Clinical considerations for a gastric Dieulafoy's disease patient: Cardiac arrhythmias caused by SARS-CoV-2 or terlipressin?
1 INTRODUCTION
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has caused the COVID-19 pandemic, is proved to involve multiple organs and systems, primarily targeting the cardiac and respiratory system. Cardiac arrhythmia, which induces by myocardial damage and subsequent cardiac dysfunction, is a major clinical manifestation in cardiac injury.1 Previous data revealed that 9%–16.7% of hospitalized patients with COVID-19 suffering an unspecified arrhythmic event2, 3 and contributed to 44% of those transferred to the ICU.3 The 17.6% of primary QTc prolongation and 0.38% of secondary torsade de pointes in COVID-19 patients were disclosed by a detailed investigation.4 In addition, other drug interventions that appear to be independent of anti-SARS-CoV-2 treatment, such as terlipressin,5 oxaliplatin, and so forth, are increasingly at risk of arrhythmias in the COVID-19 patients with gastrointestinal (GI) bleeding.
2 CASE PRESENTATION
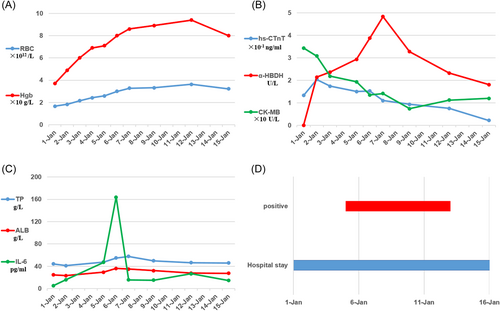
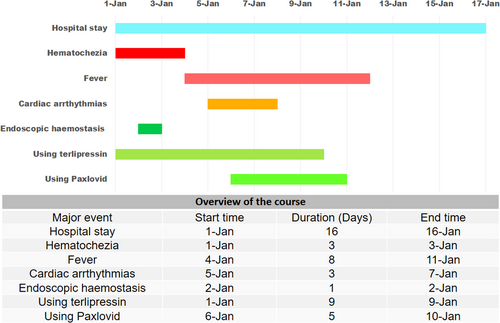
A 50-year-old male was emergency admission with chief complain of hematochezia for over 4 days on January 1. On admission, physical examination revealed an anemic face and dysphoria. Laboratory examination indicated a hypochromic microcytic anemia, hypoalbuminemia and negative for SARS-CoV-2. Moreover, acute ischemic myocardial injury was confirmed by elevated myocardial enzyme indicators (shown in Figure 1) and CT imaging of heart enlargement. From the above results, the preliminary diagnoses of obscure upper GI bleeding and acute ischemic myocardial injury have been made. We applied supportive care and symptomatic treatment, including blood transfusion, and pharmacological therapy (terlipressin iv 0.4 mg/h) immediately.
Exacerbation of hematochezia occurred on the following morning. After the punctate contrast agent extravasation from distal branches of pancreaticoduodenal artery was observed by selective visceral angiography, hemoclip therapy of endoscopic hemostasis was performed. A diagnosis of upper GI bleeding caused by Dieulafoy disease was made after the multidisciplinary clinical evaluation including specialized advices from departments of imaging, interventional medicine, vascular surgery, and gastroenterology.
Receiving endoscopic hemostasis and symptomatic treatment mentioned above, the patient acquired relief in the hematochezia. However, an abrupt low fever (38.5°C), dyspnea and intermittent arrhythmias presenting mainly as Ⅲ-degree atrioventricular block emerged on January 5. Pulmonary rales and wheezing were the prominent features with SO2 significant reduction (81%–96%). Several tests for SARS-CoV-2 nucleic acid were positive, and there were fluctuations of myocardial enzyme indicators. Chest CT showed patchy high-density shadows in the left lower lobe accompanying by a small pleural effusion. Following the diagnosis of severe SARS-CoV-2 infection, a combination of antiviral agent Paxlovid (Nirmatrelvir 300 mg/Ritonavir 100 mg po bid) and symptomatic treatments (terlipressin, omeprazole, etc) were implemented during the following days, meanwhile we strengthened monitoring for electrocardiogram.
Finishing 5-day antiviral therapy, the patient recovered well, with no recurrence of his symptoms. At the time of discharge on January 16, physical examination revealed no gross abnormalities and all abnormal indicators were improved to varying degrees (shown in Figure 1). Before compiling this manuscript, an informed consent and long-term prognoses have been confirmed by conducting a telephone follow-up on the patient. Follow-up information suggested that the patient was still alive and maintained a good quality of life.
3 DISCUSSION
Gastric Dieulafoy's disease, featured with life-threatening outcome and diagnostic conundrum, is caused by gastric submucosal constant-diameter arterial malformation.6 Via the visceral angiography, a vessel disruption and localized hemorrhages from distal branches of pancreaticoduodenal artery were confirmed in our case. Endoscopic therapy, angiographic embolization even direct surgical treatment are alternative interventions, while pharmacotherapy, such as terlipressin, plays less role in most occasions.7
The dilemma of using terlipressin for prevention of re-bleeding was required to be explored, when the patient was suffering from arrhythmias. According to available evidence,5, 7 terlipressin, used in acute esophageal variceal or severe GI bleeding, may induce arrhythmias including torsade de pointes involved with atrioventricular block.8 Besides, a systematic review demonstrated terlipressin accounted for a significant increase in ischemic adverse events when compared to placebo in hepatorenal syndrome,9 and several cases have also reported rare side effects, such as cutaneous necrosis10 or hyponatremic seizure.11 The terlipressin, like vasopressin, causes arrhythmias due to ischemic adverse effects depending on the receptors of V1R and OTR.12
Meanwhile, we could not exclude the possibility of arrhythmias caused by myocardial injury due to the SARS-CoV-2. Relevant research showed that angiotensin-converting enzyme 2 (ACE2) was employed by SARS-CoV-2 as a receptor to induce myocardial injury mediated in direct viral myocardial injury, microvascular injury, systemic hyperinflammatory response, and injury secondary to oxygen supply, and so forth.1
Risking a certain aggravation of existing arrhythmias, although, medical group maintained that the patient would benefit from terlipressin in that situation and continued the initial regime. What mainly supported us were the following three points. First, before the occurrence of arrhythmias, terlipressin has been safely used for several days. Second, there was a strong co-occurrence between arrhythmias and SARS-CoV-2 infection (shown in Figure 2). Finally, the myocardial enzyme and IL-6 indicators for evaluating the severity of myocardial injury and inflammatory response arrived to peak level after verification of SARS-CoV-2 infection (shown in Figure 1).
Inspired by the favorable outcome of the patient, medical group endorsed the decision that retention of terlipressin was implemented under the antiviral therapy. This also reminds that a targeted-oriented therapy of causative pathogen tends to be essential and critical, even the clinical situation has been confounded by multiple interfering factors.
AUTHOR CONTRIBUTIONS
Liangqi Chen and Ke Ma conceived the study. Liangqi Chen, Hongyi Li, and Quan Zhang generated and interpreted data. Ke Ma wrote the manuscript. All authors have read and approved the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
Written informed consent was obtained from the patient and his family for publication of this case report and accompanying images. Ethics review and approval of the study was not required in accordance with the local legislation and institutional requirements.
Open Research
DATA AVAILABILITY STATEMENT
The data presented in the manuscript are available, and further inquiries can be directed to the corresponding author.




