Prognostic Factors in Pediatric Early Liver Retransplantation
Abstract
The most common indications for early liver retransplantation (eRe-LT) are vascular complications and primary nonfunction (PNF). These patients are usually in a critical clinical condition that can affect their chances of survival. In fact, the survival of these patients is usually lower compared with the patients undergoing a first transplant. To the best of our knowledge, no specific series of pediatric patients undergoing eRe-LT has been published to date. Therefore, the aim of this study is to report the results of eRe-LT and to analyze factors potentially related to success or failure. Our work is of a retrospective cohort study of patients who underwent eRe-LT at the Juan P. Garrahan Pediatric Hospital of Buenos Aires, Argentina, between May 1995 and December 2018 (n = 60). Re-LT was considered early when performed ≤30 days after the previous LT. A total of 40 (66.7%) patients were enrolled due to vascular causes and 20 (33.3%) were enrolled because of PNF. Of all the relisted patients, 36 underwent eRe-LT, 14 died on the waiting list, and 10 recovered without eRe-LT. A total of 23 (63.9%) patients died after eRe-LT, most of them due to infection-related complications. Survival rates at 1 and 5 years were 42.4% and 33.9%, respectively. On univariate logistic regression analysis, Pediatric End-Stage Liver Disease (PELD)/Model for End-Stage Liver Disease (MELD) scores, transplant era, and advanced life support at eRe-LT were found to be related to 60-day mortality. However, on multivariate analysis, era (odds ratio [OR], 9.3; 95% confidence interval [CI], 1.19-72.35; P = 0.033) and PELD/MELD scores (OR, 1.07; 95% CI, 1-1.14; P = 0.036) were significantly associated with 60-day patient mortality. This study found that the level of acuity before retransplant, measured by the requirement of advanced life support and the PELD/MELD score at eRe-LT, was significantly associated with the chances of post–eRe-LT patient survival.
Abbreviations
-
- AUROC
-
- area under the receiver operating characteristic curve
-
- BMI
-
- body mass index
-
- CI
-
- confidence interval
-
- eRe-LT
-
- early liver retransplantation
-
- LDLT
-
- living donor liver transplantation
-
- LT
-
- liver transplantation
-
- MELD
-
- Model for End-Stage Liver Disease
-
- OR
-
- odds ratio
-
- PELD
-
- Pediatric End-Stage Liver Disease
-
- PNF
-
- primary nonfunction
-
- SD
-
- standard deviation
Liver transplantation (LT) has been the standard of care for end-stage liver disease, acute liver failure, and some inborn errors of metabolism over the last decades. Urgent liver retransplantation may be the only therapeutic option when the graft fails in the early posttransplant period, and it accounts for 10%-43% of pediatric and 52% of adult re-LT series worldwide.1-3 Patients who face an urgent re-LT are typically in a critical clinical condition that may affect their chances for survival. Although the results of re-LT have improved over time, much lower patient survival rates are still consistently reported for re-LT when compared with a first graft LT.4-6
The most common indications for early liver retransplantation (eRe-LT) are vascular complications and primary nonfunction (PNF). In children, different studies have evaluated factors related to re-LT success or failure, in the majority of cases combining early and late re-LT. Nevertheless, from the clinical point of view, there is a difference between these 2 conditions, complicating the analysis of series that combine the evaluation of both types of retransplantation.7-10
In the current context of organ scarcity, it is highly relevant to analyze the results of re-LT in a highly complex condition such as an early graft failure, looking for prognostic factors of success or failure in pediatric eRe-LT. To the best of our knowledge, no specific series of pediatric patients undergoing eRe-LT has been published to date. Therefore, the aim of this study is to report the results of eRe-LT and to analyze factors potentially related to success or failure in a high-volume pediatric LT unit.
Patients and Methods
- Emergency transplant for patients with acute liver failure or in need of acute re-LT (hepatic artery thrombosis <7 days after LT or primary liver graft nonfunction).
- The Pediatric End-Stage Liver Disease (PELD)/Model for End-Stage Liver Disease (MELD) system for patients with chronic liver disease.11
Population
This is a single-center retrospective cohort study of patients who underwent eRe-LT at the Juan P. Garrahan Pediatric Hospital of Buenos Aires, Argentina, between May 1995 and December 2018. Re-LT was considered early when performed ≤30 days after the previous LT. Additionally, outcomes of all patients who were relisted in emergency status (re-LT, death on the waiting list, or recovery) were reviewed.
Variables
Recipient variables were age, sex, primary diagnosis, diagnosis at previous transplant, weight, malnutrition (defined as a standard deviation [SD] z score <2 for weight or height),12 cause of graft failure, PELD/MELD score at re-LT, interval time to eRe-LT, need for advanced life support at the time of re-LT, and transplant era.
Donor and technical variables included in the analysis were donor age, sex, body mass index (BMI), whole versus technical variant graft, living versus cadaveric donor, cold ischemia time, need for vascular grafts at re-LT, blood transfusion volume, and operative time.
Allograft PNF was defined as early graft failure in the absence of vascular complications. Vascular causes of early graft failure, including hepatic artery, portal vein, or hepatic vein thrombosis, were confirmed by arteriography, computed tomography angiography, or surgery. The need for advanced life support was defined as vasopressor support, mechanical ventilation, and/or renal replacement therapy at the time of eRe-LT.
The transplant era was divided into 2 periods (May 1995 to December 2009 and January 2009 to December 2018) on the basis of structural changes in our program with a previously confirmed effect on overall posttransplant outcomes. Some of the changes included a new tacrolimus-based immunosuppressive scheme and a shift to a modern intensive care unit, specifically for the immunosuppressed population. Also, changes in vascular reconstruction techniques (arterial and portal) and thrombosis prophylaxis protocols were implemented during era 2. However, it should be noted that the division of eras is estimated, considering that changes were introduced gradually and dynamically.
Endpoints
The primary endpoint for patients who underwent eRe-LT was 60-day post–eRe-LT patient mortality. Early mortality was selected as a main endpoint because almost 90% of the post–eRe-LT deaths occurred in that period. The secondary endpoint was the outcomes for the overall urgently re-enlisted population, considering the rates of wait-list mortality, eRe-LT, or recovery without transplantation.
Statistical Analysis
Continuous variables and categorical variables were expressed as median (range) and percentages, respectively. Correlation between the variables and primary outcome (60-day post–eRe-LT mortality) was analyzed using logistic regression. Variables that demonstrated a P value of 0.1 or less at univariate analysis were manually entered in a multiple logistic regression model. The final model retained variables that were found to have a P value <0.05 in the multivariate analysis or those that were considered clinically relevant. Calibration and discriminative properties of the final model were evaluated using the Hosmer-Lemeshow test and the area under the receiver operating characteristic curve (AUROC), respectively. Patient survival in time and its association with the relevant variables are reported using Kaplan-Meier estimates, and the influence of the relevant variables was assessed with the log-rank test. All statistical analyses were performed using Stata, version 12.0 (StataCorp, College Station, TX).
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors. No informed consent has been collected because it was a retrospective study.
Results
Early Relist and Acute Retransplant Rates and Wait-List Outcomes
From 1992 to 2018, 811 LTs were performed at our hospital. A total of 60 (7.4%) patients were relisted for eRe-LT. A total of 40 (66.7%) patients were enrolled due to vascular causes, and 20 (33.3%) were enrolled because of PNF. Global rates of early vascular thrombosis and PNF requiring emergency relisting were 4.9% and 2.4%, respectively. Between 1992 and 1995, there were no early retransplants.
Of all the relisted patients, 36 (60.0%) underwent eRe-LT, 14 (23.3%) died on the waiting list, and 10 (16.7%) recovered without eRe-LT (Fig. 1).
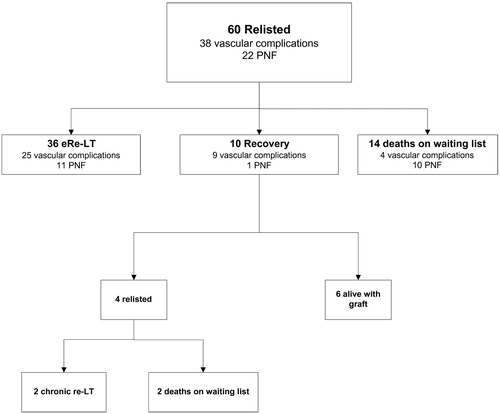
Retransplant Population: Donor and Surgical Characteristics
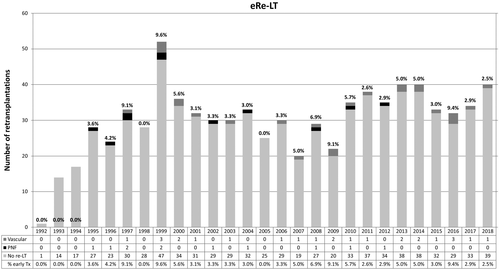
Overall, 36 patients underwent re-LT in the early posttransplantation period. The annual rates of urgent re-LT are shown in Fig. 2. A total of 33 patients received second grafts, and 3 received third grafts. All third graft re-LTs were in cases of graft failure due to PNF following a late re-LT. Median age at previous transplantation was 1.3 years (range, 0.6-14 years). The features of the patients who underwent eRe-LT are detailed in Table 1.
| Characteristics | Values (n = 36) |
|---|---|
| Age at retransplant, years | 1.3 (0.6-14) |
| Sex | |
| Female | 22 (61.1) |
| Male | 14 (38.9) |
| Primary diagnosis | |
| Cholestatic liver disease | 20 (55.6) |
| Acute liver failure | 11 (30.6) |
| Autoimmune hepatitis | 2 (5.5) |
| Malignancy | 2 (5.5) |
| Other cirrhosis | 1 (2.8) |
| Weight, kg | 9.5 (5-49) |
| Weight <10 kg | 18 (50) |
| Malnutrition (<2 SD z score) | 23 (63.9) |
| Retransplantation era | |
| 1995-2009 | 22 (61.1) |
| 2010-2018 | 14 (38.9) |
| Reason for retransplantation | |
| Vascular complications | 25 (69.4) |
| PNF | 11 (30.6) |
| Graft number | |
| Second graft | 33 (91.7) |
| Third graft* | 3 (8.3) |
| Days since previous transplantation | 8.5 (0-27) |
| Days since previous transplantation to relisting | 4.5 (0-27) |
| PELD score at time of retransplantation | 20 (0-61) |
| Advanced life support at retransplantation | 24 (66.7) |
| Vasopressor support | 19 (52.8) |
| Mechanical ventilation | 17 (47.2) |
| Renal replacement therapy | 5 (13.9) |
NOTE:
- Data are given as median (range) or n (%).
- * Only the last graft was due to acute retransplantation.
The most common primary diagnosis was cholestatic liver disease (55.6%), followed by acute liver failure (30.6%). The causes of early failure of the previous graft were vascular complications in 70% and PNF in 30%. Median time between the first transplantation and eRe-LT was 8.5 days (range, 0-27 days). All patients were hospitalized at the time of eRe-LT; 78% were in the ICU; and 66.7% required advanced life support at the time of eRe-LT.
Surgical and donor variables are summarized in Table 2. For early retransplantation allografts, 16.7% were whole grafts, whereas 83.4% were technical variant grafts. Two (5.5%) of the grafts were from living related donors. Median cold ischemia time was 420 minutes (range, 138-720 minutes). Of the recipients, 83% received massive transfusion during the retransplantation (defined as the transfusion of blood components equaling 1 or more total blood volumes within a 24-hour time frame or half of a blood volume in 12 hours). Median donor age was 22.5 years (range, 1-58 years), and median BMI was 23.4 kg/m2 (range, 11-30 kg/m2).
| Previous Transplantation (n = 36) | Early Retransplantation (n = 36) | |
|---|---|---|
| Donor variables | ||
| Age, years | 22 (1-52) | 22.5 (1-58) |
| Sex | ||
| Female | 20 (55.6) | 15 (41.7) |
| Male | 16 (44.4) | 21 (58.3) |
| BMI, kg/m2 | 23.3 (11-30) | 23.4 (11-30) |
| Recipient variables | ||
| Graft type | ||
| Whole graft | 10 (27.8) | 6 (16.7) |
| Reduced | ||
| Sections 2 and3 | 5 (13.9) | 16 (44.4) |
| Sections 2-4 | 1 (2.8) | 0 |
| Sections 1-4 | 0 | 2 (5.5) |
| Split (sections 2 and 3) | 4 (11.1) | 10 (27.8) |
| LDLT (sections 2 and 3) | 16 (44.4) | 2 (5.5) |
| Technical variant graft | ||
| Living donor | 16 (44.4) | 2 (5.5) |
| Deceased donor | 20 (55.6) | 34 (94.4) |
| Cold ischemia time, minutes | 340 (85-733) | 420 (138-720) |
| Operative time, minutes | 622 (330-1410) | 420 (300-750) |
| Vascular graft | 13 (36.1) | 21 (58.3) |
| Arterial graft | 7 (19.4) | 20 (55.6) |
| Portal graft | 6 (16.7) | 1 (2.8) |
NOTE:
- Data are given as median (range) or n (%).
Retransplantation Outcomes
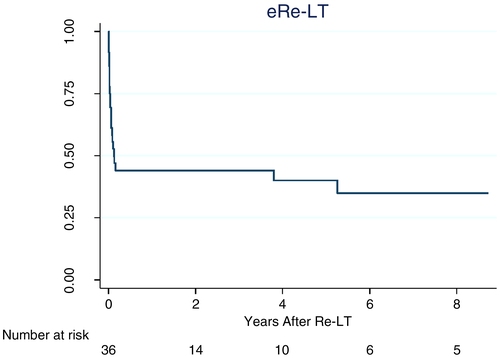
Overall, 23 of 36 (63.9%) patients died after eRe-LT. Of the 23 patients who died, 20 (87%) died within the first 60 days after re-LT. The most common causes of death were infection-related complications (Table 3). Kaplan-Meier survival estimates for the 36 eRe-LT patients are shown in Fig. 3. The 1- and 5-year patient survival rates were 42.4% and 33.9%, respectively.
| Vascular Complications (n = 25) | PNF (n = 11) | |
|---|---|---|
| Deaths | 13 (52) | 10 (90.9) |
| Survival after re-LT, days | 22.5 | 20 |
| Causes | ||
| Disseminated sepsis by a multiresistant microorganism | 9 (69.2) | 7 (70) |
| Coagulopathy | 0 | 3 (30) |
| Graft dysfunction | 4 (30.7) | 0 |
NOTE:
- Data are given as n (%).
On univariate logistic regression analysis, PELD/MELD scores, transplant era, advanced life support at eRe-LT, and PNF versus vascular cause for eRe-LT were found to be related to 60-day mortality (Table 3).
Patients of era 1 and era 2 were compared in terms of age, weight, cause of retransplantation (vascular versus primary failure), life support, and PELD score at the time of retransplantation. We did not find statistically significant differences in any of the variables mentioned among the retransplanted patients in era 1 versus era 2.
The trend toward a decrease in the percentage of primary failure as a cause of retransplantation in era 2 versus era 1 was not significant (14% versus 41% respectively; P = 0.09).
On multivariate analysis, 2 variables were significantly associated with 60-day patient mortality: era 1 versus era 2 (odds ratio [OR], 9.3; 95% confidence interval [CI], 1.19-72.35; P = 0.03) and PELD/MELD score (OR, 1.07; 95% CI, 1-1.14; P = 0.04). Advanced life support at eRe-LT showed an association that was very close to significant (OR, 7.81; 95% CI, 0.95-63.96; P = 0.05) (Table 4) and was retained in the final model because of a clear improvement in calibration and discrimination properties upon inclusion. A final model including these 3 variables showed adequate calibration (Hosmer Lemeshow test P = 0.4) and discrimination (AUROC, 0.9).
| Variable | Univariate Logistic Regression (n = 36) | Multiple Logistic Regression (n = 36) | ||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Age at previous transplant | 0.99 (0.83-1.18) | 0.96 | ||
| Urgency status for a previous transplant | 2.88 (0.62-13.5) | 0.17 | ||
| Nonwhole graft for a previous transplant | 1.36 (0.32-5.89) | 0.68 | ||
| Prior LDLT | 1.05 (0.28-3.95) | 0.94 | ||
| Any vascular graft prior to transplant | 2 (0.47-8.46) | 0.47 | ||
| Number of previous re-LT laparotomies | 1.57 (0.76-3.27) | 0.21 | ||
| Age at eRe-LT | 0.98 (0.83-1.18) | 0.90 | ||
| Weight at eRe-LT | 0.98 (0.93-1.05) | 0.70 | ||
| Weight at re-LT <10 kg | 2.5 (0.65-9.65) | 0.18 | ||
| Malnutrition | 1.11 (0.28-4.37) | 0.87 | ||
| Era of eRe-LT | 6.66 (1.5-29.63) | 0.013 | 9.3 (1.2-72.35) | 0.033 |
| PELD/MELD score at re-LT | 1.09 (1.03-1.17) | 0.004 | 1.07 (1.01-1.15) | 0.036 |
| PNF | 5.72 (1.02-32.1) | 0.047 | ||
| Donor age | 0.99 (0.95-1.04) | 0.72 | ||
| Donor BMI at re-LT | 0.84 (0.69-1.03) | 0.10 | ||
| Nonwhole graft at re-LT | 0.57 (0.09-3.61) | 0.55 | ||
| Any graft at re-LT | 0.40 (0.1-1.71) | 0.22 | ||
| Cold ischemia time at re-LT | 0.99 (0.99-1.001) | 0.09 | ||
| Operative time at re-LT | 0.99 (0.99-1.01) | 0.98 | ||
| Life support at re-LT | 14.99 (2.54-88.7) | 0.03 | 7.81 (0.95-63.96) | 0.055 |
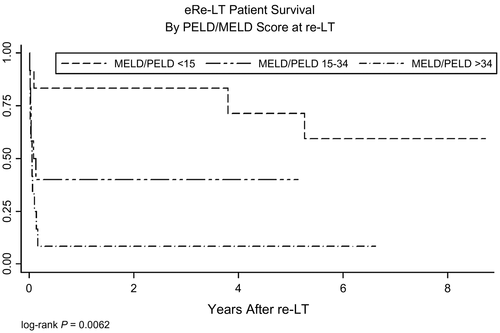
PELD/MELD score alone showed to be a good predictor for 60-day post–eRe-LT mortality, with an AUROC of 0.84 (95% CI, 0.69-0.99). Different thresholds may be proposed depending on the preferred specificity or sensibility. When stratifying PELD/MELD score at re-LT into 3 quantiles (<15, 15-34, and >34), 92% of patients in the highest quantile died in the early post–eRe-LT period, compared with 16% of those in the lowest quantile, and 58% in the intermediate group (P = 0.001). The 1-, 3-, and 5-year patient survival rates by PELD/MELD quantiles are shown in Fig. 4.
Discussion
Despite advances in surgical techniques and perioperative care, vascular complications and PNF may lead to early graft failure and may require an urgent re-LT. These complications have decreased over time, with a better understanding of the eligibility criteria of the donors, reduced cold ischemia times, and improved surgical techniques, such as longitudinal portoplasty and microsurgery for portal or arterial reconstruction, respectively. Also, rigorous monitoring of vascular flow, using Doppler ultrasonography in the intraoperative period, is essential in preventing irreversible vascular damage.13 Lastly, aggressive prevention and preemptive management of vascular complications after pediatric LT have had a major impact on graft survival and should be considered the standard of care to reduce graft losses.14, 15
When a graft fails in the early posttransplantation period, the approach of the majority of pediatric LT units is to offer the option of re-LT. Prognostic factors of success versus failure in such a complex clinical scenario are necessary. In our study, since 1992, in 4.4% of LTs an eRe-LT was necessary. In 67% of the patients, vascular complications led to the need for eRe-LT, whereas in the remaining 33% the cause was PNF, similar to reports in other pediatric series.6-10, 13, 16-18
Although over time there has been a trend toward better survival in patients undergoing eRe-LT, results are still significantly worse than after a first transplantation.1, 5, 7, 16, 17, 19, 20 Also, results in patients undergoing eRe-LT are consistently worse than in those who undergo late re-LT, and prognosis in the eRe-LT patients is also worse than in those with the other classical indication for urgent LT: acute liver failure.17
In a large single-center series of children undergoing LT, Venick et al. found that eRe-LT was an independent prognostic factor for poor outcome.1 Ng et al. reported the results of re-LT in children registered in the Studies of Pediatric Liver Transplantation database from the United States.6 The authors showed that children who underwent re-LT ≤30 days after the first LT (eRe-LT) had a significantly lower survival rate (1- and 4-year patient survival rates of 59% and 56%, respectively) compared with children who underwent late re-LT.
In a recent large series of adult patients needing urgent LT due to acute liver failure compared with eRe-LT recipients, results were considerably worse in patients who underwent eRe-LT than in those who received a first LT due to acute liver failure, showing a significant association between disease severity measured by the MELD score and post-LT results.21 In a candidate for eRe-LT, assessment of disease severity is important because of the association of the clinical condition with the probability of post–eRe-LT survival. Intensive care therapy, as associated with a requirement of advanced life support at the time of re-LT, has been shown to be an independent risk factor of mortality both in children and adults.8, 16, 22
MELD/PELD scores were developed as tools to predict mortality on the waiting list for patients with chronic liver disease. Also, some studies have shown its usefulness as a predictor of mortality in cases of acute liver failure in children.23 Nevertheless, the MELD/PELD scores have not been consistently validated for the prediction of post-LT results.
Different studies have shown that, in the context of graft failure and need for re-LT, the MELD score may be a strong predictor of survival after re-LT.24 With some variation in the proposed cutoff points, reports indicate that the higher the MELD/PELD scores, the worse the post–re-LT outcome, and they show a very low survival rate when the PELD/MELD scores are 25-30 or higher.21, 25 Similarly, a good performance of the PELD/MELD scores for the prediction of post–eRe-LT survival was observed in the present study.
An era effect on post-LT results is consistently reported in most of the large series from centers that have performed LTs over the past 25-30 years.1, 6 The learning curves and improved technologies, among others, act synergistically and asynchronously, determining better post-LT results. The eRe-LT period is a challenging and complex scenario that is likely impacted by the era effect. Therefore, in historical cohorts, the influence of the classical prognostic variables should be adjusted for possible effects of the transplant era.
In our series, we observed that when adjusting for the era of LT, the severity of the patient’s condition (as assessed using the PELD/MELD scores and the need for advanced life support at the time of re-LT) was an independent predictor for early post–eRe-LT mortality in the multivariate analysis. PNF versus vascular complications also showed higher risk for post–eRe-LT death in the univariate analysis, but it lost statistical significance in the multivariate analysis. This finding may be explained by the fact that because of inherent clinical dynamics, MELD/PELD scores for primary graft failure were systematically higher than those for vascular complications. Post–re-LT mortality occurred in the early postoperative period (within 60 days) in almost 90% of patients, showing that the critical perioperative state of the patient is the main factor affecting results.
From a practical point of view, our data suggest that patients with a MELD/PELD higher than 34 who face an eRe-LT have a very low likelihood of survival, and therefore, the decision to proceed should be carefully considered. In patients with a PELD/MELD score between 15 and 34, the additional need for advanced life support diminishes the chances of survival, and it would be valuable to wait and see if the patient’s critical condition improves, which would enhance the chances of survival. Lastly, patients with a MELD/PELD score of <15 have the best chances of survival, regardless of the need for life support.1, 6, 8, 17, 26, 27
Finally, we report a group of patients who were relisted for eRe-LT but recovered without an LT and retained their graft. Some of whom underwent later re-LT, and others permanently retained their first graft. This situation was mainly observed in patients with vascular complications, and it should remind us of the feasibility of a watch-and-wait attitude in the face of this type of complication, allowing the patient to recover and eventually undergo a re-LT under better clinical conditions.28, 29
In conclusion, with the data and the analysis provided by our experience, it can be inferred that PELD score and the need for life support were good tools for predicting the chances of survival after early retransplantation, regardless of the era in which retransplant was performed. However, cutoff points should be considered approximations with possible idiosyncratic features to our sample, due to a limited number of patients and its unicentric origin.