Decision-Making in the Treatment of Idiopathic Subglottic Stenosis: A Survey of Laryngologists
Meeting information: The Fall Voice Conference, Miami, Florida, The United States of America, Oct 21–23, 2021.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Abstract
Objective
Idiopathic subglottic stenosis (iSGS) is a rare condition involving the subglottic larynx and upper trachea, commonly affecting Caucasian females between 30 and 50 years of age. Despite its homogeneous presentation, clinical management for iSGS is yet to be standardized, leading to variability in outcomes between predominant interventions. In recognition of the heterogenicity in iSGS treatment and the need to improve patient outcomes, this study aimed to survey laryngologists to understand the factors influencing clinical decision-making and the incorporation of new treatment modalities for iSGS.
Methods
An online survey was sent to 145 academic laryngologists. The survey assessed respondents' professional backgrounds, experience treating iSGS, treatment algorithms, and how various patient factors affect management.
Results
Of the 87 (60%) laryngologists who responded to the survey, the most common clinical assessments were tracheoscopy/bronchoscopy (96.8%) and pulmonary function tests (43.6%). Endoscopic dilation (ED) was the most common primary treatment offered (97.5%): 28.7% of surveyed laryngologists offer SISI as a primary treatment, and 74.7% perform SISI as a planned postoperative treatment. The most common SISI protocol was repeated injections every 4–6 weeks for a series of 1–3 total injections. Notably, 9.2% perform the Maddern procedure. Routine algorithms of care involving surgery were most often based on prior experience and prior patient outcomes (75.9%) and conversations with colleagues (64.4%). Only 31% report using the same protocol learned during their fellowship training.
Conclusion
This survey highlights significant variation in the management of patients with iSGS. Understanding the factors that influence decision-making may lead to potential standardization in heterogeneous treatment approaches and may improve clinical outcomes.
Level of Evidence
5 Laryngoscope, 134:865–872, 2024
INTRODUCTION
Idiopathic subglottic stenosis (iSGS) is a rare disease with an unclear underlying etiology that nearly exclusively affects middle-aged Caucasian females. It involves circumferential fibrotic stenosis of the subglottic and proximal airway without cartilaginous involvement and has a high rate of recurrence.1, 2 Traditionally, iSGS diagnosis and recurrence are assessed with laryngoscopy, tracheoscopy, or bronchoscopy in the clinic or the operating room (OR). These methods involve using local laryngeal anesthesia and passing a scope beneath the vocal folds to examine the subglottic region. Recently, pulmonary function tests (PFTs) as a diagnostic tool have shown to be reliable and efficient with some surgical predictive value.3-7
Endoscopic dilation (ED) is the mainstay treatment for iSGS but has a high recurrence rate within 3 years.1, 8, 9 Recurrent dilations and the negative impact on patients' quality of life suggest investigation for a more effective adjuvant procedure.1, 10
Recent literature and clinician experiences suggest the potential of serial intralesional steroid injections (SISI) to slow disease recurrence and increase the time interval between dilations.11-15 More recently, endoscopic resection and mucosal reconstitution with epidermal grafting (i.e., the Maddern procedure)16-18 and endoscopic wedge resection with CO2 laser18 have been proposed as alternatives to the traditional cricotracheal resection (CTR) with low surgical complication risks and promising outcomes.19
In recognition of the heterogeneity in iSGS treatment and the need to improve patient outcomes, the North American Airway Collaborative (NoAAC) was established.1 NoAAC has advanced the understanding of iSGS by looking at diagnostic and treatment effectiveness across multiple institutions on a larger scale.1, 4, 10, 18 Single institutions cannot provide optimal algorithms of care, but different algorithms implemented at various institutions demonstrate which approaches can offer benefits in managing iSGS. The treatments used are understood, yet the underlying reasons, motivations for these treatments, and the integration of novel treatments remain unclear. Therefore, the aim of this study is to survey laryngologists to highlight the factors that determine clinical decision-making in the treatment of iSGS and understand how clinicians are incorporating novel treatments.
METHODS
The Institutional Review Board of the University of Southern California approved the study. An electronic survey of 39 questions was designed by a team of four fellowship-trained laryngologists. The designed survey was intended to determine laryngologist protocols and the reasoning behind the choice of treatments for iSGS. The survey assessed respondents' professional backgrounds, experience with treating iSGS, treatment algorithms, and how various patient factors affect management.
Survey
One hundred and forty-five American laryngologists practicing at academic institutions were anonymously surveyed using the web-based survey tool Qualtrics (Qualtrics, Provo, UT) between April 22, 2021, and May 25, 2021. Recipients were selected through a list curated by public sources from all U.S. academic Otolaryngology-Head and Neck Surgery (OHNS) departments. OHNS surgeons who identify as laryngologists or provided laryngology services within their practice were identified through an online search. Recipients who received the survey via email were given two email reminders to complete the survey. Laryngologists who do not treat iSGS as defined in the beginning of the survey were directed to the end of the survey. All responses were voluntary, and no compensation was provided for survey completion.
The participants were asked about their practice length, practice setting, fellowship training, other subspecialty training, NoAAC involvement, and the number of iSGS patients treated annually. Questions involved experiences with in-office tracheoscopy or bronchoscopy, PFTs, patient-reported outcome measures on dyspnea, ED, primary SISI, planned postoperative SISI, CTR, Maddern procedure, and other surgical procedures for the care of patients with iSGS.
Questions included single- or multiple-choice options, open-ended free response, and ranking of values. Questions that did not encapsulate all the possible responses were provided with an “Other” choice followed by an open-ended free response option to specify the answer. Three survey questions required participants to rank answer choices based on level of importance, with “1” being the most important, and increasing numerical values indicating decreasing levels of importance.
The complete list of survey questions can be found in Appendix S1.
Data Analysis
All the data were entered into and analyzed through Microsoft Excel (v. 2210, Microsoft Corp., Redmond, WA). Counts were tallied to determine the number and percentage of participants who indicated a particular option. The free responses were systematically categorized into common themes based on patterns and approved by a second author.
RESULTS
Eighty seven participants completed the entire survey which yielded a completion rate of 60%. Seven participants did not finish the survey, but their responses to the answered questions were included in the analysis.
Professional Background
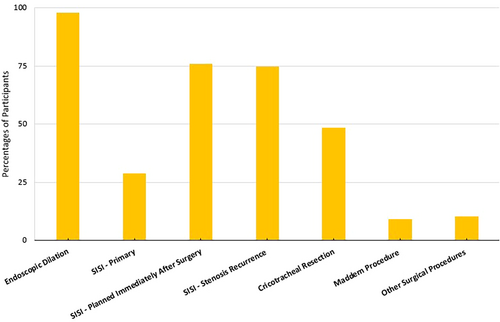
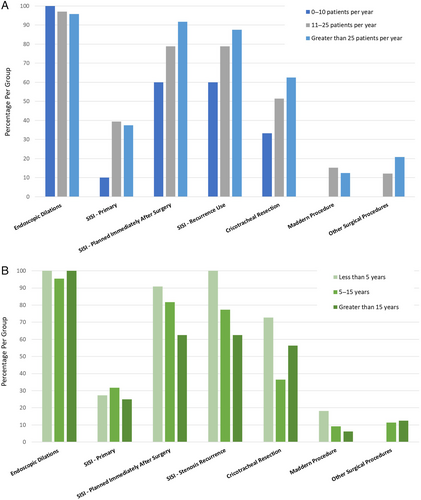
The surveyed laryngologists practice background is summarized in Table I. Types of intervention utilized for the treatment of iSGS can be found in Figure 1. The relationship between a participant's level of experience, approximate annual number of patients diagnosed with iSGS, and type of iSGS intervention employed can be found in Figure 2.
| No. of participants, n (%) | 94 (100) |
| Years in practice | |
| Less than 5 years | 11 (11.7) |
| 5–15 years | 48 (51.1) |
| Greater than 15 years | 35 (37.2) |
| Practice setting | |
| Academic setting | 89 (94.7) |
| Private practice | 1 (1.1) |
| Both academic and private | 4 (4.3) |
| Fellowship training in laryngology | |
| Fellowship-trained | 85 (90.4) |
| Not fellowship-trained | 9 (9.6) |
| NoAAC membership | |
| Member | 40 (42.6) |
| Not member | 54 (57.5) |
| Approximate no. of patients treated with iSGS | |
| 0–10 patients per year | 30 (31.9) |
| 11–25 patients per year | 36 (38.3) |
| Greater than 25 patients per year | 28 (29.8) |
Preoperative Diagnostic Tests
A total of 96.8% (91) of participants perform in-office tracheoscopy or bronchoscopy. Fifty (53.2%) respondents always perform in-office tracheoscopy or bronchoscopy when assessing patients with suspected or confirmed iSGS, and 41 (43.6%) reported only sometimes utilizing this method. The most common indications for these diagnostic assessments were inability to assess the subglottis with flexible laryngoscopy (39, 54.9%), imaging showing complex stenosis with multiple levels (16, 22.5%), and unavailable imaging (13, 18.3%).
Only 43.6% of laryngologists surveyed perform PFTs, with 13.8% always performing them. Of those who utilized PFTs (41, 43.6%), assessments were performed at the pulmonary lab (35, 74.5%) or in the physician's office with handheld device (11, 23.4%). Participants who perform PFTs reported indications such as clarifying the etiology of the patient's symptoms (15, 44.1%) and assessing disease severity (18, 52.9%). Twenty-two (23.4%) routinely had patients perform peak flow measurements at home and 49 (52.1%) reported routinely collecting validated patient-reported outcome measures on dyspnea such as dyspnea index, mMRC Dyspnea scale, or others.
Endoscopic Dilations
Most participants (85, 97.7%) routinely perform ED to treat iSGS (Fig. 1), with only a small percentage (2, 2.3%) opting for alternative procedures such as immediate planned postoperative SISI, primary treatment SISI for recurrence, CTR, and endoscopic wedge resection. Indications for ED were ranked by degree of importance (1 = most important, 5 = least important) by the respondents who offered routine ED for treatment. “Patient-reported symptoms” were ranked as the most important indication for ED (mean = 1.20, std deviation = .50, N = 85), followed by “degree of stenosis” (mean = 1.95, std deviation = .51, N = 85). After ED, 68 (78.2%) participants routinely give medications, most commonly anti-reflux medication (52, 59.8%) and inhaled steroids (41, 47.1%). Oral steroids (27, 31%) and antibiotics (26, 29.9%) were also routinely provided, although to a lesser extent. Seventeen (19.5%) reported not using any additional routine medication following ED procedure.
In-Office Steroid Injections
A total of 83.9% (73) of physicians use in-office SISI for treating iSGS. Twenty-five (34.3%) of them use SISI as a primary intervention before considering an OR intervention. Sixty-six (75.9%) use SISI planned immediately after ED (within 1–3 months) and 65 (74.7%) use SISI for stenosis recurrence after ED (Fig. 1).
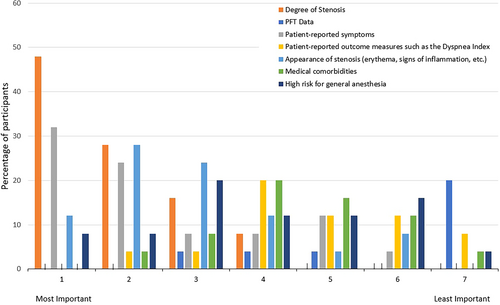
Primary Intervention
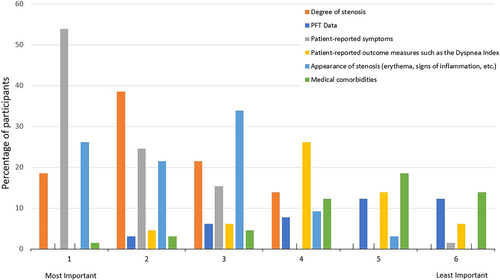
Of the 25 (34.3%) participants who use SISIs as a primary intervention, indications were ranked on degree of importance (1 = most important, 7 = least important). The “degree of stenosis” (mean = 1.84, std deviation = .97, N = 25) was classified as the most important. “Patient-reported symptoms” (mean = 2.50, std deviation = 1.59, N = 22) and “appearance of stenosis” (mean = 2.91, std deviation = 1.41, N = 22) were ranked closely as the second most important (Fig. 3).
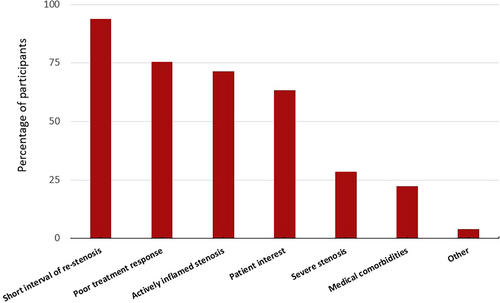
Planned Following Endoscopic Dilation
Seventeen (19.5%) participants always perform SISI as a planned procedure following ED and 49 (56.3%) perform them sometimes. The 49 participants who reported “sometimes performing planned SISI following ED” provided their reasons for doing so, with the most common reason being a previous history of short intervals of restenosis after ED (46, 93.9%) (Fig. 4).
Use for Stenosis Recurrence
Of the 65 (74.7%) participants who use SISI for recurrent stenosis after ED, indications were ranked by degree of importance (1 = most important, 6 = least important) (Fig. 5). “Patient-reported symptoms” (mean = 1.66, SD = .93, 62) was the most important indicator. The “degree of stenosis” (mean = 2.33, SD = .96, N = 60) and “appearance of stenosis” (mean = 2.38, SD = 1.09, N = 61) were ranked as the second most important indicators. Of those respondents who perform in-office SISI for recurrence of stenosis after ED (65), 42 (64.6%) repeat the same postoperative protocol, and 15 (23.1%) inject only once and reassess patient need.
SISI Protocols
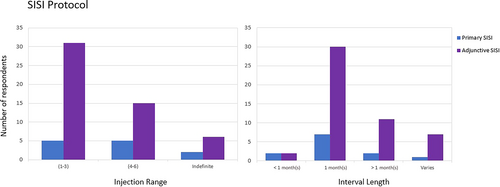
Participants described their protocol when using SISI as a primary (25) and as a planned postoperative intervention (66) for the treatment of iSGS. Triamcinolone 40 mg/mL was the most used steroid for both interventions. The percutaneous cricothyroid (transcervical) approach was preferred by 22 participants, whereas 11 preferred using flexible working channel injection. Seven participants indicated using more than one injection approach. Most used 1–3 injections during a series treatment, with a typical interval of 1 month between injections (Fig. 6). Eighteen participants indicated the interval between surgical treatment and the first injection to be on the same day (6), 1 month (7), and more than 1 month (5).
Cricotracheal Resection
Half of the participants performed CTR for iSGS (42, 48.3%) (Fig. 1). CTR were performed “after failed endoscopic management” (36, 85.7%), “for complex stenosis” (25, 59.5%) and “patient preference” (16, 38.1%). Treatment failure criteria for participants who used CTR “after failed endoscopic management” (36) included “multiple failed treatments or requiring more interventions within a short time span (<1 year)” (22, 61.1%), persistent symptoms and recurrence (9, 25%), no response to planned postoperative SISI (6, 27.3%), and patient perspective and treatment intolerance (4, 18.2%). All the participants (87) were asked about contraindicative factors against performing CTR. Common factors included multiple medical comorbidities (66, 73.6%), scar restricting mobility of the cricoarytenoid joints (57, 65.5%), scar less than 5 mm (0.5 cm) from the phonating margin of the TVF (44, 50.6%), and obesity (45, 51.7%).
Maddern Procedure
Eight (9.2%) participants reported performing the Maddern procedure for iSGS (Fig. 1). Of these participants, the Maddern procedure is offered when there is “patient preference” (6, 75%), “after failed endoscopic treatment” (4, 50%), and “for patients with complex stenosis” (4, 50%).
Other Surgical Procedures
Nine participants (10.3%) underwent other surgical procedures for the treatment of iSGS not including ED, CTR, or the Maddern procedure (Fig. 1). These participants mentioned using alternative surgical procedures such as endoscopic wedge resection (3), laryngotracheoplasty (2), tracheotomy (1), quadrantectomy without dilation (1), micro trapdoor flap (1), and micro debridement (1).
Algorithms of Care
The participants provided responses on factors that influence their algorithms of care for SISI (65, 74.7%) and surgical treatment (87, 100%) (Table II).
| Responses for algorithms of care regarding SISI n (%) | 65 (74.7) |
| Protocol based on fellowship training | 13 (9) |
| Protocol based on the literature | 45 (69.2) |
| Protocol based on previous experiences and patient outcomes | 61 (93.9) |
| Protocol based on conversations with colleagues | 45 (69.2) |
| Responses for algorithms of care regarding surgical treatment n (%) | 87 (100) |
| Protocol based on fellowship training | 27 (31) |
| Protocol based on the literature | 49 (56.3) |
| Protocol based on previous experiences and patient outcomes | 66 (75.9) |
| Protocol based on conversations with colleagues | 56 (64.4) |
DISCUSSION
Despite iSGS having a homogenous presentation, the treatment and management of this condition is varied.1 This study further validates the heterogenicity in the current standards of care and demonstrates variance across physicians. The survey data can be used as pilot data for future randomized control trials and improvement of studies. We provide insight into current treatment practices, decision-making, usage rates, and factors that influence physician rationale. We aim to provide the basis for multi-institutional randomized control trials to ultimately generate a consensus statement on the optimal guidelines for iSGS.
In the past decade, PFTs have demonstrated reliability and ease in assessing the need for surgical intervention or predict the recurrence of laryngotracheal stenosis. Carpenter et al. demonstrated peak expiratory flow (PEF) as a clinically efficient and reliable way to monitor the progression of iSGS and predict surgical intervention.3 Bhatt et al. showed PEF was a more reliable indicator of a patient's symptoms compared to the clinician's subjective assessment of stenotic degree via tracheoscopy or laryngoscopy.7 Despite their proven usefulness, the survey showed that less than half of laryngologists routinely use PFTs in caring for patients with iSGS. Although the survey did not specifically inquire about the reasons for not performing PFTs routinely, it is likely that factors such as limited clinic time or lack of equipment contribute to this.
Most laryngologists surveyed use SISI as a primary and/or planned postoperative treatment for iSGS, but only a small percentage reported routine use on all patients. Most participants perform postoperatively only “sometimes” depending on factors such as patient discussions, short interval of restenosis, poor treatment response, and an actively inflamed stenosis. Despite its widespread use, there is no established standard for determining when to perform SISI, leading to treatment variations.
The large usage of SISI is potentially attributed to prior studies demonstrating an increase in surgery free intervals for iSGS.11, 13, 15 In this survey, 1–2 cc triamcinolone 40 mg/mL was the most reported steroid and dosage used for injections through the percutaneous cricothyroid (transcervical) approach. Most participants perform a one-month interval between injections for both the primary and planned postoperative SISI treatments, with 1–3 injections being the typical number during a series treatment. For recurrence of stenosis following ED, the survey demonstrated that most participants use SISI to prevent further progression. Administration of steroid injections into the scar on a regular schedule with repeated injections over time, tailored to match the disease aggressiveness, has been shown to induce a change.15, 20
Although most laryngologists in our survey are routinely prescribing anti-reflux medications (PPIs), inhaled and oral steroids, and antibiotics following ED, the largest multicenter study by Hoffman et al., has shown that adjuvant medications do not appear to directly affect recurrence or PEF in iSGS.10 Despite this, they continue to be used in practice, raising the question about the persistence of this approach despite the lack of evidence supporting its effectiveness. There is some support that combining adjuvant medications when performing endoscopic wedge excisions leads to improved treatment outcomes. The current understanding of the endoscopic wedge excision protocol is unclear, and further research is necessary to fully understand the rationale and reasoning behind it.
Eight participants in our survey reported performing the Maddern procedure, a surgical technique that involves selective endoscopic removal of affected tissue and reconstruction with a split thickness skin graft.16-18 Although a recent comparison study showed that it has a low complication rate and improves breathing outcomes while preserving voice function, it also has a higher recurrence rate compared with CTRs.17 The low utilization of the Maddern procedure is likely due to a lack of published clinical trials demonstrating its long-term outcomes.
Nine participants use other surgical techniques, with endoscopic wedge resections with CO2 laser being one of the more frequently mentioned procedures. The involves three to four wedge excisions of stenotic scar, leaving narrow bridges in between each excised point followed by adjuvant medical therapy.19, 21 Gelbard et al. found that this procedure had a significantly lower recurrence rate than EDs and better voice outcomes with fewer complications compared to CTRs.8
The survey showed that treatment decisions are influenced by the number of iSGS patients seen annually and the physician's years of experience. Participants seeing fewer patients (0–10) are less likely to use SISIs as a primary treatment or perform the Maddern procedure and other surgical procedures (excluding CTR and ED) than those seeing more patients. Our survey demonstrates that conversations with colleagues, literature publications, experience, and patient outcomes currently define protocol refinement for SISI and surgical interventions. Only a small percentage of respondents follow the same protocol as their fellowship director.
This study's limitations include the use of a preexisting public database of member emails created from all US academic OHNS departments, which may not include all laryngologists. Additionally, the database does not include private practice laryngologists, general otolaryngologists, thoracic surgeons, or interventional pulmonologists who may have different treatment options for iSGS. Future studies could include a wider range of specialties to achieve a more overall understanding of treatment options. The open-ended nature of certain survey questions may have led participants to omit details about their SISI protocol, such as interval length, number of injections, and type of steroid used. Collecting these specific details would provide more representative data on SISI treatment protocols. The survey methodology used does not allow for making comparative statements, but it can be used to guide future studies that directly compare the efficacies of various diagnostic and treatment protocols.
CONCLUSION
This survey elucidated the heterogenic variation in the management of patients with iSGS. Recent years have demonstrated the rise of awake in-office steroid injections as a primary treatment option with varying indications and protocols with the majority of academic laryngologists performing SISI. Newer procedures such as the Maddern procedure and endoscopic wedge excisions with CO2 laser are less frequently offered at this time. Algorithms of care were mostly dependent on prior experience and patient outcomes, whereas only a minority reported using the same protocol as learned in their fellowship training. As further clinical and basic sciences studies continue to emerge, a more precise treatment standardization will improve iSGS clinical outcomes.




