T-Tube or no T-tube in the reconstruction of the biliary tract during orthotopic liver transplantation: Systematic review and meta-analysis
Abstract
The routine use of a T-tube in reconstruction of the biliary tree during orthotopic liver transplantation (OLT) is controversial. A systematic review of the literature on the use of a T-tube in reconstruction of the biliary tree was performed. Retrospective studies were only reviewed, whereas prospective randomized studies were included in the meta-analysis. An analysis of 196 studies revealed that 91 studies investigated the use of a T-tube in OLT. Fifteen retrospective studies compared different groups and were thus considered relevant; 6 prospective studies were identified, of which 5 were randomized controlled trials with a total of 639 patients. The results of the randomized controlled trials were meta-analyzed. The odds ratio (OR) for biliary complications was 1.15 [95% confidence interval (CI) = 0.28-4.72], and this revealed that there were no differences in the rate of overall biliary complications whether or not a T-tube was used (Z = 0.19, P = 0.85). A detailed analysis of the biliary complications revealed that biliary leaks developed in 24 patients in the T-tube group versus 22 patients in the no–T-tube group (OR = 1.17, 95% CI = 0.4-3.47, Z = 0.29, P = 0.77). Biliary strictures were significantly more common in the group of patients who underwent reconstruction without a T-tube (14 versus 31 events; OR = 0.46, 95% CI = 0.23-0.9, Z = 2.26, P = 0.02). In conclusion, although reconstruction of the biliary tree with a T-tube prevents the occurrence of biliary strictures and may have the potential to reduce long-term morbidity with respect to late strictures, there is no clear evidence in favor of using a T-tube during OLT. Liver Transpl 16:705-717, 2010. © 2010 AASLD.
The rapid advances in the field of liver transplantation with rising numbers of transplants per year during the last decades have resulted in significantly improved outcomes (with respect to morbidity and mortality as well as long-term survival and graft survival). This not only is a result of progress in surgical techniques but also is due to better control of immunosuppression and infections. However, biliary complications still occur in 10% to 30% of patients, with consecutive mortality rates as high as 10% in whole organ orthotopic liver transplantation (OLT).1-6 Although these numbers are superior to data from the 1970s showing morbidity rates of 34% to 50% and mortality rates of 25% to 30% due to biliary complications after OLT,7, 8 they still constitute a major challenge in transplant surgery. The risk of biliary complications seems to be even higher in OLT with reduced size organs, in split liver transplants, and in living donor liver transplants, with an increased incidence of biliary complications of 10% to 60%.9-20 To reduce biliary complications, a variety of approaches, such as different anastomoses (ie, end-to-end or side-to-side) and dissection techniques and the use of a T-tube for the duct-to-duct anastomosis, have been implemented. Although T-tubes were generally used and recommended in the 1970s and 1980s, retrospective and prospective data from the last 15 years are incoherent and suggest that using a T-tube for reconstruction increases the risk of biliary complications. However, a number of transplant centers worldwide still use T-tubes because they have some advantages, such as the option of monitoring the quality and amount of bile as indirect signs of the function of the transplanted liver. T-tubes also allow the cholangiographic assessment of the biliary anatomy and have been thought to protect the biliary anastomosis from leakage by reducing intraductal pressure. Some reports have also demonstrated that after T-tube reconstruction, there is a reduced incidence of strictures.21 In contrast, the disadvantages have been emphasized over the last years. In most of the retrospective analyses, a higher rate of biliary complications was seen. In particular, biliary leakage following removal of the T-tube remained a constant source of (severe) morbidity, in part because of the increased risk of biliary peritonitis and cholangitis. Furthermore, placing a T-tube did not seem to prevent suture-related insufficiencies or stenoses. Randomized studies of whether a T-tube should be routinely used for reconstructing the biliary tract in OLT demonstrated different results with respect to biliary complications.6, 22-25 Although the most recent meta-analysis by Sotiropoulos and coworkers26 revealed that the use of a T-tube was rather unnecessary, data from the latest randomized trial by Weiss et al.27 demonstrated that a T-tube was associated with significantly fewer overall biliary complications. We thus performed a systematic review and a (re-)meta-analysis of biliary complications in OLT with or without T-tube placement for reconstruction of the biliary tract.
Abbreviations:
CI, confidence interval; HJS, hepaticojejunostomy; m, matched; nm, not matched; ns, not specified; OLT, orthotopic liver transplantation; OR, odds ratio; PDS, polydioxanone suture.
MATERIALS AND METHODS
Search Strategy and Inclusion and Exclusion Criteria
Three authors (C.R., C.W.M., and M.W.M.) independently performed a systematic literature search (with the last search in November 2009) of the databases of the National Center for Biotechnology Information, the National Library of Medicine, the Cochrane Central Register of Controlled Trials, the Internet, and the authors' own libraries; they used “T-tube AND liver transplantation” as search terms, as previously described.28 Additionally, Google Scholar was used. However, no articles other than those retrieved with the National Center for Biotechnology Information/National Library of Medicine search were found. No language restriction was applied. The retrieved abstracts were stratified according to their relevance to the subject, and the full text of articles on the use of a T-tube for biliary reconstruction during OLT was retrieved. Additional articles were identified by cross-searching of the bibliographies of these publications. Case reports were excluded from the analysis. Retrospective studies were included in the systematic review, whereas prospective randomized studies were included in the meta-analysis. The prospective randomized trials that were included had to be conducted to study the use of a T-tube for reconstruction of the biliary tree in OLT and at least had to report on overall biliary complications.
Data Extraction
The results of the retrieved studies were meta-analyzed with respect to the number of included patients, the rates of biliary complications, bile leaks, and biliary strictures, and mortality. The data collection and assessment of methodological quality were conducted as previously reported.29 The conduct and reporting were in accordance with the Quality of Reporting of Meta-Analyses statement.30 The methodological quality was assessed separately for the prospective studies (the definition of outcome parameters and complications, completeness of follow-up, and statistical analyses). Heterogeneity was evaluated by an analysis of the comparability of the following items: the number of patients, the grade or stage of disease, and the type of surgery performed.
Statistical Analysis
The meta-analysis was performed as previously described with Review Manager (RevMan) software, version 4.2.8 (Cochrane Collaboration, Oxford, United Kingdom), and this was followed by a quality of allocation concealment. Biliary complications, bile leaks, biliary strictures, and mortality in the respective study arms were estimated as subsumed odds ratios (ORs) with 95% confidence intervals (CIs) with the random effects model of DerSimonian and Laird.31 Effects on the length of hospital stay were analyzed by the weighted mean difference approach. Statistical heterogeneity was assessed with a forest plot and the inconsistency statistic (I2). Statistical significance was considered at P < 0.05.
RESULTS
The MEDLINE search, using the search term “T-tube AND liver transplantation,” revealed 196 titles, the abstracts of which were retrieved. Of these, 105 abstracts had to be excluded because they did not deal with T-tubes in OLT. Ninety-one studies analyzed the use of a T-tube in reconstruction of the biliary tree in OLT, and they included 10 reviews, 2 case reports, and 1 letter to the editor. The full-text articles for these 91 studies were retrieved. A detailed analysis showed that of these, 22 studies compared biliary reconstruction with a T-tube to reconstruction without a T-tube (Fig. 1). Fifteen studies were retrospective, whereas 1 prospective study was found (Table 1). One retrospective study was excluded because of the surgical technique: in the study by Alsharabi et al.32 published in 2007, either a cholangiojejunal Roux-en-Y anastomosis or hepaticojejunostomy with or without a T-tube was performed for biliary reconstruction. In our opinion, the results are not comparable to those of choledochocholedochostomy with respect to the effect of a T-tube. In all, 5 randomized trials and 1 meta-analysis were identified (Table 2).
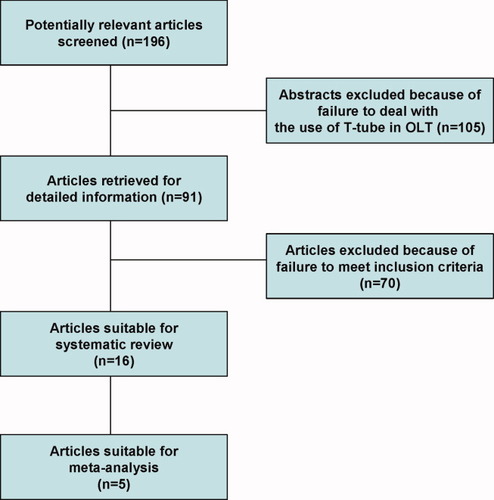
Flowchart for the systematic literature search. The flowchart shows the selection steps for the systematic literature search. The MEDLINE search using the search term “T-tube AND liver transplantation” revealed 196 titles, including 15 case reports, 13 reviews, and 10 randomized controlled trials. [Color figure can be viewed in the online issue, which is available at www.interscience.wiley.com.]
| Author (Time Period) | Study Design | Year | OLT | Full Size or Split Liver | 1. T-Tube 2. No T-Tube 3. HJS | Survival | Overall Biliary Complications | Biliary Complications | Biliary Strictures | Biliary Leakage | Endoscopy and Reoperation | Age (years) | In Favor (+)/ Against (−) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lin et al.33 (08/2001-02/2006) | Retrospective (m) | 2007 | n = 104 | Full size | 1. n = 51 2. n = 53 | ns | 14/104 (13.5%) | No difference between groups | 12/104 (11.5%) | 2/104 (1.9%) | 9/104 (8.6%) and 6/104 | ns | +/− |
| Kobayashi et al.46 (03/1999-03/2004) | Retrospective (nm) | 2007 | n = 28 | Left lobe living donor | 1. n = 17 [including T-tube (6) and external stent (11)] 3. n = 11 | 71.4% (31 months) | 11/28 (39.9%) | 1. T-tube, 0/6; external stent, 5/11 (45.5%) 3. HJS, 6/11 (54.5%) | 1. T-tube, 0/6; external stent, 3/11 (27.3%) 3. HJS, 1/11 (9.1%) | 1. T-tube, 0/6; external stent, 5/11 (45.5%) 3. HJS, 5/11 (45.5%) | ns and 1 | 17-63 | + |
| Li et al.43 (11/2002-06/2005) | Retrospective (m) | 2007 | n = 84 | Full size | 1. n = 33 2. n = 51 | ns | 16/84 (19%) | 1. n = 10 (30.3%) 2. n = 6 (11.8%) | 1. n = 5 (15.2%) 2. n = 4 (7.8%) | 1. n = 4 (12.1%) 2. n = 1 (2%) | 1. n = 9 (27.2%) 2. n = 4 (7.8%) and 1. n = 0 2. n = 1 | ns | − |
| Wojcicki et al.45 (11/1992-01/2005) | Retrospective (m) | 2006 | n = 70 | Split liver (right lobe) | 1. n = 26 (e-e) 2. n = 26 (e-e) 3. n = 18 | 1. 2/26 (mortality) 2. 3/26 (mortality) 3. 1/18 (mortality) | 18/70 (26%) | 1. n = 4 (15.4%) 2. n = 10 (38.5%) 3. n = 4 (22.2%) | 3/70 (4%) | 4/70 (6%) Leak of the surface, 11% of all | 1. n = 1 (3.8%) 2. n = 5 (19.2%) 3. n = 2 (11.1%) and 1. n = 1 2. n = 4 3. n = 0 | 19-70 | + |
| Elola-Olaso et al.42 (04/1986-09/2004) | Retrospective (m) | 2005 | n = 100 (in 96 patients) | Full size | 1. n = 50 2. n = 50 | 77% (time period ns) | 16/100 (16%) | ns | 1. n = 6 (12%) 2. n = 4 (8%) | 1. n = 3 (6%) 2. n = 0 | 2/100 (2%) and 1. n = 5 2. n = 2 | 51.93 ± 9.8 | − |
| Kusano et al.44 | Retrospective (nm) | 2005 | n = 115 | Full size | 1. n = 63 (e-e) 2. n = 52 (e-e) | ns | 31/115 (20%) | 1. n = 24 (38.1%) 2. n = 7 (13.5%) | 1. n = 16 (25.4%) 2. n = 7 (13.5%) | 1. n = 8 (12.7%) 2. n = 4 (7.7%) | ns and 1. n = 8 2. n = 29 | ns | + |
| Shimoda et al.40 (01/1998-12/1998) | Retrospective chart review (m) | 2001 | n = 147 | Full size | 1. n = 76 2. n = 71 | 83% (1 year) and 89.5% (2 years) | 36/147 (24.4%) | 1. n = 25 (32.9%) 2. n = 11 (15.6%) | 1. n = 5 (6.6%) 2. n = 6 (8.5%) | 1. n = 18 (22.7%) 2. n = 5 (7%) | 1. n = 14 (18.4%) 2. n = 6 (8.4%) and 1. n = 5 2. n = 5 | >18 | − |
| Nemec et al.41 (01/1992-12/2000) | Retrospective (nm) | 2001 | n = 118 (in 113 patients) | Full size | 1. n = 15 (e-e-GB) and n = 29 (e-e/s-s) 2. n = 67 (e-e) | 84.9% | 33/118 (27.8%) | 1. 8/15 (44.8%) and 16/29 (57.1%) 2. 11/67 (16.4%) | 20/118 (16.9%) | 13/118 (11%) | 17/118 (14.4%) and 12/118 (10.2%) | − | |
| Jeffrey et al.34 (2-year period) | Retrospective (nm) | 1999 | n = 28 (in 30 patients) | Full size | 1. n = 17 (e-e) 2. n = 11 (e-e) | ns | 14/28 (50%) | 1. n = 8 (47.1%) 2. n = 6 (54.5%) | 1. n = 5 (29.4%) 2. n = 5 (45.5%) | 1. n = 5 (29.4%) 2. n = 4 (36.4%) | +/− | ||
| Ben-Ari et al.39 | Retrospective (nm) | 1998 | n = 83 | Full size | 1. n = 15 2. n = 57 3. n = 11 | ns | 12/83 (14.5%) | 1. n = 4 (26.7%) 2. n = 7 (12.3%) 3. n = 1 (9%) | 1. n = 6 (37.5%) 2. n = 1 (1.8%) Sepsis | ns | − | ||
| Rabkin et al.5 (09/1991-06/1996) | Retrospective (nm) | 1998 | n = 227 (in 220 patients) | Full size | 1. n = 124 (e-e) 2. n = 44 (e-e) and n = 59 (s-s) | 83% (1 year) | 69/227 (30%): leak, 43/227 (19%); stricture, 26/227 (12%) | 1. n = 43 (34.7%) 2. 11/44 (25%) and 15/59 (25.4%) | 1. n = 7 (6%) 2. 10/44 (23%) and 9/59 (15%) | 1. n = 36 (29%) 2. 1/44 (2%) and 6/59 (10%) | 13/227 (6%) and 27/227 1. n = 10 2. n = 8 and n = 9 | 16-69 | +/− |
| Kizilisik et al.38 (02/1994-08/1996) | Retrospective (nm) | 1997 | n = 51 (in 49 patients) | Full size | 1. n = 20 2. n = 20 3. n = 11 | ns | 9/51 (18%) | 1. n = 8 (40%) 2. n = 1 (5%) | 1. n = 1 (5%) 2. n = 0 (0%) | 1. n = 8 (40%) 2. n = 1 (5%) | 1. n = 9 (45%) 2. n = 1 (5%) and 1. n = 0 2. n = 1 | Included children | − |
| Koivusalo et al.37 | Retrospective (nm) | 1996 | n = 90 | Full size | 1. n = 25 2. n = 59 3. n = 6 | 71% (5 years) | 1. n = 6 (24%) 2. n = 7 (12%) | 8/90 (8.9%) | 9/90 (10%) | ns | ns | − | |
| Randall et al.36 (01/1993-06/1994) | Retrospective | 1996 | n = 110 | Full size | 1. n = 59 2. n = 51 | 1. 84.7% 2. 90.6% (1 year) | 20/110 (18%) | 1. n = 13 (22%) 2. n = 7 (13.7%) | ns | ns | 1. n = 4 (6.8%) 2. n = 2 (3.9%) and 1. n = 4 2. n = 4 | >16 | − |
| Ferraz-Neto et al.35 (01/1993-12/1994) | Prospective (m) | 1996 | n = 199 (in 183 patients) | Full size | 1. n = 110 (e-e) 2. n = 89 (e-e) | ns | 1. n = 26 (23.6%) 2. n = 10 (11.2%) | ns | ns | 16-69 | − |
| Author (Time Period) | Study Design | Year | Patients | Full Size or Split Liver | 1. T-Tube 2. No T-Tube | Survival | Overall Biliary Complications | Biliary Complications | Biliary Strictures | Biliary Leakage | Endoscopy and Reoperation | In Favor (+)/ Against (−) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Weiss et al.27 (2005-2007) | Prospective, randomized | 2009 | n = 194 | Full size | 1. n = 99 (s-s) 2. n = 95 (s-s) | 1. 98% 2. 93% (1 year) | 1. n = 27 (27.3%) 2. n = 50 (52.6%) | 1. n = 7 (7.1%) 2. n = 8 (8.4%) | 1. n = 5 (5.1%) 2. n = 9 (9.5%) | 1. 9% 2. 18% and 1. n = 4 2. n = 4 | + | |
| Amador et al.22 (10/2002-03/2004) | Prospective, randomized | 2007 | n = 107 | Full size | 1. n = 53 (e-e) 2. n = 54 (e-e) | 1. 92% 2. 96% (1 year) | 38/107 (35.5%) | 1. n = 32 (60.4%) 2. n = 6 (11.1%) | 1. n = 1 (1.8%) 2. n = 3 (5.5%) | 1. n = 6 (11.3%) 2. n = 3 (5.5%) | 1. n = 8 (15.1%) 2. n = 6 (11.1%) and 1. n = 9 2. n = 4 | − |
| Scatton et al.23 (01/1994-04/1997) | Prospective, randomized | 2001 | n = 180 | Full size | 1. n = 90 (e-e; including 1 HJS) 2. n = 90 (e-e) | 1. 72.8% 2. 80.1% (3 years) | 44/180 (24.4%) | 1. n = 30 (33.3%) 2. n = 14 (15.5%) | 1. n = 3 (3.3%) 2. n = 6 (6.7%) | 1. n = 2 (2.2%) 2. n = 2 (2.2%) | 1. n = 3 (3.3%) 2. n = 4 (4.4%) and 1. n = 7 2. n = 8 | − |
| Nuno et al.24 (04/1994-12/1995) | Prospective, randomized | 1997 | n = 98 | Full size | 1. n = 50 (e-e) 2. n = 48 (e-e) | ns | 21/98 (21.4%) | 1. n = 5 (10%) 2. n = 16 (33%) | 1. n = 1 (2%) 2. n = 8 (16.7%) | 1. n = 3 (6%) 2. n = 8 (16.7%) | ns and 1. n = 3 2. n = 15 | + |
| Vougas et al.25 (01/1992-12/1992) | Prospective, randomized | 1996 | n = 60 | Full size | 1. n = 30 2. n = 30 | 1. 83.3% 2. 83.3% | 11/60 (18.3%) | 1. n = 5 (16.7%) 2. n = 6 (20%) | 1. n = 2 (6.7%) 2. n = 6 (20%) | 1. n = 1 (3.3%) | 1. n = 3 2. n = 6 and 1. n = 2 2. n = 3 | − |
Retrospective Studies
Because of the routine use of T-tubes in OLT in the 1970s and 1980s, no larger studies of biliary complications after OLT without a T-tube had been performed. Thus, we analyzed 14 retrospective studies and 1 prospective study dating from 1996 to 2007 (Table 1); except for 1 study, these were single-center experiences. The number of patients in these studies ranged from 28 to 220 patients. Anastomosis techniques varied considerably and depended on the respective center and surgeons. Some analyses also included retransplants, pediatric transplants, split liver transplants, and living donor split liver transplants or reported exclusively on 1 (or more) of these groups of patients.
Studies Demonstrating No Differences Between the T-Tube and No–T-Tube Groups
In the study by Lin and coauthors,33 the overall biliary complication rate was comparably low (overall 13.5%) without any significant differences between the group with a T-tube and the group without a T-tube. Jeffrey et al.34 also did not find any differences whether or not a T-tube was used (overall biliary complication rate of 50%); however, the total number of patients (n = 28) was quite low. In 1998, Rabkin et al.5 retrospectively analyzed 220 patients who underwent full size OLT and found a biliary complication rate of 30% without any statistical significance between the groups. However, the authors tended to recommend the use of a T-tube.
Studies Advocating Reconstruction Without a T-Tube
Most of the retrospective studies from larger transplant centers revealed a consensus of avoiding the routine use of T-tubes. Ferraz-Neto et al.35 in 1996 reported prospectively matched data after OLT in 183 patients and showed a higher rate of biliary complications in patients with biliary duct reconstruction with a T-tube. Similarly, Randall and coworkers36 reported a study in the same year showing a significantly higher morbidity rate with biliary complications in 22% of the patients with a T-tube versus 13.7% of the patients without a T-tube. They also described a difference in the 1-year survival rate, even though the difference was not significant (84.7% versus 90.6%, respectively). In 1996, Koivasalu et al.37 reported a biliary complication rate as high as 24% in patients undergoing OLT with a T-tube versus 12% in patients without a T-tube; however, because of patient group heterogeneity, the reported results were not statistically significant. Kizilisik and coworkers38 demonstrated a biliary complication rate of 40% in the T-tube group versus 5% in the no–T-tube group; although the groups were matched, the total number of patients was low, and re-OLT procedures as well as pediatric OLT procedures were included in their analysis. Ben-Ari et al.39 demonstrated in an analysis of 83 patients a significantly higher rate of biliary complications in patients with choledochocholedochostomy over a T-tube (26.7%) versus patients with choledochocholedochostomy without a T-tube (12.3%) or Roux-en-Y anastomosis without a T-tube (9%). The difference was not statistically significant because the groups were not well matched and were different in size (n = 15 with a T-tube, n = 57 without a T-tube, and n = 11 with Roux-en-Y anastomosis without a T-tube). These results were confirmed by another large retrospective single-center analysis including 147 patients that was reported in 2001 by Shimoda et al.40 The overall biliary complication rate in their study was 24.4%. However, it reached 32.9% in the group that underwent reconstruction with a T-tube but was only 15.6% in those patients in whom reconstruction had been performed without a T-tube. The authors thus suggested biliary reconstruction without a T-tube.
In 2001, Nemec et al.41 retrospectively compared biliary complications in 113 patients with biliary reconstruction over a T-tube. Choledochocholedochostomy (end-to-end) with a T-tube in the retained gallbladder was performed in 15 patients, and choledochocholedochostomy (end-to-end) over a T-tube was performed in 29 patients. Sixty-seven patients received a choledochocholedochostomy (end-to-end) without a T-tube. Biliary complications occurred in 33 of 118 OLT procedures (27.8%), of which 44.8% and 57.1% were in the T-tube groups versus 16.4% in the no–T-tube group. Elola-Olaso et al.42 published comparable results by presenting their data for 100 OLT procedures in 96 patients; 50 included reconstruction over a T-tube. Overall, biliary complications occurred in 16 of 100 cases with more postoperative complications in the T-tube group. Similarly, Li et al.43 demonstrated a biliary complication rate of about 19% (16/84) in a retrospective analysis of 84 OLT procedures. Ten of 33 patients (30.3%) that underwent reconstruction with a T-tube developed biliary complications versus only 6 of 51 patients (11.8%) that underwent reconstruction without a T-tube. Similar results were reported by Kusano et al.44 in 2005. They retrospectively analyzed biliary complications in 115 patients: 63 had received an end-to-end choledochocholedochostomy with a T-tube, and 52 underwent reconstruction without a T-tube. Biliary complications occurred in 31 of 115 patients. In the T-tube group, the rate of biliary complications was significantly higher (24/63) than that in the no–T-tube group (7/52). However, the authors still recommended the routine use of T-tubes because of the lower incidence of conversion to a hepaticojejunostomy in the T-tube group (12.5%) versus the no–T-tube group (57.1%).
Even though the differences seen in the studies seem to be obvious, the groups were mostly not perfectly matched, and thus statistical significance was often not reached.
Studies Analyzing Reduced Size Livers
The following 2 studies analyzed liver transplants with reduced size livers, such as split livers or living donor–related livers. Wojcicki et al.45 performed a retrospective analysis of biliary complications in 70 patients that underwent adult right lobe split liver transplantation and suggested the routine use of a T-tube within reduced size liver reconstruction. The same conclusion was made by Kobayashi et al.46 in 2007 when they analyzed biliary complications after left lobe living donor transplantation and demonstrated a trend toward fewer complications in the T-tube group. However, the number of patients was quite low (n = 28), and a control group was missing.
In conclusion, of the retrospective studies analyzed, only 3 favor the use of a T-tube, whereas 9 recommend biliary reconstruction without a T-tube; 3 retrospective analyses found no differences in complication rates between the T-tube and no–T-tube groups (Table 1).
Prospective Randomized Trials and Meta-Analysis
The first prospective randomized trial was performed by Vougas et al.25 and was published in 1996. Sixty patients undergoing OLT were randomized into groups of 30 patients who received biliary reconstruction [end-to-end bile duct anastomosis with polydioxanone suture (PDS) 5-0 or 6-0] with a T-tube (8-FG latex) or without a T-tube. Patients with gross differences in the diameters of the donor and recipient bile ducts were excluded from the trial. The authors reported on significant biliary complications in 5 patients in the T-tube group and in 6 patients in the no–T-tube group (no statistically significant difference). The occurrence of these complications was in both groups associated with a prolonged graft cold ischemic time. The types of biliary complications were different in the groups: although patients with a T-tube developed bile duct strictures (n = 2), a bile leak (n = 1), and cholangitis (n = 2), biliary complications in the no–T-tube group became clinically evident only as bile duct strictures. These were mostly (n = 5) late strictures (>3 months after surgery). The mortality rates in the 2 groups were comparable (n = 5).
In 1997, Nuno et al.24 reported the results of a prospective randomized study of 98 consecutive OLT procedures performed between April 1994 and December 1995. Patients were randomized into groups with or without T-tubes according to the center (group 1, center 1; group 2, center 2) in which they underwent their operation. Fifty patients were randomized to the group with T-tubes (material not specified), whereas in 48 patients, reconstruction without a T-tube was performed.
The bile duct anastomosis was fashioned as an end-to-end choledochocholedochostomy with interrupted 5-0 polyglactin sutures. Patients received the same immunosuppression. For organ preservation, University of Wisconsin solution was used, and the cold ischemic time did not exceed 12 hours. T-tubes were removed 3 months after OLT, and the average follow-up time was 9 months. Biliary complications occurred in 5 patients in whom a T-tube had been used, whereas 16 patients in the no–T-tube group developed such complications. Reoperation was necessary for 3 patients of the T-tube group and for 15 patients of the no–T-tube group. These differences were statistically significant (P < 0.01 and P = 0.003, respectively).24 Unfortunately, no detailed information regarding the mode of biliary complications (eg, leakage or leakage after T-tube removal) or the onset of biliary complications in each group (late strictures versus early strictures) was reported. In addition, the follow-up was very short, and neither patient nor graft survival rates were presented.
Scatton et al.23 in 2001 performed a multicenter, prospective, randomized controlled trial in France that included 6 transplant centers. One hundred eighty patients underwent OLT with choledochocholedochostomy between January 1994 and April 1997. They were randomized into 2 groups with 90 patients each: 1 group received an end-to-end choledochocholedochostomy with T-tubes (rubber T-tubes), and the other group underwent reconstruction without a T-tube. End-to-end choledochocholedochostomy was performed with interrupted PDS. T-tubes were clamped 7 to 14 days after OLT after cholangiography. T-tube removal was scheduled 90 days after OLT. The mean follow-up was 21.5 months in the T-tube group and 21.3 months in the no–T-tube group. University of Wisconsin solution was routinely used for organ preservation. Retransplantation, reduced size liver, and age under 18 years were exclusion criteria. The cold ischemic time was not an exclusion criterion.
One patient, randomized to the T-tube group, received a hepaticojejunostomy but was not excluded from the analysis. The overall biliary complication rate was 33.3% in the T-tube group (60% were directly related to the presence of a T-tube) versus 15.5% in the group without a T-tube (P < 0.005). The survival rate was 72.8% in the T-tube group and 80.1% in the group without a T-tube (statistically not significant). Retransplantation was necessary in 4 patients (4.4%) in the T-tube group and in 3 patients (3.3%) in the group without a T-tube.23
Detailed information about biliary complications, including the onset of the biliary complications, is given. In the T-tube group, 60% of all biliary complications were directly related to a T-tube, and the most frequent complication was cholangitis in 11.1%. Cholangitis never occurred in the no–T-tube group. Biliary leakage appeared in 10% of patients with a T-tube versus 2.2% of patients without a T-tube. Seventy-eight percent of the leaks were located at the exit site of the T-tube and occurred after T-tube removal. There was no difference in biliary strictures between the 2 groups. Biliary complications occurred in the first 2 months after OLT in the T-tube group (median delay = 38 days) versus 111 days in the no–T-tube group. The most often occurring complication in the T-tube group was cholangitis, which might be related to a diagnostic procedure (cholangiography) in these patients. Even though the complication rate was higher in the T-tube group, the number of reoperations was equal in the 2 groups (7.7% in the T-tube group versus 8.8% in the no–T-tube group).
In 2007, Amador et al.22 published a cost-effectiveness analysis of T-tube use in OLT. One hundred seven patients undergoing OLT were prospectively randomized to a T-tube group (n = 53) or a no–T-tube group (n = 54) between October 2002 and March 2004. The bile duct anastomosis was made in an end-to-end fashion with a T-tube (9-Fr silicone T-tube) or without a T-tube. The bile duct anastomosis was fashioned with single stitches of PDS 6-0 with an internal argyle 5 catheter in the no–T-tube group. In the T-tube group, the posterior face was performed with PDS 6-0 running sutures before T-tube placement, whereas the anterior face was performed with PDS 6-0 single stitches. University of Wisconsin solution was routinely used for organ preservation. Retransplantation, reduced size liver, and age under 18 years were exclusion criteria as well as a cold ischemic time over 12 hours.
The T-tube was closed 10 days after OLT without previous cholangiography. Removal of the T-tube was performed 3 months after OLT (after previous cholangiography).
The authors reported on an anastomotic bile leak in 6 of 53 patients with a T-tube (11.3%) versus 3 of 54 patients without a T-tube (5.5%). Anastomotic strictures occurred in 4 of 107 patients (3.7%): 1 in the T-tube group and 3 in the no–T-tube group (5.5%). The stricture in the T-tube group was incidental, whereas the patients in the no–T-tube group were treated by repeated dilatations over months, and 1 patient needed surgery. Twenty of 53 patients (37.7%) presented with T-tube–related complications: 10 patients presented biliary leakage after T-tube removal, and 6 of these needed surgery. Eight patients suffered from cholangitis after T-tube removal. The survival rate of patients with a T-tube was 92% after 1 year and 81% after 2 years versus 96% and 88% in the no–T-tube group (log-rank test: P = 0.06). The costs of therapeutic procedures were 28,232 euros in the T-tube group versus 16,088 euros in the no–T-tube group (P < 0.05).22
No information about the onset of biliary complications, except in the case of T-tube–related complications, was presented. The median follow-up was 30 months; however, only early biliary strictures were described.
Most recently, Weiss et al.27 published their trial in which 194 patients had been randomized (n = 99 in the T-tube group versus n = 95 in the no–T-tube group) from 2005 to 2007. Anastomosis was performed as side-to-side choledochocholedochostomy with a running suture with 6-0 Prolene for the back wall. Patients in the T-tube group received a 2.5-mm rubber T-tube. Follow-up was performed 7 days and 3, 6, and 12 months after OLT. The T-tube was removed after 6 weeks.
Although the rates of biliary leakage and strictures were not different between the 2 groups, the number of overall biliary complications was significantly higher in the no–T-tube group. Interestingly, this was a result of more frequently occurring acute pancreatitis and cholangitis in this group of patients due to more invasive diagnostics (eg, endoscopic retrograde cholangiography). Therefore, the conclusion to generally use a T-tube after OLT is not convincing.
Because the follow-up was short, no information about late biliary complications was obtained.
Because the prospective, randomized studies used a number of different endpoints (except for the rate of biliary complications), a meta-analysis of only biliary complications (biliary leaks/fistulas, biliary stenoses/strictures, and cholangitis in detail) and mortality was performed. In all, 322 patients in the T-tube group and 317 patients in the no–T-tube group were analyzed. A comparison of the total number of overall biliary complications revealed 99 events (ie, complications) in the T-tube group and 92 events in the no–T-tube group. This difference was statistically not significant (OR = 1.15, 95% CI = 0.28-4.72, Z = 0.19, P = 0.85; Fig. 2). A detailed analysis of the biliary complications revealed that biliary leaks developed in 24 patients in the T-tube group and in 22 patients in the no–T-tube group (OR = 1.17, 95% CI = 0.4-3.47, Z = 0.29, P = 0.77; Fig. 3). Conversely, biliary strictures were significantly more common in the group of patients that underwent reconstruction without a T-tube (14 versus 31 events; OR = 0.46, 95% CI = 0.23-0.9, Z = 2.26, P = 0.02; Fig. 4).
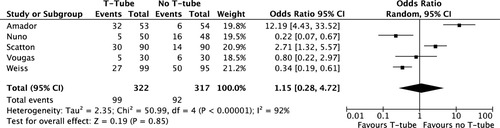
Overall biliary complications. OR estimates for overall biliary complications in the groups of patients with or without a T-tube were calculated with the random effects model. The diamond represents the overall treatment effect from the pooled studies spanning the 95% CI. The complication rate was not different between the groups (test for overall effect: Z = 0.19, P = 0.85). Values in parentheses are 95% CIs.
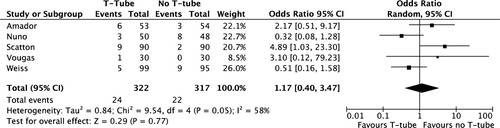
Biliary leakage. OR estimates for biliary leakage in the groups of patients with or without a T-tube were calculated with the random effects model. The diamond represents the overall treatment effect from the pooled studies spanning the 95% CI. The leakage rates were comparable between the groups (T-tube versus no T-tube; overall effect: Z = 0.29, P = 0.77). Values in parentheses are 95% CIs.

Biliary strictures. OR estimates for biliary strictures in the groups of patients with or without a T-tube were calculated with the random effects model. The diamond represents the overall treatment effect from the pooled studies spanning the 95% CI. The stricture rates were significantly lower in the T-tube group (overall effect: Z = 2.26, P = 0.02). Values in parentheses are 95% CIs.
DISCUSSION
Different techniques for comparable reconstructions are a matter of discussion in all fields of surgery. Biliary anastomosis and biliary tract complications remain a major surgical challenge after liver transplantation.41, 47, 48 Despite the advances in liver transplantation techniques, the incidence of biliary complications still ranges from 10% to 60%.4, 21, 23, 49, 50 Although there do not seem to be any differences between side-to-side and end-to-end bile duct anastomoses,3, 5, 6 the use of a T-tube is controversial.23, 25, 36 This systematic review and meta-analysis have been performed to increase the power of the single prospective studies analyzing whether a T-tube should be used for the reconstruction of the biliary tree in OLT. This detailed and systematic analysis of the retrospective studies has demonstrated an incoherent picture, with some studies suggesting benefits of using a T-tube and others arguing against such a reconstruction. Important advantages of using a T-tube are the facilitated monitoring of the quality and quantity of the produced bile as parameters of the function of the transplanted liver and the easy access for radiographic imaging of the biliary tree. Furthermore, T-tubes have been thought to protect the biliary anastomosis (ie, the duct-to-duct choledochocholedochostomy) by reducing the intraductal pressure, and some authors have also suggested that T-tubes might protect against the development of late bile duct strictures.49, 51
In the last years, there has been a shift toward abandoning the use of T-tubes for reconstruction of the biliary tract because some studies from the 1990s showed higher rates of biliary complications in patients with a T-tube and especially an increase in the risk of biliary leakage after T-tube removal with a subsequently high incidence of bile-induced peritonitis.6, 40, 52 Increased rates of biliary/anastomotic strictures after T-tube reconstruction were reported, whereas only in a small number of the retrospective reviews from this time was protection of the anastomosis found. Furthermore, the risks derived from the T-tube itself, such as cholangitis, biliary obstruction, and tube migration, seemed to outweigh the potential benefits, and this is underlined by the compound data of a number of studies showing that 10% to 60% of all postoperative biliary complications may be directly related to T-tubes.5, 23, 53 In addition to the clinically relevant differences, Amador and coworkers22 recently published a cost-effectiveness analysis that quite clearly argues against the use of a T-tube, not only because more bile leaks were found in the T-tube group but also because of the much higher costs when reconstruction with a T-tube was performed (28,232 euros in the T-tube group versus 16,088 euros in the no–T-tube group). Yet in the particular case of living donor–related liver transplantation (when there is a resection surface), the use of the T-tube might be beneficial because it seems to reduce intraductal pressure and thus the risk of a bile leak from the resection surface.9, 45, 46, 54, 55
In our meta-analysis and systematic review of whether or not a T-tube should be used in the reconstruction of the biliary tract during OLT, choledochocholedochostomy without a T-tube was not associated with a higher rate of biliary complications. However, and as expected, biliary strictures occurred significantly less frequently (or were probably at least delayed) when a T-tube was used. This would be in line with what has been known for a long time in (nontransplant) biliary tract surgery, in which placement of a T-tube usually prevents scarring of the anastomosis. However, how important is the problem of anastomotic scarring? Of 639 patients, only 17 (2%) benefited from a T-tube (in terms of developing no biliary stricture); 37 T-tubes will have to be placed to prevent 1 additional stricture. Whether or not the biliary tree will be reconstructed with a T-tube will thus much depend on the preference of a given transplant center. Although a T-tube remains an excellent tool for monitoring bile excretion (and also graft function), this may also be noninvasively accomplished with factor V determination or the indocyanine green elimination rate.
In conclusion, data on T-tube reconstruction in OLT are not unambiguous. With respect to the development of biliary strictures, there is a significant benefit in placing a T-tube. Furthermore, this may have the potential to reduce long-term morbidity because strictures can recur even years after the event and initial treatment. However, the surgeons in charge will still have to decide more according to preference than evidence.