Loss of left ventricular component of biventricular pacing with low atrial rhythm, what is the mechanism?
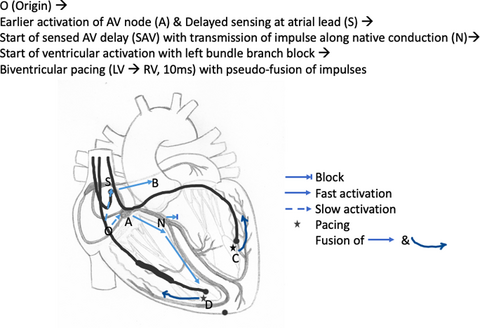
Graphical Abstract
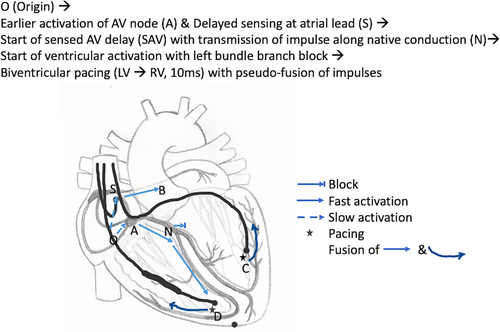
Effective biventricular pacing is important to improve survival in patients with heart failure. We report a case of a patient with heart failure, who underwent cardiac resynchronization therapy, who had loss of biventricular pacing when in low atrial rhythm. We discuss the probable mechanism for the same.
Abbreviations
-
- AV
-
- Atrioventricular
-
- CRT - D
-
- Cardiac Resynchronization Therapy with Defibrillation
-
- ECG
-
- Electrocardiogram
-
- LBBB
-
- Left Bundle Branch Block
-
- LV
-
- Left Ventricular
-
- LVEF
-
- Left Ventricular Ejection Fraction
-
- PAV
-
- Paced Atrioventricular Delay
-
- RV
-
- Right Ventricle
-
- SAV
-
- Sensed Atrioventricular Delay
1 INTRODUCTION
Effective biventricular pacing is important to improve survival in patients with heart failure 1. We report a case of a patient with heart failure, who underwent cardiac resynchronization therapy, who had a loss of left ventricular (LV) component of biventricular pacing when in low atrial rhythm. We discuss the probable mechanism for the same.
2 CASE DESCRIPTION
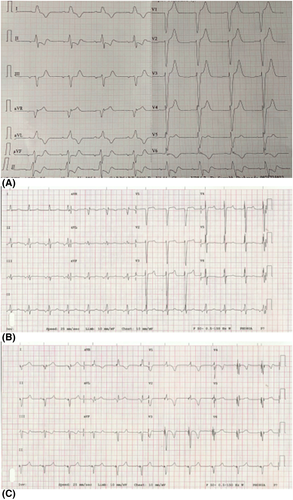
A 66-year-old male, hypertensive with old ischemic heart disease and severe left ventricular systolic dysfunction (LVEF 33%) with left bundle branch block on the ECG (QRS duration 160ms), underwent cardiac resynchronization therapy with defibrillator (CRT-D—Rivacor 7 HF-T QP from Biotronik, Berlin, Germany) for symptomatic heart failure. The device was programmed with a sensed atrio-ventricular (AV) delay of 80 ms and a Paced AV delay of 100 ms and Auto-ADAPT being OFF. The LV-RV offset with -20 ms with LV programmed to be paced 20 ms before right ventricle (RV). It was noticed that there was a loss of the left ventricular component of the biventricular pacing (loss of R wave in lead V1) on the ECG done on day 1 post-procedure (Figure 1). A repeat ECG done later, without any changes in the device programming, showed normal sinus rhythm with left ventricular pacing occurring during biventricular pacing (presence of R in lead V1). The first ECG (Figure 1) shows inverted p waves in the inferior leads II, III, aVF. This indicates the origin of the beat may be originating in the low right atrium. So, it can be assumed that low atrial rhythm has caused the loss of the R wave / the left ventricular component of biventricular pacing which is important to occur to correct dyssynchrony. This finding was corroborated by intracardiac electrograms (Figure 2).
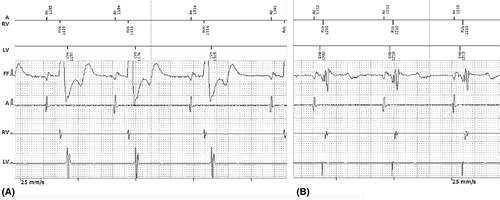
- The beat originating in the low atrium has to travel to the right atrial appendage to get sensed. That causes a delay in the sensing in the atrial lead and subsequent delay in the activation of the atrioventricular timing cycle. Due to its spatial closeness to the atrioventricular (AV) junction, native electrical impulse reaches early at the AV node and excites the native conduction system before the paced beats are delivered to the ventricles. It is evident by the lower PR interval in low atrial rhythm (120 ms, as against 140 ms in normal sinus rhythm). This results in a left bundle branch block (LBBB) pattern on the ECG (native AV conduction) and pseudo-fusion due to delayed delivery of ventricular impulse by CRT. This leads to loss of left ventricular pre-excitation and loss of effective biventricular synchrony (Figure 3).
- Native sinus beats result is near-simultaneous activation of the right and left atria. The low atrial beat takes time to reach the interatrial connections 2. So, there is a delay in the activation of the left atrium with low atrial rhythm. This may lead to mechanical dyssynchrony between the left atrium and ventricle.
Since the low atrial rhythm was a transient phenomenon, it did not cause any hemodynamic problems in the patient. Effective biventricular pacing with LV capture is important to improve the ejection fraction in the long run in patients with heart failure 3. So, it is important to ensure effective and optimum biventricular pacing during the follow up of patients who have undergone cardiac resynchronization therapy
3 LEARNING POINTS
In the case of biventricular pacing, it is important to maintain atrioventricular synchrony to get the desired clinical benefit. In our case, the development of low atrial rhythm led to a loss of the LV component of the biventricular pacing.
4 CONSENT
Informed consent has been obtained from the patient and all the identifiers have been removed from the images as per the guidelines.
CONFLICT OF INTEREST
The authors declare no Conflict of Interest for this article.