The pediatric end-stage liver disease (PELD) model as a predictor of survival benefit and posttransplant survival in pediatric liver transplant recipients
Abstract
The pediatric end-stage liver disease (PELD) model accurately estimates 90-day waitlist mortality for pediatric liver transplant candidates, but it has been unclear if PELD can identify patients who will derive survival benefit from undergoing liver transplantation (LT), if it correlates with posttransplant survival, or if it can identify patients for whom LT would be futile. Pediatric patients who underwent LT between 2001 and 2004 were enrolled through the United Network for Organ Sharing Organ Procurement and Transplant Network database. Survival benefit was measured in terms of life-years gained during the first year after LT. Complete data were available for 1,247 patients: 53% were listed as Status 1 at the time of orthotopic liver transplantation (OLT), while the remaining 47% had PELD scores. Only in patients with a PELD of 17+ or those designated as United Network for Organ Sharing Status 1 derived a survival benefit within 1 year of LT; patients with a PELD score of ≤16 did not. In addition, a statistically significant association was seen between 1-year post-OLT survival and PELD at LT (P = 0.03). No “threshold” PELD score, beyond which risk of post-LT mortality increased dramatically, was apparent. In conclusion, pediatric patients with a PELD score of 17+ derive survival benefit early after LT, and increasing PELD scores are associated with increasing transplant benefit after liver transplantation. PELD does correlate with posttransplant survival but should not be used as a marker for futility. Liver Transpl 12:475–480, 2006. © 2006 AASLD.
The Pediatric End-Stage Liver Disease (PELD) model was implemented in February of 2002 as an improved algorithm for allocating livers among pediatric orthotopic liver transplant (OLT) candidates. This model has been validated using an independent historical cohort of pediatric liver transplant candidates from a single institution and is currently being prospectively validated using national data. While it appears to be an accurate predictor of waitlist mortality, the PELD may have other uses, such as predicting post-OLT survival or identifying patients who are either too sick or too well to undergo liver transplantation.1, 2
Using a large national transplant registry, we performed the study described herein to examine the relationship between risk of pretransplant mortality (as determined by PELD score) and posttransplant outcome in the pediatric liver transplant population. In addition, we examine the “ΔPELD” and whether an upper-threshold PELD score defines futility in pediatric liver transplantation. Finally, we compared pretransplant (i.e., waiting list) and posttransplant survival for patients with various PELD scores to determine if minimum and maximum PELD values should be used as criteria for listing pediatric patients for transplantation.
Abbreviations
PELD, pediatric end-stage liver disease; OLT, orthotopic liver transplant; UNOS, United Network for Organ Sharing; LYG, life-years gained; MELD, model for end-stage liver disease.
PATIENTS AND METHODS
Patient Population and PELD Scores
Patients analyzed in this study were enrolled through the United Network for Organ Sharing (UNOS) Organ Procurement and Transplantation Network database. All patients ≤16 years of age who underwent primary liver transplantation after February of 2002 were included. Recipients of multiorgan transplants were excluded. PELD scores or UNOS Status 1 classification at the time of OLT were used for most analyses. A Δ PELD score was calculated as the difference between PELD score at the time of OLT and PELD score at the time of registration. PELD scores used in this analysis were “uncapped.” Survival data, recorded for all waiting list and transplant patients in the database, were then used for Kaplan-Meier product-limit estimates of waiting list and posttransplant survival.
Statistical Analysis
Life-years gained (LYG) were calculated as the area between the pretransplant (i.e., waiting list) survival curve and the posttransplant survival curve during the first year after listing for transplantation or after liver transplantation, respectively. In all cases, the actual (rather than predicted) survival function was used for calculations. LYG calculations are expressed as a percentage of 1 year. Cox univariate analyses were used to find determine a relationship between post-OLT survival and PELD score. SPSS version 11.0 (SPSS Corporation, Chicago, IL) was used for all statistical analyses. A P value of <0.05 was considered statistically significant.
RESULTS
Patient Demographics
Complete data were available for 1,247 pediatric OLT recipients. The median age of these patients was 2 years (range, <1 year to 16 years). Approximately 31% were younger than 1 year of age at the time of OLT, and an additional 19% were between 1 and 2 years of age.
A total of 666 recipients (53%) were listed as Status 1 at the time of OLT, while the remaining 581 (47%) had PELD scores. The median PELD score of this latter group at the time of OLT was 17 points (range, −11 to 99 points). These patients were divided into quartiles based on PELD score: −11 to 6 points (150 patients, or 12.0% of total patients), 7 to 16 points (139 patients, or 11.1%), 17 to 27 points (145 patients, or 11.6%), and ≥28 points (147 patients, or 11.8%). As demonstrated in Figure 1, the distribution of PELD scores resembled a normal distribution with a median of 17 points and a standard deviation of 14.1. points.

Histogram demonstrating the frequency of PELD scores at the time of OLT (n = 581). Dotted line represents a normal distribution with a median of 17 points and a standard deviation of 14.1 points.
The Survival Benefit of Liver Transplantation for Pediatric Patients
LYG calculations during the first year after listing for transplantation vs. first year after liver transplantation were performed for each of the 4 strata and the UNOS Status 1 patients to determine the survival benefit of liver transplantation in the pediatric population (Table 1). Patients in the 2 lowest PELD quartiles (viz. PELD of −11 to 6 and PELD of 7 to 16) who underwent transplantation experienced small decreases in LYG (−1.5 and −4.2%, respectively). Patients with PELD scores of 17 to 27 or PELD scores of ≥28 experienced large increases in LYG after transplantation (18.1 and 20.2%, respectively). UNOS Status 1 patients experienced an even higher increase in LYG after transplantation (24.8%) during the first year after transplantation. Further inspection of the pretransplant and posttransplant survival curves of patients with a PELD score of 7 to 16 demonstrated that the decrease in LYG occurred during the first 10 months after transplantation (Fig. 2A); in comparison, patients with a PELD score of 17 to 27 achieved a survival benefit by the first month after transplantation (Fig. 2b).
| Group | 1-Year Waiting List Survival (%) | 1-Year Posttransplant Patient Survival (%) | Life-Years Gained During First Year After Liver Transplantation (%) |
|---|---|---|---|
| PELD −11 to 6 | 86.8 | 93.6 | −1.5 |
| PELD 7 to 16 | 76.3 | 90.9 | −4.2 |
| PELD 17 to 27 | 65.5 | 89.4 | +18.1 |
| PELD ≥28 | 66.1 | 84.6 | +20.2 |
| UNOS Status 1 | 64.7 | 83.2 | +24.8 |
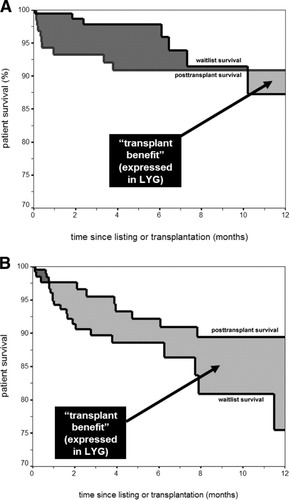
Survival benefit, measured in terms of LYG during the first year after listing vs. liver transplantation, for patients with (A) PELD scores 7 to 16 (n = 347) and (B) PELD scores of 17 to 27 (n = 360) at the time of listing or transplantation. The dark grey area between the 2 curves denotes time when waiting list survival is better than posttransplant survival, while the light grey area between the curves denotes time when waiting list survival is worse than posttransplant survival. As demonstrated by this graph, posttransplant survival does not exceed waitlist survival until 10 months after listing vs. transplantation in patients with a PELD score of 7 to 16. In contrast, posttransplant survival of patients with PELD scores of 17 to 27 exceeds waiting list survival by 1 month after listing/transplantation.
PELD vs. Post-OLT Outcome
The overall 1-year post-OLT patient survival rate for patients 16 years old or younger was 86.2%. Patient survival rates ranged from 93.6% for patients with a PELD score of −11 to 6 points to 84.6% for patients with a PELD score of ≥28 points and 83.2% for patients listed as UNOS Status 1 (Table 2). The 1-year post-OLT patient survival rates were very similar for patients in the PELD 7 to 16 and the PELD 17 to 28 strata (Fig. 3). A Cox univariate analysis demonstrated a significant correlation between PELD score at the time of OLT and post-OLT patient mortality (P = 0.03). In particular, increasing PELD scores at the time of OLT were associated with an increased risk of post-OLT mortality (hazard ratio = 1.023; 95% confidence interval, 1.002 to 1.044).
| Group | Number (% of total) | Median δPELD (range) | 1-Year Post-OLT Survival (%) | |
|---|---|---|---|---|
| Patient | Allograft | |||
| PELD −11 to 6 | 150 (12.0) | 0 (−54 to +9) | 93.6 | 83.0 |
| PELD 7 to 16 | 139 (11.1) | 0 (−13 to +18) | 90.9 | 82.1 |
| PELD 17 to 27 | 145 (11.6) | +7 (−16 to +33) | 89.4 | 83.4 |
| PELD ≥28 | 147 (11.8) | 0 (0 to +81) | 84.6 | 75.9 |
| UNOS Status 1 | 666 (53.4) | Not applicable | 83.2 | 72.7 |
| Overall | 1,247 (100) | +2 (−54 to +81) | 86.2 | 76.6 |

Patient survival rates based on stratified PELD score or UNOS status 1 classification at the time of OLT (n = 1,247).
The overall allograft survival rate at 1-year post-OLT was 76.6%. As with patient survival, allograft survival decreased for each stratum representing increasing PELD scores (Table 1). Those patients with PELD scores ranging from −11 to 6, for example, had a 1-year post-OLT allograft survival rate of 83.0%, while those with a PELD score of ≥28 had a allograft survival rate of 75.9% at 1-year post-OLT and those classified as UNOS Status 1 had a allograft survival rate of 72.7%. A univariate Cox proportional hazards analysis did not show a statistically significant association between PELD and 1-year post-OLT allograft survival (P = 0.22).
Posttransplant length of hospitalization also varied significantly with PELD quartile or UNOS Status 1 designation (Fig. 4). The mean posttransplant length of stay was 15.5 days for patients with a PELD score of −11 to 6, significantly lower than any other PELD quartile (P < 0.05). The mean posttransplant lengths of stay for patients with PELD scores of 7 to 6 and 17 to 27 were 19.0 and 19.5 days, respectively. These lengths of stay were significantly higher than those patients with PELD scores of −11 to 6 (P < 0.05) and significantly lower than patients designated Status 1 (P ≤0.01). Patients in the highest PELD quartile of ≥28 points had a mean posttransplant length of stay of 23.1 days, and patients with a the Status 1 designation had a mean posttransplant length of stay of 25.7 days.
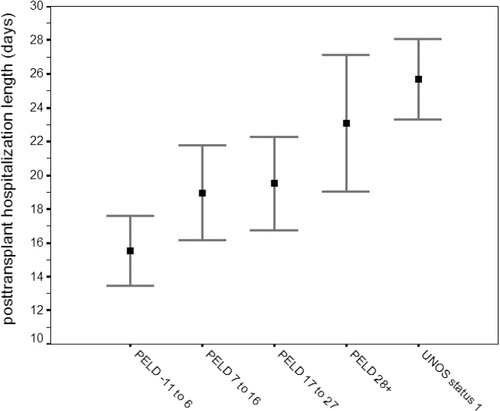
The mean posttransplant length of stay with 95% confidence interval for pediatric patients undergoing primary liver transplantation stratified by PELD score or UNOS Status 1 designation. The 95% confidence interval bars that do not overlap correspond to a P value of <0.05.
ΔPELD vs. Post-OLT Patient Survival
ΔPELD was calculated for all patients for whom a PELD score at listing and a PELD score at OLT was available (n = 394; approximately 68% of all patients with PELD score at the time of OLT). ΔPELD values ranged from −54 to +81 points; the median ΔPELD was 2 points. Two outliers were noted. The first patient had a PELD score that increased from 18 points at the time listing to 99 points at the time of OLT for a ΔPELD of +81 points. The second patient had a PELD score of 47 points at the time of registration; this decreased to −7 at the time of OLT for a ΔPELD of +54 points. A median ΔPELD of +7 was seen in the PELD 17 to 27 group; the median ΔPELD for all other PELD groups was 0 points.
A Cox univariate analysis was performed to look at the relationship between ΔPELD and patient survival rates 1 year after OLT. This analysis found no significant association between these two variables (P = 0.19). It should be reiterated, however, that 53% of patients included in this study were listed as Status 1 by the time of OLT; this significantly limited the amount of data available for calculation of ΔPELD.
PELD as a Predictor of Futility in Pediatric Liver Transplantation
Although differences in 1-year post-OLT patient survival did exist among various strata, survival of patients in highest pre-OLT risk strata (viz. PELD ≥28 and UNOS Status 1) was good, exceeding 80% at 1 year. Further substratification of very high PELD scores (e.g., PELD 50+, PELD 40+) did not reveal any PELD threshold beyond which post-OLT was poor. As such we could not identify a threshold that would suggest futility in pediatric liver transplantation. It should be noted, however, that this analysis includes only patients who underwent OLT. Patients who are no longer suitable candidates for OLT are typically removed from the waiting list by their clinicians; removal from the waiting list would have prevented their PELD score from being incorporated in this analysis.
DISCUSSION
After the Institute of Medicine determined that waiting time was a poor predictor of liver transplant candidate mortality, the United States Department of Health and Human Services asked the liver transplant community to develop an improved liver allocation algorithm. A UNOS subcommittee responded to this request. The algorithm developed by this committee was based on data from the Studies of Pediatric Liver Transplantation database (EMMES Corporation, Rockville, MD) with the goal of creating an algorithm that was simple, objective, and based on severity of disease rather than occurrence of complications of end-stage liver disease. The Pediatric Severity Scale Model Plus Age model, now renamed the PELD model, was subsequently validated as an accurate predictor of 3-month pretransplant mortality by using an independent, historical cohort of pediatric liver transplant candidates at a large liver transplant center.3 A prospective validation of the score is ongoing,4 but it is felt that PELD is less accurate than the model for end-stage liver disease (MELD).5 Both the MELD and PELD classification systems for liver transplant recipients were implemented on February 27, 2002.
The current study demonstrates several relevant findings. First, like adult liver transplant candidates prioritized using the MELD system,1, 2 the amount of survival benefit derived from liver transplantation varies among patients depending on PELD score. Expressed in terms of LYG, the survival costs of liver transplantation during the first year after transplantation appear to outweigh the survival benefits for pediatric patients with a PELD score of ≤16. Only patients with a PELD score of 17 and above experienced a net increase in LYG during the first year after transplantation. In contrast, patients with a PELD score of 17+ and those designated as UNOS Status 1 derived considerable survival benefit in terms of LYG during the first year after liver transplantation. Thus, while transplanting patients with high PELD scores may compromise posttransplant survival rates, these patients gain much more from liver transplantation than patients with low PELD scores.
A few conclusions may be noted when examining the LYG analysis in the patients with a PELD scores of ≤16. First, the pretransplant and posttransplant survival curves of patients with a PELD score of 16 to 27 intersect at approximately 10 months. This suggests that although pediatric liver transplant recipients in this category have an overall negative LYG during the first year, this initial cost is likely to be offset by survival benefits beyond the first year when transplantation occurs in the context of chronic, progressive liver diseases. Second, a LYG analysis by definition focuses only on survival; quality of life is not taken into consideration in such an analysis. As such, liver transplantation may be indicated for pediatric patients with significant impairment of quality of life due, for example, to intractable pruritis, even though the patient's PELD score may be quite low.
Rather than demonstrating minimum PELD score for transplantation in pediatric patients, we believe that these results underscore the need to promote sharing of liver allografts between local donor service areas and even between UNOS regions for pediatric candidates with a PELD score of 17+. The current practice for allocating livers to pediatric patients gives priority to those designated as Status 1 within the local donation service area; if no patient within this area is listed as Status 1, attempts are made to allocate the organ to patients designated Status 1 within the region or outside of the region. We feel that this practice of sharing between donor service areas and regions should be extended to included patients with PELD scores of 17+ (in descending order of point total). Such a practice would be more closely adherent to the mandate that organ allocation “overcome as much as possible arbitrary geographic barriers to allocation that restrict the allocation of organs to patients with the greatest medical urgency.”6
Second, a statistically significant relationship was seen between PELD and 1-year post-OLT patient survival. In particular, an increased risk of post-OLT survival was seen with increasing MELD scores at the time of OLT. In contrast to patient survival, no association was seen between PELD and allograft survival. Some similar analyses in adults have shown previous studies show a positive association between MELD and post-OLT survival of adult liver transplant recipients,7, 8 but most have reported no correlation.9-12 We were also interested in the relationship between ΔPELD and post-OLT survival. ΔMELD, or absolute change in MELD score during the 25–35 day period prior to OLT, had been introduced by Merion and colleagues, because it was thought the rate of deterioration of a patient may be a better measure of severity of end-stage liver disease that a single MELD measurement.13 Although subsequent studies did not support the incorporation of ΔMELD into the adult liver transplant allocation schema,14, 15 we calculated ΔPELD scores for patients in the current study to determine if rate of deterioration prior to OLT was associated with increased risk of mortality after OLT. We found no association between post-OLT mortality and ΔPELD scores, though we should note that the large proportion of patients listed as Status 1 (rather than with a PELD score) limited the number of patients for whom a ΔPELD score could be calculated.
PELD score at the time of OLT does not appear useful in determining futility. We must acknowledge that this analysis is likely limited by the fact that only patients who underwent OLT were included. Many pediatric patients may have been on the waiting list for liver transplantation at one time, then removed because their transplant clinicians no longer felt that they were appropriate candidates. The data of these patients were not analyzed in analyzing PELD as a determinate of futility. The fact that a large proportion of pediatric patients undergoing OLT are classified as UNOS Status 1 at the time of OLT represents another limitation. Although these patients are all deemed to be in critical need of a liver allograft, it is likely that varying degrees of severity of liver disease exist among these patients. It is entirely possible that a subset of patients within the UNOS Status 1 group may have a rate of post-OLT patient survival much lower than that of other pediatric patients, but this could not be assessed in this study.
Finally, the PELD scoring system has also been criticized for underestimating the severity of illness in pediatric patients. Shneider et al.16 recently described the Mount Sinai experience of using PELD scores in allocation and utilization of liver allografts. In this study, they reported that the PELD scoring system underestimated severity of illness, leading to increased patient waiting time and increased patient morbidity (i.e., ascites, hemorrhage, infectious complications, etc.). Furthermore, the petitioned PELD score was significantly higher than the actual PELD score that the patient received. We have also seen this at our institutional level and would agree with this position and advocate continued improvement in the PELD scoring system for improvement in identifying the patients with the greatest need for transplantation.
In summary, an increase in LYG during the first year after liver transplantation was seen only in pediatric patients listed with a PELD of 17+ or designated at Status 1 at the time of transplantation. Increased local and regional sharing may help further ensure that liver allografts are provided to those pediatric patients who stand to gain the most immediate benefit from liver transplantation. There does appear to be some relationship between pre-OLT severity of liver disease, as measured by PELD and ΔPELD, and post-OLT mortality. The correlation between these 2 measures is small, however. As such, the PELD score is limited in its ability to predict post-OLT mortality in pediatric patients.
Acknowledgements
The authors thank the United Network for Organ Sharing for the data used in this study.