Biomechanical analysis of arthroscopically assisted latissimus dorsi transfer fixation for irreparable posterosuperior rotator cuff tears—Knotless versus knotted anchors
Abstract
We compared the construct stability of traditional knotted techniques with modern knotless anchor systems used in arthroscopically assisted latissimus dorsi transfers (aLDTs) for irreparable posterosuperior rotator cuff tears. Eighteen cadaveric shoulders were age- and gender-matched to the following three groups: knotted group (two knotted anchors); knotless group (two knotless anchors); and triple anchor group (two knotless anchors; one all-suture anchor at the apex of the humeral head). All tendons were cyclically loaded in line of the aLDT over 400 cycles followed by a load to failure test. Outcome measures were the ultimate load to failure, elongation, construct stiffness, and failure modes. The triple anchor group revealed the highest ultimate load to failure (431 ± 78 N) compared with the knotted (326 ± 52 N; p = .022) and knotless (353 ± 105 N; p = .129) groups. Total elongation and construct stiffness were not significantly different comparing all three groups. The failure modes were: anchor pull-out in all specimen of the knotted group; three (50%) anchor pull-out and three suture pull-out in the knotless group (p = .046); four (67%) anchor pull-out, one (17%) suture pull-out and one tendon pull-out in the triple anchor group. Biomechanical analyses of knotless fixation techniques for aLDTs show similar construct stability and elongation compared with the traditional, knotted techniques. Bone fixation seems to be improved with the knotless anchor systems. In our practice, we continue to use the knotless fixation technique for aLDT and in the situation of weak, osteoporotic bone, we add a third (all-suture) anchor to improve construct stability.
1 INTRODUCTION
Rotator cuff tears (RCTs) are common and can cause disruption of the delicately balanced force couple of anterior (subscapularis) and posterior (infraspinatus and teres minor) rotator cuff. Typical functional deficits in irreparable posterosuperior RCTs are weakness of abduction and external rotation with diminished overhead function.1, 2 In younger patients with high demands on their shoulder, shoulder surgeons aim to restore more centered joint mechanics and thus reconstitute the posterior rotator cuff and shoulder function. The latissimus dorsi (LD) tendon transfer can function as such an external rotator and humeral head depressor3 and Gerber et al.2 were the first to describe the latissimus dorsi transfer (LDT) for irreparable posterosuperior RCTs, which became a reliable treatment option to alleviate pain and functional disability associated with irreparable posterosuperior RCTs.1, 2, 4-6
In the original description of Gerber et al.,2 an open double-incision approach involved a superior approach to the rotator cuff for tendon fixation and a second incision over the anterior border of LD muscle belly in the axilla for tendon harvesting. Using the superior approach, the deltoid muscle needs to be detached from its origin at the acromion to access the subacromial space. This bears the risk of deltoid insufficiency if the final muscle to bone repair fails to heal. With the advancements of arthroscopic surgery, shoulder surgeons expanded the LDT to arthroscopically assisted,7 or even all-arthroscopic procedures.8
Besides suture pull-out of the tendon, the most likely failure mode of a transferred tendon is related to the high stresses at the bone–tendon interface,9-11 which may be aggravated in (all-) arthroscopic procedures, where insufficient tendon release leads to even higher tension at this interface. As such, repair failures after arthroscopically assisted LDTs were observed in up to 46% of the cases, depending on the humeral head fixation technique.12 Therefore, a technically feasible, solid tendon-to-bone fixation is needed, especially if the tendon fixation is performed arthroscopically. In the author's institution, tendon transfers around the shoulder were performed over 25 years, and the technique evolved over time. However, especially the transition from open to arthroscopic tendon fixation needed adjustments of the tendon-to-bone anchorage system. During the fixation (i.e., knot tying) the construct is highly loaded, leading to high stress on the suture—anchor–eyelet interface potentially harming the sutures integrity. As we experienced suture breakage during the knot tying using rotator cuff push-in anchors,13 we moved on to a modern knotless suture fixation device.
Thus, the first aim of this biomechanical cadaveric study was to compare primary construct stability and failure modes of the aforementioned two different anchor systems for tendon-to-bone fixation in LDT. Furthermore, we wanted to analyze the potential benefit of an additional third (all-suture) anchor placed at the apex of the humeral head.
We hypothesized that the knotless anchor group will reveal non-inferior ultimate load to failure, construct stiffness, and different failure modes compared with the knotted group and that a third anchor will add significant fixation strength.
2 PATIENTS AND METHODS
The institutional review board and local ethics committee approved this controlled laboratory study.
2.1 Experimental design
We established a biomechanical study design to evaluate the influence of anchor systems and number of anchors on construct stiffness, ultimate load to failure and failure modes of the LDT. We obtained 18 fresh-frozen hemitorsi from Science Care (Phoenix). The mean age was 80.1 ± 8.2 years and there were 9 male and 9 female donors. As determined by CT-scan, all shoulder specimens had intact glenohumeral joints and further CT-scan evaluation included bone mineral density assessment in a 1 × 1 cm area at the anterior portion of the greater tuberosity to ensure comparable bone quality for anchor fixation.14 This region of interest corresponds to the tendon-to-bone fixation area in LDTs.15 There was no significant difference in mean bone density between the three groups (knotted group: 68 ± 54 HU; knotless group: 83 ± 44 HU; triple anchor group: 83 ± 88 HU; p = .898).
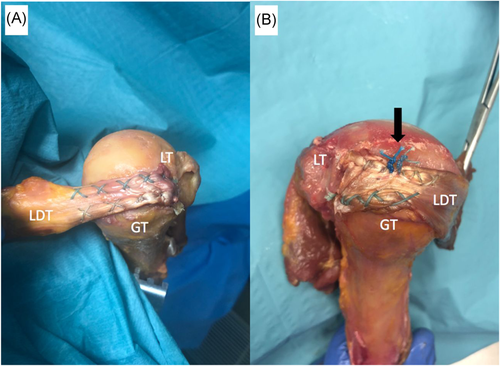
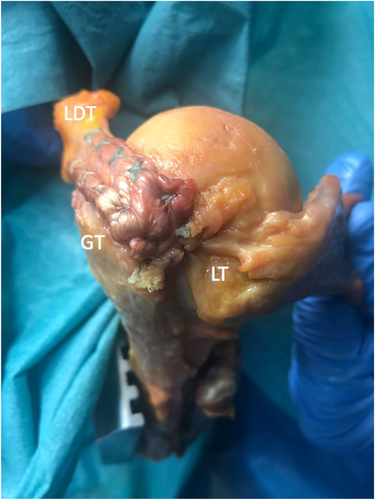
We fixed in all three groups the latissimus dorsi tendon to the anterior aspect of the greater tuberosity with two anchors (Figure 1A). As observed in our experience with LDTs in the situation of weak, osteoporotic bone, an additional fixation point (1 all-suture anchor) at the bone–cartilage interface at the apex of the humeral head may provide additional stability to the transferred tendon and therefore constituted the third testing group (Figure 1B).
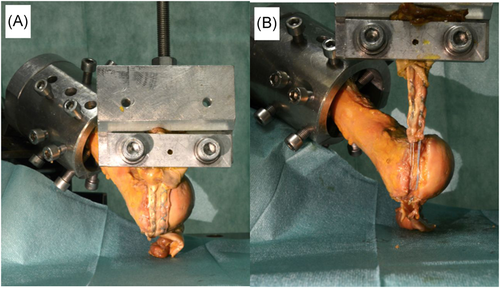
The line of pull along the LDT directed in all groups posteroinferiorly, resembling the in vivo passage between the deltoid and the teres minor in 90° of clinical abduction,2 which corresponds to a line of 60° to the humeral shaft in the coronal plane, and pointing posteriorly in the sagittal plane (Figure 2).
Each group contained randomly assigned specimens and two fellowship-trained shoulder surgeons (Lukas Ernstbrunner and Paul Borbas) conducted the LD tendon harvest and fixation. We used a standardized testing protocol to ensure reproducibility and all testings were conducted on the same day as tissue preparation.
2.2 Specimen preparation
We thawed the 18 age- (within 5 years) and gender-matched fresh-frozen cadaveric shoulders for 24 h under room temperature. The two shoulder surgeons dissected all shoulders using a deltopectoral approach. After removing the skin, superficial tissue, and the pectoralis major muscle, we identified the tendon of the LD, carefully separated it from surrounding tissue, and sharply harvested it from the intertubercular groove. We cut the LD muscle at the level of the distal tip of the scapula. We then dissected the humeral heads free from soft tissues except the subscapularis tendon, and exarticulated and cut the humera 2 cm distal to the deltoid tuberosity. We kept all specimens moist with phosphate-buffered saline to prevent dry out during specimen preparation, surgical repair, and testing.
2.3 Surgical technique
- -
Knotted group (2 SuperQuick anchors; Mitek, DePuy Synthes, Raynham, MA)
- -
Knotless group (2 4.5 mm PEEK ReelX anchors; Stryker, Kalamazoo, MI)
- -
Triple anchor group (2 PEEK ReelX anchors; 1 double-loaded Iconix Speed all-suture anchor; Stryker, Kalamazoo, MI)
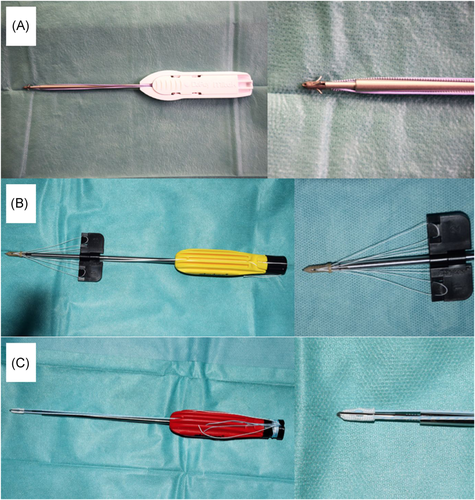
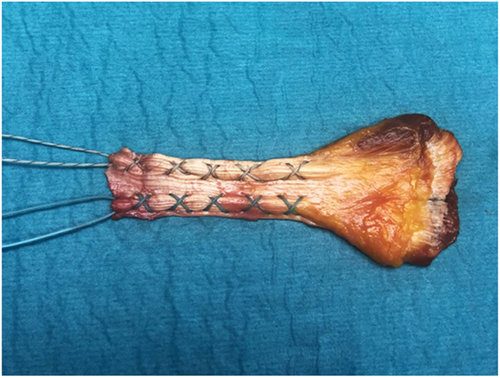
We inserted all anchors according to the manufacturer's description. The harvested LD tendon was loaded with two cords of No. 2 FiberWire (Arthrex) in a 5-crossings stitching technique (Figure 4).
The SuperQuick anchors in the knotted group were unloaded and one free suture limb of each FiberWire cord was pulled through the eyelet of one of the two anchors before insertion. We pulled the transferred LD tendon down to the anterior portion of the greater tuberosity and tied the sutures on top of the tendon with sliding knots.16 In the knotless group, we pulled both free suture limbs of each FiberWire through the eyelet of one of the two ReelX anchors and pulled the LD tendon down to the inserted anchors as per the manufacturer's description. In the triple anchor group, we established an additional fixation point at the bone–cartilage interface at the apex of the humeral head by inserting the double-loaded Iconix Speed suture anchor. We passed one free suture limb of each nonabsorable suture cord through the tendon and tied the sutures in a single-stitch technique on top of the tendon.
2.4 Experimental testing
We fixed the proximal humerus in a custom-made jig, which was adjustable in six degrees of freedom. The humerus was oriented along its shaft axis at an angle of 60° to the LD tendon, which we wrapped around the humeral head so that it directed vertically in line with a large clamp. We secured the muscle belly of the LD with this clamp to spread out the muscle completely for equal clamping stress distribution. We connected the transferred LD tendon to a 20 kN load cell of a uniaxial material testing machine (Zwick 1456, Zwick Roell) and pulled as described above (Figure 5).
We preloaded the tendons to 10 N at 1 N/s over 5 s. After preloading, we performed two successive cyclic non-destructive tests at 0.5 Hz with 200 cycles between 5 and 30 N followed by 200 cycles between 5 and 60 N.17 This was followed by a linear load to failure test at 20 mm/min loading speed.
2.5 Primary outcomes
During cyclic loading, we recorded the applied load as well as the global displacement of the specimen to calculate the construct stiffness of the repair, which was computed as the average slope of the force-displacement curves during cyclic loading. It defines the necessary amount of force (N) to stretch (mm) the construct.17 Furthermore, we calculated the total elongation during each set of the 200 cycles, which is defined as the irreversible elongation from first to the last cycle. After completion of the cyclic loading protocol, we performed a linear load to failure test in order to analyze the ultimate load to failure as well as failure modes, and calculated elongation at failure, which indicates the amount of device elongation which occurred until the ultimate load to failure was reached.
2.6 Statistical analysis
Sample size calculation was based on a comparable biomechanical cadaveric study of LDT fixation techniques.17 We assessed the Normal distribution of data with the Shapiro-Wilk test. We calculated descriptive data using mean and standard deviation. We compared the three groups with the paired t-test. For categorical variables, we used the Fisher exact test. Significance was set as p < .05 and all p values were two-tailed.
3 RESULTS
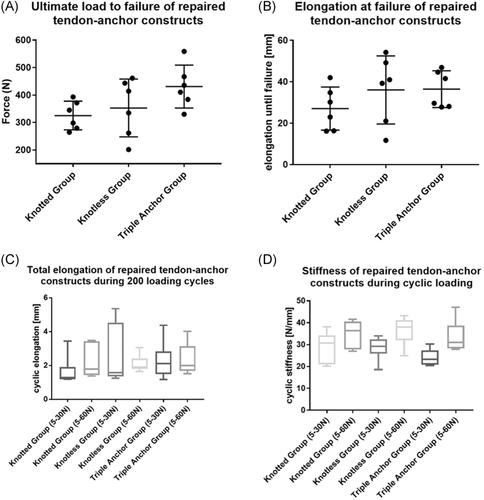
The amount of total elongation was not significantly different comparing all three groups but was the lowest for the knotted group during the 5–30 N loading cycles (1.6 ± 0.9 mm), and higher for the knotless (2.6 ± 1.8 mm; p = .338) and triple anchor groups (2.3 ± 1.1 mm; p = .795). For higher loading cycles, elongation was consistent within all three groups, independent of type or numbers of anchors (knotted, 2.3 ± 0.9 mm; knotless, 2.3 ± 0.7 mm; and triple anchor, 2.4 ± 0.9 mm). There were no significant differences observed in terms of stiffness of the constructs comparing all three groups (p > .05).
Although the knotless- and triple anchor groups showed comparable elongation at failure (36.1 ± 16.5 and 36.5 ± 8.9 mm), the knotted group showed the shortest, yet insignificant, elongation before failure (27.1 ± 10.4 mm; p = .399 [vs. knotless group], p = .159 [vs. triple anchor group]).
Although not statistically significant, the knotless group showed a higher ultimate load to failure compared with the knotted group (353 ± 105 N vs. 326 ± 52 N; p = .615). The triple anchor group revealed the highest forces (431 ± 78 N) compared with the knotted (326 ± 52 N; p = .022) and knotless (353 ± 105 N; p = .129) groups.
The reason for failure in all specimens of the knotted group was anchor pull-out (100%), whereas in the knotless group, half had an anchor pull-out (50%) and the other half a suture pull-out (p = .046). In the triple anchor group, four had an anchor pull-out (67%), one suture pull-out (17%), and the remaining one a tendon pull-out (17%). Further details are presented in Table 1 and Figure 6.
| Variable* | Knotted group | Knotless group | Triple anchor group | p (knotted. vs. knotless) | p (knotless vs. triple anchor) | p (knotted vs. triple anchor) |
|---|---|---|---|---|---|---|
| Ultimate load to failure, N | 325 ± 52 | 352 ± 105 | 431 ± 78 | .615 | .129 | .022 |
| Elongation at failurea, mm | 27.1 ± 10.4 | 36.1 ± 16.5 | 36.5 ± 8.9 | .399 | .939 | .159 |
| Total elongation, 5–30 N cyclesb, mm | 1.6 ± 0.9 | 2.6 ± 1.8 | 2.3 ± 1.1 | .338 | . 795 | .299 |
| Total elongation, 5–60 N cyclesc, mm | 2.3 ± 0.9 | 2.3 ± 0.7 | 2.4 ± 0.9 | .977 | .929 | .942 |
| Construct stiffness, 5–30 N cyclesd, N/mm | 29.0 ± 7.0 | 28.6 ± 5.3 | 24.1 ± 3.8 | .888 | .080 | .223 |
| Construct stiffness, 5–60 N cyclese, N/mm | 35.0 ± 6.1 | 36.5 ± 6.4 | 33.6 ± 7.3 | .508 | .358 | .730 |
| Failure modes, n (%) | ||||||
| Anchor pull-out | 6 (100) | 3 (50) | 4 (67) | n.a. | n.a. | n.a. |
| Suture pull-out | 0 | 3 (50) | 1 (17) | n.a. | n.a. | n.a. |
| Tendon pull-out | 0 | 0 | 1 (17) | n.a. | n.a. | n.a. |
- * Data are presented as mean ± standard deviation.
- a Elongation at failure indicates the amount of device elongation which occurred until the ultimate load to failure was reached.
- b Total elongation during 200 cyclic loading between 5 and 30 N is defined as the irreversible elongation from first to the last cycle.
- c Total elongation during 200 cyclic loading between 5 and 60 N is defined as the irreversible elongation from first to the last cycle.
- d Construct stiffness was measured during 200 cyclic loading between 5 and 30 N as the overall stiffness of tendon, suture, and anchoring. Stiffness is defined as the necessary force to elongate a construct over a defined distance.
- e Construct stiffness was measured during 200 cyclic loading between 5 and 60 N as the overall stiffness of tendon, suture, and anchoring. Stiffness is defined as the necessary force to elongate a construct over a defined distance.
4 DISCUSSION
Shoulder surgeons advanced the LDT from an extensive open procedure to an arthroscopically assisted,7 or even all-arthroscopic procedure.8 There are, however, certain failure modes associated with high stresses at the bone–tendon interface,9-11 which may be aggravated in (all-) arthroscopic procedures due to insufficient tendon release. The reported repair failure rate after arthroscopically-assisted LDTs is up to 46%.12 We performed LDTs over the last 25 years at our institution and especially the transition from open to arthroscopic tendon fixation needed adjustments of the tendon-to-bone anchorage system. During that time, we experienced suture breakage during the knot tying using rotator cuff push-in anchors (knotted group in the current study).13 We, therefore, moved on to a modern knotless suture fixation device (knotless group in the current study) and started using an additional fixation point (1 all-suture anchor) at the bone–cartilage interface at the apex of the humeral head in the situation of weak, osteoporotic bone (triple anchor group in the current study).
The main finding of this biomechanical cadaveric study of different anchor-fixation techniques for arthroscopic LDTs is that the recently introduced knotless fixation technique shows similar construct stiffness, elongation, and ultimate load to failure compared with the traditional, knotted anchor technique used with open surgery. Failure modes were significantly different, with anchor pull-out in all shoulders of the knotted group compared with 50% anchor pull-out in the knotless group, suggesting that bone fixation is superior with the knotless ReelX anchors. We also observed that significantly higher construct stability can be achieved by adding a third (all-suture) anchor at the apex of the humeral head, which should be considered especially in the situation of weak, osteoporotic bone.
The LDT has been described to reconstitute the posterior rotator cuff and force couple in younger patients with irreparable posterosuperior RCTs.1, 2, 4-6 It usually internally rotates, adducts, and extends the humerus, but when transferred to the greater tuberosity, the LDT functions effectively as an external rotator and humeral head depressor that is counterbalanced by the deltoid and intact subscapularis.1-3
The original description of Gerber et al.,2 which involves an open double-incision approach, one superior approach to the rotator cuff and another incision in the axilla just over the anterior border of latissimus dorsi muscle belly, was recently expanded with the advancements of arthroscopic surgery, and arthroscopically assisted7 or even all-arthroscopic techniques8 have been described. The all-arthroscopic technique may have the main disadvantage that an appropriate release of the latissimus dorsi muscle belly is difficult, making it almost impossible to transfer the tendon to the desired fixation point at the anterior part of the greater tuberosity and leading to a high tension at the tendon-to-bone fixation interface. In contrast, the arthroscopically assisted LDT allows for an appropriate latissimus dorsi release and offers some potential benefits over the open technique such as the iatrogenic deltoid insufficiency can be avoided18; the remaining posterosuperior rotator cuff as well as subscapularis lesions can be detected and effectively repaired; and the passage of the tendon between the posterior deltoid muscle and the teres minor can be visualized and prepared arthroscopically, making it easier to define this interval through the axillary incision.
High stresses at the tendon–bone interface is the main failure mode reported in tendon transfers.9-11 The overall tendon rupture rate of 258 pooled arthroscopic assisted LDTs is 2.7%.6 Although this number indicates that fixation failures involve only a small proportion of all arthroscopic (assisted) LDTs, its reported incidence goes up to 46% in certain case series.12 Failure at the tendon–bone interface may be attributed to the anatomy of the latissimus dorsi tendon, which was described as a long and broad but very thin tendon.19 As such, fixation quality is of tremendous importance and with the advancements of anchor systems, we have adapted our technique for arthroscopically assisted LDTs from traditional knotted anchors to modern knotless anchor systems.
The ultimate load to failure in the knotless group was not higher compared with the knotted technique. The limited number, age, and bone quality of shoulders used in each group may be one of the reasons why the ultimate load to failure comparing the knotted with the knotless group was not statistically significant besides an absolute difference of 27 N favouring the knotless group. The observed construct strengths in both (knotted and knotless) groups were higher by approximately 100 N compared with a previous biomechanical analysis of LDT fixation techniques using an interference screw versus suture anchors.17 This may be due to different/better fixation techniques, but may also be attributed to the different lines of pull, which was in our study along the in vivo passage of the LDT in posteroinferior direction between the deltoid and the teres minor and not perpendicular to the fixation construct.17
There were significant differences in failure modes comparing all three groups. All anchors in the knotted group failed by anchor pull-out, which was significantly different compared with the knotless group, where half had an anchor pull-out and the other half a suture pull-out. Four specimens in the triple anchor group had an anchor pull-out, the remaining two had a suture pull-out or tendon pull-out. This difference in failure modes may indicate that bone fixation is superior with the knotless ReelX anchor. Our failure modes are in contrast to a previous biomechanical study looking at fixation techniques in arthroscopic LDTs, as none of their constructs in the anchor group failed by anchor pull-out.17 This, however, needs to be interpreted in light of the fact that ultimate load to failure was lower in their study, and failure modes may be similar to our results with loads beyond 300 N and similar tendon loading with the 5-crossings stitching technique. Furthermore, although Diop et al.17 used four Twinfix PK 6.5 mm anchors (Smith and Nephew), failure loads are known to be lower with Twinfix anchors compared with ReelX anchors used in the current study.20 Another limitation associated with our biomechanical model is that it can only address the primary, postoperative properties of the tested fixation techniques. Also, the applied loads were realistic but cannot resemble in vivo conditions.
Although not studied, insufficient suture reinforcement of the tendon may be another failure mode. Previous reports emphasized therefore the use of an additional allograft tendon to cover and further reinforce the tendon suture interface.21, 22 This biomechanical study showed that the used 5-crossings stitching technique (Figure 4) provided a solid and strong tendon reinforcement, as tendon pull-out was only observed once as a failure mode.
The highest ultimate load to failure was achieved by adding a third (knotted all-suture) anchor in addition to the 2 knotless anchors. To the best of our knowledge, this is the first study confirming our hypothesis, that a third anchor at the bone–cartilage interface at the apex of the humeral head provides additional stability to the transferred tendon. We usually use such additional stabilization to avoid a potential windshield wiper effect of the transferred tendon and especially in weak bones, which was proved to provide higher ultimate loads to failure in an osteoporotic bone model.23
Total construct elongation was higher in the knotless and triple anchor group during the initial 30 N cycles than in the 60 N cycles, indicating the need for higher tensioning forces to allow the friction-dependent mechanism of sutures to work. Under the higher loading protocol, in which all anchors were already tensioned over 200 loading cycles, total elongation was almost identical comparing all three groups and showed a nonlinear increase in mean total elongation, a phenomenon that was also observed in a similar biomechanical study.17 Although meticulous care was taken to minimize the following, elongation until failure could be partially influenced by a cheese-wiring effect of sutures cutting through the tendons and/or slippage at the clamps.24
Unique in this study is that in all groups ultimate construct failure (e.g. anchor pull-out) was observed after more than 20 mm of construct elongation. Failure of arthroscopically assisted LDTs most frequently occur at the bone–tendon interface,11, 12 and elongation at failure of more than 20 mm was also observed in clinical studies, which is significantly associated with inferior objective and subjective results.11
In conclusion, biomechanical analyses of knotless fixation techniques for arthroscopic LDTs show comparable ultimate load to failure, construct stiffness, and elongation compared with the traditional, knotted techniques. Both techniques provide sufficient fixation strength of up to 350 N with low elongation after cyclic loading, but bone fixation seems to be improved with the knotless anchor systems. In our practice, we continue to use the knotless fixation technique for aLDT and in the situation of weak, osteoporotic bone, we add a third (all-suture) anchor to improve construct stability.
ACKNOWLEDGMENTS
This study was funded by the Alwin Jaeger Foundation. Material support was provided by Stryker (anchor systems) and Arthrex (suture material). Neither the foundation nor the companies had an influence on study design, data collection, or interpretation of the results or the final manuscript. None of the mentioned authors had received personal financial support related to this study.
AUTHOR CONTRIBUTIONS
All authors have made substantial contributions to all of the following: (1) the conception and design of the study (Lukas Ernstbrunner, Paul Borbas, Elias Bachmann, Karl Wieser), (2) acquisition of data (Lukas Ernstbrunner, Paul Borbas, Marco Rohner, Sascha Brun), (3) analysis and interpretation of data (Lukas Ernstbrunner, Paul Borbas, Sascha Brun, Elias Bachmann), and (4) drafting the article or revising it critically for important intellectual content (Lukas Ernstbrunner, Paul Borbas, Elias Bachmann, Samy Bouaicha, Karl Wieser). All authors have read and approved the final submitted manuscript.