Computed tomography-based preoperative muscle measurements as prognostic factors for anastomotic leakage following oncological sigmoid and rectal resections
Abstract
Background
Oncological sigmoid and rectal resections are accompanied with substantial risk of anastomotic leakage. Preoperative risk assessment and patient selection remain difficult, highlighting the importance of finding easy-to-use parameters. This study evaluates the prognostic value of contrast-enhanced (CE) computed tomography (CT)-based muscle measurements for predicting anastomotic leakage.
Methods
Patients that underwent oncological sigmoid and rectal resections in the LUMC between 2016 and 2020 were included. Preoperative CE-CT scans, were analyzed using Vitrea software to measure total abdominal muscle area (TAMA) and total psoas area (TPA). Muscle areas were standardized using patient's height into: psoas muscle index (PMI) and skeletal muscle index (SMI) (cm2/m2).
Results
In total 46 patients were included, of which 13 (8.9%) suffered from anastomotic leakage. Patients with anastomotic leakage had a significantly lower PMI (22.1 vs. 25.1, p < 0.01) and SMI (41.8 vs. 46.6, p < 0.01). After adjusting for confounders (age and comorbidity), lower PMI (odds ratio [OR]: 0.85, 95% confidence interval [CI] 0.71–0.99, p = 0.03) and SMI (OR: 0.93, 95%CI 0.86–0.99, p = 0.02) were both associated with anastomotic leakage.
Conclusion
This study showed that lower PMI and SMI were associated with anastomotic leakage. These results indicate that preoperative CT-based muscle measurements can be used as prognostic factor for risk stratification for anastomotic leakage.
Abbreviations
-
- ASA
-
- American Society of Anesthesiology
-
- AUC
-
- area under the curve
-
- BMI
-
- body mass index
-
- CE
-
- contrast enhanced
-
- CRT
-
- chemoradiotherapy
-
- CT
-
- computed tomography
-
- LAR
-
- low-anterior resection
-
- OR
-
- odds ratio
-
- PMI
-
- Psoas Muscle Index
-
- ROC
-
- receiver operating characteristics
-
- ROI
-
- region of interest
-
- SMI
-
- Skeletal Muscle Index
-
- TAMA
-
- total abdominal muscle area
-
- TPA
-
- Total Psoas Area
1 INTRODUCTION
Rectosigmoid resections are associated with a high risk of postoperative complications causing morbidity and mortality.1, 2 Major complications occur in 15%–18% of the patients, with anastomotic leakage being the most frequent with an incidence of up to 10%.3-5 However, risk stratification is challenging, given that multiple studies have shown that a wide variety of factors correlate with risk of postoperative complications.6 This highlights the importance of accurate prediction models, that use robust clinical parameters to assess frailty and the associated surgical risk for these patients.6, 7 This is particularly important given that, with the increasing age of patients undergoing this type of surgery, the number of frail older adult patients increases.8 Preoperative selection of frail patients and subsequent targeted interventions, such as physical prehabilitation programs, have been shown to be potentially beneficial, leading to a reduction of postoperative complication rates.9-11
Recently, some studies are reporting that skeletal muscle and psoas muscle volumes can be used as a proxy for patient frailty.7 Low skeletal muscle volume or psoas muscle volume is defined as sarcopenia, which can be relatively easily assessed using computed tomography (CT). Studies have shown that CT-based measurements of abdominal muscles, including the psoas muscle, have the potential in predicting adverse outcome in surgical patients.12, 13
This study explores the potential prognostic value and clinical use of CT-based preoperative muscle measurements, such as skeletal muscle index (SMI) and psoas muscle index (PMI), in an attempt to predict anastomotic leakage after oncological rectosigmoid resections.
2 METHODS
2.1 Study population and treatment
All patients who underwent sigmoid or rectal resection for primary colorectal cancer in the Leiden University Medical Center (LUMC) between January 2016 and December 2020 were retrospectively included in this study. Exclusion criteria were: (temporary) construction of stoma during primary surgery, emergency surgery, palliative intended surgery, distant metastasis at time of diagnosis of the primary tumor, and endoscopic resection. Patient characteristics (e.g., age and comorbidity) and clinical data (e.g., type of surgery and complications) were collected from the electronic medical record and the LUMC cancer registry. This study was approved by the Medical Ethics Committee of the LUMC (ID number G21.093).
2.2 CT-based measurements
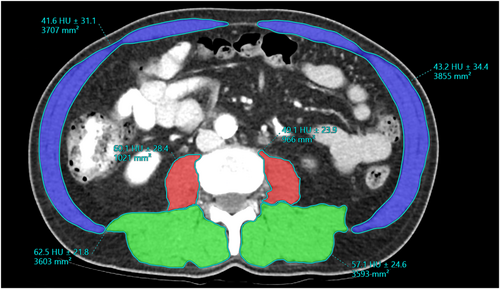
All included patients had a preoperative contrast-enhanced (CE) abdominal CT in portal venous phase of no more than 3 months before surgery. Analysis of CT-scans was performed using Vitrea (version 7.14.2.227, Canon Medical). Muscle areas were determined by manually segmenting a region of interest (ROI) in the skeletal- and psoas muscles on the portovenous phase of the CE-CT images. The CT slice at the level of the inferior part of L3 was chosen for analysis, which is conform the criteria of previous studies.7, 13 Subsequently, the skeletal muscles and psoas muscle areas determined from the segmented ROIs (mm2).7, 13, 14 Total abdominal muscle area (TAMA) was categorized into specific abdominal muscle groups; psoas muscles, back muscles (erector spinae and quadratus lumborum muscles), lateral muscle (external- and internal oblique and transversus abdominis) and rectus abdominis (Figure 1). Additionally, total psoas area (TPA) was calculated by the sum of both psoas muscles. Two researchers (RTK and CJR) independently performed the image segmentation after ensuring an interobserver variability correlation of at least 0.8 in a training set, under supervision of a radiologist (ANC). Disagreements regarding measurements were resolved by discussion, with ANC acting as a third observer when necessary. The muscle areas were adjusted by patient's height (m) to standardize the measurement between patients. The height-normalized muscle areas (muscle indices) of the psoas and skeletal muscles (TAMA), PMI and SMI were used for further analysis. The units for muscle areas were cm2 and muscle indexes, cm2/m2.
2.3 Anastomotic leakage
All complications that occurred during 90 days after surgery were registered and reviewed. Anastomotic leakage was defined as a defect of the intestinal wall or abscess at the site of the colorectal anastomosis, diagnosed or confirmed by contrast enema, furthermore, an abscess around the anastomosis, for which endoscopic, percutaneous or operative re-intervention was required.
2.4 Statistical analysis
Odds ratios (OR) with 95% confidence intervals and p-values were reported for each variable to assess the impact of all patient- and treatment characteristics, multivariable analysis was conducted using clinically-relevant variables. Mann–Whitney U and chi-squared test were used to assess patient- and treatment characteristics. A p-value of <0.05 was considered statistically significant. The Spearman's ρ correlation coefficient was used to assess interobserver variability in CT muscle surface area scoring. To show clinical use of CE CT-based muscle parameters, nomograms were constructed based on a regression model using the rms package in R. The predictive strength of the prediction models used to construct the nomograms was measured by the Area Under the Receiver Operating Characteristics (ROC) Curve (AUC). All analyses were done using R version 4.1.2 in RStudio. ROC curves and AUC scores were calculated using the pROC package, plots were made using the ggplot2 package.
3 RESULTS
3.1 Patient characteristics
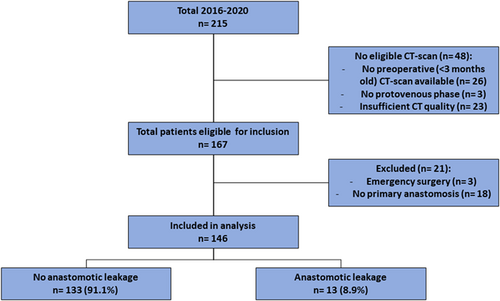
A total of 215 patients underwent a sigmoid or rectal resection between 2016 and 2020 of which 48 were excluded because a CT scan was not present (Figure 2). Additionally, patients with emergency surgery (n = 3) and patients with stoma construction during primary surgery (n = 18) were excluded. Of the in total 146 included patients, 13 (8.9%) suffered from anastomotic leakage. There was a significant difference between the group of patients that suffered from anastomotic leakage and the group that did not with respect to age and the use of minimally invasive techniques (Table 1). There were no significant differences observed in comorbidities.
| No anastomotic leakage | Anastomotic leakage | p-value | |
|---|---|---|---|
| n = 133 (91.1%) | n = 13 (8.9%) | ||
| Age (median) | 59 (50–71) | 68 (37–86) | <0.01 |
| Gender (male) | 80 (60.2%) | 5 (38.5%) | 0.22 |
| ASA score | 0.95 | ||
| 1–2 | 26 (19.5%) | 3 (23.1%) | |
| 3–4 | 12 (9.0%) | 10 (76.9%) | |
| Comorbidity | 74 (55.6%) | 10 (76.9%) | 0.24 |
| BMI (median) | 25.0 (19.5–41.3) | 25.9 (17.5–34.7) | 0.93 |
| pT-stage | 0.69 | ||
| 0 | 1 (0.8%) | 0 (0.0%) | |
| 1–2 | 58 (43.6%) | 6 (46.2%) | |
| 3–4 | 74 (55.6%) | 7 (53.8%) | |
| pN-stage | 0.74 | ||
| 0 | 81 (60.9%) | 9 (69.2%) | |
| ≥1 | 52 (39.1%) | 4 (30.8%) | |
| Neo-adjuvant chemoradiotherapy (CRT) | 23 (17.3%) | 4 (30.8%) | 0.41 |
| Type of surgery | 0.25 | ||
| Low-anterior resection (LAR) | 64 (48.1%) | 9 (69.2%) | |
| Sigmoid resection | 69 (51.9%) | 4 (30.8%) | |
| Minimally invasive | <0.01 | ||
| Open | 4 (3.0%) | 2 (15.4%) | |
| Laparoscopic | 129 (97.0%) | 11 (84.6%) |
3.2 CT-based measurements
Results showed that the manual segmentation (Figure 1) of the muscles on CT images were highly reproducible, with the Spearman's ρ correlation coefficient >0.87. (Table 2).
| Coefficient | p-value | |
|---|---|---|
| Total Abdominal Muscle Area (TAMA) | 0.99 | <0.01 |
| Total Psoas Area (TPA) | 0.95 | 0.01 |
| Psoas left | 0.89 | 0.04 |
| Psoas right | 0.87 | 0.05 |
| Psoas Muscle Index (PMI) | 0.91 | 0.03 |
| Skeletal Muscle Index (SMI) | 0.99 | <0.01 |
3.2.1 Muscle measurements
Patients that suffered anastomotic leakage had significantly lower preoperative TPA (median: 77.5 cm2 vs. 59.6 cm2, p = 0.02) and lower TAMA (median: 144.2 cm2 vs. 111.8 cm2, p = 0.01) (Table 3). Additionally, comparing the PMI and SMI between both groups, both parameters were significantly lower in the anastomotic leakage groups (p < 0.01).
| No anastomotic leakage | Anastomotic leakage | p-value | |
|---|---|---|---|
| n = 133 (91.1%) | n = 13 (8.9%) | ||
| Total Psoas Area (TPA) (cm2) (median) | 77.5 (37.7–196.3) | 59.6 (39.7–101.4) | 0.01 |
| Total Abdominal Muscle Area (TAMA) (cm2) (median) | 144.2 (70.1–377.1) | 111.8 (73.8–191.1) | 0.02 |
| Psoas Muscle Index (PMI) (cm2/m2) (mean) | 25.05 (14.7–64.1) | 22.1 (14.2–28.7) | <0.01 |
| Skeletal Muscle Index (SMI) (cm2/m2) (mean) | 46.6 (27.0–123.1) | 41.8 (26.5–54.1) | <0.01 |
3.2.2 Uni- and multivariable analysis
A higher age (OR: 1.07, 95% CI 1.01–1.13, p = 0.02) and lower PMI (OR: 0.87, 95% CI 0.77–0.99, p = 0.03) and SMI (OR: 0.94, 95% CI 0.88–0.99, p = 0.04) were in univariable analysis significantly associated with anastomotic leakage (Table 4). After adjusting for confounders (age and comorbidity), a lower PMI (OR: 0.85, 95% CI 0.71–0.99, p = 0.03) and SMI (OR: 0.93, 95% CI 0.86–0.99, p = 0.02) were both significantly associated with the occurrence of anastomotic leakage.
| OR | p-value | Adjusted OR* | p-value | |
|---|---|---|---|---|
| Age | 1.07 (1.01–1.13) | 0.02 | – | |
| Sex (male) | 0.41 (0.13–1.33) | 0.14 | ||
| ASA score** | – | |||
| 1 | Ref | – | Ref | |
| 2 | 0.82 (0.21–3.25) | 0.78 | 0.99 (0.21–4.56) | 0.99 |
| 3 | 0.72 (0.07–7.68) | 0.79 | 0.81 (0.06–10.34) | 0.87 |
| Comorbidity | 2.58 (0.68–9.79) | 0.16 | – | |
| Type of surgery | ||||
| Low Anterior Resection (LAR) | Ref | – | Ref | |
| Sigmoid resection | 0.63 (0.18–2.15) | 0.46 | 0.45 (0.12–1.62) | 0.21 |
| T-stage | ||||
| 1 | Ref | – | – | |
| 2 | 0.56 (0.1–3.6) | 0.57 | 0.33 (0.05–2.41) | 0.28 |
| 3 | 0.47 (0.08–2.68) | 0.42 | 0.28 (0.04–1.99) | 0.21 |
| 4 | 1.62 (0.19–13.93) | 0.66 | 0.78 (0.08–8.18) | 0.84 |
| Neoadjuvant therapy | 2.13 (0.60–7.50) | 0.24 | 1.43 (0.37–5.51) | 0.61 |
| BMI | 0.99 (0.86–1.14) | 0.90 | 0.97 (0.84–1.11) | 0.66 |
| Psoas Muscle Index (PMI) | 0.87 (0.77–0.99) | 0.03 | 0.85 (0.71–0.99) | 0.03 |
| Skeletal Muscle Index (SMI) | 0.94 (0.88–0.99) | 0.04 | 0.93 (0.86–0.99) | 0.02 |
- * Adjusted for age, comorbidity,
- ** ASA, American Society of Anesthesiologists.
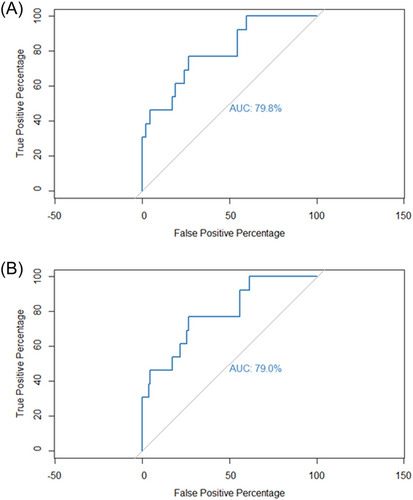
3.3 Nomograms
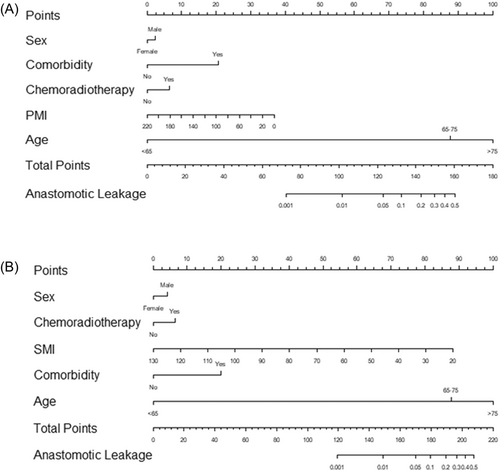
For preoperative prediction of anastomotic leakage regression model-based prediction models, using clinically- and statistically relevant parameters (age, gender, comorbidity, chemoradiotherapy, and SMI or PMI), were made. The prediction model using PMI had an AUC of 79.8% (Figure 3A) and using SMI as muscle parameter had an AUC of 79.0% (Figure 3B), respectively. Additionally, clinically usable nomograms were constructed using these prediction models with using PMI (Figure 4A) as muscle parameter and one using SMI (Figure 4B).
4 DISCUSSION
This study investigated the value of CT-based cross-sectional measurements of abdominal and psoas muscles as a prognostic factor for anastomotic leakage after curative intended oncological sigmoid or rectal resection. Cross-sectional measured abdominal and psoas muscle area were significantly lower in patients that suffered from anastomotic leakage. Furthermore, both PMI and SMI are both prognostic factors for anastomotic leakage following sigmoid and rectal resection.
Recent studies have shown an association between lower muscle volumes and short-term surgical outcomes after colorectal surgery.7, 12, 13 Literature reports that cross-sectional lumbar muscle areas are well correlated with muscle mass in the whole body.15, 16 However, analysis of CT images using a single-muscle approach such as the psoas major muscle, might be less laborious and therefore more realistic in a clinical setting, validation is, however, still lacking.17 As shown by Jones et al.,7 TPA and TAMA on the L3 level correlates well with clinical outcomes.7 However, these reports also showed that TAMA was more reproducibly measured by CT analysis than TPA. This is also observed in our study as the interobserver variability is higher in the TPA.
The association between low muscle mass and anastomotic leakage might be partly explained by frailty, since previous studies have shown an association between frailty and anastomotic leakage following colorectal surgery as well.7, 18, 19 However, there is no consensus on markers for determining patient frailty at this time, and identification of frail patients is still difficult.20, 21
Skeletal muscle depletion is defined as a decrease in muscle mass, and it occurs when protein degradation exceeds protein synthesis. Potential causes of muscle atrophy are ageing, malnutrition, long-term immobilization, as well as various serious and often chronic diseases, such as chronic heart failure, chronic obstructive lung disease, renal failure, AIDS, sepsis, anorexia nervosa, and muscular dystrophies among others. Furthermore, skeletal muscle depletion may be the result from cancer too, as part of the cancer-cachexia syndrome.22-24 Cancer cachexia is a wasting syndrome characterized by weight loss, anorexia, asthenia, and anemia. The pathogenicity of this syndrome is multifactorial, due to a complex interaction of tumor and host factors leading to muscle protein breakdown, thus to cachexia-related sarcopenia.23, 25 Several studies have shown a clear correlation between lower muscle mass and an increased inflammatory state due to tumor cachexia and frailty.26, 27 This might explain the association between sarcopenia and anastomotic leakage as well since a more katabolic and inflammatory state may hamper healing capacity in tissues such as bowel tissue resulting in anastomotic leakage.28, 29
Additionally, aging in patients might explain this association, since CT-based muscle measurement may be more accurate than just age since it is more representative for biological age compared with calendar age. Ageing leads to trunk muscle attenuation, but such age-related differences vary widely between muscle groups.30 Thicknesses of rectus abdominis, internal oblique, and external oblique muscles were 36%–48% smaller for older than younger adults.31 Additionally, trunk muscle deficits with increasing age may have important implications for physical function, disability, pain, and risk of injury in older adults.32
Accurate prediction of postoperative complications and especially anastomotic leakage could improve preoperative patient selection, treatment decision and shared-decision making. An important dilemma in patients undergoing sigmoid or rectal resection is whether or not to construct an anastomosis and/or (temporary) stoma.33 An important consideration is the risk of anastomotic leakage since a (temporary) diverting stoma can reduce the rate of clinical symptomatic anastomotic leakage.6, 34 Furthermore, measuring a low muscle mass on the preoperative CE-CT could be an indication for prehabilitation programs, since low muscle mass may be reversible.9, 11, 35 Especially, in rectal cancer patients undergoing neo-adjuvant chemo(radio)therapy, there is a greater window of preoperative optimization by physical exercise, which has been shown to be safe and feasible.36 Prehabilitation programs have been shown to objectively improve physical fitness.37 Additionally, since patients with lower skeletal muscle mass may experience more chemotherapy toxicity, this might be used in shared decision-making and treatment planning as well.38, 39
4.1 Limitations
Although this study provides insights in the used of CT-based muscle measurements, this study has some limitations. Since, patients included in this study were selected to be fit for surgery by expert opinion, this may lead to allocation bias. Additionally, some patients were excluded because of unavailability of CT examinations or insufficient quality. However, the occurrence allocation bias is unavoidable in this type of retrospective study. Due to the relatively low sample size an validation of the prediction models was not possible. Furthermore, this was a single-center study in an academic teaching hospital where comorbidity/competing risks were possibly not fully known by applied comorbidity classification, this affect generalizability.
5 CONCLUSION
In this exploratory analysis, low SMI and PMI were predictive for anastomotic leakage and show potential in treatment planning, shared decision making and engaging in prehabilitation programs. Since abdominal CT scans are routinely being performed for preoperative staging and treatment planning, they can easily be used to quantify muscle volumes without additional examinations or costs.
ACKNOWLEDGMENTS
This research was supported by the Leiden University Medical Center (LUMC).
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
SYNOPSIS
Oncological sigmoid and rectal resections are accompanied with substantial risk of anastomotic leakage, preoperative risk assessment remains difficult. This study shows that using enhanced (CE) computed tomography (CT) – based muscle measurements can predict anastomotic leakage following oncological sigmoid and rectal resections.