PK, Califano JA. Promoter methylation and inactivation of tumour-suppressor genes in oral squamous-cell carcinoma. Lancet Oncol. 2006; 7: 77-82.
- 29Burgener JM, Zou J, Zhao Z, et al. Tumor-Naïve multimodal profiling of circulating tumor DNA in head and neck squamous cell carcinoma. Clin Cancer Res. 2021; 27: 4230-4244.
- 30Miller BF, Petrykowska HM, Elnitski L. Assessing ZNF154 methylation in patient plasma as a multicancer marker in liquid biopsies from colon, liver, ovarian and pancreatic cancer patients. Sci Rep. 2021; 11: 221.
- 31Anderson BW, Suh YS, Choi B, et al. Detection of gastric cancer with novel methylated DNA markers: discovery, tissue validation, and pilot testing in plasma. Clin Cancer Res. 2018; 24: 5724-5734.
- 32Bach S, Sluiter NR, Beagan JJ, et al. Circulating tumor DNA analysis: clinical implications for colorectal cancer patients. A systematic review. JNCI Cancer Spectrum. 2019; 3:pkz042.
- 33Young GP, Symonds EL, Nielsen HJ, et al. Evaluation of a panel of tumor-specific differentially-methylated DNA regions in IRF4, IKZF1 and BCAT1 for blood-based detection of colorectal cancer. Clin Epigenetics. 2021; 13: 14.
- 34Wang Y, Yu Y, Ye R, et al. An epigenetic biomarker combination of PCDH17 and POU4F2 detects bladder cancer accurately by methylation analyses of urine sediment DNA in han Chinese. Oncotarget. 2016; 7: 2754-2764.
- 35Grimwood J, Gordon LA, Olsen A, et al. The DNA sequence and biology of human chromosome 19. Nature. 2004; 428: 529-535.
- 36Lleras RA, Adrien LR, Smith RV, et al. Hypermethylation of a cluster of Krüppel-type zinc finger protein genes on chromosome 19q13 in oropharyngeal squamous cell carcinoma. Am J Pathol. 2011; 178: 1965-1974.
- 37Lleras RA, Smith RV, Adrien LR, et al. Unique DNA methylation loci distinguish anatomic site and HPV status in head and neck squamous cell carcinoma. Clin Cancer Res. 2013; 19: 5444-5455.
- 38Gaykalova DA, Vatapalli R, Wei Y, et al. Outlier analysis defines zinc finger gene family DNA methylation in tumors and saliva of head and neck cancer patients. PLoS One. 2015; 10:e0142148.
- 39Eisenbeis CF, Singh H, Storb U. Pip, a novel IRF family member, is a lymphoid-specific, PU.1-dependent transcriptional activator. Genes Dev. 1995; 9: 1377-1387.
- 40Nam S, Lim JS. Essential role of interferon regulatory factor 4 (IRF4) in immune cell development. Arch Pharmacal Res. 2016; 39: 1548-1555.
- 41Wong RWJ, Tan TK, Amanda S, et al. Feed-forward regulatory loop driven by IRF4 and NF-κB in adult T-cell leukemia/lymphoma. Blood. 2020; 135: 934-947.
- 42Li X, Zhai S, Zhang J, et al. Interferon regulatory factor 4 correlated with immune cells infiltration could predict prognosis for patients with lung adenocarcinoma. Front Oncol. 2021; 11:698465.
- 43Theveneau E, Mayor R. Cadherins in collective cell migration of mesenchymal cells. Curr Opin Cell Biol. 2012; 24: 677-684.
- 44Lin Y, Li Z, He Z, Guan T, Ma J. Clinical and prognostic significance of protocadherin-10 (PCDH10) promoter methylation in bladder cancer. J Int Med Res. 2012; 40: 2117-2123.
- 45Haruki S, Imoto I, Kozaki K, et al. Frequent silencing of protocadherin 17, a candidate tumour suppressor for esophageal squamous cell carcinoma. Carcinogenesis. 2010; 31: 1027-1036.
- 46Hu X, Sui X, Li L, et al. Protocadherin 17 acts as a tumour suppressor inducing tumour cell apoptosis and autophagy, and is frequently methylated in gastric and colorectal cancers. J Pathol. 2013; 229: 62-73.
- 47Wang XB, Lin YL, Li ZG, Ma JH, Li J, Ma JG. Protocadherin 17 promoter methylation in tumour tissue from patients with bladder transitional cell carcinoma. J Int Med Res. 2014; 42: 292-299.
- 48Tegeder I, Geisslinger G. Opioids as modulators of cell death and survival—unraveling mechanisms and revealing new indications. Pharmacol Rev. 2004; 56: 351-369.
- 49McLaughlin PJ, Stucki JK, Zagon IS. Modulation of the opioid growth factor ([Met(5)]-enkephalin)-opioid growth factor receptor axis: novel therapies for squamous cell carcinoma of the head and neck. Head Neck. 2012; 34: 513-519.
- 50Suzuki M, Chiwaki F, Sawada Y, et al. Peripheral opioid antagonist enhances the effect of anti-tumor drug by blocking a cell growth-suppressive pathway in vivo. PLoS One. 2015; 10:e0123407.
- 51Roperch JP, Incitti R, Forbin S, et al. Aberrant methylation of NPY, PENK, and WIF1 as a promising marker for blood-based diagnosis of colorectal cancer. BMC Cancer. 2013; 13: 566.
- 52Salhia B, Kiefer J, Ross JTD, et al. Integrated genomic and epigenomic analysis of breast cancer brain metastasis. PLoS One. 2014; 9:e85448.
- 53Zagon IS, Smith JP, McLaughlin PJ. Human pancreatic cancer cell proliferation in tissue culture is tonically inhibited by opioid growth factor. Int J Oncol. 1999; 14: 577-584.
- 54Zhang H, Yu Z, Wu B, Sun F. PENK inhibits osteosarcoma cell migration by activating the PI3K/Akt signaling pathway. J Orthop Surg. 2020; 15: 162.
- 55Zhang Y, Fang L, Zang Y, Xu Z. Identification of core genes and key pathways via integrated analysis of gene expression and DNA methylation profiles in bladder cancer. Med Sci Monit. 2018; 24: 3024-3033.
- 56Missler M, Südhof TC. Neurexophilins form a conserved family of neuropeptide-like glycoproteins. J Neurosci. 1998; 18: 3630-3638.
- 57Faryna M, Konermann C, Aulmann S, et al. Genome-wide methylation screen in low-grade breast cancer identifies novel epigenetically altered genes as potential biomarkers for tumor diagnosis. FASEB J. 2012; 26: 4937-4950.
- 58Wu X, Lv D, Lei M, et al. A 10-gene signature as a predictor of biochemical recurrence after radical prostatectomy in patients with prostate cancer and a Gleason score >/=7. Oncol Lett. 2020; 20: 2906-2918.
- 59Jin JS. The detection of tumor location and lymph node metastasis by aberrant NXPH1 and NXPH2 expressions in pancreatic ductal adenocarcinomas. Chin J Physiol. 2016; 59: 348-354.
- 60Decock A, Ongenaert M, Cannoodt R, et al. Methyl-CpG-binding domain sequencing reveals a prognostic methylation signature in neuroblastoma. Oncotarget. 2016; 7: 1960-1972.
- 61Xia Y, Li X, Tian X, Zhao Q. Identification of a five-gene signature derived from MYCN amplification and establishment of a nomogram for predicting the prognosis of neuroblastoma. Front Mol Biosci. 2021; 8:769661.
- 62Imajyo I, Sugiura T, Kobayashi Y, et al. T-box transcription factor Brachyury expression is correlated with epithelial-mesenchymal transition and lymph node metastasis in oral squamous cell carcinoma. Int J Oncol. 2012; 41: 1985-1995.
- 63Roselli M, Fernando RI, Guadagni F, et al. Brachyury, a driver of the epithelial-mesenchymal transition, is overexpressed in human lung tumors: an opportunity for novel interventions against lung cancer. Clin Cancer Res. 2012; 18: 3868-3879.
- 64Palena C, Polev DE, Tsang KY, et al. The human T-box mesodermal transcription factor Brachyury is a candidate target for T-cell-mediated cancer immunotherapy. Clin Cancer Res. 2007; 13: 2471-2478.
- 65Pinto F, Pértega-Gomes N, Pereira MS, et al. T-box transcription factor brachyury is associated with prostate cancer progression and aggressiveness. Clin Cancer Res. 2014; 20: 4949-4961.
- 66Cottone L, Cribbs AP, Khandelwal G, et al. Inhibition of histone H3K27 demethylases inactivates brachyury (TBXT) and promotes chordoma cell death. Cancer Res. 2020; 80: 4540-4551.
- 67Hamilton DH, David JM, Dominguez C, Palena C. Development of cancer vaccines targeting brachyury, a transcription factor associated with tumor epithelial-mesenchymal transition. Cells Tissues Organs. 2017; 203: 128-138.