In vivo test of a radiography-based navigation system for control of derotational osteotomies
Abstract
Malalignment of the femur is a frequently encountered problem in orthopaedics entailing manifold consequences for the affected patients. Corrective osteotomies, necessary to restore the physiological and anatomical relationships, face great challenges due to no existing reliable gold standard for intraoperative control of torsional malalignment. The aim of this study was to test a novel radiography-based navigation tool for control of derotational osteotomies in a clinical environment. In a first—and preliminary—case-controlled study on 12 patients (level 3 of evidence), the achieved torsional correction measured with implementation of the navigation tool was compared with measurements from pre- and postoperative computed tomography (CT) scans.
The navigation tool was able to acquire and process all relevant data and capture possible malrotation during surgery with only little deviations of 1.61° ± 0.86° (mean ± standard deviation) from the measurements based on CT scans. Next, the system will be used to assist surgeons for more precise treatment avoiding maltorsion after derotational osteotomies.
1 INTRODUCTION
Being congenital or caused by fracture treatment, malalignment of the femur is a frequently encountered problem in orthopaedics and traumatology.1 Especially after intramedullary nailing of femoral shaft fractures maltorsion of more than 15° occurs in 15% to 41% of all patients.2-4 Consequences are hip and/or knee pain that might be accompanied by restricted movement.2, 5, 6 Another long-term problem following torsional malalignment of the femur is related to the risk of degenerative osteoarthritis of the knee and/or hip.7, 8 A recent finite element study reported initiation of significantly higher stresses in the patellofemoral joint at 10° maltorsion.9 Moreover, previous biomechanical work revealed a significantly higher stress in the knee joint at only 5° maltorsion.1 In case of existing malalignment leading to clinical complaints, a corrective osteotomy has to be considered to restore the physiological and anatomical relationships.10
The treatment procedure, being most commonly described in the literature, applies the Schanz pins principle, as proposed by Strecker and Dickschas11 and further developed by Schröter et al.12 It is technically challenging and may result in deviations of up to 15°.4 According to Vetter et al,4 33% of the patients suffer from residual deformities of more than 10°. All procedures require a postoperative computed tomography (CT) or magnetic resonance imaging to check for possible remaining torsional malalignment.
Currently, there is no existing gold standard for intraoperative control of torsional correction. Computer-assisted systems might be helpful, but lack wider acceptance due to high costs, complexity during usage and difficulties to be integrated into standard clinical routines. Weil et al13 reported a prolonged surgery by approximately 30 to 35 minutes if navigation is applied. Additionally, despite high personnel and technical efforts, torsional malalignment of up to 7.7° remains.
Therefore, our objective was to develop an efficient intraoperative measurement tool to improve surgical precision and consequently avoid complications related to corrective osteotomies. The aim of this study was to prove the method in a clinical environment and to test its feasibility.
2 MATERIALS AND METHODS
2.1 Radiography-based navigation tool
By using an existing technology platform,14 we developed a radiography-based navigation tool for derotational osteotomies. The underlying principle was proposed and developed by Windolf et al.14 and is based on determining the spatial position and orientation of cylindrical holes from their lens-shape projections in X-ray images. The explicit nature of the projections allows for accurate, robust, and distinct calculation of the spatial orientation of an object equipped with a known hole pattern from a single X-ray image.
The realized prototype for corrective osteotomies utilizes a conventional C-arm as imaging and navigation means. It consists of two radiopaque reference flags made of medical grade stainless steel (316L, electropolished, passivated) featuring a defined hole pattern, and an image-processing unit connected to the C-arm (Figure 1).
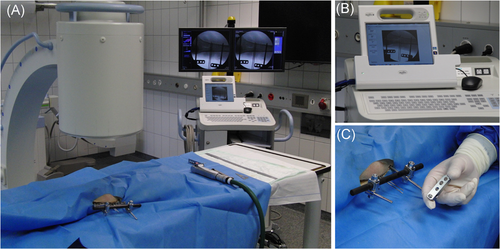
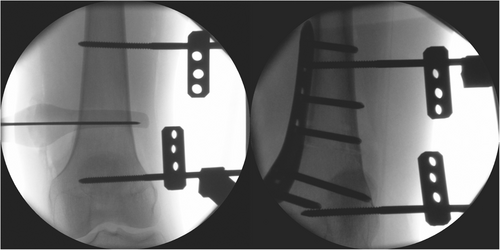
The reference flags serve as markers for tracking of the performed correction and are clamped to the Schanz pins, which are routinely attached to the proximal and distal bone fragments (Figure 2). An image acquisition device (VGA frame-grabber, AV.io HD, Epiphan Systems Inc, Ottawa, Canada) connects an external computer to the monitor output signal of the C-arm, which allows image transfer and processing. The software algorithm (Matlab, Mathworks Inc, Natick) automatically detects both reference flags in an X-ray image and computes their spatial relation. A first image defines a baseline scene of the preosteotomy state (Figure 2A). After osteotomizing, the performed anatomical correction can be tracked from a successive X-ray image with respect to the baseline in terms of torsion, curvature, and varus-valgus angles (Figure 2B).

2.2 System test and accuracy assessment
A benchmark test was conducted to test the system and assess the accuracy. Two cylindrical artificial bone fragments (SYNBONE, Malans, Switzerland) were axially aligned and vertically mounted on a testing machine (MTS Mini Bionix II 858; MTS Systems Corp, Eden Prairie, MN). One of the fragments was fixed to the machine base, whereas the other was attached to the torsional actuator. Each fragment was equipped with Schanz pins and marker flags. Torsional correction was simulated by rotating the fragment at the machine actuator around its longitudinal axis in 5° steps from −30° to 30°. A radiographic image was captured after each step using a C-arm (Siemens Arcadis Varic, Siemens Healthcare GmbH, Erlangen, Germany). This procedure was repeated five times using five different C-arm positions. The captured radiographs were processed with the software and the torsion was calculated with respect to the initial image at 0°.
Accuracy was assessed according to the definition from Schröter et al15 by mean and standard deviation of the absolute differences between measured and actual rotation of the machine actuator.
2.3 Clinical investigation
2.3.1 Design
This study is classified as a case-controlled study, level of evidence 3. The study was approved by the local ethics committee (309/2016BO1). All patients gave informed consent to participate.
The routinely used intraoperative radiographs with the visible markers were saved and processed retrospectively. No intraoperative feedback was given to the surgeon. Performed derotational osteotomy was calculated after the surgery and compared to the results from a three-dimensional (3D) registration method based on pre- and postoperative CT scans.
2.3.2 Patients
Eighteen patients were considered for the study, six being with congenital deformities (three complex ones) while 12 suffered from posttraumatic torsional malalignment. Two patients were excluded due to medical issues. Another patient dataset could not be used because the repair-construct was altered after the very final X-ray image. For three patients not all necessary analyses could be done due to incomplete intraoperative image storing. As a result, 12 patients (three males, nine females) were included in the analysis (mean age 36 years, range: 22-74).
2.3.3 Clinical procedure
Preoperatively, torsional alignment was measured via CT applying the Waidelich method16 and using the contralateral leg to calculate the required rotation angle. During surgery, when possible, the osteotomy plane was marked by two k-wires. The proximal Schanz pin was inserted into the bone. A triangular metal wedge (DePuy Synthes, Zuchwil, Switzerland) was used for placing the distal Schanz pin in the desired corrective angle in the axial plane. This procedure was performed in accordance with the approach described by Schröter et al12 Additionally, an external fixator was mounted and both reference flags were attached to the Schanz pins (Figure 3).
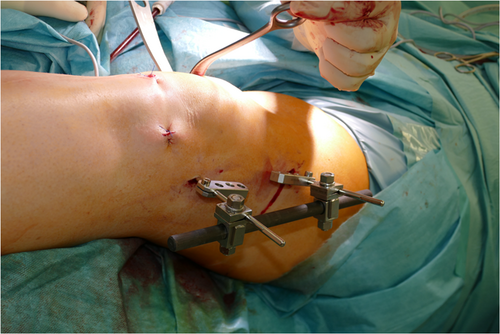
Following, an X-ray image was taken and stored to verify the correct osteotomy plane. A transverse osteotomy was then performed with an oscillating saw. The external fixator was partially loosened and the fragments were rotated such that the Schanz pins were visually aligned in the axial plane. Then, the external fixator was retightened and internal fixation was performed either with an intramedullary nail or a plate. The final X-ray was taken and the Schanz pins were removed. Figure 4 depicts exemplarily an X-ray image before osteotomizing (baseline, Figure 4A) and after plate positioning (Figure 4B). All images were taken with a Siemens Arcadis Varic C-arm and stored as Digital Imaging and Communications in Medicine (DICOM) files.
Clinical CT scans (SOMATOM Definition Edge, Siemens Healthcare GmbH, Erlangen, Germany) of the hip, knee, and ankle were performed pre- and postoperatively.
2.3.4 Data evaluation
The intraoperatively obtained radiographic image pairs (baseline and final image) were processed after surgery using the developed image-processing algorithm. The torsional corrections were computed for all patients.
The pre- and postoperation CTs were imported into Amira software (Amira V6.4.0; FEI Company, Hillsboro, OR) as a comparative reference and each performed torsional correction was measured applying a two-step 3D registration procedure. First, the postoperative CT scan of the treated femur was aligned to the preoperative scan by registering and superimposing the proximal parts. In the second step, the distal femoral region was accordingly registered. The resulting transformation returned the torsional correction as rotation around the longitudinal bone axis.
The average difference and standard deviation were calculated between the radiographic and CT based results as a measure for accuracy15 of the newly developed navigation tool.
The accuracy of the navigation tool was measured as described in Schröter et al15 by the mean and standard deviation of the absolute differences between the radiographic and CT based results. Additional linear regression analysis was employed on these two parameters.
3 RESULTS
The developed navigation tool prototype processed all acquired X-ray images during the benchmark testing without systematic errors and with resulting accuracy of 0.61° ± 0.65°. These results were deemed sufficient to enter into first clinical trials.
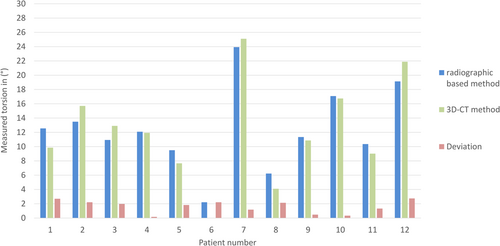
The measured torsional correction in 12 patients is presented in Figure 5 for both the radiography-based navigation tool and the 3D CT based method. The red bars indicate the deviations between the two methods, which are a minimum 0.2° and 2.7° maximum. The resulting accuracy of the newly developed navigation tool derived from the clinical data were 1.61° ± 0.86°.
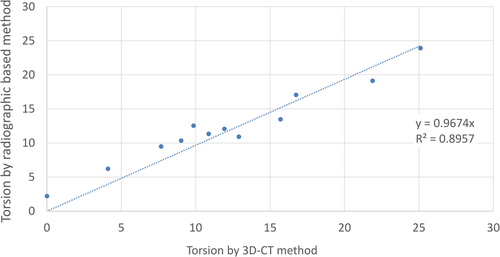
The linear regression analysis revealed a strong correlation between radiographic and CT measurements (R2 = .9, Figure 6).
4 DISCUSSION
To date, there is no existing gold standard for intraoperative control of torsional correction when performing derotational osteotomies. So far, no intraoperative measuring aid has gained broader acceptance in clinics. We developed and tested a simple and efficient navigation tool for this purpose. The results from this preliminary in vitro and clinical study are encouraging with regard to revision surgeries and congenital torsional deformities. We could show that the proposed navigation system was able to measure relevant data capturing possible malrotations during surgery. Overall, the proposed navigation tool works reliably and accurately with a maximum error of 2.7° detected among all measurements and patients. However, the system is still in a prototype state, applied in a blinded clinical study design without intraoperative feedback to prevent any risk of malrotation from potentially erroneous system output. Further studies with a validated and regulated medical device with integrated intraoperative feedback are necessary. Such a system would allow surgeons to accurately control torsion directly during surgery in order to prevent excessive maltorsion. This would lead to a significant enhancement of the torsional correction procedures, as they currently often require time-consuming setting up of the equipment, are complex to operate and thereby prolong the surgery, as it is for example the case with application of fluoroscopic-based computerized navigation systems. Currently, despite the use of computerized navigation systems, maltorsions of up to 7.7° still remain (2.9° on average among all treated patients).13 Vetter et al4 reported 33% of patients with remaining deformities of more than 10°. Weil et al13 stated that there is no clear evidence for decrease of femoral maltorsion with the use of current assistance techniques.
Moreover, all procedures performed during surgery, such as the cortical step sign or the lesser trochanter profile, require a CT scan after surgery to control for potential torsional errors. To date, a postoperative CT scan measurement is universally accepted as an accurate measurement of femoral torsion.17 However, this imaging step would be redundant with the use of the proposed navigation tool, thus reducing the overall radiation exposure.
The following advantages of the proposed navigation tool are essential. The system is simple to integrate into current surgical procedures and existing clinical workflows, including the use of a standard C-arm. A significant increase in surgery time is not expected as the only additional step includes the attachment of the described metallic markers to the Schanz pins.
Potential risks of the system use include the possibility of an unintended rotation of the markers around the Schanz pins or rotation of the pins themselves inside the bone. In such a case, the reference to the bone gets changed and in turn negatively affects the results. Even though the system includes detection methods, it cannot fully consider such mistakes during calculation, thus implying a risk of calculating wrong values. Furthermore, one prerequisite for the system is X-ray imaging during surgery, which could impose the patient to a certain dose of radiation. In this study no additional X-ray imaging was necessary and all relevant data could be captured with the routinely taken X-ray images during the surgical workflow. However, in some cases, an additional X-ray image might be necessary. However, during a postoperative CT scan for verification of the correct torsional alignment, the patient is exposed to an even higher amount of radiation.
A limitation of the system is that it performs measurements via snapshots of the surgical field and hence does not give real-time feedback to the surgeon. Another possible restriction might be related to the field of the C-arm view—in order to capture both markers in one image, it is necessary to position the C-arm very close to the patient. During our investigation, this was not a problem in any of the cases. Furthermore, conventional C-arms might have distortions in their peripheral regions of the images. This problem differs depending on the used C-arm. The analyzed images might be erroneous if the marker flags are depicted in the peripheral regions of the image. Furthermore, the range of torsion registration is limited to approximately ±30° in relation to the image plane due to holes’ disappearance in the projection. However, this is expected to be a rather theoretical problem, as large torsional corrections of more than 30° are seldomly conducted. For example, Vetter et al4 reported 6.6% of patients with such excessive corrections (including one patient with a torsional correction of 38°).
Finally, it has to be kept in mind that the system can only help execute surgical planning. Being assisted by the navigation system, precise planning and angle measurements have to be done by the surgeon. All in all, the scope of the system application is for corrections of existing maltorsion. Of course, it would have been better to avoid them right in the beginning. However, cases, where corrections of maltorsion are necessary, will always exist. Our system is promising as an assistant navigation tool to control intraoperatively performed over- or under-corrections of torsional malalignment. Probably it will be a useful navigation tool even in primary surgeries with the use of intramedullary nails. For example, in case of femoral fracture fixation using an external fixator when a torsional CT scan could give information of the torsion and the Schanz pins combined with the flags could be used for intraoperative control.
Additionally, following its validation, the proposed navigation system can be implemented in procedures for corrections of varus or valgus, flexion, or extension, as well as for translational corrections.
5 CONCLUSION
The current study proved the ability of the proposed radiography-based navigation system to measure all relevant data and to capture possible femoral malrotations during surgery with only little deviations from the standard measurements with the use of CT scans. Further development steps are necessary for the introduction of the system in the clinics as an assisting tool helping the surgeons to operate more precisely, avoiding malrotations.
ACKNOWLEDGMENTS
The authors are not compensated and there are no other institutional subsidies, corporate affiliations, or funding sources supporting this work unless clearly documented and disclosed. This study was performed with the assistance of the AO Foundation via the AOTC System.
AUTHOR CONTRIBUTIONS
MW and JB developed the system, JB processed and evaluated the data. LG developed the idea of the in vivo study and was responsible for ethical approval. SS and LG performed the in vivo part and acquired the data. All authors contributed to the study design. LG, JB, and MW interpreted the data. LG wrote the manuscript. JB, SS, MW, BG, and GR provided critical revision. All authors have read and approved the submitted version.