Sex based disparities in hospitalization and readmission outcomes for complete atrioventricular block: Insights from United States readmission data
Abstract
Background
Sex disparities in cardiovascular disorders are well-documented, but data on hospitalization and readmission outcomes in the context of sex for Complete Heart Block (CHB) remains limited.
Methods
We analyzed the 2016–2020 Nationwide Readmission Database to identify patients with a principal diagnosis of CHB. Men served as the control group, while women comprised the study cohort. The primary outcome was mortality. Secondary outcomes included odds of cardiac arrest, ventricular tachycardia, heart failure, mechanical ventilation use, all-cause 30-day readmission, total and early pacemaker use, length of stay (LOS), and total hospitalization charges (THC). Multivariate regression models adjusted for confounders.
Results
Among 175,257 patients with CHB, 45% were female. Female sex was associated with higher odds of mortality (adjusted OR [aOR] 1.42, 95% CI 1.3–1.55) compared to males. Additionally, females had higher odds of cardiac arrest (aOR 1.13, 95% CI 1.06–1.2), ventricular tachycardia (aOR 1.1, 95% CI 1.05–1.17), heart failure (aOR 1.18, 95% CI 1.14–1.22), mechanical ventilation use (aOR 1.1, 95% CI 1.03–1.17), and all-cause 30-day readmission (aOR 1.1, 95% CI 1.03–1.14). Women also had lower odds of total pacemaker use (aOR 0.92, 95% CI 0.88–0.96) and early pacemaker use (aOR 0.89, 95% CI 0.86–0.82). Female patients exhibited longer LOS (4.13 days vs. 3.86 days, p < 0.001) but incurred lower THC ($89,908 vs. $94,590, p = 0.002).
Conclusion
Female sex in CHB patients was associated with higher mortality and adverse events but lower pacemaker use compared to male patients.
1 INTRODUCTION
A growing body of research underscores the presence of significant sex disparities in outcomes following cardiovascular-related hospitalizations. Numerous studies have consistently shown that female patients are at a higher risk of short-term morbidity and mortality during various cardiovascular emergencies compared to their male counterparts.1 Among these conditions, one of the most critical is complete heart block (CHB)—a life-threatening cardiac emergency that carries high risks of morbidity and mortality.2 Given the severity of CHB, prompt diagnosis and intervention are essential to optimizing patient outcomes.
Despite the extensive documentation of sex differences in cardiovascular care, research specifically addressing how sex impacts clinical outcomes in CHB remains limited. This scarcity of data represents a critical gap in understanding whether female patients with CHB experience unique risks compared to males. Given that sex-based disparities have been observed in other cardiovascular conditions, it is reasonable to hypothesize that female sex may also predispose patients with CHB to worse hospitalization outcomes, such as increased mortality and morbidity. If confirmed, this finding highlights the need for heightened attention to sex-specific factors in the clinical management of CHB from the point of hospital admission.
This study aims to evaluate whether female sex is independently associated with adverse outcomes in patients hospitalized for CHB. Through a comprehensive analysis of national data and a review of the existing literature, we seek to uncover the mechanisms that may be driving these disparities and to propose areas where clinical interventions can be tailored to mitigate these risks.
2 MATERIALS AND METHODS
2.1 Data source and ethics statement
The Nationwide Readmissions Database (NRD) is part of the Healthcare Cost and Utilization Project (HCUP), which is overseen by the Agency for Healthcare Research and Quality (AHRQ). It is one of the most comprehensive inpatient data sources in the United States.3, 4 The NRD is constructed using billing data submitted by hospitals to HCUP. HCUP applies appropriate weighting variables to ensure that the data accurately reflects national trends in healthcare utilization. Given that NRD data is de-identified and publicly accessible, this research did not require prior approval from the any Institutional Review Board.
2.2 Study population and outcomes
The NRD was queried for the period between January 1, 2016, and December 31, 2020, to identify adult patients (aged ≥18 years) with a primary diagnosis of CHB, based on the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code I442. To ensure the accuracy of CHB diagnoses, only patients with a principal diagnosis of CHB where included. The patient cohort was divided into two groups by sex: male patients served as the control group, while female patients formed the cohort group under investigation.
We systematically collected baseline demographic data and comorbidities using ICD-10-CM codes, which included a comprehensive range of cardiovascular and non-cardiovascular conditions. Specifically, we assessed comorbidities such as prior stroke, prior acute myocardial infarction (AMI), body mass index (BMI), atrial fibrillation, hypertension, dyslipidaemia, pulmonary hypertension, chronic obstructive pulmonary disease (COPD), prior percutaneous coronary intervention (PCI), prior coronary artery bypass grafting (CABG), as well as lifestyle risk factors like tobacco and alcohol use. A full list of ICD-10-CM codes used for diagnoses and procedures is available in Table S1. The primary outcome of this study was inpatient mortality. Secondary outcomes included odds of mechanical ventilation use, cardiac arrest, ventricular tachycardia, heart failure, total pacemaker use, early pacemaker use, all-cause 30-day readmissions, hospital length of stay (LOS), and total charges. Early pacemaker use was defined as pacemaker intervention within the 1st day of hospitalization.
2.3 Statistical analysis
To account for the complex survey design of the NRD, we incorporated weighting variables, strata, and clustering into our statistical analysis. This approach ensures that our findings are nationally representative and that the calculation of standard errors and p-values is accurate. Specifically, we applied hospital discharge weights provided by the NRD to generate national-level estimates, which correct for unequal probabilities of selection and account for survey design complexities.
To enhance the robustness of our analysis, we included all primary sampling units (hospitals), thereby minimizing the risk of underestimating standard errors and ensuring the proper calculation of p-values. All analyses were conducted using Stata 18.0 (College Station, TX), a statistical software specifically designed to handle complex survey data. Within Stata, appropriate survey procedures were applied to integrate the weights, strata, and clusters, ensuring that our estimates were both precise and unbiased.
Descriptive statistics were generated to summarize patient characteristics based on sex. To explore associations between patient characteristics and clinical outcomes, logistic regression models were utilized allowing for adjustment of the NRD's complex sampling design. Initially, unadjusted odds ratios (uORs) for both primary and secondary outcomes were calculated using univariate logistic and linear regression analyses. Multivariable logistic and linear regression analyses were subsequently conducted to control for potential confounders, including age, median household income by ZIP code, sepsis, in-hospital PCI and CABG usage, and comorbidities, measured by the 1993 Deyo adaptation of the Charlson Comorbidity Index (CCI), which is suitable for use with NRD data5.
For continuous variables, comparisons were made using Student's t-tests, while categorical variables were compared using the Rao-Scott chi-square test, which adjusts for the survey design. Given the non-normal distribution of LOS, we utilized a weighted generalized linear model with a gamma distribution and log link function. For all analyses, a p-value <0.05 was considered statistically significant.
3 RESULTS
3.1 Patient characteristics
Among patients with a primary diagnosis of CHB (N = 175,257), 45% (N = 78,865) were women. Female patients where older (mean age 77 years vs. 75 years), more likely to have Medicare as a primary payer (85% vs. 80%, p <.001), and a lower mean comorbidity index (2.12 vs. 2.35). On the other hand, female patients were less likely to have a prior MI (6.5% vs. 11%, p <.001), dyslipidemia (51% vs. 56%, p <.001), Atrial Fibrillation (18% vs. 20%, p <.001), COPD (13% vs. 15%, p <.001), prior PCI (7% vs. 13%, p <.001), prior CABG (5% vs. 14%, p <.001), tobacco use (26% vs. 43% p <.001) and alcohol use (0.8% vs. 3%, p <.001) compared to male patients. Additionally female patients were more likely to have hypertension (45% vs. 42%, p <.001), prior stroke (9.6% vs. 9%, p =.011), pulmonary hypertension (3.3% vs. 2.1%, p <.001) and sever obesity (BMI ≥40 42% vs. 31%, p <.001) compared to male patients. Baseline characteristics of patients stratified by sex are shown in Table 1.
| Female group (n = 78,865) | Male group (n = 96,392) | p value | |
|---|---|---|---|
| Age category, % | p <.001 | ||
| 18–34 | 0 | 0 | |
| 35–65 | 13 | 17 | |
| >65 | 87 | 83 | |
| CCI score, % | p <.001 | ||
| 0 | 23 | 21 | |
| 1 | 23 | 22 | |
| 2 | 19 | 18 | |
|
≥3 |
35 | 39 | |
| Median household income, % | p <.001 | ||
| $1–$49,000 | 26 | 24 | |
| $50,000–$64,999 | 28 | 28 | |
| $65,000–$85,999 | 26 | 26 | |
| ≥$86,000 | 20 | 22 | |
| Insurance, % | p <.001 | ||
| Medicare | 85 | 80 | |
| Medicaid | 3 | 4 | |
| Private | 11 | 15 | |
| BMI, % | p <.001 | ||
| BMI 25–29, % | 9 | 11 | |
| BMI 30–39, % | 49 | 59 | |
| BMI ≥40, % | 42 | 30 | |
| Hypertension, % | 46 | 42 | p <.001 |
| Dyslipidemia, % | 52 | 56 | p <.001 |
| Prior PCI, % | 7 | 13 | p <.001 |
| Atrial Fibrillation, % | 18 | 20 | p <.001 |
| Prior CABG, % | 5 | 14 | p <.001 |
| Alcohol use, % | 0.8 | 3 | p <.001 |
| COPD, % | 13 | 15 | p =.013 |
| Pulmonary Hypertension, % | 3.3 | 2.1 | p <.001 |
3.2 Primary and secondary outcomes
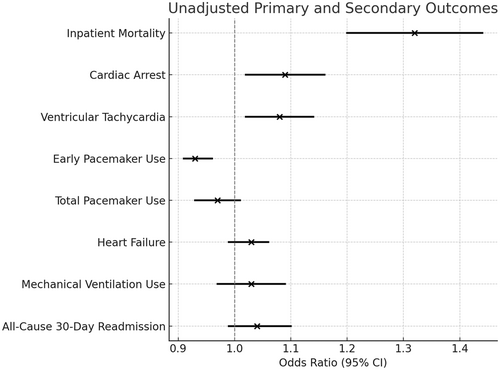
In the unadjusted analysis, among patients with CHB, female sex was associated with a 32% increase in inpatient mortality (unadjusted OR [uOR] 1.32, 95% CI 1.2–1.44, p < 0.001) during index hospitalization. Additionally, female sex was associated with higher odds of cardiac arrest (uOR 1.09, 95% CI 1.02–1.16, p =.008), ventricular tachycardia (uOR 1.08, 95% CI 1.02–1.14, p =.006), and lower odds of early pacemaker use (50% vs. 52%, uOR 0.93, 95% CI 0.91–0.96, p <.001). No differences were observed between female and male patients regarding total pacemaker use (82.7% vs. 83.2%, uOR 0.97, 95% CI 0.93–1.01, p =.123), heart failure (uOR 1.03, 95% CI 0.99–1.06, p =.08), mechanical ventilation use (uOR 1.03, 95% CI 0.97–1.09, p =.279), and all-cause 30-day readmission (uOR 1.04, 95% CI 0.99–1.1, p =.126). Unadjusted outcomes are shown in Figure 1.
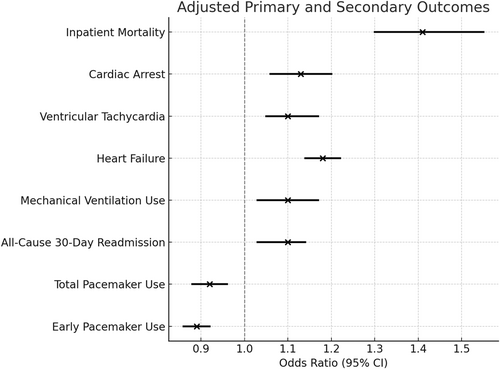
After adjustment for baseline characteristics, female sex remained associated with higher odds of inpatient mortality (adjusted OR [aOR] 1.41, 95% CI 1.3–1.55, p <.001) compared to male sex in cases of CHB. Additionally, after adjustment for confounders, female sex was associated with higher odds of cardiac arrest (aOR 1.13, 95% CI 1.06–1.2, p <.001), ventricular tachycardia (aOR 1.1, 95% CI 1.05–1.17, p <.001), heart failure (aOR 1.18, 95% CI 1.14–1.22, p <.001), mechanical ventilation use (aOR 1.1, 95% CI 1.03–1.17, p = 0.004), and all-cause 30-day readmission (aOR 1.1, 95% CI 1.03–1.14, p =.004). Female sex was also associated with lower odds of total pacemaker use (aOR 0.92, 95% CI 0.88–0.96, p <.001) and early pacemaker use (aOR 0.89, 95% CI 0.86–0.92, p <.001) compared to male patients hospitalized with CHB during the index hospitalization. Adjusted outcomes are shown in Figure 2.
3.3 LOS and THC
Among patients with CHB, the mean LOS was 4.13 days for female patients and 3.86 days for male patients and this prolonged LOS in female patients compared to male patients remained statistically significant while adjusting for confounders (adjusted increase 0.4 days, 95% CI 0.3–0.44 days, p <.001). Contrariwise, among patients with CHB the mean THC were lower in female patients compared to male patients ($89,908 vs. $94,590). Sed lower THC in female patients compared to male patients remained significant after adjusting for confounders (adjusted decrease $1832, 95% CI (−) $2929– (−) $735, p =.001).
4 DISCUSSION
To our knowledge, this is the first study to examine sex disparities among United States. patients hospitalized with CHB. Our findings reveal that female patients with CHB have distinct clinical profiles compared to their male counterparts. Women face higher risks of adverse outcomes, including increased mortality, cardiac arrest, ventricular tachycardia, heart failure, 30-day readmissions, and a greater need for mechanical ventilation. Despite experiencing longer hospital stays, female patients incur lower total charges and are less likely to early pacemaker intervention compared to male patients.
4.1 Demographic and clinical risk
Among patients with a primary diagnosis of CHB, 45% were female. Female patients admitted for CHB were found to have fewer comorbidities compared to their male counterparts, a finding consistent with prior studies.6 Specifically, females were less likely to present with traditional cardiovascular comorbidities, such as a history of AMI, dyslipidemia, prior PCI or CABG, as well as modifiable behavioral risk factors like tobacco and alcohol use. Similar demographic differences between sexes have been observed in other cardiovascular diseases, such as AMI and heart failure, where men generally exhibit a higher incidence of classic heart disease risk factors than women.7, 8
In contrast, female patients admitted for CHB were more likely to have a history of hypertension, prior stroke, pulmonary hypertension and sever obesity. These observations are consistent with findings in current literature, which reveal notable sex disparities in the prevalence, awareness, treatment, and management of hypertension. Typically, men exhibit higher rates of hypertension in younger age groups, while older women tend to demonstrate a greater overall prevalence,9 a trend that aligns with our demographic data. Similarly, research highlights sex differences in stroke prevalence, indicating that older women experience a higher incidence compared to their male counterparts.10 Furthermore, pulmonary hypertension is more frequently diagnosed in women than in men,11 and this condition has been proposed to be independently linked to worse functional outcomes and increased mortality rates in patients suffering from high-grade conduction disease.12 Female patients also exhibited higher rates of sever obesity compared to men. Obesity is an additional characteristic that would predispose patients to a higher cardiovascular disease related morbidity and mortality.13 Furthermore, several studies have reported that obesity is linked to a higher prevalence of conduction disease as well as increased severity of conduction abnormalities through mechanisms related to structural and functional changes to the heart.14-16 Given these findings, further research to thoroughly explore the demographic and clinical risk profile differences between male and female patients with CHB is crucial, as understanding these disparities could inform tailored interventions and improve patient outcomes.
4.2 In-hospital outcomes
This study reveals significant sex-based disparities in outcomes and management CHB patients. Female patients face increased odds of adverse outcomes, including higher inpatient mortality, cardiac arrest, ventricular tachycardia, heart failure, mechanical ventilation use, and 30-day readmissions. A female sex was also associated with a lower likelyhood for total and early pacemaker implantations compared to men, aligning with broader evidence of systemic sex biases in cardiovascular disease treatment.
The reduced pacemaker utilization in female patients is particularly concerning given the device's established necessity in CHB management. Pacemakers are crucial for addressing conduction abnormalities, stabilizing bradycardia, and preventing complications like syncope and sudden cardiac arrest.17 Concurrent literature demonstrates that female patients consistently face intervention delays across cardiovascular care, including lower rates of percutaneous coronary interventions and left ventricular assist device implantation during AMI or cardiogenic shock hospitalizations.18 In CHB cases, delayed pacemaker implementation may increase women's vulnerability to life-threatening arrhythmias, particularly ventricular tachycardias, which occur more frequently in women due to sex-based QT interval differences.19
These disparities extend to other electrophysiologic conditions. For instance, prior studies demonstrated that in older patients (≥80 years) men received more dual-chamber devices than women for AV block and sick sinus syndrome.20 Women with atrial fibrillation report more severe symptoms and reduced quality of life but receive fewer referrals for advanced interventions like catheter ablation.21-23 Female CHB patients present distinct demographic and clinical risk characteristics. While they show lower prevalence of traditional cardiovascular risk factors, they exhibit higher rates of pulmonary hypertension and severe obesity. Pulmonary hypertension can obscure CHB presentation and increase right ventricular failure risk, while obesity complicates procedural access and increases pacemaker implantation risks.
Age-related disparities compound these issues, as older female patients receive fewer diagnostic tests and therapeutic interventions compared to younger females or males.24 This age-sex interaction often leads to treatment delays, which are strongly associated with adverse outcomes.25-28 The combination of delayed diagnosis, underutilized pacemaker implementation, and increased cardiac arrest and heart failure could contribute to higher mortality and readmission rates among female patients.
Addressing these inequities requires a multifaceted approach, including increased healthcare provider awareness, standardized guideline adherence, and targeted strategies to improve treatment access for female patients. Further research must investigate the underlying mechanisms of these disparities, including clinical decision-making biases, symptom presentation differences, and systemic barriers to care, to develop effective interventions for improving women's CHB outcomes.
4.3 Hospital LOS and THC
Among hospitalizations for CHB, female sex was linked to a longer average LOS and lower THC compared to male sex. This trend may be attributed to the increased likelihood of in-hospital adverse outcomes that female patients experience, which often necessitates a higher level of intensive care. Conversely, the association between female sex and lower THC is less straightforward. For instance, some studies have argued the presence of sex disparities in resource utilization and quality of care for postmenopausal women, particularly in cardiovascular disease management.23 Therefore, additional research is essential to further investigate the influence of sex on LOS and THC in CHB cases and other related conduction disorders. Understanding these dynamics could help inform more equitable healthcare practices and resource allocation for both male and female patients.
4.4 Limitations and strengths
The findings of this study should be interpreted with caution due to several inherent limitations associated with research utilizing the NRD. Firstly, there may be potential inaccuracies or incomplete information in the ICD-10 codes employed for patient classification. Secondly, details about CHB such as its etiology, patient baseline EKG characteristics and chronicity, were not factored into the analysis used in this study. Furthermore, specific details regarding regarding access to subspecialty services such as cardiovascular electrophysiology were not available. Additionally, NRD does not differentiate between secondary diagnoses that are present at admission and those identified during hospitalization, which restricts our ability to draw conclusions about the timing and duration of these secondary diagnoses.3 Furthermore, the NRD does not capture data regarding race, as such race was not adjusted for during our analysis. Despite these limitations, it is noteworthy that the AHRQ routinely conducts data quality assessments on the NRD, which helps to enhance the integrity of the data and minimize the risk of errors. Moreover, when appropriately weighted, the NRD sample reflects a broad cross-section of the US population, allowing for a more comprehensive understanding of inpatient outcomes.
5 CONCLUSIONS
This analysis reveals significant sex-based disparities in CHB treatment and outcomes. Female patients experienced delayed and reduced pacemaker utilization alongside higher rates of fatal and non-fatal complications. Despite longer hospital stays, a female sex was associated with lower THC when compared to male sex, suggesting the presence of sex based disparities in pacing interventions for CHB. These findings parallel documented sex disparities across cardiovascular care, likely stemming from delays in guideline-directed treatment, under-studied sex based clinical risk differences, and inconsistent application of diagnostic and therapeutic interventions.
Healthcare providers must recognize female patients as a high-risk group for adverse outcomes in high-grade conduction disease. This understanding should drive focused research into the root causes of these inequities and inform targeted interventions. By addressing these systemic disparities, the medical community can work toward reducing cardiovascular disease burden and establishing more equitable, sex-specific approaches to patient care that improve outcomes for all populations.
FUNDING INFORMATION
The authors have nothing to report.
CONFLICT OF INTEREST STATEMENT
The authors have nothing to report.
ETHICS STATEMENT
Given that the data used in this study was derived from the Nationwide Readmissions Database, which is de-identified and publicly accessible, this study did not require approval from any Institutional Review Board. Additionally, written informed consent from participants was not required in accordance with local and national guidelines.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are not publicly available due to their containing information that could compromise the privacy of research participants. However, the data are available from the Healthcare Cost and Utilization Project (HCUP) Central Distributor upon reasonable request at https://www.hcup-us.ahrq.gov/tech_assist/centdist.jsp. The underlying data used in this manuscript come from the Nationwide Readmissions Database (NRD), which is maintained by the Agency for Healthcare Research and Quality (AHRQ). Researchers can request access to the NRD through the HCUP Central Distributor by contacting them via email at [email protected].




