Pelvic tilt between supine and standing after total hip arthroplasty an RSA up to seven years after the operation
This manuscript is part of my thesis with the title “Wear and migration in total hip arthroplasty measured with Radiostereometric Analysis,” which was defended in February 2018.
Abstract
The pose of the prosthetic components after total hip arthroplasty (THA) is commonly evaluated on conventional radiographs. Any change of the pelvic position after the operation in supine and between supine and standing position with time will influence validity of the measurements. We evaluated the changed pelvic tilt angle (PTA) in supine and standing position up to 7 years after operation. The aims of our study were (a) to evaluate if the PTA change over time after THA, (b) to assess any difference in PTA between supine and standing positions, and (c) to investigate whether factors such as gender, the condition of the opposite hip or low-back pain have any influence on PTA after THA. Repeated radiostereophotogrammetric radiographs of 106 patients were studied. Patients had been examined in the supine position postoperatively, and in both supine and standing positions at 6 months and 7-year follow-up. Measurements of supine patients showed an increasing mean posterior pelvic tilt over time. From supine to standing, the pelvis tilted in the opposite direction. At 6 months, the mean anterior tilt was 3.6° ± 3.8° (confidence interval [CI]: 2.8° to 4.3°) which increased to 6.4° ± 3.9° (CI: 5.7° to 7.2°) at 7 years. The mean changes in pelvic rotations around the longitudinal and sagittal axis were less than 1 degree, in both positions. In individual patients, this change reached about 11.0 degrees in supine and 18.0 degrees when standing.
1 INTRODUCTION
Orientation of the acetabular component during total hip arthroplasty (THA) is essential to avoid complications such as dislocation, impingement and accelerated bearing wear, which can lead to osteolysis around the implant and cause loosening.1-4
Dislocations are one of the most frequent complications after THA, leading to revision surgery.5, 6 Posterior dislocations are reported to occur more often, however, anterior dislocations account for about 20% of all dislocations.7-10 Despite proper positioning of the acetabular component, the risk of dislocation may vary due to factors such as patient's characteristics, implant design, and surgical technique.11, 12 Implant instability and asymmetrical loading of the acetabular component may also be an effect of excessive pelvic tilt. Pelvic tilt is defined as the angle between the anterior pelvic plane and a vertical line in the standing position. The rotation of the pelvis leads to anterior tilt (the upper portion of the pelvis tips forward) and posterior tilt (upper portion of the pelvis tips backward).13 There is an increasing interest in the relation between the pelvic position and presence of spinal deformities or disease since such disorders might influence the risk of dislocation after THA.
The orientation of the cup after operation with THA is commonly evaluated on standard pelvic radiographs, which routinely are exposed in the supine position. However, most activities of daily living are performed in the upright position. The orientation of the cup relative to the pelvis is set during the operation, but the pelvic tilt might change when the patient is mobilized, partly because of release of contractures during the operation and partly because of subsequent stretching of the soft tissues with time. Such changes might influence the validity of determination of cup orientation based on supine radiographs. Radiostereometric analysis (RSA) enables accurate evaluations14-16 of changes in the pelvis orientation, such as supine and standing and over time. Detailed studies of changes in pelvic tilt between supine and standing and over time may be of value when interpreting the cup orientation after THA using conventional radiography. Increased knowledge in this field may be of value to optimize the outcome of hip arthroplasty and may also facilitate our understanding of issues related to impingement and instability after THA.
We aimed to use RSA to evaluate if PTA changes over time in patients with total hip prosthesis and if the pelvic tilt differs between supine and standing positions at 6 months and 7 years after the operation. We also evaluated whether factors such as gender, the status of the opposite hip, or presence of any low-back disability influence the PTA after THA. To our knowledge, this is the first report on changes of pelvic tilt using RSA in patients operated with THA.
2 PATIENTS AND METHODS
2.1 Level of evidence: level II, diagnostic study
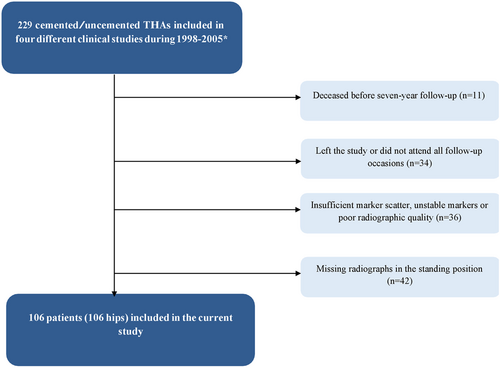
One hundred and six patients (106 hips) were selected from four different studies. All the patients underwent THA and were included in prospective clinical RSA trials evaluating cup migration and femoral head penetration at Sahlgrenska University Hospital between 1998 and 2005 (Figure 1). During the operation, tantalum markers had been inserted into the bone and the polyethylene liner or the cup. The selection criteria were patients who underwent cemented or uncemented THA for primary or secondary osteoarthritis (OA) of the hip and who were scheduled for follow-up including supine and standing examination on at least two occasions (at 6 months and 7 years after surgery), in addition to the supine postoperative RSA examination. The purpose of examining patients in supine and standing positions was to evaluate any potential differences in femoral head penetration between these two positions.20 Only hips marked in the segment of interest, that is, the acetabular bone with at least three tantalum markers or more and with a scatter corresponding to a condition number less than 125 and a mean error of rigid body fitting corresponding to at most 0.35 mm were included.21, 22 One hundred and six patients (106 hips) fulfilled the inclusion criteria (Figure 1). All patients had provided informed consent for the insertion of tantalum markers during the operation and the subsequent RSA examinations. Approval was obtained through the Regional Ethics Committee, S 257-00, R312-98, Ö449-00, and Ö450-00. Patient demographic data are presented in Table 1.
| Gender | |
| Male | 39 |
| Female | 67 |
| Age, y | 59 (30-78) |
| Weight, kg | 75 (51-112) |
| Height, cm | 170 (155-195) |
| BMI, kg/m2 | 26 (19-35) |
| Bilateral THA | |
| No | 42 |
| Yes | 48 |
| During the follow-up | 16 |
| Low-back pain | |
| No | 78 |
| Yes | 28 |
| Contralateral hip at 7 y | |
| Normal | 14 |
| Osteoarthritis | 28 |
| THA | 64 |
- Abbreviation: THA, total hip arthroplasty.
The primary outcome parameter was the pelvic rotations about the transverse axis (anterior or forward tilt [+] and posterior or backward [−] tilt) (Table 2A). Pelvic rotations about the other two axes (longitudinal, y-axis, and sagittal, z-axis) are also presented (Tables 2B and 2C).
| n | Mean (SD) | 95% CI | P valuea | |
|---|---|---|---|---|
| Supine | .010 | |||
| Postoperative—6 mo | 106 | −2.0° (3.0°) | −2.6° to −1.4° | |
| Postoperative—7 y | 106 | −2.7° (2.9°) | −3.3° to −2.2° | |
| Supine to standing | ||||
| 6 mo | 106 | 3.6° (3.8°) | 2.8° to 4.3 | <.001 |
| 7 y | 106 | 6.4° (3.9°) | 5.7° to 7.2° |
- Abbreviations: CI, confidence interval; SD, standard deviation; THA, total hip arthroplasty.
- a The Student t test.
| n | Mean (SD) | 95% CI | P valuea | |
|---|---|---|---|---|
| Supine | ||||
| Postoperative—6 mo | 106 | 0.66° (3.1°) | 0.06° to 1.3° | .31 |
| Postoperative—7 y | 106 | 0.34° (3.1°) | −0.26° to 0.95° | |
| Supine to standing | ||||
| 6 mo | 106 | 0.37° (4.2°) | −0.1.2° to 0.44° | .49 |
| 7 y | 106 | −0.05° (3.9°) | −0.80° to 0.69° |
- Abbreviations: CI, confidence interval; SD, standard deviation; THA, total hip arthroplasty.
- a The Student t test.
| n | Mean (SD) | 95% CI | P valuea | |
|---|---|---|---|---|
| Supine | ||||
| Postoperative—6 mo | 106 | −0.59° (3.7°) | −1.3° to 0.13° | .39 |
| Postoperative—7 y | 106 | −0.86° (3.5°) | −1.5° to -0.17° | |
| Supine to standing | ||||
| 6 mo | 106 | 0.51° (3.7°) | −0.21° to 1.2° | .49 |
| 7 y | 106 | 0.75° (3.4°) | 0.09° to 1.4° |
- Abbreviations: CI, confidence interval; SD, standard deviation; THA, total hip arthroplasty.
- a The Student t test.
Of 106 patients, 42 had a unilateral hip prosthesis throughout the study period, 16 patients underwent surgery with a hip prosthesis on the contralateral side during the follow-up period of 7 years and 48 patients had bilateral hip prosthesis when the study was initiated. In this latter group, and in those patients with both hips followed with RSA, the hip with the optimum scatter and visibility on stereoradiographs of tantalum markers in the pelvis was selected. To determine the condition of the contralateral hip in patients with a unilateral prosthesis at the last follow-up (n = 42), conventional radiographs were reviewed. They revealed that 14 patients had a normal hip and 28 suffered from OA on the contralateral side.
We also reviewed the medical records of all patients regarding the incidence of low-back pain. A history of low-back pain was considered to be or to have been present if the patients had visited our department because of this condition during the follow-up or had complained of low-back pain at any follow-up visits after the hip operation. In 28 of the 106 patients, low-back problems had been documented. None of the patients had undergone spinal fusion. We also reviewed the medical records of all patients regarding the incidence of hip dislocation corresponding to a mean follow-up period of 12 years (range: 7-16 years) after operation. None of the patients had undergone revision surgery due to hip dislocation.
2.2 Radiostereometric analysis
For the purpose of this study, we calculated the motions of tantalum markers inserted into the pelvis (the pelvic bone segment) in relation to the coordinate system defined by the calibration cage. These motions are by convention labeled absolute motions of the pelvic bone or segment. In this way, true positional changes of the pelvis represented by markers in the acetabulum can be determined between different positions such as supine and standing or over time with the patient examined in the same or at varying positions.
During the operation, spherical tantalum markers with a diameter of 0.8 mm or 1.0 mm diameter were inserted into the bone and into the polyethylene of the cup. Although only three visible and well-defined markers in each segment of interest are necessary for a complete radiosterometric evaluation, five to nine markers were inserted into the acetabular region of the pelvis to optimize marker spread and compensate for loose or invisible markers.
To ensure alignment of the laboratory coordinate axes to the pelvis, the orientation of the patient in relation to the cage was standardized in the reference position (supine position), so that the transverse axis should pass throw the two anterior iliac spines. When examined standing the patient had the arms crossed on the chest at a standard position.
To evaluate the reproducibility of the RSA measurements, two sets of RSA images (double examinations) of 20 patients in the supine position at the same visit were performed. The patients were repositioned between the examinations, without moving the calibration cage and X-ray tubes. All patients were examined using a uniplanar technique.21 Stereoradiographic measurements and analysis were performed with UmRSA Digital measure and UmRSA Analysis software 6.0 (RSA Biomedical, Umeå, Sweden).
2.3 Statistical analysis
Statistical analysis was performed using IBM SPSS, version 20.0.0. All RSA data were normally or close to normally distributed (Shapiro-Wilk; P < .05). The data are presented as the mean ± standard deviation (SD) at a confidence interval (CI) level at 95%. Paired-samples t tests were used to evaluate any differences between two repeated observations from the same patients and an independent sample t test or one-way analysis of variance was used for comparison between different groups. Statistical significance was assumed at P values less than .05.
Generalized linear models were constructed in which pelvic tilt in supine position and from the supine to the standing position at 6 months and 7 years were used as dependent variables, with gender, the status of the contralateral side (only at the 7-year follow-up) and low-back pain (only at 7-year follow-up) as predictors. Age was used as a covariate.
The precision of pelvic position was calculated as 95% CI using the SD of the difference measured between two examinations multiplied by the critical value (t) obtained from the T-table. The precision was calculated from zero by assuming that the pelvic tilt between the two examinations had no specific direction. Precision of the double examination measurements was found to be ±3.3° for rotations about the transverse axis, ±1.3° for the longitudinal and ±4.5° for the sagittal axis (± describes the 95% CI of individual patients).
3 RESULTS
3.1 Changes in PTA in supine position
The pelvis tended to show an increased posterior tilt with increasing follow-up. Between the postoperative and the follow-up examination at 6 months the posterior tilt reached a mean of −2.0° ± 3.0° (CI: −2.6° to −1.4°), which increased to −2.7° ±2.9° (CI: −3.3° to −2.2°) at 7 years (P = .01) (Table 2A). The mean changes around the longitudinal and sagittal axes were less than 1 degree, in both supine and standing positions (Tables 2A and 2B).
3.2 Changes in PTA between supine and standing position
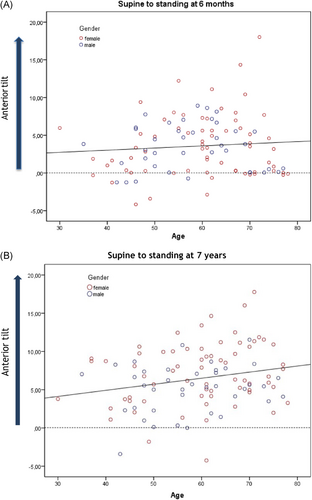
From supine to standing, the mean change was 3.6° ± 3.8° (CI: 2.8° to 4.3°) at 6 months which increased to 6.4° ± 3.9° (CI: 5.7° to 7.2°) at 7 years (P < .001) (Table 2A). At 6 months, five patients demonstrated anterior tilt changes above 10 degrees reaching a maximum of 18 degrees (Figure 2A). Nineteen patients demonstrated an anterior tilt above 10 degrees at the 7-year follow-up (Figure 2B).
3.3 Influence of different factors on PTA
3.3.1 Gender
At 6 months, the mean change in posterior pelvic tilt was greater (P = .02) in females (−2.5° ± 3.0°) than in males (−1.1° ± 2.6°) in the supine position. At 7 years this posterior tilt had increased in both females and males to −3.1° ± 3.0° and −2.1° ± 2.8°, respectively (females vs males: P = .08). Between supine and standing, there was no difference between the genders at 6 months. Compared to the male participants, females showed a significant larger anterior tilt from supine to standing at 7 years (7.2° ± 4.1° vs 5.1° ± 3.2°; P = .01) (Table 3).
| Female | Male | |||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | 95% CI | Mean (SD) | 95% CI | P valuea | |
| Supine | ||||||
| Postoperative—6 mo | 67/39 | −2.5° (3.0°) | −3.2° to −1.7° | −1.1° (2.6°) | −2.0° to −0.29° | .02 |
| Postoperative—7 y | 67/39 | −3.1° (3.0°) | −3.8° to 2.4° | −2.1° (2.8°) | −3.0° to −1.2° | .08 |
| Supine to standing | ||||||
| 6 mo | 67/39 | 3.6° (4.2°) | 2.6° to 4.6° | 3.5° (3.0°) | 2.5° to 4.5° | .84 |
| 7 y | 67/39 | 7.2° (4.1°) | 6.2° to 8.2° | 5.1° (3.2°) | 4.1° to 6.2° | .01 |
- Abbreviations: CI, confidence interval; SD, standard deviation; THA, total hip arthroplasty.
- a The Student t test.
3.3.2 Low-back pain
In the supine position, no significant differences in PTA were observed between the patients with or without low-back pain at any of the two follow-up occasions (P > .05). From supine to standing, a weak and insignificant tendency toward larger anterior tilt was observed in patients with no low-back pain on both occasions.
3.3.3 Linear regression analysis
For females measured in the supine position at 6 months, regression analysis of rotations about the transverse axis (dependent value) showed an increased posterior tilt (P = .01) and a tendency toward increasing posterior tilt with age (P = .06) (Table 4A). From the supine position postoperatively to supine at 7 years, a moderate association between female gender and posterior pelvic tilt was observed (P = .06), but no association with age (P = .56) or back pain (P = .35) (Table 4A).
| Supine-supine | ||||||
|---|---|---|---|---|---|---|
| Postoperative—6 mo | Postoperative—7 y | |||||
| β | 95% CI | P value | β | 95% CI | P value | |
| Gender | ||||||
| Female | −1.4 | −2.60 to −0.32 | 0.01 | −1.10 | −2.20 to 0.06 | .06 |
| Malea | 0a | |||||
| Age | .05 | −0.00 to 0.10 | 0.06 | 0.02 | −0.04 to 0.06 | .56 |
| Low-back pain | ||||||
| Yes | -0.58 | 0.63 to −1.80 | .35 | |||
| Noa | 0a | ⋯ | ⋯ | |||
- Abbreviation: CI, confidence interval.
- a Reference
At 6 months, changes in pelvic tilt from supine to standing positions were not significantly correlated with gender (0.90) or age (0.40). Significant increases in anterior pelvic tilt from supine to standing positions at 7 years (Table 4B) were associated with female gender (P = .004) and patient age (P = .02).
| Supine to standing | ||||||
|---|---|---|---|---|---|---|
| 6 mo | 7 y | |||||
| β | 95% CI | P value | β | 95% CI | P value | |
| Gender | ||||||
| Female | .09 | −1.40 to 1.60 | .90 | 2.10 | 0.69 to 3.60 | .004 |
| Malea | ||||||
| Age | .03 | −0.04 to 0.09 | .40 | .07 | 0.01 to 0.13 | .02 |
| Opposite hip | ||||||
| Normala | −0.01 | −2.10 to 2.10 | .99 | |||
| OA | 1.30 | −0.36 to 2.90 | .13 | |||
| THA | ||||||
| Low-back pain | ||||||
| Yes | −1.50 | −3.10 to 0.05 | .06 | |||
| Noa | ||||||
- Abbreviations: CI, confidence interval; OA, osteoarthritis; THA, total hip arthroplasty.
- a Reference
Any influence of the status of the opposite hip was only studied for supine to standing at 7 years, because the exact time frame for the development of OA on the nonoperated side could not be established. Analysis of supine to standing results at 7 years did not reveal any influence of the opposite side (normal, OA, or THA) on the recorded PTA (Table 4B).
4 DISCUSSION
A steep acetabular cup inclination increases the risk of dislocation and is also considered as an important reason for increased wear regardless of the material used.23-25 Routinely, the inclination of the cup is determined postoperatively on radiographs exposed in the supine position. The patient will, however, perform numerous activities when upright and, between supine and standing, the rotation of the pelvis about the transverse axis might change. Any change in pelvic orientation after the operation in the supine position and between the supine and standing position during the postoperative period will influence validity of cup orientation measurements.
A limitation of our study is that we were unable to evaluate pelvic orientation prior to THA, because the RSA technique requires maker beads to be inserted into the bone. However, several studies have found no significant difference between preoperative and postoperative PTA.23, 26, 28 Another possible limitation is that double examinations in the standing position were not performed. We had no ethical approval to repeat both the supine and standing examinations and since we hypothesized that the supine examination would have the largest variability, we chose to perform double examinations in this position.
We found that, when the patient is measured in the supine position, the PTA changes over a period of 7 years. This change in terms of increasing posterior tilting was comparatively small and more pronounced in females than in males. After operation, extension defect caused by the hip disease can be expected to decrease and even disappear. Our observation of increasing posterior tilt over time could reflect that the soft-tissue distraction continues up to at least 6 months after the operation and even during longer in some patients. In changing from a supine to standing position, the pelvis tilted in the opposite (ie, anterior) direction. This anterior tilt increased with time and became significant at 7-year follow-up especially in women. The increased pelvic tilt in woman may be associated with age-related changes of the spine due to osteoporosis, which increases with age and especially in females.29-32 Female gender and increasing age have previously been found to be consistent with larger variations of PTA,33 which is consistent with our findings. Those authors evaluated changes in PTA in 86 patients in the supine and standing positions 2 to 4 years after operation and reported a significant difference in PTA between those positions. In addition, they found that the amount of pelvic tilt prior to surgery was a contributory factor. Ishida et al27 reported that patients with large preoperative anterior tilt demonstrated greater changes of this parameter after operation. However, there seems to be some disagreement in the literature regarding the impact of preoperative pelvic tilt on the extent of postoperative tilting of the pelvis in the standing position.26, 28, 34 We found that the status of the contralateral hip had no effect on the PTA. One could speculate that untreated OA on the opposite side in these patients would result in more anterior pelvic tilt than in those with a normal hip on the opposite side, due to soft-tissue contracture.
Similar to our observations, Tamura et al35 observed a posterior pelvic tilt supine at the 1-year follow-up, which tended to level out at the following examinations. Contrary to our observations, however, these authors observed a posterior tilt in an increasing number of patients with time and especially between the 5- and 10-year follow-up. The reason for this difference is not known but could be perhaps be related to differences in demography and especially different diagnoses of hip diseases. We think that the precision of our measurements mainly was related to the ability of the patient and the examiner to obtain a standardized alignment at the reference position, to randomly occurring changes of the pelvic tilt supine and standing and, to a relatively much smaller degree, the resolution of RSA itself. Previous studies seem to have focused their error analysis on the measurement methodology and not to individual variations in pelvic positioning. Several studies (Nishihara et al,36 Pierrepont et al,37 Tamura et al,35 Uemara et al38) matched three-dimensional measurements or reconstructions from computed tomography images to conventional radiographic images. They found a high correlation between these measurements and in one of these studies, a median absolute error of 1.5 degrees was reported,38 but none of these calculations seem to be based on repetition of the examination procedure. In our study, we only repeated examination supine to study precision. Further studies with repeated examinations of the standing position in one and the same patient could also be of interest, but at the time period for this study, we had no ethical allowance for expansion of the double examinations.
In the previous studies quoted above, the pelvic positions were determined based on anatomical landmarks and the change of pelvic tilt between these positions were computed. We measured change of pelvic tilt corresponding to rotations about the transverse axis of the RSA calibration cage by determination of position changes of clusters of markers inside the pelvic bone. We were therefore unable to account for any differences between the groups at the starting or reference supine position which is a limitation.
Patients with low-back problems might be expected to have reduced mobility of the spine and the pelvis. The evaluation of low-back pain in our study was retrospective and could, therefore, be regarded as suboptimal. However, the differences between patients with or without low-back pain were small and amounted to only one to two degrees on average. These findings were consistent with a meta-analysis comparing pelvic kinematics in patients with and without low-back pain, which reported no difference between these patient groups.39-42 According to our findings and in patients without spinal fusion, the influence of low-back problems on the stability of a hip prosthesis seems to be small.
5 CONCLUSION
Up to 7 years after insertion of a THA, the pelvis tilts slightly posteriorly in the supine position. When rising to standing, we found that the pelvis tilts in the opposite direction. This tilt increased with time and reached an average of about 7 degrees in females and 5 degrees in males. For many patients, the individual changes are small and most probably have minor effects on the outcome of the procedure. In individual cases, this tilt might be high as much as 15 to 20 degrees. Female patients displayed larger changes in pelvic tilt in both supine and standing positions. A large PTA after THA may cause dislocation or influence the rate of wear of the articular surface. If possible, identification of these patients before the operation could be beneficial to obtain guidelines for optimum cup positioning or choice of implants with built-in increased resistance to dislocation.43 Increased knowledge of postoperative changes of pelvic tilt may contribute to the understanding of adverse outcomes after THA and how to reduce the risk of their occurrence.
ACKNOWLEDGMENTS
The project was supported by the Felix Neubergh Foundation, IngaBritt and Arne Lundbergs Research Foundation, Hjalmar Svenssons Foundation, Zimmer-Biomet, Warsaw, United States.
CONFLICT OF INTERESTS
One of the authors of this paper is a board member of RSA Biomedical and has a financial relationship with the organization that could influence or bias the content of the paper.
AUTHOR CONTRIBUTION
JKÄ was responsible for the study conception and design. BSH collected the data and performed the analysis and drafted the manuscript. JKÄ and MM critically reviewed and contributed to the paper. All authors read and approved the final manuscript.