Music therapy and weight gain in preterm infants: Secondary analysis of the randomized controlled LongSTEP trial
Sofia Bauer-Rusek and Shachar Shalit contributed equally to this study.
Abstract
Objectives
This study assessed the association between MT and weight gain among preterm infants hospitalized in Neonatal Intensive Care Units.
Methods
Data collected during the international, randomized, Longitudinal Study of Music Therapy's Effectiveness for Premature Infants and their Caregivers (LongSTEP) study were compared between the MT group and the standard care (SC) group. Weights were recorded at birth, enrollment, and discharge. Weight percentiles, Z-scores, weight gain velocity, and extrauterine growth restriction (EUGR) were calculated.
Results
Among 201 preterm infants included, no significant differences in weight parameters (weight, weight percentiles, weight Z-scores; all p ≥ 0.23) were found between the MT group (n = 104) and the SC (n = 97) group at birth, enrollment, or discharge. No statistical differences in EUGR represented by change in Z-scores from birth to discharge were recorded between MT and SC (0.8 vs. 0.7). Among perinatal parameters, younger gestational age (p = 0.005) and male sex (p = 0.012) were associated with increased risk of EUGR at discharge. Antenatal steroid treatment, systemic infection, bronchopulmonary dysplasia, neurological morbidities, retinopathy of prematurity, necrotizing enterocolitis, parental factors (amount of skin-to-skin care, bonding, anxiety, and depression questionnaire scores), and type of enteral nutrition did not significantly influence weight gain parameters (all p > 0.05).
Conclusions
In the LongSTEP study, MT for preterm infants and families was not associated with better weight parameters compared to the SC group. The degree of prematurity remains the main risk factor for unfavorable weight parameters.
Highlights
What is Known
-
Music therapy (MT) may enhance the growth of preterm infants through its favorable effect on physiological stability.
-
MT may promote the maturation of sucking behavior and enhance parent–infant bonding.
What is New
-
MT for preterm infants and families was not associated with better weight gain in the secondary analysis of the LongSTEP (Longitudinal Study of Music Therapy's Effectiveness for Premature Infants and their Caregivers) randomized controlled trial.
-
Degree of prematurity remains the main risk factor for unfavorable weight gain parameters.
1 INTRODUCTION
Appropriate growth is an important aspect of health and development during pregnancy, infancy, and childhood1, 2 and is associated with better clinical and neurodevelopmental outcomes for preterm infants.3, 4 The growth of preterm infants is influenced by many elements, including genetic factors, prenatal conditions, degree of prematurity, morbidities, nutrition, and developmental supportive care.5-8 Monitoring the growth of this sensitive population is complex and requires specific tools and expertise.9-13 Developmentally supportive care (DC) interventions were developed to reduce stress and discomfort and therefore may reduce energy expenditure and allow caloric intake to be used for growth.14, 15 Enhancing parent–infant bonding may increase breastfeeding duration and rate, reduce infants' stress, and stabilize vital signs that may lead to better growth.14, 15
Music therapy (MT), one of the DC modalities, is intended to support infant development and parent–infant relationships by empowering parents in their parental roles and in understanding their infant's behavior.16, 17 MT may enhance the growth of preterm infants through its favorable effect on physiological stability, including heart rate and breathing,18 may promote maturation of sucking behavior,19-21 and enhance parent–infant bonding.18-22
Previous studies evaluating the effect of MT on weight gain among preterm infants produced inconsistent results.7, 18 Lack of study power and retrospective design,22 uncontrolled studies,23 short assessment periods,19-21 different types of MT interventions,19, 21, 24 and evaluation of different growth parameters7 have contributed to the challenges in evaluating the effect of MT on weight gain among preterm infants.
The present study assessed the effect of MT on weight gain of preterm infants during hospitalization in the neonatal intensive care unit (NICU) by analyzing data accumulated during the Longitudinal Study of Music Therapy's Effectiveness for Premature Infants and their Caregivers (LongSTEP) study, a large, multinational, randomized clinical trial.17
2 METHODS
2.1 Participants and settings
From August 2018 to April 2020, 213 families of preterm infants (<35 weeks gestation at birth) from seven level III NICUs and one level IV NICU in five countries (Argentina, Colombia, Israel, Norway, and Poland) were enrolled in the LongSTEP study. The primary objective of this prospective, randomized study was to evaluate the effects of MT during NICU hospitalization, and for 6 months after discharge home, on mother–infant bonding, parental anxiety, and maternal depression compared to standard care (SC). Preterm infants who were born at less than 35 weeks' gestation were likely to be hospitalized a minimum of 2 weeks after enrollment and had been declared by NICU staff as medically stable to start MT, and were eligible for the study, if they had parents who: (1) provided written, site-specific informed consent, (2) were willing to engage in at least 2 of 3 MT sessions per week, (3) had sufficient understanding of the respective national language(s) to answer questionnaires and participate in MT, and (4) possessed sufficient mental capacity to complete the intervention and questionnaires.
MT consisted of parent-led, infant-directed singing. Our use of the concept denoted a reciprocal process wherein infants through their communicative behavior actively directed parents' use of voice, while parents then direct their singing to the infant's responses in the moment. MT sessions were conducted at bedside or in the family's room during skin-to-skin time, feeding, or with the infant lying in the incubator or cot. Sessions were approximately 30 min duration. The time spent actively making music depended on infant tolerance.
For very preterm infants, MT contained cautious use of parental singing and toned voice (e.g., single notes, simple melodies, or short musical phrases adapted from children's songs or parent-preferred music) matched to infant state and engagement cues, such that the infant “directed” the parent's use of voice.
From week 32 and onwards, MT was expanded by adding increased musical complexity and interplay. Accompanying instruments were used sparingly to underline the importance of parental voice. The detailed study design and results concerning the preplanned outcomes in the NICU period are reported elsewhere.17 DC modalities were part of the routine policy of the participating NICUs. Weight gain patterns were not preplanned or reported as an outcome in the original study and are the primary focus of the current study.
The main goal of the present study was to evaluate the effect of MT on weight gain of preterm infants during their hospitalization in the NICU. Secondary goals were to evaluate the association between weight gain and variables, such as gestational age, antenatal steroid treatment, neonatal morbidities (systemic infection, bronchopulmonary dysplasia [BPD], retinopathy of prematurity [ROP], necrotizing enterocolitis [NEC], intraventricular hemorrhage [IVH], and periventricular leukomalacia [PVL]), parental factors (duration of skin-to-skin care, bonding, anxiety, and depression questionnaire scores), and the amount of breast milk feeding.
Nutritional guidelines were not detailed for the sites participating in the LongSTEP study but all sites had a similar approach. Mothers were encouraged to provide their infants with breast milk; otherwise, preterm infant formula was provided orally or by tube feeding. Feedings were advanced according to local protocols, but all sites added human milk fortifier to breast milk when the infant reached 90–120 cc/kg. Feeding was stopped or delayed when clinical signs of abdominal tenderness or NEC was suspected or confirmed. Feeding was stopped for 3 h after blood transfusion or treatment with nonsteroidal anti-inflammatory drugs for patent ductus arteriosus. BPD was diagnosed as the need for intermittent positive pressure ventilation in the first week of life for more than 3 days and supplemental oxygen for more than 28 days. Mild BPD was defined as breathing room air; moderate BPD as requiring oxygen supplementation (FiO2 < 0.3); and severe BPD as requiring FiO2 ≥ 0.3 or positive pressure ventilation at 36 weeks gestation according to the criteria of Jobe and Bancalari.25 Systemic infection was considered if positive blood cultures coincided with clinical signs suggesting infection. NEC was determined by clinical and radiologic criteria of Bell et al.26 Only definite NEC (Bell stages II–III) was included. ROP was graded according to the international classification of the Committee for the Classification of Retinopathy of Prematurity and was recorded as the most severe stage in either eye.27 IVH was diagnosed by cranial ultrasound and graded according to Papile et al.28 PVL was diagnosed by ultrasound, with grading from 1 to 4 in accordance with Rennie.29
2.2 Outcome measures
Infants' weight (in g) was recorded at birth, study enrollment, and discharge (three points). Weight percentiles for each measurement were calculated and were converted into Z-scores according to the Fenton fetal–infant growth chart30 (using http://www.peditools.org).31 Z-scores define a person's anthropometric measurements (e.g., weight, head circumference, or length) compared with a growth chart in terms of the number of standard deviations below or above the growth chart median (50th percentile).4, 13
Extrauterine growth restriction (EUGR) was defined as “none” when the weight Z-score decreased up to 0.8 standard deviations (SD) from birth to discharge; “moderate” when the weight Z-score decreased 0.8–2 SD; and “severe” if the decline was greater than 2 SD from birth to discharge.12
Growth velocity was calculated as weight at discharge minus birth weight divided by hospitalization days (g/day) from birth to discharge.
2.3 Statistical analysis
Characteristics of the data were evaluated using descriptive statistics. The effects of treatment (MT) on weight gain were evaluated by testing group differences in weight at discharge using a linear mixed-effects model (analysis of covariance) adjusted for sex, time in NICU, and site, due to stratified randomization (weight [discharge]− weight [enrollment] + group + sex + time + 1/site). As the amount of missing data was <10%, the data were analyzed as a complete set. The same model, but without duration or sex, was used to analyze the outcomes of Fenton Z-scores and Fenton percentiles. For the secondary analysis of the Fenton EUGR scale, we examined the effects of other variables, including sites, using a generalized logistic model with two categories (normal and nonnormal growth, corresponding to 0 and 1, 2, or 3). No statistically significant differences were found between the participants included in this study (N = 201) and those who were excluded from the current study (N = 12). The data were therefore assumed to be missing at random and imputation was not carried out. Data were analyzed using statistical software R version 4.2.2.
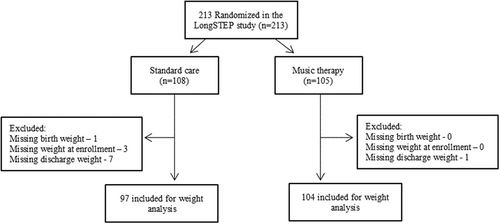
3 RESULTS
A total of 213 participants were enrolled and randomly assigned to the LongSTEP study. Participants assigned to MT received a mean (SD) of 10.0 (6.0) sessions. Eighty-seven of 105 (83%) received per-protocol MT (≥6 sessions). Mothers were present at 84 sessions (SD 6.0), fathers at 2.2 (SD 3.4), and both parents at 2.7 (SD 3.7). Mean (SD) session length was 30.8 (11.2) min. Data from 201 infants were analyzed in the current study. We excluded infants who had missing weight measurements (11 in the SC group and one in the MT group; Figure 1). The baseline characteristics of the infants in the MT and SC groups are described in Table 1. They were not statistically different.
| Characteristic | SC (n = 97) | MT (n = 104) | Total (n = 201) |
|---|---|---|---|
| Sex (female)a | 51 (53) | 49 (47) | 100 (50) |
| Singleton pregnancya | 72 (74) | 69 (66) | 141 (70) |
| GA at birth (weeks)b | 30.7 (2.7) [22.9, 34.7] | 30.3 (2.6) [25.3, 34.3] | 30 (2.6) [22.9, 34.7] |
| GA < 28 weeksa | 14 (15) | 21 (20) | 35 (17) |
| GA 28–32 weeksa | 37 (38) | 47 (45) | 84 (42) |
| GA 32–35 weeksa | 46 (47) | 36 (35) | 82 (41) |
| Antenatal steroidsa | 85 (88) | 84 (81) | 169 (84) |
| IVH grade 3–4a | 1 (1) | 2 (2) | 3 (1) |
| PVL grade 2–3a | 1 (1) | 3 (3) | 4 (2) |
| Bronchopulmonary dysplasia | |||
| Nonea | 54 (55) | 54 (52) | 108 (54) |
| Milda | 27 (28) | 27 (26) | 54 (27) |
| Moderatea | 11 (12) | 11 (11) | 22 (11) |
| Severea | 5 (5) | 12 (11) | 17 (8) |
| Systemic infectiona | 18 (19) | 28 (27) | 46 (24) |
| Necrotizing enterocolitisa | 4 (4) | 1 (1) | 5 (2) |
| ROP, grade 3–4a | 7 (7) | 9 (9) | 16 (8) |
| >50% mother's breast milka | 53 (55) | 65 (63) | 118 (59) |
| <50% mother's breast milka | 27 (28) | 24 (23) | 51 (26) |
| Donor breast milk ± infant formulaa | 3 (3) | 2 (2) | 5 (2) |
| >90% infant formulaa | 13 (14) | 13 (12) | 26 (13) |
| Skin-to-skin care | |||
| >4 days/weeka | 65 (67) | 68 (68) | 133 (67) |
| ≤4 days/weeka | 31 (33) | 35 (35) | 66 (33) |
| PBQ total scoreb | 6.7 (6.4) [0, 31] | 7.7 (9.1) [0, 62] | 7.2 (7.9) [0, 62] |
| GAD-7 mother scoreb | 6.1 (5.3) [0, 21] | 6.4 (4.8) [0, 19] | 6.3 (5.1) [0, 21] |
| EPDS scoreb | 7.8 (4.9) [0, 20] | 8.5 (5.2) [0, 24] | 8.2 (5.1) [0, 24] |
| Length of NICU stay (days)b | 44 (24) [15, 118] | 52 (30) [13, 146] | 49 (27) [13, 146] |
| Duration of study (days)b | 27 (15) [5, 71] | 31(21) [6, 96] | 29 (19) [5, 96] |
Weight parameters (weight, weight percentile, weight Z-scores) at birth, study enrollment, and discharge are presented in Table 2. No differences in weight parameters were recorded between the groups at any time point. Weight gain velocity was also similar between study groups (Table 2). No statistical difference in EUGR, represented by change in Z-scores from birth to discharge, was recorded between MT and SC (Table 2). Table 3 presents the linear mixed model for weight parameters. During the study period, weight parameters were not correlated with the study group (SC vs. MT). However, weight parameters were correlated with birth weight, male sex, and length of stay.
| Parameters | Standard care (n = 97) | Music therapy (n = 104) |
|---|---|---|
| At birth | ||
| Weight (g)a | 1412 (445) [480,2440] | 1375 (421) [620, 2335] |
| Weight percentilea | 42 (27) [0, 97] | 43 (24) [1, 95] |
| Weight Z-scorea | −0.30 (0.92) [−2.62. 1.94] | −0.22 (0.77) [−2.29, 1.66] |
| At enrollment | ||
| PMA (weeks)a | 33.0 (1.7) [27.4, 36.0] | 33.0 (2.3) [27.0, 44.0] |
| Age (days)a | 17 (15) [2, 72] | 21 (20) [2, 125] |
| Weight (g)a | 1612 (385) [705, 2730] | 1630 (453) [820, 3680] |
| Weight percentilea | 23 (19) [0, 82] | 22 (18) [0, 81] |
| Weight Z-scorea | −0.96 (−0.79) [−3.06, 0.91] | −0.94 (0.75) [−3.25, 0.86] |
| At discharge | ||
| Weight (g)a | 2416 (440) [1646, 4140] | 2485 (479) [1640, 4320] |
| Weight percentilea | 20 (21) [0, 92] | 18 (17) [0, 82] |
| Weight Z-scorea | −1.17 (0.97) [−3.46, 1.43] | −1.30 (1.03) [−5.13, 0.92] |
| Extrauterine growth restrictions | 0.7 (0.77) [0, 3] | 0.8 (0.74) [0, 3] |
| Noneb | 41 (42) | 39 (37) |
| Moderateb | 52 (54) | 61 (59) |
| Severeb | 4 (4) | 4 (4) |
| Weight gain velocity (g/day)a, c | 21 (7) [−6, 36] | 20 (8) [−12, 35] |
- Abbreviation: PMA, postmenstrual age.
- a Mean (SD) [min, max].
- b n (%).
- c Some babies were discharged before regaining their birthweight, explaining the negative growth velocity.
| Outcome at discharge | Weight (g)a | Fenton Z-scorea | Fenton percentilea |
|---|---|---|---|
| Group—Standard carea | 41.02 [−26.08, 108.11] (0.235) | 0.14 [−0.03, 0.31] (0.233) | 1.975 [−1.37, 5.32] (0.251) |
| Length of stay (days)a | 20.61 [18.29, 22.93] (0.000) | ||
| Male sexa | 74.45 [7.03, 143.86] (0.031) | ||
| Weight at enrollmenta | 0.807 [0.70, 0.91] (0.000) | ||
| Weight Z-score at enrollmenta | 0.98 [0.87, 1.09] (0.000) | ||
| Weight percentile at enrollmenta | 0.734 [0.65, 0.83] (0.000) |
- a Regression coefficient [95% confidence interval] (p value).
EUGR was significantly influenced by gestational age at birth and male sex; both were associated with an increased risk of EUGR at discharge (Table 4). Singleton birth, presence of neurological morbidities, antenatal steroid treatment, other neonatal morbidities (systemic infection, BPD, ROP, or NEC), parental factors (duration of skin-to-skin care, bonding, anxiety, and depression questionnaire scores), and type of enteral nutrition did not significantly influence the weight parameters in the study cohort.
| Male sexa | −0.95 [−1,73, −0.21] (0.013) |
| Gestational age at birtha | −0.18 [−0.34, −0.02] (0.026) |
| Singleton pregnancy, noa | −0.21 [−1.05, 0.64] (0.637) |
| Fenton Z-score at birtha | 0.38 [−0.02, 0.81] (0.065) |
| Antenatal steroid treatmenta | −0.48 [−1.53, 0.51] (0.352) |
| Systemic infection, yesa | 0.29 [−0.79, 1.39] (0.603) |
| Bronchopulmonary dysplasia, yesa | 0.77 [−0.38, 1.98] (0.193) |
| Retinopathy of prematurity, yesa | −0.38 [−1.61, 0.81] (0.527) |
| Necrotizing enterocolitis, yesa | −0.62 [−3.15, 2.61] (0.652) |
| Neurological morbidity, yesa | 0.99 [−0.02, 2.08] (0.062) |
| Skin-to-skin care ≥4 days/weeka | −0.94 [−2.26, 0.31] (0.158) |
| Edinburgh postnatal depression scale at enrollmenta | −0.02 [−0.09, 0.05] (0.614) |
| Nutrition ≥50% mother's milka | 0.06 [−0.91, 0.92] (0.883) |
- Abbreviation: CI, confidence interval.
- a Regression coefficient [95% CI] (p value).
4 DISCUSSION
In this subanalysis of data from the LongSTEP study,17 we found that MT during NICU hospitalization was not associated with better weight parameters compared to preterm infants who received SC. This finding does not support previous studies that showed that MT was associated with better weight gain.19-23
Adequate growth of preterm infants is correlated with health, well-being, and favorable neurodevelopmental outcomes. Growth is affected by many factors, including environmental, genetic, demographic, comorbidities, and standard of care.5, 32 Therefore, it is not surprising that MT alone did not significantly influence weight parameters in the cohort. Of note, is that the use of pacifier-activated music in previous studies19-21 could lead to reinforcement of sucking behavior, whereas MT targeted in between feedings as in the LongSTEP study did not do so. The mother listening to music while expressing milk may increase quantity and macronutrients, whereas music that is targeted solely at the infant might not have this effect. However, the effect of those music interventions on growth was not well-demonstrated.7
Extreme prematurity increased the risk for EUGR in our cohort. However, in contrast to other studies,8 systemic infection during the NICU stay, gastrointestinal, respiratory, and neurological comorbidities were not significantly associated with EUGR. This could be because most of our cohort had mild comorbidities that did not substantially affect weight gain.
We found that male preterm infants were at higher risk for EUGR. Our findings are in agreement with those of other studies that demonstrated more morbidities and higher mortality among male preterm infants, which may be associated with EUGR.33-35
The LongSTEP study investigators choose to diagnose BPD according to the definition of most study centers.25 We are aware that new definitions are gaining wider use but did not implement them in the current study to avoid different results than those in the LongSTEP study.16, 17
Preterm birth imposes an unnatural separation between infants and their families, which contributes to increased stress and anxiety among babies and parents.36, 37 Lack of sufficient, consistent presence of a primary caregiver (usually the parents) is correlated with failure to thrive.38 The NICUs in our cohort were located in countries where public support and welfare initiatives ensured consistent parental presence during hospitalization.16 Furthermore, all NICUs had implemented DC modalities to support infants and families.15, 39, 40
Duration of skin-to-skin care as well as parental bonding, anxiety, and depression scores did not affect weight gain patterns in our cohort. This could be explained by the strong parental presence and high compliance with skin-to-skin care interventions (almost daily among most participants) and by the support system DC NICUs offer. It is also possible that parents who consented to participate in an MT trial have special characteristics.41
Of note, despite DC interventions, the EUGR rate of babies born <1500 g (very low birth weight) in our cohort (n = 109) was approximately 40%, which is consistent with the rates reported in large cohort studies that included NICUs; many without a special emphasis on DC.8, 42 This further demonstrates the complex, multifactorial influences on growth patterns.
Growth remains the most important key to assessing nutrition adequacy of preterm infants.4 Our data included information on human milk feeding, which is an important yet partial aspect of neonatal nutritional care. Both nutritional care and growth assessment require expertise to accurately interpret the data, adjust treatment, and allow optimal conditions for sufficient growth.43
Some parameters of nutrition recommendations for preterm infants are not strongly validated.44 Growth of preterm infants during their NICU stay is divided into three periods: adaptation to extrauterine life, transition from parenteral to enteral feeding, and full enteral feeds and stable growth.45 The vast differences in postnatal age of study enrollment (Table 2) and partial data regarding nutritional intake (Table 1) made it difficult to interpret weight parameters. Furthermore, definition and classification of EUGR are not yet validated as having a prognostic yield and are highly variable depending on the growth reference used. Both the American Academy of Pediatrics46 and the European Society of Pediatric Gastroenterology, Hepatology and Nutrition44 recommend using a growth chart based on a large, robust database. Therefore, we chose the Fenton fetal–infant growth reference.30 EUGR is useful for monitoring growth both in clinical and research settings, but it should be interpreted cautiously and in conjugation with other growth measures, such as velocity.4
Site-specific differences in weight gain patterns and in aspects of care known to affect growth, such as gestational age at discharge13 and human milk feeding,47, 48 highlight the influence of local practices and populations on growth outcomes.44 Unfortunately, we could not draw any firm conclusions because the sample size per site was small. Nevertheless, local practices should be assessed regularly as part of NICU policies.
The strength of this study is the prospective nature of the cohort. In addition, the data concerning DC modalities offer a unique, holistic insight into aspects not usually addressed in literature related to growth or nutritional assessments.49, 50
The main limitation is that weight gain does not equal growth. Length and head circumference measurements are fundamental for appropriate growth assessment; however, these were not included in the LongSTEP study. Furthermore, although some general nutritional guidelines were adopted by all sites, data on nutritional intake were limited. Of note, the length and timing of interventions varied significantly (Table 1), which may influence the effect of MT on weight gain parameters. Furthermore, the study was not powered to detect a difference in weight gain between the MT and SC groups; therefore, we might not have detected the effect of MT on weight gain, which larger studies might find.
In conclusion, MT for preterm infants and families was not associated with better weight gain parameters compared to the control group. Whether MT and/or weight gain patterns will correlate with future neurodevelopment and attachment is yet to be determined by the LongSTEP study results. Degree of prematurity and male sex remains the most significant risk factors for unfavorable weight outcomes, advocating focus on the very preterm infants and offering individually adjusted care to improve outcomes.
Future studies assessing the effect of MT on development and growth should be designed with early and long durations of MT intervention and include extremely, very, and late preterm infants, detailed data on nutritional intake, and assessment of complete anthropometric data, before, during, and after the study period. The study protocol should include guidelines for nutritional support to avoid differences in nutritional support among sites.
ACKNOWLEDGMENTS
Funding for the main LongSTEP trial was provided by the Research Council of Norway (No. RCN 273534). Additional funding was provided by the Faculty of Fine Art, Music and Design at the University of Bergen and POLYFON Knowledge Cluster for Music Therapy. The current study: “Music therapy and weight gain in preterm infants” was not funded.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
The main trial received ethics approval from the Regional Committees for Medical and Health Research Ethics in Norway and was supplemented by ethics approvals in each participating country. The current study was included in the approvals granted for the LongSTEP study (ClinicalTrials.gov Identifier: NCT03564184).




