Establishing a recommended duration of blood glucose monitoring in nondiabetic patients following orthopaedic surgery
This study was approved by our institutional review board.
Abstract
Previous studies have demonstrated that blood glucose (BG) levels should be monitored for at least 1 week after orthopaedic surgery in diabetic patients, but no study has determined how long nondiabetic patients should be monitored. As postoperative elevations in BG have deleterious effects, determining a duration for monitoring the BG of nondiabetic patients after major orthopaedic surgery is needed to detect hyperglycemic events, create comprehensive protocols for nondiabetic orthopaedic patients, and reduce adverse outcomes. A retrospective study was conducted including consecutive patients who underwent a major orthopaedic surgery at a community hospital. A BG level of 150 mg/dl was the cutoff used to define hyperglycemia according to our institutional guidelines. A χ2, analysis of variance, and subgroup analysis were performed separately. Greater than 67% of nondiabetic patients experienced a high BG level (>150 mg/dl) after surgery. We found that nondiabetic patients reached their postoperative maximum BG level at 20 h, which was sooner compared to diabetic patients. We discovered more than 92% of nondiabetic patients reached a maximum BG levels within the first 72 h of hospitalization, while the BG levels after this period were found to be within normal limits in greater than 87% of cases. We propose that BG management be instituted in nondiabetics from the preoperative period to 72 h after surgery, including patients who are same-day discharges. There may not be a need to continue inpatient BG monitoring beyond the first 72 h for nondiabetic hospitalized patients with extended hospitalizations.
1 INTRODUCTION
Several factors have been reported as modifiable risk factors to mitigate adverse outcomes after orthopaedic surgeries, including elevated perioperative blood glucose (BG) levels, and orthopaedic surgeons should address these risk factors to reduce complications. While much research has focused on preoperative BG control, postoperative hyperglycemia, a physiologic response to neuroendocrine stress hormones that trigger the release of inflammatory cytokines and counterregulatory hormones, can also lead to devastating complications.1-3 Even patients without a diagnosis of diabetes mellitus (DM) can develop postoperative hyperglycemia, and these patients are at increased risk of serious postoperative complications, including surgical site infection, periprosthetic joint infections, and a longer hospital stay.4-6 Furthermore, BG variability after orthopaedic procedures has also been shown to be associated with adverse postoperative outcomes in both diabetic and nondiabetic patients due to the hyperglycemia-related impairment of the immune response.7, 8
An optimal glycemic management strategy in patients undergoing major surgical procedures continues to be debated. Several randomized controlled trials studying tight perioperative BG control (80 mg/dl < BG < 110 mg/dl) have reported inconsistent outcomes, including some that have reported adverse outcomes.9-11 Among different thresholds suggested, the Critical Care Society recommends that a BG > 150 mg/dl (8.3 mmol/L) should trigger insulin therapy,11 which is in line with the recommendation of Takesue et al.4 Among nondiabetic patients undergoing major surgical procedures specifically, Raju et al. supported the practice of targeting BG levels to less than 150 mg/dl. Several recent studies investigating the timing of BG measurement among orthopedic patients have reported substantial heterogeneity.5-7, 12, 13 Notably, in a recent work by Varady et al.,14 the night of surgery has been suggested as the most sensitive time for detecting hyperglycemia.15, 16
Previous studies have demonstrated that BG levels should be monitored for at least 1 week after orthopaedic surgery in diabetic patients,17 but no study has been conducted to determine how long nondiabetic patients should be monitored. Thus, the purpose of this study was to determine the time after major orthopaedic surgery in nondiabetic patients that BG should to be monitored to detect hyperglycemic events. This information can be used to provide a higher level of patient care by developing comprehensive protocols for nondiabetic orthopaedic patients to maintain postoperative BG at stable levels and intervene when necessary to minimize the time patients spend in a hyperglycemic state.
2 METHODS
Level of evidence: 3. This retrospective study was approved by an Institutional Review Board and conducted from May 2019 to May 2020 including consecutive patients who underwent major orthopaedic surgery, including posterior or posterolateral lumbar arthrodesis with or without a graft, primary total hip, primary total knee, and primary total shoulder arthroplasties at a community hospital within a large integrated health care system. In May 2019, a quality improvement program to standardize the testing and treatment of perioperative hyperglycemia in all patients (DM and non-DM patients) was established and all major orthopaedic surgery patients were included. A BG level of 150 mg/dl was the cutoff point used to define hyperglycemia according to our institutional guidelines. Patients with missing BG laboratory results or those who underwent a bilateral, unicompartmental, or revision surgery were excluded. There were 14 patients excluded for missing BG values; these patients had no statistical differences from our non-DM group and the missing values was due to individual practitioners not yet participating in the quality improvement program. As we queried data from our institutional database management system, we were not presented with numbers of excluded surgical procedures, thus they were not available for analysis.
Patient demographic information was collected, including age, sex, body mass index (BMI), along with diabetic status. Patients were placed into three categories based on their maximum BG level during their inpatient hospital stay: normal (BG < 150 mg/dl), borderline (150–180 mg/dl), and high (>180 mg/dl) for both DM and non-DM patients. The results reported are (1) the time from the end of surgery to the time of the first hyperglycemic event (>150 mg/dl) and (2) the time to occurrence of the maximum BG level. Given that patients with a hospital length of stay less than 3 days may not be effectively evaluated for the temporal pattern of postoperative BG fluctuations, these patients (n = 267) were excluded before analyzing the BG maximum results. BG was measured every 6 h, and all patients, regardless of their diabetic status, were started on a liquid diet and a standard insulin sliding scale (subcutaneous regular insulin injections according to their BG levels) immediately postoperatively. When tolerated, the diet was then advanced to a standardized carbohydrate diet with the same amount of carbohydrates (45 gm) in each meal. Patients were discharged after they tolerated solid foods, achieved successful pain management, and ambulated with an assistive walking device. Institutional review board approval was obtained before initiating this study.
Our primary outcomes were the time from the end of surgery to the time of the first hyperglycemic event (>150 mg/dl) and occurrence of the maximum BG level and the time after major orthopaedic surgery in nondiabetic patients that BG should be monitored to detect hyperglycemic events. Secondary outcomes included the probability of detecting a hyperglycemic event after this time period and the average maximum postoperative BG level among nondiabetic patients.
SPSS Software System ver. 22.0 (IBM) and Prism (v 9.0; GraphPad software Inc) were used for statistical data analyses. A χ2 test was used to test for differences in proportions between groups and an analysis of variance was used to test for differences in means between the groups. A subgroup analysis for the type of procedure was also performed separately. A value of p < 0.05 was considered to be statistically significant.
3 RESULTS
There were 428 patients in this cohort, with an age range from 26 to 94 years of whom 57% were female (Table 1). The average age and BMI of patients were 68 ± 10 years and 31 ± 7 kg/m2, respectively. A total of 246 patients (57%) were obese, with a BMI above 30 kg/m2, 123 patients (29%) were overweight (25 < BMI < 29.9 kg/m2), and 59 patients had a normal BMI (<25 kg/m2) (Table 1). Forty-five patients (10%) underwent a lumbar spinal fusion, 58 patients (14%) received a total shoulder arthroplasty, 174 patients (41%) underwent a total knee arthroplasty, and 151 patients (35%) received a total hip arthroplasty.
| Demographics | |
|---|---|
| Age (years), mean ± SD | 68 ± 10 |
| Female, % (n) | 57 (243) |
| BMI (kg/m2), mean ± SD | 31 ± 7 |
| Diabetes, % (n) | |
| Diabetes mellitus | 32 (135) |
| Nondiabetes mellitus | 68 (293) |
| BMI, % (n) | |
| Normal (<25 kg/m2) | 14 (59) |
| Overweight (25–29.9 kg/m2) | 29 (123) |
| Obese (30+ kg/m2) | 57 (246) |
| Procedure, % (n) | |
| Hip arthroplasty | 35 (151) |
| Knee arthroplasty | 41(174) |
| Shoulder arthroplasty | 14 (58) |
| Spinal fusion | 10 (45) |
- Abbreviation: BMI, body mass index.
Of these patients, 135 patients were diabetic (32%) and 293 patients were nondiabetic (68%). There were 95 nondiabetic patients (33%) who had BGmax levels below the normal threshold (150 mg/dl) during their entire inpatient postoperative course and 198 (67%) who experienced a BGmax level (>150 mg/dl) after surgery (Table 2). The average maximum postoperative BG level among nondiabetic patients was 175 ± 47 mg/dl, which was significantly lower than for diabetic patients in our study (214 ± 56 mg/dl; p < 0.001).
| Nondiabetics | Cases, % (n) | Diabetics | Cases, % (n) | p value |
|---|---|---|---|---|
| <150 mg/dl | 33 (95) | <150 mg/dl | 9 (12) | <0.001a |
| 150–180 mg/dlb | 30 (89) | 150–180 mg/dlb | 20 (27) | 0.007a |
| >180 mg/dla | 37 (109) | >180 mg/dla | 71 (96) | <0.001a |
| Total | 100 (293) | Total | 100 (135) |
- a High BGmax that received insulin.
- b Borderline BGmax that received insulin.
- c Statistically significant.
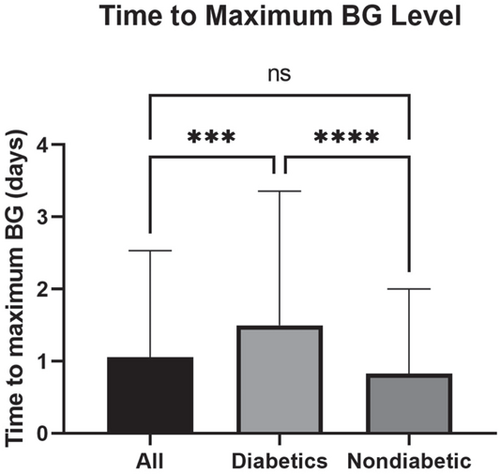
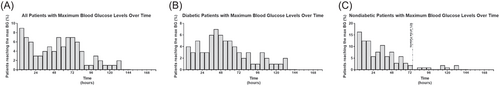
The average time between the end of surgery and the occurrence of the maximum BG level in all patients was 25 ± 35 h. This period of time was significantly shorter among nondiabetics (20 ± 28 h) compared to diabetic patients (36 ± 44 h; p < 0.001; Figure 1). The overall distribution of maximum BG levels over time is shown in Figure 2A. Despite the reported average time to maximum BG level of 36 h in all diabetic patients, we found that still 28% of diabetic patients had a peak BG level after the first postoperative 72 h, as shown in Figure 2B. We also determined that more than 92% of nondiabetic patients (148 out of 161 patients) reached their maximum BG levels within the first 72 h of hospitalization (Figure 2C).
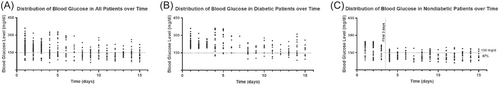
The distribution of all BG test results is depicted in Figure 3A–C. The average time to BG level that was treated (>150 mg/dl) was not significantly different between diabetic (16 h) and nondiabetic (17 h) patients (p = 0.3). Similar to the findings for the time to BGmax in nondiabetic patients, 87% of nondiabetic patients had BG < 150 mg/dl after 72 h postoperatively (Figure 3C). There were no episodes of hypoglycemia as a result of the insulin intervention for elevated BG levels.
There were no significant differences between different procedural subgroups (hip arthroplasty, knee arthroplasty, shoulder arthroplasty, and spinal fusion) in terms of maximum BG levels, time to BGmax, or time to BG level that was treated (Table 3; p > 0.1).
| Hip arthroplasty | Knee arthroplasty | Shoulder arthroplasty | Spine fusion | p value | |
|---|---|---|---|---|---|
| Age (years), mean ± SD | 71 ± 12 | 65 ± 9 | 62 ± 16 | 69 ± 9 | 0.1 |
| BMI (kg/m2), mean ± SD | 31 ± 6 | 28 ± 7 | 29 ± 6 | 33 ± 8 | 0.4 |
| BGmax (mg/dl), mean ± SD | 195 ± 53 | 189 ± 52 | 187 ± 64 | 197 ± 71 | 0.2 |
| Time to BGmax (hrs), mean ± SD | 41 ± 16 | 47 ± 18 | 48 ± 19 | 41 ± 17 | 0.2 |
| Time to 150 mg/dL BG (h), mean ± SD | 13 ± 9 | 17 ± 14 | 19 ± 7 | 12 ± 9 | 0.1 |
- Abbreviation: BMI, body mass index.
4 DISCUSSION
Hyperglycemia is a very common finding among patients undergoing orthopaedic surgeries, and also has strong associations with adverse surgical outcomes.18-20 Current findings indicate that more than 67% of nondiabetic patients experience a high BG level (>150 mg/dl) after surgery, for which they likely should be treated. We found that nondiabetic patients reached their postoperative maximum BG level at 20 h, which was sooner after surgery compared to diabetic patients. Interestingly, we found out that more than 92% of nondiabetic patients reached their maximum BG levels within the first 72 h of hospitalization, while the BG test results after this period were within the normal range in more than 87% of cases. These findings indicate that the surgically induced stress response takes place during a very narrow window of time following orthopaedic surgeries in nondiabetic patients. There may be limited clinical benefit for BG measurement beyond the first 3 days postoperatively. However, nondiabetic patients are more likely to eventually develop an infection if the postoperative BG level is elevated, even if only transiently, because of a halt in neutrophil activity.5, 7 Therefore, preoperative, intraoperative, or early postoperative BG management strategies should be considered to address transient hyperglycemia.
This study had several limitations. First, it is possible that a small number of patients who underwent one of the major orthopaedic surgeries evaluated in our study did actually have underlying diabetes mellitus that was not recognized until the postoperative period. While this possibility is rare, our institution follows a thorough preoperative screening algorithm including performing a complete blood count, basic metabolic panel and evaluating for any history of elevated fasting BG levels, which if indicative, a Hemoglobin A1C level was obtained. For patients who were assumed to be nondiabetic preoperatively (by virtue of the laboratory and history interpretation) but demonstrated hyperglycemia postoperatively, we referred the patients back to their primary care provider for evaluation of possible Diabetes Mellitus. We also had a cohort with varied demographics in terms of age, BMI, and types of surgeries. However, the demographic variability of our patients is characteristic of daily practice and can be generalized to patients undergoing major orthopaedic procedures. In addition, this study was retrospective and cross-sectional; therefore, we had a subsequent limitation to the assessment of exposure and outcomes. We were not able to evaluate the effectiveness of the systematic measurement and management of postop BG levels among nondiabetic patients in terms of complication rates. Prospective studies are warranted to evaluate if reducing postoperative glycemic variability reduces complication rates. Finally, although the 150 mg/dl threshold for BG was used as a cutoff point for our analysis and is in line with previous recommendations,4 some studies have proposed 137–140 mg/dl as the ideal level for initiating corrective insulin for mitigating the risk of adverse outcomes.5, 11, 21
While vigilance with perioperative BG monitoring seems appropriate, pressures exist to reduce the inpatient hospital length of stay following elective arthroplasty procedures, with a significant portion being moved to the ambulatory setting. To balance these pressures with that of appropriately monitoring perioperative BG levels to reduce the risk of complications, clinicians must understand the appropriate length of time postoperatively that BG levels should be monitored in orthopaedic patients. Some elements of BG surveillance may need to be shifted to home health services.
Previous studies have suggested different cutoff points as appropriate for starting insulin treatment to reduce the likelihood of adverse outcomes.5, 11, 21, 22 According to our institutional guideline, we used a cutoff of 150 mg/dl, which is in line with the recommendation of Takesue et al.4 Consistent with previous studies,23, 24 we initially observed that the maximum BG level occurs in the first 24 h postoperatively (91%) in most cases when measured every 6 h, but after excluding patients with a hospital stay of less than 3 days, the period that most patients reached their BG maximum peak levels was beyond the first 24 h and within the first 72 h. No difference in BG related variables could be detected among different procedural subgroups.
Mraovic et al.7 studied perioperative hyperglycemia in 1948 patients undergoing orthopaedic procedures and found that nondiabetic patients were three times more likely to develop an infection if the postoperative BG level was elevated. Kheir et al.5 also found that nondiabetic patients were significantly more likely to develop periprosthetic joint infections due to elevated BG levels compared with diabetic patients, and suggested that immediate and strict postoperative glycemic control may reduce postoperative complications in this group of patients, as even mild hyperglycemia was significantly associated with periprosthetic joint infection (BG > 137 mg/dl). These findings, combined with the high prevalence and specific pattern of postoperative hyperglycemia in patients without diabetes demonstrated in our study, shed light on the need for and the importance of developing guidelines for BG monitoring and management in this patient group.
Current findings are among the first to report that having a systematic measurement of BG in nondiabetics is crucial to the effective management of BG levels. While other studies in the literature are mainly focused on the first 48 h after surgery,9, 12 Maradit Kremers et al.6 found any single high BG result within one week after orthopaedic surgery to be significantly associated with adverse outcomes. Our data support a greater than 90% probability that BG Max would occur within 72 h in nondiabetic patients. Therefore, we suggest that dietary restriction and BG management continue for first 72 h after the surgery. There seems to be no need to continue this approach beyond the first 72 h in nondiabetic patients. Preoperative carbohydrate loading, defined as administrating oral carbohydrate drinks before surgery, is a preventive approach that could be considered as a potential option in these patients. It has been shown to reduce postoperative insulin resistance and hyperglycemia25 and has a positive effect on perioperative markers of surgical outcomes,26 but further studies are required to assess preoperative carbohydrate loading as an adjunct in improving postoperative outcomes in nondiabetic orthopaedic patients.
In summary, postoperative hyperglycemia is a common finding in nondiabetic patients, and we propose that BG management be instituted in this group of patients from the preoperative period to the first 72 h after surgery, even in patients who go home the same day as surgery. There may not be a need to continue inpatient BG monitoring beyond the first 72 h for nondiabetic hospitalized patients with longer hospital stays.
CONFLICT OF INTERESTS
Authors Todd M. O'Brien, Shayan Hosseinzadeh, Kimberly I. Verrier, and Tyler J. Humphrey have no conflicts of interest to disclose. Author Christopher M. Melnic is a speaker and paid consultant for Smith & Nephew and receives research support from Zimmer Biomet. Author Antonia F. Chen receives royalties from SLACK publishing, consulting fees from ACI, Stryker, bOne, Pfizer, Avanos, Irrisept, Convatec, 3M, Zimmer, Heraeus, American Medical Foundation, DePuy, is a board member of Recro, receives research support from OREF, and other support from Joint Purification Systems, Sonoran Biosciences, Graftworx, Hyalex, Irrisept. Author Hany S. Bedair receives royalties from and is a paid consultant for Exactech and Smith & Nephew, has stock options in Exactech, receives research support from Zimmer Biomet, and receives royalties from Wolters Kluwer. These conflicts of interest are stated here but are unrelated to the present study.
AUTHOR CONTRIBUTIONS
Todd M. O'Brien and Shayan Hosseinzadeh made substantial contributions to research design, or the acquisition, analysis or interpretation of data and drafting and revising the paper. Antonia F. Chen, Kimberly I. Verrier, Christopher M. Melnic, Tyler J. Humphrey, Hany S. Bedair participated in drafting and revising the paper. All authors have read and approved the final manuscript.