Long-Term Stability and Safety of the Soundbridge Coupled to the Round Window
Abstract
Objective
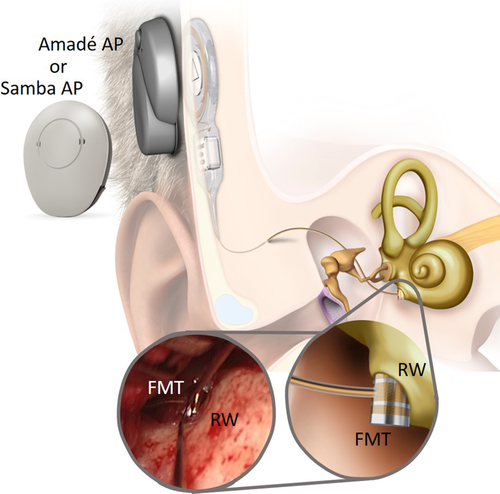
The objective of the study was to demonstrate the long-term outcomes of patients implanted with the active middle ear implant (AMEI) Vibrant Soundbridge (VSB) through coupling the floating mass transducer (FMT) to the round window (RW).
Methods
This retrospective study evaluated the short- and long-term clinical performance (audiological outcomes) and safety (revisions/explantations) of the VSB coupled to the RW between 2013 and 2019 at the St. Pölten University Hospital, Austria. For the outcome analysis, the sample was divided into a short-term examination group followed up for less than 12 months (<12 months) and a long-term examination group followed up for more than 12 months (>12 months). Cumulative survival outcomes were separately analyzed for subjects with and without cholesteatoma.
Results
46 patients with an average long-term follow-up period of 31.43 months (13–75 months) were investigated. Complications requiring revision surgery were reported in total in seven patients with cholesteatoma (15.2%) and none in subjects without cholesteatoma (0%). Residual hearing was not affected by VSB surgery. Word understanding on the Freiburger monosyllabic speech test improved significantly at 65 dB (P < .0001) and 80 dB (P < .0001), and these outcomes were stable for long-term follow up.
Conclusion
The VSB coupled to the RW is a safe implantation method for patients with conductive or mixed hearing loss. Hearing improvement was stable for the long-term follow-up up to 74 months. The revision rates are directly related to the underlying pathology of cholesteatoma (with radical cavity); thus, this special cohort requires additional counseling on potential complications.
Level of Evidence
4 (Case-series) Laryngoscope, 131:E1434–E1442, 2021
INTRODUCTION
Nowadays, a great variety of hearing aids can provide satisfactory hearing rehabilitation. While acoustic hearing aids are regularly used for sound enhancement, a few limitations are known1; especially in cases with mixed hearing loss, the necessary output to overcome the conductive component and the amplification of sound reaching the inner ear is not given.2 Therefore, alternative devices have been developed over the last two decades. Among the most commonly used devices (i.e. bone conduction (BC) devices, cochlear implants, and auditory brainstem implants), the active middle ear implant (AMEI), namely the Vibrant Soundbridge (VSB, MED-EL, Austria), was the device of interest in the research presented herein. Increasing technological progress and surgical expertise in otological implantation have resulted in the fast growth and expansion of this field. Especially AMEIs have evolved to a well-established rehabilitation method to treat not just sensorineural, but also recently conductive hearing loss (CHL) or mixed hearing loss (MHL) by using different coupling options.3 The first VSB implantation was performed by Ugo Fisch in 1996, where the floating mass transducer (FMT) was coupled to the incus, creating mechanical waves that directly stimulated the inner ear. Since then, several attachment/coupling options allowing for various complicated middle ear conditions have been identified to implant the AMEI in various different locations. Exemplary structures are the short and long process of the incus, the stapes head, the stapes footplate,4 and the round window (RW).5 In 2006, Colletti et al. introduced a new coupling modality by attaching the FMT of the AMEI onto the RW membrane instead of the incus. With this new attachment, a new era in the treatment of CHL and MHL started, using the advantages of the transcutaneous transmission and preservation of an intact skin as well as direct coupling to the cochlea through the RW membrane, providing more gain and better sound transmission in the higher frequencies. Since then, RW coupling has been proved effective on patients with CHL or MHL, which presumes a vibration of the RW membrane.5 This produces opposite phase vibrations of the stapes footplate in the oval window (OW), an effect, which has been called reverse sound stimulation, leading to bulk fluid flow between the two windows, resulting in a wave traveling down the basilar membrane.5
The coupling, alignment and connection force of the FMT on the RW seems crucial for the effective transfer of mechanical stimulus to the cochlea. Evidence on safety and long-term stability of RW coupling is still scarce. The senior author of the manuscript (GMS) performed over 320 VSB surgeries in the past ten years and 175 during the time frame under investigation (2013–2019). The majority of FMT placements were onto the incus (57%), OW placement occurred in 13% of the cases, and the remaining 29% were performed with RW attachment.
Therefore, this retrospective chart review aimed to investigate the long-term stability and efficacy of RW coupling in patients with mild to severe CHL or MHL implanted with an AMEI.
MATERIALS AND METHODS
All patients, who received an AMEI between 2013 and 2019, with the FMT attached to the RW were included. Coupling modality was chosen based on the patient's middle ear anatomy and type of hearing loss as recommended by the manufacturer's indication criteria (MED-EL, Innsbruck, Austria). Age limit for study inclusion was 18 years or older. Exclusion criteria were loss to postoperative follow-up due to unwillingness/non-response/death. All implantations were conducted by one experienced surgeon (GMS). The study was approved by the Lower Austrian Ethics Committee (GS1-EK-4/594-2019).
Clinical routine involves audiological tests, performed in a sound-isolated room with audiometers operated by certified speech therapists. Pure tone audiograms with BC thresholds at 250, 500, 1000, 2000, and 4000 Hz and air conduction (AC) thresholds measured at 250, 500, 1000, 2000, 4000, 6000, and 8000 Hz were performed. BC tests are repeated directly after surgery. Subsequent follow-up tests included a short-term follow-up, which was defined as the first 12 months after implantation and a long-term follow-up was characterized as all visits past the 12 months mark and every following year.
Freiburger monosyllabic speech tests are performed at 65 and 80 dB to analyze the percentage of word understanding (pre- and post-operatively in the short- and long-term follow-up).
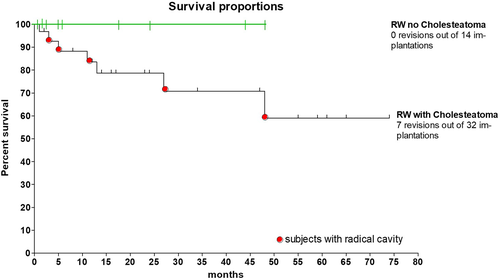
Complication and revision rates were compared in the long- and short-term time frames to evaluate patient safety and benefit of the device and presented as Kaplan–Meier Survival Curves.
Data Analysis
The statistical analysis was conducted using GraphPad Prism version 5.00 for Windows, (GraphPad Software, San Diego, CA, U.S.A., www.graphpad.com). Non-parametric Wilcoxon signed-rank test was used to test for significant differences between two test conditions in the audiological measurements. Descriptive statistics were performed for age, gender, average follow-up period, etc. and are summarized in Table 1. Subjects with a complication are presented on the individual level, whereas the remaining cohort is summarized as mean for long-term versus short-term group. In-depth surgical details are given in Table 2.
| Short-Term | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #ears | ID | Daily Wearing Time (hr) | Sex | Side | Age at Surgery | Cholesteatoma | HA Usage Prior | Length of Surgery | Revision | Reason for Revision | Time till Revision (d) | F/ U in Months |
| 1–26 | #1 - #26 individual outcomes summarized (mean and standard deviation SD. min. max) | |||||||||||
| 27 | #027 | 15 | F | L | 28 | 1 | 0 | 01:04 | 1 | cable extrusion | 176 | 1 |
| 28 | #028 | 13 | M | R | 9 | 1 | 0 | 01:14 | 1 | cable extrusion | 355 | 5 |
| 29 | #029 | 12 | M | L | 35 | 1 | 0 | 01:13 | 1 | repositioning unknown cause | 92 | |
| 30 | #030 | 16 | M | L | 23 | 1 | 0 | N/A | 1 | cable extrusion | 1463 | 2 |
| 31 | #031 | N/A | F | L | 82 | 1 | 1 | 01:05 | 1 | Surditas - > CI | 49 | |
Total ears n = 31 |
Mean | 13.08 | 13 F | 16 L | 51.61 | 22 | 7 | 1:25 | 5 | 3 Cable extrusions | 427.00 | 1.84 |
| SD | 4.13 | 18 M | 15 R | 17.63 | 00:15 | 1 Surditas | 590.89 | 2.06 | ||||
| min | 1 | 9 | 01:04 | 1 unknown cause | 49 | 1 | ||||||
| max | 18 | 82 | 02:05 | 1463 | 9 | |||||||
| Long-Term | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| #Ears | ID | Daily Wearing Time (hr) | Sex | Side | Age at Surgery | Cholesteatoma | HA Usage Prior | Length of Surgery | Revision | Reason for Revision | Time till Revision (d) | F/ U in Months |
| 1–13 | #32 - #43 individual outcomes summarized (mean and standard deviation SD. min. max) | |||||||||||
| 14 | #44 | N/A | M | L | 51 | 1 | 0 | N/A | 1 | Cable extrusion | 840 | 42 |
| 15 | #45 | N/A | F | L | 38 | 1 | 0 | 01:08 | 1 | Cable extrusion | 402 | 22 |
Total Ears n = 15 |
Mean | 13.19 | 9 F | 8 L | 50.21 | 10 | 4 | 1:21 | 2 | 2 Cable extrusions | 621.00 | 31.86 |
| SD | 4.27 | 6 M | 7 R | 16.32 | 00:21 | 309.71 | 15.78 | |||||
| Min | 5 | 22 | 00:43 | 402 | 12 | |||||||
| Max | 16.5 | 80 | 01:56 | 840 | 59 | |||||||
| Short-Term | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| # Ears | ID | # Pre-operated Ears < 3 | # Pre-operated Ears ≥ 3 | # T | # T + M | # C + T | # C + T + M | # C + RC | # Canal wall Up M | # Canal Wall Down M |
| 1–26 | #1 – #26 individual outcomes summarized | 15 | 9 | 8 | 2 | 8 | 4 | 5 | 24 | 5 |
| 27 | #027 | 1 | — | — | — | — | 1 | — | 3 | |
| 28 | #028 | 1 | — | — | — | 1 | — | — | ||
| 29 | #029 | 1 | — | — | — | — | —- | 1 | — | |
| 30 | #030 | 1 | — | — | — | 1 | — | — | — | |
| 31 | #031 | — | 1 | — | — | — | — | 1 | — | |
Total ears n = 31 |
SUM | 18 | 11 | 8 | 2 | 9 | 5 | 8 | 24 | 8 |
| Long-Term | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| # ears | ID | # Pre-operated Ears < 3 | # Pre-operated Ears ≥ 3 | # T | # T + M | # C + T | # C + T + M | # C + RC | # Canal wall Up M | # Canal wall Down M |
| 1–13 | #32 – #43 individual outcomes summarized | 8 | 3 | 3 | — | 2 | — | 8 | 5 | 8 |
| 14 | #44 | — | 1 | — | — | — | — | 1 | — | 2 |
| 15 | #45 | — | 1 | — | — | — | — | 1 | — | |
Total ears n = 15 |
SUM | 8 | 5 | 3 | — | 2 | — | 10 | 5 | 10 |
- CH = cholesteatoma; M = mastoidectomy; RC = radical cavity; T = tympanoplasty.
Long-term stability and audiological differences in dependence of time were investigated by comparing groups of pre- and post-operatively short-term (< 12 months) versus long-term (≥12 months) after implantation. Long-term performance was tested comparing the Freiburger monosyllabic speech test at 65 and 80 dB. Outcomes were rated as statistically significant with a significance level of P ≤ .05. For the safety outcomes, a Kaplan–Meier Survival analysis was performed calculating for each time interval a ‘survival’ probability calculated as the number of subjects surviving divided by the number of patients at risk.
RESULTS
Patients
Pre-operative and follow-up data of the VSB, with the FMT coupled to the RW without a coupler, were fully available for 45 subjects (46 ears) (Fig. 1). Short-term follow-up data were accessible for 31 subjects (31 ears) and long-term follow-up data were available for 14 subjects (15 ears). The mean age for the short-term group was 51.61 ± 17.63 years (range: 9–82), and the group comprised of 18 men and 13 women. The mean follow-up of the short-term group was 1.84 ± 2.06 months (range: 1–9). The long-term group exhibits 15 ears in 14 subjects with a mean age of 50.21 ± 16.32 years (range: 22–80) and a mean follow-up of 31.86 ± 15.78 months (range: 12–59).
Out of the 45 subjects, 41 subjects underwent several, at least one, on average 4 previous tympanoplasty surgeries (surgical details are summarized in Table 2); 32 of them due to chronic cholesteatoma out of which 18 (five underwent revision surgery) had a radical cavity. Surgical approach of canal wall up Mastoidectomy was performed in 29 cases (24 short-term and 5 long-term), and canal wall down Mastoidectomy was performed in 18 cases (8 short-term and 10 long-term) (Table 2). 25 patients had one or more medical comorbidities, including hypertension, diabetes, lung disease, or cardiovascular disease. 11 subjects were wearing hearing aids prior to surgery. Out of the 46 investigated ears, 34 reported their daily usage with a mean of 13.13 hours per day, which did not differ between the short-term and long-term groups (13.08 ± 4.13 vs 13.19 ± 4.27). The high daily usage is an indicator for the satisfaction and wearing comfort of the users.
Surgical Results
The mean surgery time was similar in both groups: 1:25 hours ± 0:15 in the short-term group and 1:21 hours ± 0:21 in the long-term group. No complications occurred during surgery, one patient had temporary facial nerve palsy immediately after surgery, one patient had vertigo, both incidents were resolved before leaving the hospital (on day 3).
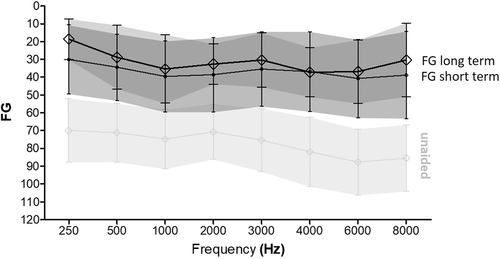
Audiological Outcomes
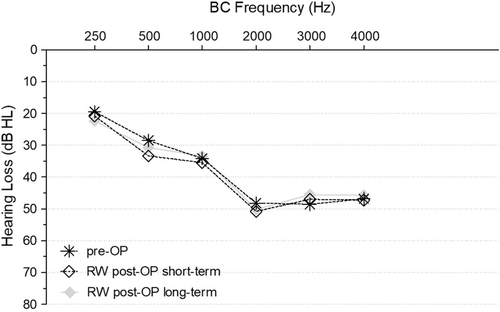
The mean difference of the surgery's impact on residual hearing was tested comparing the pre- and postoperative short- and long-term (BC) thresholds (Fig. 2). The difference between the groups compared to the unaided/pre-op condition was less than 5 dB over all frequencies, which is characterized as clinically insignificant (short-term P = .8182 and long-term P = .8438) (Table 3). This indicates that the residual hearing is not affected by VSB surgery, neither directly after surgery nor in the long-term follow-up.
| Pre-op | Short-Term | Long-Term | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measured | Mean | SD | Measured | Mean | SD | Measured | Mean | SD | |||||
| @ 65 dB | 8.97 | ± | 19.47 | WRS Benefit | @ 65 dB | 51.84 | ± | 26.64 | WRS Benefit | @ 65 dB | 51.25 | ± | 30.43 |
| @ 80 dB | 33.17 | ± | 32.687 | @ 80 dB | 49.88 | ± | 31.88 | @ 80 dB | 45.67 | ± | 33.18 | ||
| Frequency | Mean | SD | Functional gain | Frequency | Mean | SD | Functional gain | Frequency | Mean | SD | |||
| 250 | 68.15 | ± | 16.36 | 250 | 30 | ± | 19.05 | 250 | 18.64 | ± | 10.89 | ||
| 500 | 69.07 | ± | 14.55 | 500 | 34.41 | ± | 18.34 | 500 | 28.85 | ± | 17.23 | ||
| 1000 | 72.22 | ± | 14.50 | 1000 | 39.56 | ± | 19.79 | 1000 | 35.38 | ± | 18.34 | ||
| 2000 | 66.67 | ± | 16.76 | 2000 | 38.53 | ± | 20.56 | 2000 | 32.69 | ± | 11.03 | ||
| 3000 | 69.44 | ± | 18.78 | 3000 | 35.44 | ± | 20.63 | 3000 | 30.38 | ± | 14.61 | ||
| 4000 | 75.37 | ± | 14.80 | 4000 | 36.91 | ± | 22 | 4000 | 37.31 | ± | 13.25 | ||
| 6000 | 80.37 | ± | 20.33 | 6000 | 40.74 | ± | 21.73 | 6000 | 36.92 | ± | 17.05 | ||
| 8000 | 80.74 | ± | 18.43 | 8000 | 38.83 | ± | 24.07 | 8000 | 30.42 | ± | 19.84 | ||
| Frequency | Mean | SD | BC thresholds | Frequency | Mean | SD | BC thresholds | Frequency | Mean | SD | |||
| 250 | 20.00 | ± | 11.77 | 250 | 22.50 | ± | 12.97 | 250 | 22.69 | ± | 12.35 | ||
| 500 | 30.36 | ± | 16.11 | 500 | 33.57 | ± | 14.06 | 500 | 31.92 | ± | 17.62 | ||
| 1000 | 36.07 | ± | 15.71 | 1000 | 35.36 | ± | 15.25 | 1000 | 35.00 | ± | 17.20 | ||
| 2000 | 47.50 | ± | 12.67 | 2000 | 50.36 | ± | 14.74 | 2000 | 51.54 | ± | 16.25 | ||
| 3000 | 45.71 | ± | 15.42 | 3000 | 43.93 | ± | 16.55 | 3000 | 43.08 | ± | 18.09 | ||
| 4000 | 44.29 | ± | 13.71 | 4000 | 41.43 | ± | 16.81 | 4000 | 42.69 | ± | 15.76 | ||
The postoperative functional hearing gain was stable for the RW coupling group when comparing short- and long-term outcomes (Fig. 3). This demonstrates long-term stability of audiological outcomes. Mean differences were clinically insignificant for all frequencies (P = .1235).
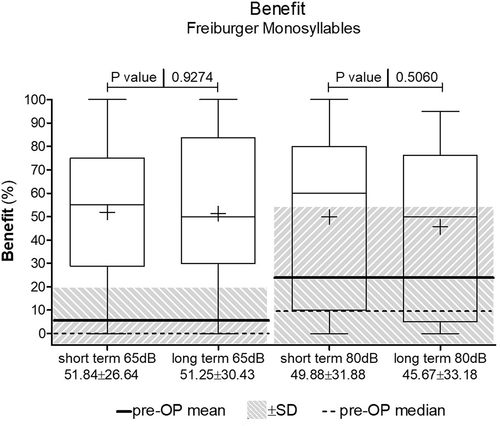
The Freiburger monosyllabic speech test was performed on all patients prior to implantation and post-operatively in the short-term and long-term follow-up with a presentation level of 65 and 80 dB. The improvement from the unaided to the aided condition was in both groups at both presentation levels highly significant (P < .0001). The mean improvement at 65 dB was 51.84 ± 26.64% in the short-term group and 51.25 ± 30.43% in the long-term group, which was not significantly different (P = .9274). The improvement at a presentation level of 80 dB SPL was 49.88 ± 31.88% in the short-term group and 45.67 ± 33.18% in the long-term group, which was not significantly different (P = .506). The mean outcomes for both groups can be seen in Table 3.
Safety
The insignificant differences in functional gain and word recognition scores proves the stability of the RW coupling. The difference of less than 5 dB in BC thresholds compared between the pre-op, post-op, and short-term and long-term groups underlines the safety of the procedure in not affecting the residual hearing through vibroplasty (Fig. 4). Nonetheless, five complications occurred within the first year in the short-term group and two in the long-term group (after 840 and 402 days, respectively). Reasons for revision surgery were extrusion of the cable into the outer ear canal (n = 5) due to reoccurring cholesteatoma and one subject presented with poor cochlear reserve due to progressive hearing loss (Fig. 5). Latter were explanted and received a cochlear implant. One subject required 3 months post-op repositioning of the FMT; the cause could not be identified. The total revision rate was 15.2% (7 out of 46). Explantation without reimplantation did not occur in any of the analyzed cases. The ‘survival’ probability calculated via Kaplan–Meier Survival analysis is shown in Figure 5. For the analysis, the outcomes were split between the groups with and without cholesteatoma. The outcomes clearly show the correlation between underlying pathology, that is, between cholesteatoma and radical cavity, and revision rate on the subject's survival rate (%). Over a course of 74 months, the survival proportion of the cholesteatoma group was 59.06% whereas the survival proportion of the group with no underlying pathology was 100% (max. F/U time was 48 months).
DISCUSSION
The VSB has been proven to be a safe alternative to hearing aids in a short-term setting in several previously published articles. Long-term studies have been published examining the stability,6 patient satisfaction,7 technical follow-up, and complications8 of the device. Few studies have shown long-term follow-up audiological results.6, 9-11 Evidence for long-term audiological outcomes is still scarce and needs further research.
This study provides the results of an investigation on audiological long-term outcomes of patients who received a VSB with the FMT coupled to the RW in a single-center study. The main aim was to demonstrate the long-term audiological benefit and stability of this surgical approach indicated for subjects with mild to severe MHL or CHL.
Revision rates and reasoning were provided, and different patient collectives were examined. Ernst et al. reported in his systematic review outcomes of the VSB as treatment for MHL or CHL; 19 publications, including 294 individuals were identified and compared to BH devices and middle ear surgery plus hearing aids.12 Thirteen studies comprising 196 patients reported on adverse events after surgery. Out of these, 32 subjects (16.3%) were identified to have postoperative complications,12 which is slightly higher than our patient cohort experienced over a period of up to 74 months. The most reported complication was FMT cable extrusion into the outer ear canal, with an occurrence rate of 6.6%. In total, 20 patients had revision surgery (10.2%). The here calculated revision rate was 15.2% as a result of the underlying pathology of reoccurring cholesteatoma and radical cavities. Colletti et al. reported two necessary explantations because of misdiagnosed severe hearing loss. Brkic et al. reported an explantation rate of 10.2%.10 The revision rate of VSB implantation with RW coupling was 29% in the 17 patients reviewed by Schraven et al.6 Our retrospectively analyzed results yielded a slightly lower revision rate of 15.8%. Emphasis needs to be placed on the fact that most of the patient cohort presented with several tympanoplasties performed elsewhere beforehand. Except for four subjects, who had unreported pre-operative interventions, the average number of reconstructive middle ear surgery was four and went up to seven in two cases.
Device failure was reported by one patient, following a mechanical impact. Similar outcomes were reported by Zwartenkot et al.8 (7% technical failure rate) and Brkic. et al. (4.0%).10 None of our patients were revised due to postoperative infections, other studies showed infection rates of 2.5% and 8.3%, respectively. Furthermore, none of our patients required second surgery due to pain complications.
The most common short-term complication in 13 different studies analyzed was FMT extrusion, with a mean occurrence rate of 6.6%.12 The cable extrusion to the outer ear canal has been addressed in a consensus statement by Beltrame, Sprinzl et al.,13 with the recommendation of drilling a deep groove for the conductor link to avoid postoperative cable extrusion.
All studies reported significant improvement in hearing thresholds. Our results are comparable with the published results of other studies, which measured a summarized average functional gain of 29.6 dB after 3 months, which did not change significantly in time.12 Ernst et al also reported speech recognition improvement between 52% and 81% after at least 6 months of use with the Freiburger monosyllabic words,12 which is similar to what our patients exhibited.
As mentioned earlier, long-term clinical outcomes of RW coupling of the VSB are still scarce. The first long-term assessment after implantation was published by Schmuziger et al.9 in 2006, although the coupling method was not stated in this article. Here, the subjective outcome of patient satisfaction was measured using the standardized International Outcome Inventory for Hearing Aids, the Glasgow Benefit Inventory, and the Visual Analog Scales for 20 patients. In addition, 15 patients underwent audiological testing at the follow-up appointment, including pure tone audiogram and speech audiometry in silence and in noise. The follow-up examination was undertaken after a mean of 42 months. Although the subjective feedback was satisfactory to very satisfactory in over half of the patients, there was no significant benefit when compared to hearing aids. High satisfaction may also be concluded in the here investigated patient cohort when summarizing the long daily wearing time of the processor (mean > 13 hours).
The first long-term follow-up article regarding the specific RW application of the VSB was published in 2013 by Liliana Coletti et al.11 Here, a collective of 50 patients with extensive ossicular chain defects was followed up.
Solely patients with extensive ossicular chain defects, chronic otitis media procedures with unsuccessful surgery, radical cavities or congenital aural atresia, and no benefit and/or no acceptance of conventional hearing aids or bone-anchored hearing aids were included in this study by Colletti et al.11 The long-term safety and efficacy at 24-month follow-up were analyzed using the outcome measures BC and AC thresholds, air-bone gap threshold, Freiburger speech test at 65 dB HL, and intraoperative and postoperative complications and FMT displacement, or extrusion rate. 60-month follow-up was available for 33 patients. Four patients were reported with complications due to VSB failure and misdiagnosed severe hearing loss. 50% of all patients previously had multiple ear surgeries without success comparable to the here presented patient cohort. Like our results, the differences between the mean BC thresholds tested pre- and post-operatively were not statistically significant different. Brkic et al.10 reported on long-term results of 118 VSB devices implanted in 103 patients at a mean follow-up period of 7.9 years (range 0.7 months - 17.9 years). In total, medical or technical complications occurred in 19 patients (16.1%). The main reasons were infection (n = 4), wire extrusion into the outer ear canal (n = 4), progressive hearing loss (n = 13), or device failure (n = 4). Most complications occurred for the RW coupling group, over half (52.3%) of all complications were reported out of this group10 indicating the importance of preoperative counseling and exact surgical clarification and planning of possibilities away from the pathology.
Our results clearly show that there was no evidence on harm to both components of hearing, neither in the short-term nor in the long-term follow-ups: tested BC thresholds to ensure that residual hearing had not been affected due to the surgical intervention were not affected neither in the short-term nor in the long-term post-operative setting. Conclusion.
Since the first introduction of the VSB in 1993, extensive research has been undertaken, but long-term data, especially on the coupling to the RW, is still scarce. The hearing improvement in the investigated cohort proved to be stable in long-term follow-up of up to 74 months. Residual hearing was not affected, neither in the short-term, nor in the long-term follow-ups. The audiological benefit is satisfactory and stable also in the long-term follow-up for the Freiburger monosyllabic speech test and the pure tone audiogram at the frequencies 0.5,1,2,4 kHz (PTA4). The users reported a long daily wearing time of >13 hours per day, indicating the high patient satisfaction. The overall complication rate was reasonable given the fact that most of the patients underwent several unsuccessful middle ear reconstructions. The most common complication requiring a revision was the extrusion of the cable to the outer ear canal and was solely found in cholesteatoma subjects. This issue was addressed in a consensus statement by a group of experts, including the senior surgeon who implanted the entire cohort reviewed in this study.
In conclusion, based on the beneficial audiological outcomes, the evaluation of complications and the patient-reported high satisfaction and wearing time, the VSB coupled to the RW proved to be a safe and stable implantation method for hearing improvement for patients within the device's indication range. The revision rates were directly related to the underlying pathology of cholesteatoma (with radical cavity) and previous middle ear operations; thus, this special cohort requires additional counseling and prior surgical planning and caution on potential complications.