Low COVID-19 vaccine coverage and guardian acceptance among pediatric transplant recipients
Zhigang Zheng and Yefeng Lu contributed equally to this work.
Abstract
To investigate COVID-19 vaccine coverage in immunosuppressed children, assess guardians' intention to vaccinate children, and determine reasons and associated factors. In addition, we attempted to capture the characteristics of them with Omicron. We obtained the vaccination coverage and guardian vaccine acceptance among pediatric transplant recipients through a web-based questionnaire conducted from April 12 to 28, 2022, and performed the statistical analysis. Seven organ transplant recipient children with Omicron were also clinically analyzed. The three-dose vaccine coverage for liver transplant (n = 563) and hematopoietic stem cell transplantation (n = 122) recipient children was 0.9% and 4.9%, and guardian vaccine acceptance was 63.8%. Independent risk factors for vaccine acceptance were the child's age, geographic location, type of transplant, guardian's vaccination status, guardian's level of distress about epidemic events, guardian's risk perception ability, anxiety, and knowledge of epidemic control. The main reasons for vaccine hesitancy were fear of vaccine-induced adverse events and doubts about efficacy. Ultimately, most children infected with Omicron have mild or no symptoms and are infected by intra-family. Since vaccine coverage and guardian acceptance are lowest among liver transplant children, and the infected are mainly intra-family, we should devise more targeted education and vaccination instructions for their guardians.
Abbreviations
-
- EBV
-
- epstein-barr virus
-
- HSCT
-
- hematopoietic stem cell transplantation
-
- LT
-
- liver transplant
-
- PRCPS
-
- perceived risk of COVID-19 pneumonia scale
-
- SAS
-
- self-rating anxiety scale
1 INTRODUCTION
By September 2022, more than 609 million people were infected by COVID-19, with approximately 6.5 million deaths. Several countries were affected by health and economic crises following the rapid spread of COVID-19. COVID-19 is the biggest current global public health threat, causing the infection of around one million people every day.1-3 Unfortunately, poor control of the spread of SARS-CoV-2 in many parts of the world has provided opportunities for the virus to continue to mutate.4, 5 Recently, the Omicron variant BA2.0 that attacked Shanghai spread at an unprecedented rate, which spread more than fourfold as rapidly as the Delta variant6 and also exhibited a strong immune evasion capability. We speculate that it might be the most dominant strain in subsequent world epidemics.7-9 During the outbreak in Shanghai, the number of infected cases increased daily by more than 20 000; the youngest infected were 10 days old. Additionally, several hospitals in Shanghai reported cases of infected pediatric organ transplant recipients, which indicated that the Omicron variant could spread faster and wider than anticipated.
To prevent a COVID-19 pandemic, many countries deployed vaccines, mainly including recombinant vaccines, mRNA vaccines, inactivated vaccines, and adenoviral vector vaccines, to fight against the virus. However, vaccine coverage across different populations in different regions was nonuniform.10-12 Since pediatric organ transplant recipients are maintained in an immunosuppressed state for long periods, they have a higher risk of infection and mortality than normal individuals.13, 14 Numerous authorities such as the American Association for the Study of Liver Diseases, the Chinese Society of Hepatology, the European Association For The Study Of The Liver, the American Academy of Pediatrics (AAP), the UK Medicines and Healthcare products Regulatory Agency, and the European Medicines Agency have indicated that the overall safety and benefits of the COVID-19 vaccine compare very favorably with the risks of vaccine-related diseases. For instance, it has been confirmed that vaccination can prevent Multiple System Inflammatory Syndrome in Children (MIS-C). Vaccinating most individuals in the population is important to prevent further transmission of the infection.15 However, no firm guidelines were provided for the countries to follow a COVID-19 vaccination protocol. Thus, many patients showed vaccine hesitancy, which the WHO regarded as one of the top 10 global health threats in 2019.11
As of September 15, 2022, the AAP reported a total of 14 682 832 cases of COVID-19 in children, with children accounting for 18.4% of all cases. According to the Chinese Center for Disease Control and Prevention, the number of positive infections in Shanghai's local population under the age of 18 accounts for approximately 6.5% of the total positive infections. Children represent a significant proportion of the infected population, and as the infection and vaccination status of this group of pediatric transplant recipients are not yet known, promoting vaccination and changing the opinions of guardians of immunosuppressed children to support vaccination are the most effective measures to control COVID-19; thus, we conducted this study. We determined vaccine coverage of pediatric transplant recipients in China and the attitudes of parents to offer guidance for the vaccination of immunosuppressed children.
2 METHODS
2.1 Study design and participants
Data for this study were obtained through an online questionnaire on the effects of COVID-19 on immunosuppressed children and their willingness to be vaccinated (questionnaires and scales are shown in Supporting Information material “Introduction to Questionnaires and Scales”). The questionnaire mainly included: basic child and family information, full-course vaccination vaccine coverage (post-transplant children have a significantly lower vaccine response than normals due to their long-term immunosuppression, So we recommend that they receive three doses of vaccination) and willingness to vaccinate and their reasons, knowledge of COVID-19 prevention and control, the impact of the current Shanghai Omicron outbreak, and clinical characteristics of the seven Omicron-infected children.
The study was conducted from April 12 to 28, 2022. The study included the responses of the guardians of 563 children who underwent liver transplantation (LT) at the Department of Liver Surgery, Renji Hospital and Shanghai Children's Hospital, Shanghai Jiao Tong University School of Medicine, and 122 children who underwent hematopoietic stem cell transplantation (HSCT) at the Children's Medical Center, Shanghai Jiao Tong University School of Medicine, as well as, 13 immunosuppressed children with other liver diseases and 9 immunosuppressed children with other blood diseases. We performed a descriptive analysis of the results and used logistic regression models to predict the vaccine-hesitant population. Additionally, we acquired the responses of seven organ transplant recipients infected with Omicron (five children with LT and two children with HSCT).
2.2 Data collection and valid questionnaires processing
Since more than 90% of Chinese people use the online social media platform WeChat and we have long established a WeChat patient follow-up group for patients belonging to our departments, we chose to create an online web-based questionnaire and distribute it to the WeChat public platform and the WeChat patient group to facilitate completion by parents. Before that, we created a paper version of the questionnaire, distributed it to 33 patients who were hospitalized, and collected and asked for their feedback to improve the questionnaire and ensure its logic and rationality. Electronic informed consent was set at the beginning of the questionnaire.
The CHERRIES checklist for reporting the results of the Internet e-survey was complied with.16
We called back parents of Omicron-infected children and asked them to upload reports of their first positive nucleic acid and when they turned negative.
A total of 808 questionnaires were received, with 707 valid questionnaires. Eligible participants were: pediatric transplant recipients or children with other immunosuppressive diseases (Figure 1). The following is the processing procedure for screening valid questionnaires.
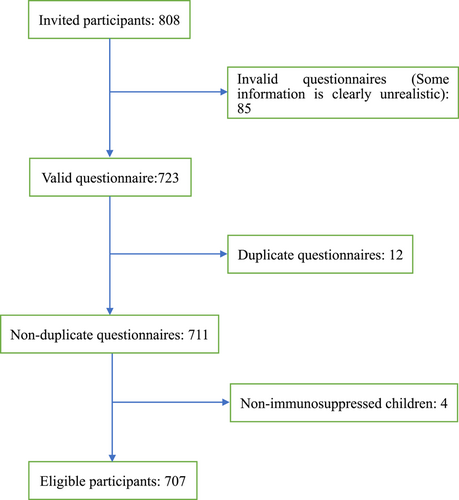
(1) To prevent missing data, we set each question in the questionnaire as “must select” or “must fill in”; (2) at the same time, if a participant fills in a response that is significantly unrealistic (e.g., weight of “2000 kg” or height of “1000 cm”), we will make a callback, and if participants are missing, we will exclude these questionnaires; (3) in case of duplicate questionnaires (two or more questionnaires filled out by the same participant), we will also conduct a follow-up phone call to confirm, and if the participant is missing, we will choose to include the last questionnaire filled out.
2.3 Statistical analysis
Cross-tabulations and χ2 tests were used to assess the unadjusted associations between each characteristic of the participants and the vaccination intention outcomes. To determine the differences in vaccination intentions between guardians of children who underwent LT and HSCT, we used the same method to analyze the differences in various characteristics between these groups. Additionally, partial features were supplemented by Fisher's exact test, and we performed ANOVA to determine the correlation between BMI and acceptance.
Next, we selected the features (p < 0.1) to be included in the binary logistic regression. To determine the presence of a linear relationship between the logit-transformed values of the continuous independent and dependent variables, we used the Box−Tidwell method. Additionally, to optimize the fit of the model, we used Collinearity diagnostics to exclude collinearity between the independent characteristics. Based on the comprehensive consideration of statistical experts and Collinearity testing, we hypothesized that the guardian acceptance might be significantly correlated with their vaccination history, their long-term administrative area of residence, the local epidemic situation, and the economy. Thus, the guardians' intention to vaccinate, the economic situation of their place of residence, and the epidemic situation were not included in the binary logistic regression model.
Finally, to evaluate the model performance, we conducted the Hosmer−Lemeshow goodness-of-fit test and listed the residuals.
All analyses were performed using the SPSS, version R26.0.0.0 (IBM).
3 RESULTS
3.1 High vaccine hesitancy and very low vaccine coverage in pediatric organ transplant recipients
Of the 685 pediatric organ transplant recipients (563 LT recipients and 122 HSCT recipients), only 106 were immunized with the COVID-19 vaccine and only 11 children had completed the full-course vaccination. Thirty-four of 563 (6.0%) LT children received two doses, and a total of 41 of 122 (33.6%) HSCT children received two doses.
Moreover, out of 707 children, the guardians of only 451 (63.7%) children were willing to vaccinate their children with the COVID-19 vaccine. Additionally, vaccine coverage among LT children was considerably lower than that among HSCT children (9.4% vs. 43.4%), and there was a substantial difference in their willingness to be vaccinated (59.3% vs. 82.0%). Thus, we found that the proportion of liver transplant recipients undergoing long-term immunizations was substantially higher than that of HSCT children (96.8% vs. 8.2%). Only 15.1% of the children with LT were over 100 months old, significantly younger than the children with HSCT (59.8%). Similarly, the proportion of children with no education (37.7%) and those in kindergarten (40%) was higher in the LT group than in the HSCT group (14.8% and 18.0%); 67.2% of the children with HSCT were above elementary school grade, which might be related to the requirement of the local policy to vaccinate students in compulsory education (Table 1).
| Basic survey | LT (n = 563) | HSCT (n = 122) | p Value |
|---|---|---|---|
| How many doses of vaccines has your child received? | 0.001 | ||
| 0 | 510 (90.6) | 69 (56.6) | |
| 1 | 14 (2.5) | 6 (4.9) | |
| 2 | 34 (6.0) | 41 (33.6) | |
| 3 | 5 (0.9) | 6 (4.9) | |
| Are you willing to have your baby vaccinated? | <0.001 | ||
| Yes | 334 (59.3) | 100 (82.0) | |
| No | 229 (40.7) | 22 (18.0) | |
| Age group (m) | <0.001 | ||
| ≥100 | 85 (15.1) | 73 (59.8) | |
| 50−100 | 251 (44.6) | 37 (30.3) | |
| 30−50 | 135 (24.0) | 7 (5.7) | |
| <30 | 92 (16.3) | 5 (4.1) | |
| Current educational stage | <0.001 | ||
| No education has been accepted | 212 (37.7) | 18 (14.8) | |
| Kindergarten | 225 (40.0) | 22 (18.0) | |
| Primary school | 100 (17.8) | 56 (45.9) | |
| Junior school | 21 (3.7) | 18 (14.8) | |
| High school | 5 (0.9) | 8 (6.6) | |
| Is the child currently taking immunosuppressants? | <0.001 | ||
| Yes | 545 (96.8) | 10 (8.2) | |
| No | 16 (2.8) | 112 (91.8) | |
| Number of correct answers to prevention and control knowledge questions | 0.072 | ||
| 0 | 133 (23.6) | 32 (26.2) | |
| 1 | 299 (53.1) | 57 (46.7) | |
| 2 | 118 (21.0) | 25 (20.5) | |
| 3 | 13 (2.3) | 8 (6.6) | |
| Score of PRCPS | 0.21 | ||
| 9−16 | 86 (15.3) | 15 (12.3) | |
| 17−24 | 260 (46.2) | 56 (45.9) | |
| 25−32 | 195 (34.6) | 41 (33.6) | |
| 33−40 | 22 (3.9) | 10 (8.2) | |
| Crude score of SAS | 0.62 | ||
| <44 | 141 (25.0) | 35 (28.7) | |
| 45−49 | 281 (49.9) | 53 (43.4) | |
| 50−54 | 127 (22.6) | 30 (24.6) | |
| >54 | 14 (2.5) | 4 (3.3) | |
- Abbreviations: HSCT, hematopoietic stem cell transplantation; PRCPS, perceived risk of COVID-19 pneumonia scale; SAS, self-rating anxiety scale.
3.2 The willingness of guardians to vaccinate was influenced by various complex factors
3.2.1 Correlation of participant characteristics with vaccine hesitancy
Approximately 14.0% of the participants were under 30 months old, while 35.4% of the children were less than 50 months old. Their current educational status also varied, with about 32.1% of the children not yet receiving education. Nearly 58.4% of the guardians lived in economically underdeveloped areas with a GDP of less than RMB 1000 billion. Most children (78.5%) were on long-term immunosuppressive therapy, with a history of infection (58.1%) accounting for the majority. About 60.4% of the guardians scored less than 25 on the perceived risk of COVID-19 pneumonia scale (PRCPS), indicating that they perceived themselves to be at low risk of infection. Only two guardians had a crude self-rating anxiety scale (SAS) score of 39, while the others scored over 40, indicating that almost everyone had at least mild anxiety (Supporting Information: Table 3).
Overall, the factors that were more strongly associated with reluctance to vaccinate babies included age (30−100 months), not yet in elementary school, pediatric LT, the types of immunosuppressants used, living in East and Northeast China, long-term residents of Shanghai or cities with a GDP of RMB 50−100 billion, a very serious epidemic in their city, and the lack of awareness of changes in cases in their location, among others. Also, the guardians of HSCT children were more willing to vaccinate their babies. Additionally, the guardians who were reluctant to get vaccinated were more reluctant to vaccinate their babies. This pattern was also found regarding their vaccination status, that is, guardians who abandoned vaccination mid-way were less willing to vaccinate their babies, and only 42.9% of the guardians who had not yet received the COVID-19 vaccine chose “Yes,” that is, they were willing to vaccinate their children. In the epidemic prevention and control knowledge test, we found that 72.4% of the guardians who answered 0 questions correctly were willing to vaccinate, while 56.1% and 62.1% answered one and two questions correctly, respectively, indicating that guardians who knew little about the prevention and control of the epidemic were more willing to vaccinate their babies, while guardians who knew more about the prevention and control were less likely to vaccinate their babies. Regarding the results of the PRCPS, the two groups with the largest differences between them were “17−24” and “25−32” (also the two groups with the largest samples). The results suggested that guardians who felt they had a relatively high risk of infection were more willing to vaccinate their babies. The SAS results showed that guardians with a greater level of anxiety were less likely to vaccinate their children.
The location of residence (East and Northeast China) was also an independent risk factor, and parents from South China were relatively more accepting of the vaccine (77.8%). Guardians living in cities with relatively advanced economic levels (GDP ≥1000 billion) were more willing to vaccinate their children, but Shanghai was an exception, with only 42.6% of the guardians living in Shanghai permanently willing to do so. Initially, it was surprising to find that 21 guardians chose “Extremely serious” as a response to the question “What is the status of the epidemic in your permanent residence?” Then, we found that 12 of these 21 guardians were from Shanghai. Thus, we conducted telephone follow-ups with vaccine refusal populations in Shanghai and Northeast China, where we learned that repeated outbreaks had eroded their confidence in the vaccine, that even vaccinated populations were not effective in preventing infection, and that there was a risk of adverse vaccine reactions.
3.2.2 A binary logistic regression model for predicting vaccine acceptance
After adjusting for participant characteristics (Table 2, Characteristics with univariate tests p > 0.05 and factors tested for covariance were not included), the characteristics closely associated with vaccine hesitancy included age (30–50 months), long residence in Northeast and East China, pediatric LT, guardians who were not vaccinated and unaware of changes in the number of cases at their location, guardians who were more bothered by epidemic events, less knowledgeable about prevention and control, and relatively more anxious and less perceptive about the epidemic. Children >100 months old were 74% less likely to select “No” than children <30 months old (OR: 2.724 [CI: 1.085−6.844]). Compared to guardians living in East China, those living in South China and Southwest China were 2.5 and 2 times more likely to vaccinate their children (OR: 2.509 [CI: 1.350−4.662]) and (OR: 2.043 [CI: 1.125−3.708]). In contrast, guardians who completed three doses of the COVID-19 vaccine were only about one-fifth as likely to be hesitant to vaccinate their children as guardians who had not received the COVID-19 vaccine (OR: 4.357 [CI: 1.953−9.722]). Guardians who were unaware of the changes in cases were about three times more likely to choose “No” than those who were aware of changes in the number of cases (OR: 0.344 [CI: 0.171−0.691]). Extreme distress about the epidemic increased the likelihood of vaccine hesitation more than threefold (OR: 0.242 [CI: 0.065−0.899]). Additionally, guardians who answered only one question correctly were less likely to vaccinate their babies than those who were more knowledgeable about prevention and control (OR: 0.508 [CI: 0.325−0.793]). SAS and PRCPS also showed significant differences, while other characteristics, including the child's education status and immunosuppressant use, among others, did not show a significant correlation with vaccine hesitancy. The results of the Hosmer−Lemeshow tests were not significantly different (p = 0.927), and the area under the curve was 0.755 (Supporting Information: Figure 1), which indicated that the model fit and performance were highly satisfactory.
3.2.3 Reasons for choosing or rejecting the COVID-19 vaccine
Of the 451 parents who chose to vaccinate their children (Tables 3), 83.1% selected the response “Worried about being infected with COVID-19,” and nearly half (42.4%) of these parents selected this response because they believed in the safety and efficacy of the vaccine. Some of the participants (16.2%) were forced to vaccinate their children because of local and school policies. Notably, 35.7% of the participants chose the response “Volunteering to do our part to prevent and control the epidemic,” which indicated a strong sense of dedication.
Among the 256 participants who were hesitant about vaccines, the main reason (96.5%) was the worry that vaccination would cause injury to their children, followed by doubts about the efficacy of the current vaccines (23.8%).
3.2.4 Impact of the Omicron variant epidemic in Shanghai
From the previous results, we learned that participants who were long-term residents of Shanghai were reluctant to receive the COVID-19 vaccine due to the current epidemic (Table 4; 57.4% rejected the vaccine), probably considering that they should be strictly quarantined now rather than going out.
| Characteristic | p Value | OR (95%CI) |
|---|---|---|
| Age group (m) | ||
| <30 | 0.008 | Reference |
| 30−50 | 0.913 | 0.961 (0.468−1.971) |
| 50−100 | 0.725 | 1.163 (0.503−2.689) |
| ≥100 | 0.033 | 2.724 (1.085−6.844) |
| Current educational stage | ||
| No education has been accepted and kindergarten | Reference | |
| Primary school and higher education | 0.192 | 1.550 (0.803−2.993) |
| Geographical location(administrative regions) | ||
| Eastern China | 0.005 | Reference |
| Northern China | 0.027 | 1.969 (1.081−3.588) |
| Central China | 0.719 | 1.111 (0.627−1.970) |
| Southern China | 0.004 | 2.509 (1.350−4.662) |
| Northeastern China | 0.181 | 0.473 (0.158−1.417) |
| Southwestern China | 0.019 | 2.043 (1.125−3.708) |
| Northwestern China | 0.736 | 0.849 (0.328−2.201) |
| Type of disease | ||
| Pediatric liver transplantation | 0.074 | Reference |
| Hematopoietic stem cell transplantation | 0.023 | 3.069 (1.164−8.091) |
| Immunosuppressed children with other liver diseases | 0.917 | 1.086 (0.230−5.132) |
| Immunosuppressed children with other blood diseases | 0.181 | 4.910 (0.477−50.513) |
| Number of types of Immunosuppressants used | ||
| 0 | 0.919 | |
| 1 | 0.611 | 0.792 (0.321−1.949) |
| 2 | 0.676 | 0.810 (0.301−2.177) |
| 3 | 0.803 | 1.265 (0.199−8.040) |
| Number of doses of vaccination for guardians | ||
| 0 | 0.000 | Reference |
| 1 | 0.066 | 3.614 (0.917−14.238) |
| 2 | 0.113 | 1.975 (0.851−4.584) |
| 3 | 0.000 | 4.357 (1.953−9.722) |
| Are you aware of the changes in the number of cases at your location? | ||
| Yes | Reference | |
| No | 0.003 | 0.344 (0.171−0.691) |
| Please recall the recent outbreak of COVID-19 and briefly describe how much this event bothered you. | ||
| Never botheration | 0.022 | Reference |
| Mild botheration | 0.043 | 0.288 (0.086−0.961) |
| Moderate botheration | 0.213 | 0.462 (0.137−1.558) |
| Severe botheration | 0.259 | 0.488 (0.140−1.697) |
| Extremely severe annoyance | 0.034 | 0.242 (0.065−0.899) |
| Number of correct answers to prevention and control knowledge questions | ||
| 0 | 0.025 | Reference |
| 1 | 0.003 | 0.508 (0.325−0.793) |
| 2 | 0.206 | 0.707 (0.413−1.210) |
| 3 | 0.565 | 0.716 (0.230−2.233) |
| Crude score of SAS | ||
| <44 | 0.006 | Reference |
| 45−49 | 0.358 | 0.816 (0.530−1.258) |
| 50−54 | 0.001 | 0.429 (0.256−0.718) |
| >54 | 0.175 | 0.464 (0.153−1.408) |
| Score of PRCPS | ||
| 9−16 | 0.009 | Reference |
| 17−24 | 0.326 | 0.770 (0.456−1.298) |
| 25−32 | 0.132 | 1.534 (0.879−2.677) |
| 32 | 0.772 | 1.155 (0.436−3.057) |
- Note: We used collinearity diagnosis as well as a combination of considerations to exclude some features with multiple collinearity before inclusion.
- Abbreviations: OR, odds ratio; PRCPS, perceived risk of COVID-19 pneumonia scale; SAS, SAS, self-rating anxiety scale.
- Binary logistic regression model logit = natural log [Pr(yes)/Pr(no)].
| Reason | Number | Percentage |
|---|---|---|
| Why would you like to have your baby vaccinated? | n = 451 | |
| Worry about being infected with COVID-19 | 375 | 83.1 |
| Confidence in vaccine safety and efficacy | 191 | 42.4 |
| Volunteering to do our part to prevent and control the epidemic | 161 | 35.7 |
| Influenced by the positive publicity of the government and society | 139 | 30.8 |
| Be urged to be vaccinated by units and schools | 73 | 16.2 |
| Influenced by those around you | 32 | 7.1 |
| Why would you not like to have your baby vaccinated? | n = 256 | |
| Fear of vaccine-induced adverse events | 247 | 96.5 |
| Doubts about the efficacy of vaccines | 61 | 23.8 |
| Mental rejection | 11 | 4.3 |
| Inconvenient or no time for vaccination | 3 | 1.2 |
| Others have been vaccinated, there is no need to vaccinate | 2 | 0.8 |
| The epidemic is basically under control and there is no need for vaccination | 1 | 0.4 |
| Characteristic | Intent to be vaccinated | p Value | |
|---|---|---|---|
| Yes (n = 451) | No (n = 256) | ||
| Gender | 0.77 | ||
| Female | 233 (67.9) | 110 (32.1) | |
| Male | 218 (59.9) | 146 (40.1) | |
| BMI | 0.58 | ||
| Mean (SD) | 17.66 (5.01) | 17.88 (5.81) | |
| Range | 3.59−47.84 | 11.87−49.95 | |
| Age group (m) | 0.006 | ||
| <30 | 72 (75.0) | 24 (25.0) | |
| 30−50 | 89 (58.6) | 63 (41.4) | |
| 50−100 | 177 (59.8) | 119 (40.2) | |
| ≥100 | 113 (69.3) | 50 (30.7) | |
| Current educational stage | 0.039 | ||
| No education has been accepted and kindergarten | 303 (61.3) | 191 (38.7) | |
| Primary school and higher education | 148 (69.5) | 65 (30.5) | |
| Type of disease | <0.001 | ||
| Pediatric liver transplantation | 334 (59.3) | 229 (40.7) | |
| Hematopoietic stem cell transplantation | 100 (82.0) | 22 (18.0) | |
| Immunosuppressed children with other liver diseases | 9 (69.2) | 4 (30.8) | |
| Immunosuppressed children with other blood diseases | 8 (88.9) | 1 (11.1) | |
| Number of types of Immunosuppressants used | <0.001 | ||
| 0 | 120 (78.9) | 32 (21.1) | |
| 1 | 271 (60.2) | 179 (39.8) | |
| 2 | 54 (56.3) | 42 (43.8) | |
| 3 | 6 (66.7) | 3 (33.3) | |
| Number of types of previous viral and bacterial infections | 0.473 | ||
| 0 | 196 (66.2) | 100 (33.8) | |
| 1 | 155 (60.5) | 101 (39.5) | |
| 2 | 89 (63.6) | 51 (36.4) | |
| 3 | 11 (73.3) | 4 (26.7) | |
| Geographical location (administrative regions) | 0.010 | ||
| Eastern China | 217 (60.4) | 142 (39.6) | |
| Northern China | 52 (70.3) | 22 (29.7) | |
| Central China | 44 (59.5) | 30 (40.5) | |
| Southern China | 63 (77.8) | 18 (22.2) | |
| Northeastern China | 7 (38.9) | 11 (61.1) | |
| Southwestern China | 53 (69.7) | 23 (30.3) | |
| Northwestern China | 15 (60.0) | 10 (40.0) | |
| Total GDP of the city where the parent usually lives (billion RMB) | 0.004 | ||
| >1000 | 172 (69.6) | 75 (30.4) | |
| 500−1000 | 61 (61.0) | 39 (39.0) | |
| <500 | 198 (63.3) | 115 (36.7) | |
| Shanghai | 20 (42.6) | 27 (57.4) | |
| Whether the guardians themselves are willing to be vaccinated? | <0.001 | ||
| Yes | 446 (66.0) | 230 (34.0) | |
| No | 5 (16.1) | 26 (83.9) | |
| Number of doses of vaccination for guardians | <0.001 | ||
| 0 | 15 (42.9) | 20 (57.1) | |
| 1 | 10 (62.5) | 6 (37.5) | |
| 2 | 91 (53.2) | 80 (46.8) | |
| 3 | 335 (69.1) | 150 (30.9) | |
| Number of correct answers to prevention and control knowledge questions | 0.013 | ||
| 0 | 126 (72.4) | 48 (27.6) | |
| 1 | 214 (58.5) | 152 (41.5) | |
| 2 | 96 (65.8) | 50 (34.2) | |
| 3 | 15 (71.4) | 6 (28.6) | |
| Score of PRCPS | 0.026 | ||
| 9−16 | 68 (64.8) | 37 (35.2) | |
| 17−24 | 187 (58.1) | 135 (41.9) | |
| 25−32 | 174 (70.2) | 74 (29.8) | |
| 32 | 22 (68.8) | 10 (31.3) | |
| Crude score of SAS | 0.020 | ||
| <44 | 126 (69.6) | 54 (30.4) | |
| 45−49 | 228 (65.5) | 120 (34.5) | |
| 50−54 | 86 (54.1) | 73 (45.9) | |
| >54 | 11 (57.9) | 8 (42.1) | |
| What is the status of the epidemic in your permanent residence? | 0.018 | ||
| Few or almost no epidemic | 216 (64.9) | 117 (35.1) | |
| Occasional confirmed infections | 220 (65.1) | 118 (34.9) | |
| Extremely serious | 15 (41.7) | 21 (58.3) | |
| Are you aware of location prevention and control measures? | 0.076 | ||
| Yes | 437 (64.5) | 241 (35.5) | |
| No | 14 (48.3) | 15 (51.7) | |
| Are you aware of the changes in the number of cases at your location? | 0.009 | ||
| Yes | 431 (65.0) | 232 (35.0) | |
| No | 20 (45.5) | 24 (54.5) | |
| What is the most significant impact of the pandemic on you? | 0.108 | ||
| Work and learning | 114 (65.5) | 60 (34.5) | |
| Daily life | 205 (64.1) | 115 (35.9) | |
| Family reunion | 53 (62.4) | 32 (37.6) | |
| Mood | 26 (81.3) | 6 (18.8) | |
| Others | 53 (55.2) | 43 (44.8) | |
| Please recall the recent outbreak of Newcastle pneumonia and briefly describe how much this event bothered you? | 0.022 | ||
| Never botheration | 19(82.6) | 4 (17.4) | |
| Mild botheration | 150 (58.8) | 105 (41.2) | |
| Moderate botheration | 161 (67.4) | 78 (32.6) | |
| Severe botheration | 87 (68.5) | 40 (31.5) | |
| Extremely severe annoyance | 33 (52.4) | 30 (47.6) | |
- Abbreviations: PRCPS, perceived risk of COVID-19 pneumonia scale; SAS, SAS, self-rating anxiety scale.
The results of the survey (Supporting Information: Table 4) showed that 170 of 707 participants showed a positive change (initially unwilling to vaccinate to now willing to vaccinate) as a result of the Shanghai epidemic; however, 14 showed a negative change (initially willing to vaccinate to now unwilling to vaccinate), indicating that the epidemic strongly affected the guardians' awareness of prevention and control. Of the 177 participants with positive changes (including 144 children with LT and 24 children with HSCT), 78.2% thought that the transmission of Omicron was too rapid and the epidemic was too severe in Shanghai to change their decision due to the fear of infection; 7.6% of these participants were concerned that Omicron might affect the children more severely (especially immunosuppressed children) and reported having seen similar news or social media articles. Among those with negative transitions (11 children with LT and 3 children with HSCT), 6 were concerned that vaccination might cause adverse reactions, such as fluctuations in liver function or changes in blood counts, and 5 considered transplant recipient children unsuitable for vaccination. In a survey on the sleep status of children during the epidemic, only 7.4% of the parents expressed dissatisfaction relative to the pre-epidemic period, indicating that the epidemic impacted the daily lives of the children very mildly.
3.2.5 Seven cases of Omicron infection in pediatric organ transplants
In this survey (Supporting Information: Table 5), 7 infected children participated (five LT recipients and two HSCT recipients), all of whom were located in Shanghai and infected with the Omicron variant. None of the LT children were vaccinated with the COVID-19 vaccine, and 4 of the guardians were infected. Of the 5 LT children, 3 were less than 3 years old, all were being administered immunosuppressants, and 2 had been infected with EBV. Three of the parents identified their children as infected by intrafamilial transmission, and 2 children, based on the results of a population nucleic acid test, had a high probability of also being affected due to intrafamilial transmission, considering that 6 of their family members were also infected. Fortunately, 3 infected children were asymptomatic, and the other 4 were not severely symptomatic. Five children were untreated and were only quarantined at home, in the hospital, or at centralized isolation facilities. Only 2 children were hospitalized. The infection changed the attitude toward the vaccine, and the guardians of 3 children, who had initially rejected the vaccine, were now willing to get vaccinated stating various reasons.
Almost all guardians were from East China (Shanghai and around Shanghai). Four of the guardians did not answer any questions correctly, which indicated their extremely low awareness of protection. Additionally, most of them had PRCPS scores above 32, indicating that they perceived the risk of infection as very high. This might be due to the direct effect of the infection. The crude SAS score of 6 guardians was 45–54; a population with a SAS score above 45 had a stronger association with vaccine hesitancy in previous predictions. Given that the 6 guardians did not complete the vaccination course, today's infection substantially confirmed our analysis.
The average time to conversion to negative for the 7 children was 18.3 days, which was higher than the previous data for the whole population (7−14 days). The cumulative number of liver transplant recipients at Renji Hospital is approximately 6000, and the survey showed that there were 9 infected patients (4 adults and 5 children) in this Shanghai pandemic, which is lower than the proportion of the whole population in Shanghai pandemic (2.7%), which is directly related to the fact that our liver transplant recipients have developed long-term habits of wearing masks and standard hand washing. Although the risk of infection in transplant recipients is reduced through long-term good hygiene education, the rate of severe disease does not seem to be as well. One of the 10 kidney transplant recipients and one of the 9 LT recipients in Renji Hospital presented with severe symptoms, a higher rate than the disclosed population rate of severe disease, which may suggest a significant risk of severe disease as well as death among transplant recipients.
4 DISCUSSION
In our study, we investigated COVID-19 vaccination coverage in pediatric organ transplant recipients compared to a negligible rate of full-course vaccination in guardians (68.6%). The number of Omicron infections in Shanghai increased by more than 20 000 per day. Children are important transmitters of the COVID-19 virus and can pose a significant risk to the elderly or other age groups, although the risk is lower than that of transmitting the influenza virus.17 Several studies have shown the critical role of the COVID-19 vaccine in reducing the risk of serious illness, hospitalization, mortality, and medical stress.18 Additionally, the immunological effects of SOT recipients of the COVID-19 vaccine have been demonstrated in many studies. The study was conducted in the third year of the epidemic and at the peak of the Omicron pandemic, and the Omicron variant was found to be more infectious than all previous strains (R0 > 9). Martin Hibberd, a professor at the London School of Hygiene and Tropical Medicine, suggested that the R0 of Omicron could reach 10,19 suggesting that at least 90% of the population would need to be vaccinated to develop effective herd immunity; however, some studies found that vaccine coverage was much lower than this target.
The attitude of the guardians revealed by the survey was discouraging. Early surveys conducted in the United States also showed parental resistance to COVID-19 vaccination in children, although most of the infected vaccinated individuals were mildly ill, and only a few children died due to COVID infection.20 Less than 64% of the guardians were willing to vaccinate their children, and this was not enough to prevent and control the epidemic. However, because children on long-term immunosuppression have a lower immune function than normal people,21 both AALSD and the Chinese Medical Association have a positive attitude toward COVID-19 vaccination for liver transplant recipients. Different information that can be obtained from different areas can largely contribute to these associations. For example, in economically backward areas, people are relatively less educated,22, 23 which might affect their judgment of the situation based on the information they receive and their knowledge regarding the prevention and control of the disease. The strength of the propaganda of the local government on various matters of the epidemic and the vaccine promotion strategies might also directly affect the attitude of the public, as found in the study, where people trusted more than questioned the government and doctors. A study found that the recommendations of doctors can greatly increase confidence in vaccines.24 Therefore, organizations and anti-epidemic workers must spread the correct information to combat false information and rumors that appear on social media to eliminate political and public health hazards. This requires the continuous efforts of governments, anti-epidemic workers, and the public.25 Inaccurate or inappropriate dissemination of information on the epidemic might be dangerous.26 Also, online platforms have the ethics and obligation to screen information and reduce the circulation of fake information, negative inducements, and harmful social bots to the masses.27-29
Additionally, schools have educated children about the disease and urged them to get vaccinated, and in many countries, the government has offered free vaccination to fight the virus. However, many people with relatively low education and low social awareness still avoid vaccination. We can use predictive models to more accurately target and educate populations at a higher risk of vaccine hesitation. The general lack of knowledge about the prevention and control of the epidemic in the population put individuals in a relatively passive position; for example, several children were infected by other family members. Some studies have shown that face-to-face interventions can eliminate vaccine hesitancy, which requires a more accurate distinction between those who are willing to be vaccinated and those who are vaccine-hesitant or reject vaccination.30 In this study, we also showed that guardians were mostly ignorant of the prevention and control measures, and had low PRCPS scores and high SAS scores. Two studies conducted in the United States showed that the extent to which participants perceived infection with COVID-19 substantially influenced their intention to get vaccinated.31 In contrast to previous findings by Bendau et al.,32 the SAS scores in this study showed that greater anxiety of the population within a certain range was associated with lesser willingness to vaccinate their children. However, the willingness of the parents to get vaccinated was unaffected, which suggested that parents might be overly cautious when dealing with the medical issues of their children. Of course, this is directly related to many factors, such as the vague definition of suitable/contraindicated groups for vaccination, the lack of publicity/civic education, and the lack of openness and transparency of information on the efficiency/safety of vaccination, which has led to many people's doubts. There was also a significant level of vaccine hesitancy in a study conducted in Zhejiang, China, regarding the attitudes of the guardians toward influenza vaccination of their children.33
Based on the fact that Omicron infections in children with organ transplants occur primarily due to intrafamilial transmission, we suggest developing special homes, epidemic prevention campuses, and vaccination guidelines (handbooks and online videos) for this special population of children with organ transplants and continuously improving these facilities and guidelines to reduce direct transmission within the family. Also, since most students have been vaccinated, psychological counseling and reassurance should be provided by healthcare providers, guardians, and schools to avoid causing psychological harm to children with organ transplants.
5 STRENGTHS AND LIMITATIONS
The Department of Liver Surgery at Renji Hospital, Shanghai Jiao Tong University School of Medicine, is the largest pediatric LT center in the world, and its pediatric LT volume has ranked first in the world for many years, providing an adequate sample size. We believe that our study is representative of pediatric organ transplant recipients, and most importantly, we are the first study to focus on COVID-19 vaccination coverage and intentions and Omicron variant infection in an immunosuppressed population of children who are organ transplant recipients.
We consider that the main limitation of this study is that most patients infected with Omicron were apprehensive, so only 7 cases completed the questionnaire, which may have caused some degree of bias in the analysis of infection symptoms. In addition, because this study was conducted based on an online survey, we were unable to test the veracity of the participants' answers.
AUTHOR CONTRIBUTIONS
Prof. Feng Xue and Prof. Qiang Xia designed the project. Prof. Feng Xue, Prof. Yanbo Zhu, Dr. Ji Wu, and Dr. Zhigang Zheng completed the questionnaire design. Prof. Jing Chen, Prof. Ting Zhang, and Prof. Qing Cao, in charge of patient recruitment. Prof. Yi Luo, Dr. Yefeng Lu, Dr. Ming Wang, Dr. Ping Wan, Dr. Tao Zhou, Dr. Mingxuan Feng, Dr. Jianyun Zhu, and Dr. Hao Ji responsible for questionnaire collection. Prof. Yanyan Song and Dr. Zheng conducted the statistical analysis, and Dr. Zheng wrote the manuscript. All authors were involved in interpreting the analysis results and reading through the final version.
ACKNOWLEGMENTS
This work was supported by the National Natural Science Foundation of China (grant numbers 82170669); Shanghai Municipal Hospital Three-year-project for Clinical Skills' Promotion and Innovation (grant numbers SHDC2020CR 2003A); Renji Hospital Clinical Research Innovation and Cultivation Fund (grant numbers PYI-17-002).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
Our study was certified by the Ethics Committee of Renji Hospital, Shanghai Jiao Tong University School of Medicine. This survey was described in detail to all participants, who completed this questionnaire with full knowledge and consent to the study.
Open Research
DATA AVAILABILITY STATEMENT
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors. The data that support the findings of this study are available from the corresponding author upon reasonable request.




