Acute liver failure in Spain: Analysis of 267 cases
Abstract
The cause of acute liver failure (ALF) is a major determinant of its outcome. Acetaminophen (paracetamol) overdose is a leading cause of ALF in some developed countries, whereas in others, such as Spain, it is extremely rare. To analyze the etiology, characteristics, and outcome of ALF in Spain, we performed a retrospective analysis of 267 patients whom we observed from 1992 to 2000. Seventeen tertiary-care hospitals with active liver transplantation (LT) programs contributed data. Causes of ALF were viral hepatitis in 98 (37%; hepatitis B virus in 75 patients), unknown in 86 (32%), drug or toxic reactions in 52 (19.5%; acetaminophen overdose in 6), and miscellaneous in 31 (11.6%). Overall survival was 58%. LT was performed in 150 patients, with a survival of 69%. Despite fulfilling criteria, 51 patients were not transplanted because of contraindications; their survival was only 7.8%. Forty-seven (85.5%) of 55 patients without transplant criteria survived. Hepatitis B virus is the most common cause of ALF in Spain, although the origin of 30% of cases remains undetermined. Acetaminophen overdose represents a very rare cause of ALF. LT was performed in >50% of cases. Patients without transplant criteria had a very good prognosis; those who fulfilled these criteria but who had contraindications for transplantation had a high mortality rate. Liver Transpl, 2007. © 2007 AASLD.
Acute liver failure (ALF) is a syndrome characterized by the development of hepatic encephalopathy (HE) together with signs of hepatocellular insufficiency, especially jaundice and coagulation disorders, in patients without previous liver disease.1 The prognosis of this serious disorder improved dramatically with the introduction of orthotopic liver transplantation (OLT) in the late 1980s.
Epidemiological studies have pointed out that ALF is a wide, heterogeneous syndrome involving several diseases with different patterns, prognoses, and outcomes. Furthermore, marked geographical differences have been identified, making the translation of data from one area to another difficult.2 In fact, most studies are from the United States (one of the studies involving the whole country)3-6 and the United Kingdom (studies from single centers),7, 8 where acetaminophen (paracetamol) overdose accounts for 20-75% of all ALF cases.3-8 There is general agreement that these figures are markedly reduced in countries, such as Spain, in which attempts at suicide by acetaminophen are anecdotal, a result of ignorance and the fact that acetaminophen is not available over the counter.9-11 This difference, as well as its effect on the outcome of ALF (far better in ALF due to acetaminophen ingestion3, 4, 12 and hepatitis A3, 4, 13 than in ALF due to other causes) in countries other than the United States, the United Kingdom, and eastern countries, has been poorly investigated.
The aim of the present study was to investigate the clinical characteristics (including epidemiology and etiology) and outcome of what is to date the most extensive series of patients with ALF ever studied in Spain.
Abbreviations
ALF, acute liver failure; LT, liver transplantation; HE, hepatic encephalopathy; OLT, orthotopic liver transplantation; HBV, hepatitis B virus.
PATIENTS AND METHODS
A questionnaire was given to hepatologists in 27 hospitals around Spain to ascertain how many patients with ALF were recorded from January 1, 1992, to December 31, 2000. All the centers involved had liver units and were either referral centers for liver patients or liver transplantation (LT) centers with at least 2 years' experience in OLT. One doctor from each liver unit collected all the cases handled in the unit during the period of study. Each case was identified with the patient's name, date of birth, and hospital ID to avoid duplication. Diagnosis of ALF was established according to clinical, analytical, and histological criteria, if available. ALF was identified in the first health care center following the accepted criteria: acute, life-threatening deterioration of liver function in the absence of preexisting liver disease characterized by the presence of jaundice, impairment in liver function determined by the prothrombin time (prothrombin index <40% or international normalized ratio of prothrombin time ≥1.5), and encephalopathy, which can be a late symptom. In all cases, data from all patients fulfilling these criteria were collected, regardless of age, suspected cause of ALF, or comorbidities. ALF was classified as fulminant when HE appeared within the first 2 weeks after the onset of jaundice and as subfulminant when appearing between weeks 3 and 8.14 In addition, patients were also classified according to the O'Grady classification15 as having hyperacute, acute, or subacute impairment.
We requested information for all patients admitted at each center who met this definition. The following variables were recorded: demographic, clinical, laboratory, and outcome data including LT, death, and survival without OLT within the current admission. Etiologic diagnoses were made at each study center on the basis of accepted diagnostic criteria including clinical history, laboratory values, imaging studies, and, in some cases, histologic characteristics. ALF was considered to be indeterminate when clinical, laboratory evaluations (including toxicological screening, serologic markers for viral hepatitis A, B, and C, and autoantibodies), and imaging studies were inconclusive.
The management of the whole series of patients, although determined at each site, was uniform and followed accepted published guidelines. In summary, it includes prevention of hypoglycemia, bacterial and fungal infections, upper gastrointestinal tract bleeding, and renal failure; conventional treatment of HE and hypovolemia or hypervolemia; monitoring of hemodynamic (central venous or Swan-Ganz catheter) and oxygen status (SaO2); and monitoring of the intracranial pressure and electroencephalogram waveforms in patients presenting grade III or IV HE, and treating those patients with pathological findings.
All patients, especially those fulfilling criteria for LT, were transferred to a LT unit. Candidacy for LT was determined at each individual center according to the King's College Guidelines16 except for one center, which used the following criteria to define the need for LT: grade III or IV of HE regardless of the patient's clinical evolution; progression of encephalopathy after a transient period of improvement; and absence of improvement after a 3-day period of supportive management in patients with subfulminant ALF and grade I or II HE.17
Spontaneous survival was defined as survival without OLT.
The questionnaires were checked for missing values and inconsistencies at the data coordination center. To assess the annual incidence and the point prevalence of ALF in Spain, each participating center was asked to provide the date of diagnosis of each patient as well as the overall population it served.
Statistical Analysis
Data were entered into an Access database and analyzed by SPSS software (SPSS, Chicago, IL). Data are reported as means with standard deviations. Categorical variables were compared by the Fisher exact test, and continuous variables were compared with the unpaired Student t test (or nonparametric Mann-Whitney rank sum test for unpaired data). The actuarial probability curves were constructed by the Kaplan-Meier method and compared with the log rank test. Statistical significance was established at a P value of <0.05.
RESULTS
Seventeen centers from 11 autonomous communities, covering a population of 21.66 million inhabitants, answered the questionnaire. The total Spanish population on January 1, 2001, was 41.11 million inhabitants. A total of 267 patients with ALF were identified during the 9-year period. We are aware that the retrospective design of our study could be an important pitfall when calculating the incidence of the disease. In fact, we know that we lost patients from the 10 centers because they did not give us their data, and we probably lost data from other hospitals when they failed to refer their patients to LT centers, mostly because the patients had severe comorbidities that conferred a poor prognosis. Taking into account these limitations, the estimated incidence of ALF during the study period was of 1.4 cases per million inhabitants per year.
Demographic Characteristics and Clinical Data
Age at diagnosis varied widely, from 1 to 79 years (mean, 36.8 years), with 57% of patients younger than 40 at presentation. Twenty patients were children (≤14 years). One hundred eighteen patients (44%) were male. All patients but 7 (2.7%) were Spanish (although all except one were white).
Fulminant hepatic failure accounted for 60% of cases; 37% were subfulminant. According to O'Grady's classification, 42% were hyperacute, 38% acute, and 16% subacute. Time from jaundice to encephalopathy could not be accurately established in 9 cases.
At presentation, grade I HE was the most frequent finding (48%), with only 13% of the patients presenting deep coma (grade IV HE), although these figures reversed during follow-up (40% of the patients developed grade IV, whereas 16% remained in grade I). The mean interval from onset of symptoms to encephalopathy was 15.8 ± 17 days.
It is of note that 15 patients (5.6%) had no HE at presentation but developed it during admission.
Causes of ALF
Viral hepatitis was the most frequent cause of ALF, accounting for 98 patients (37%). Among these 98 patients, 75 (28%) had acute hepatitis B, 11 (4%) had hepatitis B and D, and acute hepatitis A and C accounted for 5 (2%) patients each. Two patients had nonhepatotrophic viruses causing ALF.
Cryptogenic/indeterminate liver failure was the second most common cause of ALF involving 86 patients (32.2%).
Drug or toxic reactions were responsible for 52 cases (19.5%) of ALF. Acetaminophen was the less commonly implicated drug, being responsible for only 6 cases (2.2%). Idiosyncratic reactions to antituberculosis therapy were deemed responsible for 13 cases (4.9%), and Amanita mushroom poisoning was responsible for 10 cases (3.7%). The remaining 23 cases were due to different toxic substances or drugs.
Last, there was a miscellaneous group of 31 patients (11.6%), including 13 cases (4.9%) of autoimmune hepatitis, presenting as ALF; 6 cases (2.2%) of ischemic origin; 8 cases (3%) of a neoplastic infiltration; 2 cases (0.7%) of acute Wilson disease; and 2 cases (0.7%) of acute fatty liver of pregnancy.
There were significant differences in the cause of ALF according to the period of study (P = 0.003). From 1992 to 1995, 61 (42%) of 145 cases were due to viral infection; this percentage fell to 37 (30%) of 122 cases in the next 5 years. Conversely, there was an increase in the incidence of toxic substance– or drug-related ALF during the last period of the study (27% vs. 13% in the former).
Extrahepatic Complications
Sixty-two percent of the patients presented medical complications at admission. The most frequent complication was the development of hypoglycemia (26%) followed by ascites (24%), upper gastrointestinal bleeding (15%), clinical signs of cerebral edema (14.7%), respiratory failure (10%), and overt infection (9%).
During follow-up, the incidence of these complications increased to up to 75% of the patients. Forty-three patients (16%) had intracranial pressure monitoring by an extradural device placed as per protocol (clinical suspicion of cerebral edema or progression to grade III or IV HE). Cerebral edema, diagnosed either by intracranial pressure monitoring or by combined clinical and computed tomography data, was found in 88 patients (33.7%).
Outcome
The overall survival was 155 (58%) of 267 patients (Fig. 1). Two hundred twelve fulfilled criteria for emergency OLT, with 150 receiving a liver graft (56% of the overall series, 71% of those patients fulfilling criteria for transplantation). The survival among this group of transplanted patients was 69.3% (104 patients). Eleven patients died while waiting for a graft (4% of the overall series), and the remaining 51 patients (19.1%) were not transplanted because of contraindications to the procedure. These contraindications were: advanced age (>65 years, 18 cases), expected short-term survival due to concomitant diseases (acquired immunodeficiency syndrome in 4 cases, disseminated cancer in 10 cases), severe active systemic bacterial infections precluding OLT (5 cases), other organ failure (3 cases), or active, repeated, and long-term drug addiction (11 cases, 22% of the group of patients in whom OLT was contraindicated). Four patients in this group survived (Fig. 1).
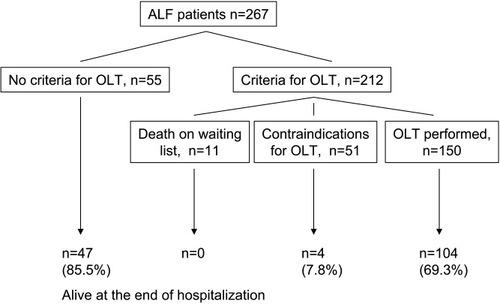
Outcome of 267 patients with acute liver failure.
Fifty-five patients were considered to not fulfill criteria for emergency OLT (Fig. 1). Eight patients of this group (14.5%) finally died from nonhepatic causes; the remaining 47 patients survived (85.5% of the group) (Table 1).
| Variable | Group 1* (OLT criteria) (n = 161) | Group 2 (no OLT criteria) (n = 55) | Group 3 (OLT contraindicated) (n = 51) | P |
|---|---|---|---|---|
| Age (yr), median (range) | 33 (1-69) | 31 (1-78) | 54 (2-79) | 0.0001 |
| Gender (M/F) | 60/101 | 27/28 | 31/20 | 0.009 |
| Days of jaundice-HE, median (range) | 13 (1-120) | 7 (1-48) | 7 (1-39) | 0.0001 |
| HE at admission (%) | 0.015 | |||
| 0 | 11% | 0% | 4% | |
| I | 34% | 59% | 35% | |
| II | 27% | 17% | 31% | |
| III | 17% | 17% | 14% | |
| IV | 11% | 7% | 16% | |
| Hospitalization (days), median (range) | 28 (1-330) | 13 (1-380) | 7 (1-47) | 0.0001 |
| Etiology, n (%) | 0.012 | |||
| Virus | 59 (36.7%) | 22 (40%) | 17 (33.3%) | |
| Toxic | 24 (14.9%) | 13 (23.6%) | 15 (29.4%) | |
| Unknown | 63 (39.1%) | 9 (16.4%) | 14 (27.5%) | |
| Other | 15 (9.3%) | 11 (20%) | 5 (9.8%) | |
| Viral ALF, n (% of all series) | NS | |||
| HBV | 44 (27.3%) | 15 (27.2%) | 16 (31.4%) | |
| HBV+HDV | 7 (4.3%) | 4 (7.3%) | 0 | |
| HAV | 3 (1.9%) | 2 (3.6%) | 0 | |
| HCV | 5 (3.1%) | 0 | 0 | |
| Other viruses | 0 | 1 (1.8%) | 1 (2%) | |
| Complications during admission, n (%) | ||||
| Hypoglycemia | 38 (24.4%) | 14 (26.4%) | 23 (46.9%) | 0.009 |
| Bleeding | 18 (11.5%) | 7 (13%) | 16 (32.7%) | 0.002 |
| CRRT needed | 12 (7.7%) | 4 (7.4%) | 6 (12%) | NS |
| Respiratory failure | 23 (14.6%) | 7 (13%) | 17 (34.7%) | 0.003 |
| Severe infections | 29 (18.7%) | 17 (31.7%) | 28 (56%) | 0.0001 |
| Cerebral edema | 64 (40.5%) | 6 (11.1%) | 18 (36.7%) | 0.0001 |
| Shock | 11 (7.2%) | 4 (7.5%) | 21 (42.9%) | 0.0001 |
| Coma (grade IV HE) | 10 (18.9%) | 60 (37.3%) | 37 (74%) | 0.0001 |
| Outcome (end of hospitalization), n (%) | 0.0001 | |||
| Alive | 104 (64.6%) | 47 (85.5%) | 4 (7.8%) | |
| Dead | 57 (35.4%) | 8 (14.5%) | 47 (92.2%) |
- Abbreviations: OLT, orthotopic liver transplantation; HE, hepatic encephalopathy; ALF, acute liver failure; HBV, hepatitis B virus; HDV, hepatitis D virus; HAV, hepatitis A virus; HCV, hepatitis C virus; CRRT, continuous renal replacement therapy.
- * Group 1 included those patients listed for emergency OLT but who died while waiting for a graft.
Emergency OLT Status Comparison
According to the presence or absence of criteria to perform emergency OLT, patients could be classified as those fulfilling OLT criteria and entering the waiting list (group 1), those not fulfilling OLT criteria (group 2), or those who, despite reaching OLT criteria, could not be transplanted because of contraindications to the procedure (group 3). Group 1 included 150 patients who received liver grafts (Table 2), and 11 died while waiting for a liver.
| Variable | OLT (n = 150) | No OLT (n = 62) | P |
|---|---|---|---|
| Age (yr), median (range) | 32 (1-69) | 50 (2-79) | 0.0001 |
| Gender (M/F) | 55/95 | 36/26 | 0.004 |
| Days of jaundice-HE, median (range) | 14 (1-120) | 7 (1-56) | 0.003 |
| HE at admission (%) | NS | ||
| 0 | 12% | 3% | |
| I | 33% | 37% | |
| II | 28% | 27% | |
| III | 16% | 18% | |
| IV | 11% | 14% | |
| Hospitalization (days), median (range) | 30 (2-330) | 6 (1-47) | 0.0001 |
| Etiology, n (%) | NS | ||
| Virus | 56 (37.3%) | 20 (32.3%) | |
| Toxic | 21 (14%) | 18 (29%) | |
| Unknown | 59 (39.3%) | 18 (29%) | |
| Other | 14 (9.3%) | 6 (9.7%) | |
| Viral ALF, n (% of all series) | NS | ||
| HBV | 41 (27.3%) | 19 (30.6%) | |
| HBV+HDV | 7 (4.7%) | 0 | |
| HAV | 3 (2%) | 0 | |
| HCV | 5 (3.3%) | 0 | |
| Other viruses | 0 | 1 (1.6%) | |
| Complications during admission, n (%) | |||
| Hypoglycemia | 35 (24.1%) | 26 (43.3%) | 0.006 |
| Bleeding | 14 (9.7%) | 20 (33.3%) | 0.0001 |
| CRRT needed | 8 (5.5%) | 10 (16.4%) | 0.012 |
| Respiratory failure | 18 (12.3%) | 22 (36.7%) | 0.0001 |
| Severe infections | 27 (18.8%) | 30 (49.2%) | 0.0001 |
| Cerebral edema | 56 (38.1%) | 26 (43.3%) | NS |
| Shock | 7 (4.9%) | 25 (42.4%) | 0.0001 |
| Coma (grade IV HE) | 53 (35.3%) | 44 (72.1%) | 0.0001 |
| Outcome (end of hospitalization), n (%) | 0.0001 | ||
| Alive | 104 (69.3%) | 4 (6.5%) | |
| Dead | 46 (30.7%) | 58 (93.5%) |
- Abbreviations: OLT, orthotopic liver transplantation; HE, hepatic encephalopathy; ALF, acute liver failure; HBV, hepatitis B virus; HDV, hepatitis D virus; HAV, hepatitis A virus; HCV, hepatitis C virus; CRRT, continuous renal replacement therapy.
- * Patients actually transplanted (OLT) or not (no OLT, including patients with contraindications to OLT and those who died while on the waiting list).
In the group of transplanted patients, the median time from listing to actual OLT was 39 ± 39 hours. Eighty-three patients underwent OLT 24 hours or less after inclusion on the waiting list (51.5% of the 161 patients listed for emergency OLT, 11 of whom died before receiving the graft). The mean age of the transplanted patients was 34 ± 17 years, and 63% were women. The main cause was unknown (in 39% of the cases) followed by hepatitis B virus (HBV)-related ALF (27%). HE was predominantly mild (grade I) at admission, although it changed to grade II to IV during follow-up with no differences compared with the overall series of patients. As expected, these transplanted patients experienced fewer complications during follow-up than those not receiving OLT despite its being indicated (Tables 1 and 2).
The patients not receiving a liver graft because of contraindications to OLT were predominantly men (60%) with a mean age of 48 ± 21 years. The main cause of ALF in this group was HBV (Table 1). The incidence of complications, both at admission and during follow-up, was higher in this group compared with the overall series and the patients receiving OLT. Liver function tests and other analytical parameters were similar in the 2 groups (data not shown).
Patients who did not fulfill criteria for LT were equally distributed by gender (1:1), with a mean age of 34 ± 16 years. As in the other groups, the main cause was HBV-related ALF. Complications were less frequently observed both at admission and during follow-up (Table 1). Prothrombin time remained lower compared with the other 2 groups of patients throughout hospitalization (25.9 ± 19% vs. 16.6 ± 10.8% in patients of group 1 vs. 14.9 ± 9.9% in patients of group 3; P < 0.0001). There were no statistically significant differences in other analytical parameters (data not shown).
When we excluded data from patients from the center without the use of the King's College Criteria to define the need for emergency LT, the results did not differ.
DISCUSSION
At present, large, published epidemiological studies on ALF involving more than a single center (national surveys) have only been performed with Anglo-Saxon populations3-8 and in Eastern countries.9, 11 The observed discrepancies in the management and prognosis of ALF patients may be the result of differences in etiologies (i.e., acetaminophen in the United Kingdom and the United States, and hepatitis E in India) and in the capacity to perform emergency OLT. It is important to emphasize that etiology may be a key factor determining the outcome of these patients, even in developed countries with facilities for emergency OLT. Acetaminophen overdose, either accidental or with suicidal intent, is the major cause of ALF in the United Kingdom (50-70%),7, 8 and it accounts for a high proportion of cases in the United States (19-39%).3-6 This etiology clearly differs from others because it carries a better prognosis,3, 4, 12 results in a lower likelihood of LT in cases with indication for emergency OLT (mainly as a result of psychiatric contraindications), and has a specific and effective treatment.12, 18
The current study analyses the cause and outcome of ALF in Spain. It should be stressed that the retrospective design of the study did not allow us to reach conclusive results, and we recommend careful interpretation until a prospective study can confirm the results. Our data show an extraordinarily low incidence of acetaminophen-related ALF, accounting for <2.5% of cases. These results clearly contrast with those observed in Anglo-Saxon3-8 and other non–Anglo-Saxon developed countries (France; J. Bernuau, personal communication), which are seeing a progressive increase of this etiology. The low incidence of acetaminophen overdose is probably because in Spain, it is rarely used as a method of suicide, and because acetaminophen is not an over-the-counter drug, as it is in other countries.
The main causes of ALF in Spain are HBV infection and cryptogenic or indeterminate causes. Two-thirds of our cases were due to these 2 causes. Toxic substances or drugs other than acetaminophen, mainly antituberculosis drugs, were responsible for nearly 20% of the cases. Because all these causes result in a worse prognosis than acetaminophen overdose and infection with hepatitis A or E, the global expected death rate in cases not receiving emergency OLT in our series would have been high. In a series from one of the participating centers before the OLT era, the overall mortality was 78.4%.19 Thus, considering that all 212 patients who fulfilled OLT criteria had a >90% probability of dying (93.5%, Table 2) if they did not undergo OLT, the expected mortality rate in our whole series of patients would be 77.1%. This figure is in keeping with the mortality reported in drug-induced ALF (75%) and ALF of indeterminate origin (83%) if emergency OLT is not performed, and it clearly contrasts with the spontaneous survival of acetaminophen-related ALF in recently published series in the United States (68%).3
As shown in the Results, the incidence of viral ALF decreased in the course of the study. This decrease would tend to increase during the next few years as a result of the introduction of HBV vaccination. HBV vaccine was introduced as universal and mandatory in young adolescents in 1991, but it was not uniformly performed throughout the country. Unfortunately, no information regarding the profile of ALF in Spain after universal HBV vaccination is available yet.
The prognosis of ALF has been dramatically changed by the introduction of emergency OLT. In this sense, the overall survival observed in our patients was 58% (35% increase in survival from that expected without emergency OLT). By using the classical King's College criteria for emergency OLT in all centers except one, which applies another previously reported score,17 patients who were not transplanted because they did not fulfill these criteria had an excellent survival (85.5%, Table 1). Moreover, death in this group of patients (8 cases) was due to extrahepatic causes. There were no differences in ALF etiology between patients who did or did not fulfill the criteria for emergency OLT (Table 1).
It is important to note that despite having a very short listing time (<24 hours in nearly half of the listed patients), 11 patients died while waiting for a graft. This figure is nevertheless clearly lower than that observed in United States, where >30% of patients listed for emergency OLT died while waiting for a graft.3 The differences may be the result of the Spanish policy for obtaining and distributing liver grafts. When one patient enters the waiting list because of ALF, a “0 alert” is activated, and therefore, the first cadaveric liver available in the country goes to this patient, even if it is not compatible (although we usually wait for a compatible organ). By following this policy, the median time on the waiting list for ALF patients (including primary liver dysfunction after elective OLT) in 2005 was of 3.5 days (range, 1-98 days), with 71% of the grafts ABO compatible (National Transplant Organization, ONT, Liver Transplantation Report 2005). However, the objective should be no deaths on waiting list. That is why we consider it to be extremely important to transfer patients with severe acute hepatitis to transplant centers as soon as possible for inclusion on the waiting list immediately after identifying the need for emergency OLT. Furthermore, it should be remembered that “the liver fails before encephalopathy.”20 Consequently, 15 patients in our series (5.6%) showed no encephalopathy at admission but developed it while hospitalized.
Fifty-one patients were not listed for emergency OLT despite fulfilling the criteria because of contraindications to the procedure. Some of these contraindications, but not all, were unavoidable. Others, such as active and severe infections, brain edema, and multiorgan failure, were of note mainly because there are efficient preventive and therapeutic maneuvers that nowadays should be applied in all patients with ALF. The need to know and apply these measures, as well as others directed at specifically preventing liver damage, means that we highly recommend the transfer of these patients to LT units at diagnosis.
In summary, acute HBV infection is the most common cause of ALF in Spain, followed by drug or toxic reactions. Among those, acetaminophen overdose represents a very rare cause. It is of note that, despite an exhaustive search for possible etiologies, >30% of cases remain of undetermined origin. LT was highly applicable in those patients fulfilling emergency OLT criteria (>70%) with a good survival rate. Patients who did not reach transplant criteria had a very good prognosis. On the other hand, patients with OLT criteria but with contraindications for transplantation showed an extremely poor prognosis.
These results should be considered cautiously because of the retrospective design and the need to the findings to be confirmed by a prospective study. The future study should focus on the possible changes in both the etiology of ALF (the role of HBV after the introduction of HBV vaccine as well as the drugs most commonly involved in ALF) and its outcome (e.g., applicability and results of artificial liver support or albumin dialysis, improvement of the criteria for emergency OLT).
Acknowledgements
The Spanish Group for the Study of Acute Liver Failure includes: Hospital Clínic, Barcelona: J. Tost, J.M. Salmeron, J. Fernàndez; Hospital Reina Sofía, Córdoba: J.L. Montero; Hospital Universitari La Fe, Valencia: J. Berenguer; Hospital 12 de Octubre, Madrid: G. Castellano; Arantzazu Ospitalea, Donostia: A. Castiella; Hospital Puerta del Mar, Cádiz: F. Díaz; Hospital Universitario Marqués de Valdecilla, Santander: E. Fábrega; Clínica Universitaria, Pamplona: J.I. Herrero; Hospital Infantil La Paz, Madrid: P. Jara; Hospital Virgen de las Nieves, Granada: R. Martín-Vivaldi; Complexo Hospitalario Juan Canalejo, A. Coruña: A. Otero; Hospital Central de Asturias, Oviedo: L. Rodrigo; Hospital, Vigo: D. Rodríguez; Hospital Gregorio Marañón, Madrid: M. Romero Portales; Hospital Son Dureta, Ciutat de Mallorca: P. Vaquer; Hospital Universitari Vall d'Hebron, Barcelona: V. Vargas; Hospital Universitario del Río Hortega, Valladolid: R. Velicia.




