Transoral Robotic Surgery Excision of Lingual Thyroglossal Duct Cysts Including the Central Hyoid Bone
Editor's Note: This Manuscript was accepted for publication on August 25, 2020
The authors have no funding, financial relationships, or conflicts of interest to disclose.
Abstract
View Video S1 Laryngoscope, 131:E1345–E1348, 2021
INTRODUCTION
Thyroglossal duct cysts (TGDCs) confined to the base of tongue present a unique surgical challenge due to their location. Here we present two patients who underwent transoral excision of a lingual thyroglossal duct cyst and the central portion of the hyoid bone via a novel transoral robotic surgery (TORS) approach, the first published description of such an approach. This was possible due to TORS, which provides a high level of dexterity, superior visualization, and increased precision and maneuverability in this difficult-to-access location while avoiding a scar in the neck.
The use of transoral robotic surgery in pediatric head and neck surgery is still in its infancy, but indications continue to expand as surgeons successfully and safely employ this minimally invasive technology for novel pathologies. Currently, the majority of TORS procedures in pediatric patients fall into two categories—laryngeal cleft repairs and lingual tonsillectomies. However, TORS can be considered for other pediatric airway, base of tongue, and parapharyngeal pathologies that are difficult to access via traditional approaches.
A thyroglossal duct cyst is a congenital mass that can present anywhere along the embryonic migration path of the thyroid, including the base of tongue (lingual type).1 Lingual TGDCs are rare and comprise only 0.6% to 3% of thyroglossal duct remnants and may be improperly classified as a vallecular cyst.1 The traditional Sistrunk procedure involves transcervical en bloc resection of the cyst, central hyoid bone, epithelial tract, and suprahyoid muscle to limit recurrence. A modification of the classic Sistrunk procedure, which utilized the concept of the posthyoid space (PHS), allows for safe and complete resection of the middle third of the hyoid bone.2
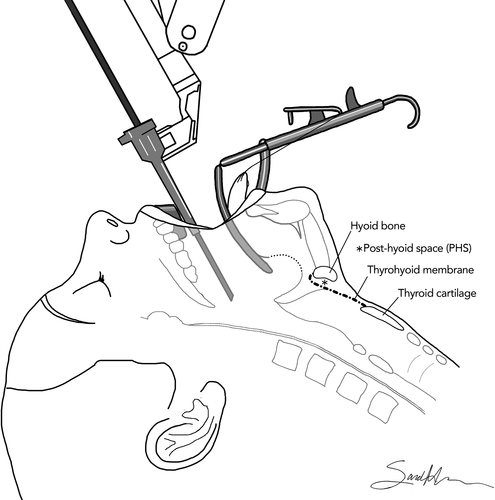
Lingual TGDCs present a unique challenge due to their location and usually require a combined approach—both transoral and transcervical—for complete excision. However, in these two cases, we combined the increased maneuverability and visualization provided by TORS with the anatomical concept of the PHS (Fig. 1) to allow for safe and complete transoral excision of a lingual TGDC and central hyoid while avoiding an external scar. Bounded anteriorly and laterally by the hyoid bone, posteriorly by the thyrohyoid membrane, and superiorly by the vallecula,2 the PHS can theoretically also give transoral access to anterior cervical masses.
METHODS
This study was exempt from institutional review board approval according to our institutional policy.
Patient 1
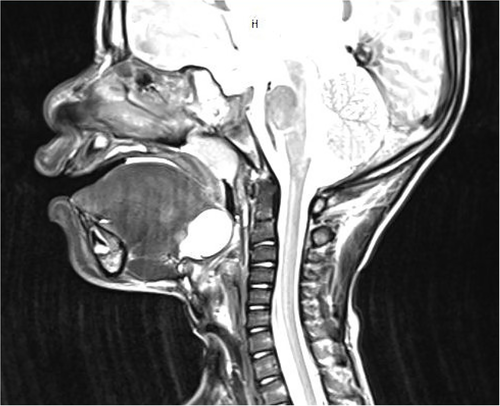
A 3-year-old medically complex male with a history of prematurity (26 weeks), intraventricular hemorrhage, repaired atrial and ventricular septal defects, bronchopulmonary dysplasia, laryngomalacia, subglottic stenosis, gastrostomy tube dependency, and tracheostomy dependency was noted to have a cystic base of tongue mass on routine bronchoscopy. Magnetic resonance imaging (MRI) demonstrated a 2.3 × 1.6 × 1.9-cm lobulated cystic lesion in the tongue base abutting the posterior hyoid bone (Fig. 2), most consistent with a lingual TGDC.
Because the mass caused significant epiglottic retroflexion and obstruction precluding eventual decannulation, we recommended excision. Given the need for laryngotracheal reconstruction in the future, we prioritized minimizing scarring in the neck and avoided a combined approach. TORS excision of the cystic lesion with removal of the central portion of the hyoid bone was recommended.
Patient 2
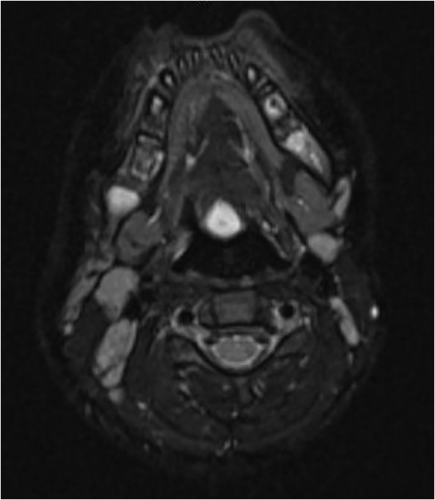
A 3-year-old girl presented with 1 year of progressive solid food dysphagia with frequent coughing and gagging on solids leading to solid food aversion. She was taking only liquids and refusing any food that required chewing. Flexible laryngoscopy revealed a cystic mass in the vallecula. MRI demonstrated a 9-mm nonenhancing cystic lesion at the midline tongue base near the foramen cecum, most consistent with a lingual TGDC (Fig. 3).
Operative Steps
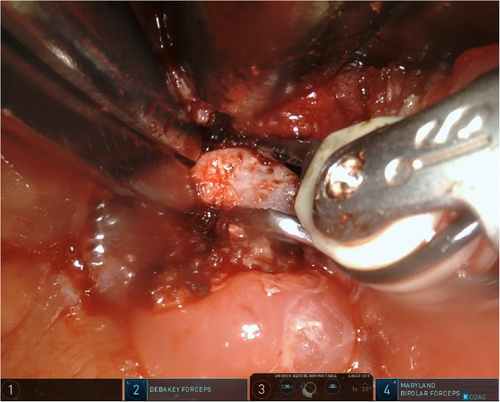
General anesthesia was induced, and ventilation was carried out via the existing tracheostomy (patient 1) or a nasotracheal tube (patient 2). They received perioperative antibiotics and steroids. A Crowe-Davis or Dingman mouth gag provided exposure, and the patient was placed in suspension. The da Vinci Xi robot (Intuitive Surgical, Sunnyvale, CA) was docked and loaded with a 30° telescope, monopolar Bovie electrocautery, and a Maryland bipolar dissector. The lesion (Fig. 4) was freed circumferentially with blunt dissection and electrocautery until complete removal was achieved.
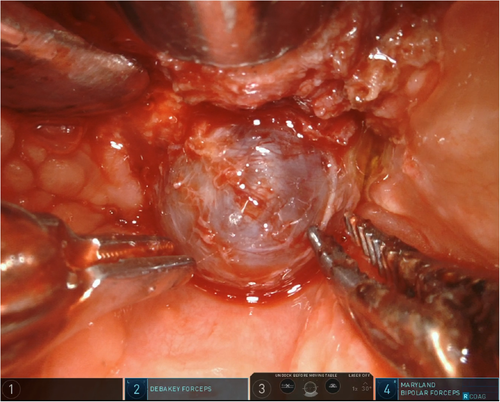
Next, external pressure was applied to the hyoid to displace it into the transoral field. The Maryland bipolar was used to dissect on to the posterior surface of the hyoid bone (Fig. 5). The infra- and suprahyoid muscles were divided. Extreme care was taken to stay midline to avoid the lingual arteries. One centimeter of the central hyoid was isolated by cutting the bone on either side with long, adult, laparoscopic Mayo scissors (Fig. 6). Remaining soft tissue attachments were divided, and the bone was removed. An epiglottopexy was then performed by suturing the lingual epiglottis to the tongue base musculature with 3-0 polydioxanone suture. The purpose of this was to prevent airway obstruction from epiglottic retroflexion and to help close any connection between the oropharynx and the neck (Video S1).

Postoperative Course
Patient 1
Pain was controlled with acetaminophen and ibuprofen. Home gastrostomy tube feeds were resumed. No bleeding or respiratory issues transpired, and he was discharged home on postoperative day 1. Histopathology was consistent with a thyroglossal duct cyst. Two weeks after surgery, flexible laryngoscopy demonstrated a well-healed base of tongue and upright epiglottis.
Patient 2
The patient was extubated in the operating room and she had no immediate or delayed respiratory concerns. Pain was managed with acetaminophen, ibuprofen, and narcotics for breakthrough pain. She initially refused oral intake, but slowly improved to a soft diet. No penetration or aspiration occurred on video fluoroscopic swallow study. Pathology demonstrated a cystic mass. She was discharged on postoperative day 6. Within 2 weeks, she regained the ability to eat solid food.
DISCUSSION
TGDCs are the most common congenital anomaly of the neck. Although rare, lingual TGDCs are more often symptomatic and can cause dysphagia, airway obstruction, and obstructive sleep apnea.1 Additionally, they may be overlooked during clinical exam because they do not present as obvious neck masses. Even if laryngoscopy is performed, lingual TGDCs can be misdiagnosed as glossoptosis, laryngomalacia, or supraglottitis in the case of an infected cyst. Although the Sistrunk procedure is the mainstay of management, novel approaches to both cervical and lingual TGDCs have been described.
Although some have proposed that marsupialization or simple cystectomy of lingual TGDCs is sufficient for long-term control,3, 4 others have demonstrated recurrence rates as high as 100% with these approaches.5 Recurrence rates seem to be higher when lingual TGDCs are closely related to the hyoid bone, and in these cases, some advocate for transoral excision followed by a traditional transcervical Sistrunk procedure.1 For example, Zhang et al. described seven patients diagnosed with lingual thyroglossal duct cysts with a close relationship to the hyoid that underwent cystectomy or marsupialization between one and eight times with cyst recurrence soon after every operation.5 All patients had a pathological diagnosis of a thyroglossal duct cyst and subsequently underwent a modified transcervical Sistrunk procedure with no subsequent recurrence after 2 years. This study demonstrates the importance of removing cysts in their entirety, including the hyoid bone, if the cyst is closely related to it.
The TORS tactic takes advantage of the midline approach to the posthyoid space, which is relatively devoid of blood vessels and lymphatics, to allow for safe and complete transoral resection of the middle third of the hyoid bone. Bounded anteriorly and laterally by the hyoid bone, posteriorly by the thyrohyoid membrane, and superiorly by the vallecula,2 the PHS can theoretically also give transoral access to anterior cervical masses. Overall, cyst location, imaging, and proximity to the hyoid should guide decision making regarding removal of the central hyoid.
An endoscopic cystectomy technique with laser ablation of the surgical cavity was also recently described for lingual thyroglossal duct cysts.6 Six infants were successfully managed with this technique, which utilizes carbon dioxide laser and microlaryngeal instruments, although recurrence rates were not reported. Our technique differs significantly given the application of robotic surgery and the removal of the central portion of the hyoid bone through the base of tongue, which has never been described. Our approach is not feasible in infants given the size of current robotic instrumentation, and we agree with standard endoscopic cystectomy as a first step in this population.
In the two cases described here, we achieved a scarless and minimally invasive alternative to traditional lingual TGDC approaches that also minimizes the chance of recurrence. This was facilitated by the unique features of TORS, which combines four-handed manipulation (including console and assistant surgeon), three-dimensional visualization, and improved dexterity and precision.
CONCLUSION
We present the first published description of a purely transoral approach for excision of a lingual TGDC and central portion of the hyoid bone, which adds to the scarce literature on performing such surgery robotically and performing TORS on children in general. Although we believe this approach is effective and minimally invasive, further studies are needed to confirm safety and to determine whether outcomes are comparable to traditional approaches.
ACKNOWLEDGMENTS
The authors thank Vidal Maurrasse for his voiceover work.




