Liver transplantation versus liver resection for hepatocellular carcinoma in intention to treat: An attempt to perform an ideal meta-analysis
Potential conflict of interest: Nothing to report.
Benjamin Menahem, Alexis Laurent, Arnaud Alves, and Guy Launoy participated in the design of the study. Benjamin Menahem, Alexis Laurent, and Jean Lubrano reviewed the articles. Benjamin Menahem and Alexis Laurent produced the statistics. Christophe Duvoux, Andrea Mulliri, Charlotte Costentin, and Ariane Mallat participated in the reviewing and editing of the article.
Abstract
This meta-analysis compared the effects of liver transplantation (LT) and liver resection (LR) on overall survival (OS) and disease-free survival (DFS) in patients with hepatocellular carcinoma (HCC) small transplantable HCC or within Milan criteria. Articles comparing LR with LT for HCC, based on Milan criteria or small size, published up to June 2015 were selected, and a meta-analysis was performed. No randomized controlled trial has been published to date comparing survival outcomes in patients with HCC who underwent LR and LT. Nine studies were identified, including 570 patients who underwent LR and 861 who underwent LT. For HCC within the Milan criteria, the 1-year OS rates following LR and LT were 84.5% (473/560) and 84.4% (710/841), respectively (odds ratio [OR], 0.98; 95% confidence interval [CI], 0.71-1.33; P = 0.8), and the 5-year OS rates were 47.9% (273/570) and 59.3% (509/858), respectively (OR, 0.60; 95% CI, 0.35-1.02; P = 0.06). One-year DFS rates were similar (OR, 1.00; 95% CI, 0.39-2.61; P = 1.00), whereas the 3-year DFS rate was significantly lower in the LR group (54.4%, 210/386) than in the LT group (74.2%, 317/427; OR, 0.24; 95% CI, 0.07-0.80; P = 0.02), and the 5-year DFS rate was significantly lower for LR than LT (OR, 0.18; 95% CI, 0.06-0.53; P < 0.01). For small HCCs, the 5-year OS rate was significantly lower for patients who underwent LR than LT (OR, 0.30; 95% CI, 0.19-0.48; P < 0.001). In conclusion, relative to LR, LT in patients with HCC meeting the Milan criteria had no benefits before 10 years for OS. For DFS, the benefit is obtained after 3 years. Liver Transplantation 23 836–844 2017 AASLD.
Abbreviations
-
- AFP
-
- alpha-fetoprotein
-
- CLD
-
- chronic liver disease
-
- CI
-
- confidence interval
-
- DFS
-
- disease-free survival
-
- EASL
-
- European Association for the Study of the Liver
-
- HCC
-
- hepatocellular carcinoma
-
- ITT
-
- intention-to-treat
-
- LR
-
- liver resection
-
- LT
-
- liver transplantation
-
- MELD
-
- Model for End-Stage Liver Disease
-
- ND
-
- not detailed in studies
-
- NS
-
- not significant
-
- OR
-
- odds ratio
-
- OS
-
- overall survival
-
- RCT
-
- randomized controlled trial
-
- WL
-
- waiting list
Hepatocellular carcinoma (HCC) is one of the most common forms of cancer worldwide and the main type of primary liver cancer. Approximately 90% of patients with HCC have chronic liver disease (CLD) and cirrhosis.1 Liver transplantation (LT) is the best theoretical treatment for HCC because it cures both the tumor and the underlying CLD.2 However, as a result of organ shortages, guidelines have restricted LT to HCC patients with an expected 5-year overall survival (OS) rate of > 50%,3 similar to the 5-year OS rate following LT for benign liver diseases of 70%.4
The clinical practice guidelines of the European Association for the Study of the Liver (EASL)–European Organization for Research and Treatment of Cancer on the management of HCC recommend liver resection (LR) as first-line treatment for patients with solitary tumors and very well-preserved liver function (evidence 2A; recommendation 1B).5 The latter has been defined as normal bilirubin concentration plus either a hepatic venous pressure gradient ≤10 mm Hg or platelet count ≥100,000/µL.5
This study was designed to compare LT with LR in patients with HCC eligible for LT, and split in 2 groups: those with only small transplantable HCC (<3 cm) and expand to those meeting the Milan criteria. Studies of intention-to-treat (ITT) populations were identified because graft shortage may result in patients being on the waiting list (WL) for LT for a long time. During this time, patients may die or become ineligible for LT. Indeed, the mean dropout rate has been reported to be 23%.6 Study end points included OS and disease-free survival (DFS).
Methods
DATA SOURCES
Databases, including MEDLINE, the Cochrane Collaboration, the Cochrane Clinical Trials Registry, and EMBASE, were searched using the terms “hepatocellular carcinoma” AND “resection” AND “liver transplantation” AND “cirrhosis” AND “RANDOM” for studies published in English through June 2015. Abstracts selected were reviewed independently by 2 researchers (B.M. and A.L.). Case studies, abstracts from congresses, unpublished data, and review articles were excluded.
INCLUSION AND EXCLUSION CRITERIA
All studies comparing OS and DFS in ITT populations of patients with underlying CLD who underwent LR and LT for HCC were included in this meta-analysis. Only clinical studies in humans and randomized controlled trials (RCTs) were selected. Studies comparing LT and LR in patients with etiology other than HCC, such as cholangiocarcinoma, hepatocholangiocarcinoma, and fibrolamellar HCC, were excluded, as were studies assessing OS and DFS after recurrence following first-line LR or LT. Prospective quantitative data on short-term and longterm OS and DFS and on the number and location of recurrences were extracted from the included articles.
DEFINITIONS
Oncologic LT was defined as transplantation within Milan criteria.7 Oncologic LR was defined as anatomical resection or resection with targeted margins >2 cm.8, 9 Patients eligible for major resection included those with chronic hepatitis or Child-Pugh class A cirrhosis, no esophageal varices, and a platelet count ≥100 × 109/L, whereas patients eligible for minor resections had varices of grade ≤2; all patients had an estimated remnant liver volume ≥50%.2 Transplantable and resectable HCC had to fulfill the 3 previous definitions. Small transplantable HCCs were defined as solitary HCCs of diameter ≤ 3 cm in patients with CLD (METAVIR F3-F4).5
DATA REVIEW AND EXTRACTION
After identifying eligible studies, 2 investigators (B.M. and A.L.) read the titles and abstracts of selected studies; after applying the exclusion criteria, the investigators read the full-text articles to determine eligibility for inclusion. They also reviewed the bibliography of selected articles and meta-analyses. Disagreements regarding inclusion were settled by consensus or, if necessary, by consultation with a third investigator (J.L.). Data extracted included study date; design; number of patients in each group; sex; age; number lost to follow-up; mean time on the LT WL; inclusion and exclusion criteria of the studies; 1-, 3-, 5-, and 10-year OS and DFS rates; and number and location of recurrences in each patient group. The quality of the studies was determined using the PRISMA statement.10
STATISTICAL ANALYSIS
All statistical analyses were performed using Review Manager 5.0 software (Cochrane Collaboration, Oxford, UK). Heterogeneity was assessed by I2 statistics with values above 50% defined as heterogeneous. If there was no evidence of heterogeneity, a fixed model was used; otherwise a random-effects model was used. Odds ratios (OR) and 95% confidence intervals (CIs) were calculated for each trial based on the number of evaluable patients and to confirm effect size estimation and test criteria. P value for overall effect was calculated using the Z test, with significance defined as a P value < 0.05. Publication bias and a sensitivity analysis were also performed, the latter during the review process when the particularities of the studies were identified.
Results
STUDY CHARACTERISTICS
Figure 1 shows a flowchart of study selection. The initial search identified 687 studies, of which 678 were excluded. Reasons for exclusion included study type or design of study, absence of peer review, study inclusion of patients with and without cirrhosis, inclusion of patients outside the Milan criteria, failure to report the main primary outcome of this meta-analysis, the performance of LR and/or LT for causes other than HCC and no ITT analysis. The 9 studies identified included 570 patients who underwent LR and 861 who underwent LT; none of these studies were an RCT (Table 1).
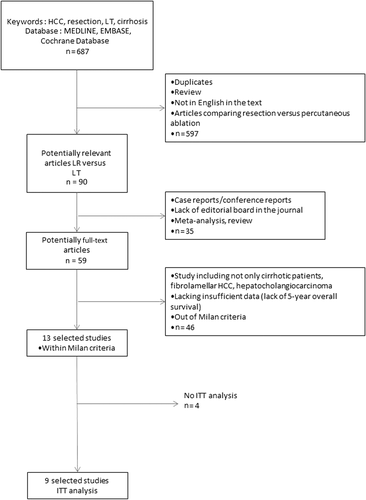
Flowchart of the meta-analysis.
| Author/Year | LR/LT | Mean Time on WL (days) | Treatment on WL, n (%) | Dropout Rate, n (%) | Child-Pugh Score | MELD Score | Multinodular | Tumor Size, mm, mean ± SDd | Mean Length of Follow-up, Years | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LR | LT | LR | LT | LR | LT | |||||||
| Llovet et al.6 (1999) | 77/87 | 105 ± 111 | NA | 8 (9.2) | A: 74 B: 3 C: 0 | A: 37 B: 38 C: 12 | NA | 13 | 33 | 33.4 ± 18.2 | 24.1 ± 13.8 | 5 |
| Bigourdan et al.11 (2003) | 20/17 | 24 | 0 (0) | 0 (0) | A: 20 | A: 17 | NA | 2 | 6 | 27.9 ± 12.7 | 37.5 ± 13.6 | 5 |
| Shah et al.12 (2007) | 121/140 | 231 | 41 (29) | 30 (21) | NA | Yes | 1.3 (1-3) | 2.4 (1-3) | 40 | 31 | 10 | |
| Baccarani et al.13 (2008) | 38/48 | 118 | 48 (100) | 2 (4.2) | A: 74 B: 26 C: 0 | A: 41 B: 42 C: 17 | No | 6 | 31 | 35 ± 11 | 37 ± 25 | 5 |
| Koniaris et al.14 (2011) | 33/237 | NA | NA | 37 (14.4) | NA | Yes | NA | NA | NA | NA | 5 | |
| Adam et al.15 (2012)a | 97b/101b | 171b | 59 (79) | 23 (31) | A: 80 B: 10 C: 1 | A: 19 B: 45 C: 37 | Yes | 0 | 0 | 33.5 ± 13.1 | 33.0 ± 18.6 | 10 |
| Sogawa et al.16 (2013)a | 56/75 | 88 ± 121b | 67 (56) | 16 (21.3) | A: 55 B: 1 C: 0 | A: 28 B: 47 C: 0 | Yes | 6 | 25 | 12 ± 8 | 17 ± 13 | 10 |
| Sapisochin et al.17 (2013)a | 95/122 | NA | NA | 3 (2.5) | A: 88 B: 7 C: 0 | A: 62 B: 47 C: 10 | No | 10 | 39 | 32.9 ± 11 | 32.4 ± 9.9 | 10 |
| Jiang et al.18 (2014)c | 33/34 | 105 ± 111 | NA | 8 (9.2) | A: 33 | A: 34 | No | 2.3 ± 0.5 | 2.4 ± 0.5 | 33.4 ± 18.2 | 24.1 ± 13.8 | 5 |
- a Data about solitary HCC available.
- b Data about small HCC available.
- c All patients transplantable in the LR group.
- d Mean for patients meeting the Milan and ICSF criteria in the study.
RESULTS OF THE META-ANALYSIS
Small Hepatocellular Carcinomas
Only 1 study reported short-term and longterm OS and DFS rates for patients with small HCCs who underwent LR or LT (See Table 2).
| OS, years | DFS, years | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 3 | 5 | 10 | 1 | 3 | 5 | 10 | |
| Actual meta-analysis - small HCC, LT versus LR | ND | ND | ND | ND | ND | ND | ND | ND |
| Actual meta-analysis - within Milan criteria, LT versus LR | NS | NS | NS | Favors LT | NS | Favors LT | Favors LT | ND |
Milan Criteria
Of the 9 studies that reported results in patients who met the Milan criteria, 8 reported 1-year and 3-year OS rates, all 9 reported 5-year OS rates, and 4 reported 10-year OS rates. These studies included 570 who underwent LR and 858 who underwent LT. The 1-, 3-, and 5-year OS rates were similar in patients who underwent LR and LT. Specifically, their 1-year OS rates were 84.5% (473/560) and 84.4% (710/841), respectively (OR, 0.98; 95% CI, 0.71-1.33; P = 0.8); their 3-year OS rates were 65.3% (326/499) and 69.6% (401/576), respectively (OR, 0.81; 95% CI, 0.49-1.33; P = 0.40); and their 5-year OS rates were 47.9% (273/570) and 59.3% (509/858), respectively (OR, 0.60; 95% CI, 0.35-1.02; P = 0.06; Fig. 2). In contrast, the 10-year OS rate was significantly lower in the LR than in the LT group (29.8% [110/369] versus 50.0% [219/438]; OR, 0.40; 95% CI, 0.23-0.68; P < 0.001).
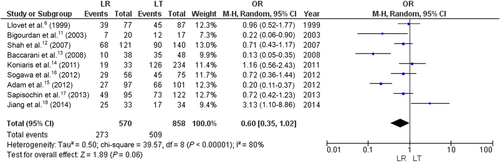
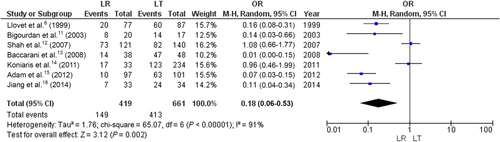
Five-year OS in ITT analysis.
A total of 6 of the 9 studies also reported 1- and 3-year DFS rates, 7 reported 5-year DFS rates, and only 1 reported 10-year DFS rates. DFS was analyzed in 419 patients who underwent LR and 661 who underwent LT. Their 1-year DFS rates were similar: 83.4% (333/399) and 78.6% (513/652), respectively (OR, 1.00; 95% CI, 0.39-2.61; P = 1.00). However, the 3-year DFS rate was significantly lower in the LR (54.4% [210/386]) than in the LT (74.2% [317/427]) group (OR, 0.24; 95% CI, 0.07-0.80; P = 0.02; Fig. 3). Similarly, the 5-year DFS rate was significantly lower in the LR (35.6% [149/419] than in the LT (62.5% [413/661]) group (OR, 0.18; 95% CI, 0.06-0.53; P < 0.01; Fig. 4).
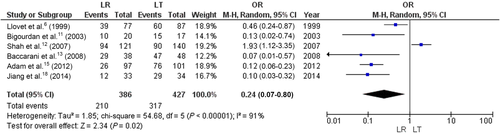
Three-year DFS in ITT analysis.
Five-year DFS in ITT analysis.
A total of 8 of the 9 studies reported recurrence rate, which was significantly higher in the LR (53.3% [572/1073]) than in the LT (12.9% [136/1050]) group (OR, 9.61; 95% CI, 6.57-14.06; P < 0.001; Fig. 5).
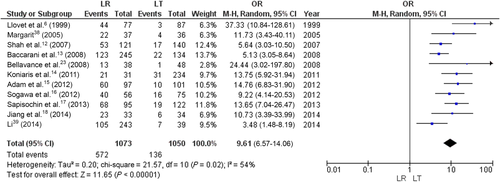
Recurrence rate.
Sensitivity and Publication Bias
Sensitivity and publication bias were also analyzed. Combined ORs for 1-, 3-, and 5-year DFS rates; 3-, 5-, and 10-year OS rates; and overall and intrahepatic recurrence rates were calculated with fixed and random-effects models and the results were compared. A high risk of bias was observed because none of these studies was randomized or blinded and all were retrospective analyses. Attrition bias could not be determined because some of these studies did not report dropout rates. Furthermore, as statistically significant data tend to be published more than negative trials, our results may have been influenced by publication bias.
Discussion
This meta-analysis of patients with CLD who developed HCC within the Milan criteria and underwent LR or LT found no between-group difference in 1-, 3-, and 5-year OS rates. However, 10-year OS rates were higher in patients who underwent LT. A comparison of DFS rates showed that they were similar at 1 year, but that 3- and 5-year DFS rates were higher in patients who underwent LT than LR.
Oncologic LT has been defined as LT in patients who meet the Milan criteria. In 2012, a French multicenter study reported that the addition of alpha-fetoprotein (AFP) concentration to the Milan criteria improved the performance of the Milan criteria.4 No study to date, however, has compared LR with LT in patients meeting these AFP-enhanced criteria. Moreover, at present, the Milan criteria remain the international reference in European and US guidelines.19
Oncologic LR has been defined, according to EASL guidelines,19 as LR performed in patients with solitary HCC < 5 cm with resection margins >2 cm. We used the criterion of a single tumor to compare outcomes in patients with primary tumors and to exclude patients with metastatic disease or multicentric carcinogenesis. The 5-cm threshold was chosen because the LT group consisted of patients who met the Milan criteria, in which the maximum diameter of solitary tumors is 5 cm. Resection margins were included in the selection process, as 2 procedures were being compared. Resection margins for solitary HCCs < 2 cm have a greater effect on survival than microvascular invasion or the presence of satellite nodules.8, 9 EASL guidelines for resection of HCC include chronic hepatitis or Child-Pugh class A cirrhosis, no esophageal varices, and a platelet count ≥100 × 109/L for major resections and grade ≤2 varices for minor resections, and an estimated remnant liver volume ≥50%.19 No study to date, however, and no RCT, has compared outcomes in patients with resectable HCC undergoing oncologic LT or oncologic LR, precluding the performance of an ideal meta-analysis. We therefore performed an actual meta-analysis by comparing survival outcomes in patients undergoing oncologic LT within the Milan criteria with oncologic LR, including nonresectable patients with Child-Pugh B and C cirrhosis.
Although 1-year DFS rates did not differ significantly in patients who underwent LT and LR, 3- and 5-year DFS rates were significantly higher in the LT group. Most patients with HCC who undergo LR have single nodules <5 cm in diameter and a 1-year DFS after resection of approximately 80%.2, 20 The 1-year DFS rate after LT has also been reported to be approximately 80%.21 At 3 and 5 years, however, LT is superior because it cures both the tumor and the underlying liver disease that can again give rise to a tumor.22 LT removes micrometastases, which may not be removed by LR, allowing micrometastases within the remnant liver to progress postoperatively.23 Indeed proximal and distal margins of 10 mm have been recommended for HCCs ≤3 cm, whereas, for larger tumors, a proximal resection margin of 10 mm and a resection distal margin of 20 mm have been recommended.24 DFS could not be analyzed in patients with solitary HCC <3 cm because only 1 study included this population.15
The 1-, 3-, and 5-year OS rates in patients who fulfilled the Milan criteria were similar after LT and LR. Specialized centers have reported 5-year OS rates of 80% after LT, whereas large registries have somewhat lower 5-year OS rates, approximately 65%.25 OS is strongly dependent on dropout rates.6 The 9 studies included in this meta-analysis reported dropout rates ranging from 9.2% to 31%.6, 13, 15-18, 26
The 10-year OS rate was significantly higher in patients who underwent LT than LR. However, this result was based on only 4 studies. In 3 of these 4 studies, patients undergoing LR were older than those undergoing LT.15-17 Older patients, especially those with cirrhosis, have a higher risk of death, which may explain the between-group difference in longterm OS rate.27 Analyses of survival should consider possible biases in group composition.28
Of the 9 studies, 8 assessed tumor size as the main criterion in comparing LR with LT. One study, however, assessed patients with multiple nodules and found that the DFS rate was higher in patients who underwent LT.18 To address the effect of multifocal carcinogenesis on DFS after LR, patients were divided into groups with tumors in the same lobe or in different lobes. The DFS rate was higher in patients with localized rather than with disseminated disease. Taken together, the results of this meta-analysis reinforce the current European Practical guidelines,19 which put resection as the first-line treatment option for patients with solitary tumors. By consequence, the present study implies that the strategy of primary resection and salvage LT is to be preferred to primary upfront LT. This implication is based not only on the graft-saving it induced in the area of graft shortage but also on its intrinsic results (DFS and OS).
One limit of this analysis was the lack of published RCTs.29 Moreover, to our knowledge, no RCT comparing LR with LT is ongoing or registered at https://clinicaltrials.gov. In the organ transplantation setting, it is extremely difficult to organize RCTs, in particular from the multifaceted perspective of WLs.30 For example, in France, the inclusion of AFP concentration with the Milan criteria has resulted in the lack of prioritization of patients with resectable and transplantable HCCs on the national WL, with a salvage LT program proposed.31
Other limitations of this meta-analysis are those consistent with the conventional limitations of meta-analyses based on retrospective studies, including recruitment, selection, and confounding biases. There are 2 major causes of recruitment bias. First, all patients are not referred to LT programs. Second, even if transplanted, patients are managed in tertiary referral centers; resectable patients are often managed in other centers where radiofrequency ablation may be performed.32 Selection biases are also inherent in retrospective studies. Indeed, age and tumor features, including number and size, were not strictly comparable in different studies.6, 15 Confounding bias can result especially from competing risks of death. Patients with good longterm prognosis, including those with resectable and transplantable HCCs, have a 5-year OS rate of 85%.2, 33 These patients, however, should be further analyzed by competing risk because diseases associated with immunosuppression are a major threat after 5 years.28
In conclusion, the results of this meta-analysis, assessing patients with HCC within the Milan criteria who underwent LT or LR, found that OS rate was significantly higher for LT only at 10 years. Thus, during an era of graft shortages, LR has several advantages over LT, the 2 most important being its immediate availability and an OS rate comparable to LT.2 This study underlines the need to continue the reflection about the influence transplant-related survival benefit should have on the prioritization for LT.34-37