Excess risk for acute myocardial infarction mortality during the COVID-19 pandemic
Yee Hui Yeo, Maggie Wang, and Xinyuan He contributed equally to this study.
Susan Cheng and Fanpu Ji are co-senior authors.
Abstract
The COVID-19 pandemic has had a detrimental impact on the healthcare system. Our study armed to assess the extent and the disparity in excess acute myocardial infarction (AMI)-associated mortality during the pandemic, through the recent Omicron outbreak. Using data from the CDC's National Vital Statistics System, we identified 1 522 669 AMI-associated deaths occurring between 4/1/2012 and 3/31/2022. Accounting for seasonality, we compared age-standardized mortality rate (ASMR) for AMI-associated deaths between prepandemic and pandemic periods, including observed versus predicted ASMR, and examined temporal trends by demographic groups and region. Before the pandemic, AMI-associated mortality rates decreased across all subgroups. These trends reversed during the pandemic, with significant rises seen for the youngest-aged females and males even through the most recent period of the Omicron surge (10/2021–3/2022). The SAPC in the youngest and middle-age group in AMI-associated mortality increased by 5.3% (95% confidence interval [CI]: 1.6%–9.1%) and 3.4% (95% CI: 0.1%–6.8%), respectively. The excess death, defined as the difference between the observed and the predicted mortality rates, was most pronounced for the youngest (25–44 years) aged decedents, ranging from 23% to 34% for the youngest compared to 13%–18% for the oldest age groups. The trend of mortality suggests that age and sex disparities have persisted even through the recent Omicron surge, with excess AMI-associated mortality being most pronounced in younger-aged adults.
Abbreviations
-
- AMI
-
- acute myocardial infarction
-
- ASMR
-
- Age-standardized mortality rate
-
- CDC WONDER
-
- the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research
-
- COVID-19
-
- Coronavirus Disease 2019
-
- ICD-10
-
- International Classification of Diseases–Tenth Revision
-
- NVSS
-
- National Vital Statistics System
-
- SAPC
-
- semiannual percentage change
1 INTRODUCTION
The excess mortality seen during the Coronavirus Disease 2019 (COVID-19) pandemic has been undeniably profound. In the United States and worldwide, rates of excess mortality due to COVID-19 have been especially elevated for adults aged 65 years or older, males, and racial/ethnic minority groups.1, 2 Importantly, the measurable total excess in mortality includes deaths attributed to several major non-COVID-19-specific causes.3, 4 A substantial proportion of these non-COVID-19-specific deaths include cardiovascular deaths due to ischemic heart disease.4 Before the pandemic, ischemic heart disease was the leading worldwide cause of death—but with steadily improving downward trends in year-to-year mortality rates, observed through 2019.5, 6 Unfortunately, analyses of mortality trends since 2020 indicate that the COVID-19-associated excess in ischemic heart disease mortality has effectively erased these prior gains.4
The exact drivers of excess ischemic heart disease mortality seen during the pandemic remain unclear, although many probable and potential causes have been identified. For instance, there is now abundant evidence of how patients with pre-existing or newly developed cardiovascular conditions have experienced gaps and delays in access to care, especially during periods of COVID-19 surge.7-10 Additionally, mounting data demonstrates that a proportion of COVID-19-affected individuals are at increased risk for thrombogenic events, including acute coronary events, either during or following the acute infection phase.11 It is also possible that the excess in cardiovascular risks observed during earlier phases of the pandemic was associated to generally more severe COVID-19 illness caused by more virulent variants of SARS-CoV-2. To further understand the nature and potential origins of excess mortality attributed to ischemic heart disease during the pandemic and their changes over time, we analyzed national vital statistics data to comprehensively examine and compare temporal trends in mortality rates across demographic groups and geographic regions in the United States.
2 MATERIALS AND METHODS
2.1 Study design and population
We studied de-identified death data from the Centers for Disease Control and Prevention's National Vitals Statistics System (NVSS), which processed data from the death certificate of >99% of American decedents, updated to March 31, 2022.12 Decedents' demographic data include age, sex, and clinical data, which include the cause of death. The cause of death is documented as an entity and record axis. The entity axis exhibits all causes of death found in the death certificate, while the record axis presents a refined list by combining associated diagnoses and excluding diagnoses that are overlapped or fail the logical check.13 Given a higher specificity, we derived the cause of death from the record axis. Data between January 1, 2012, and December 31, 2020, were downloaded from the Vital Statistics Online Data Portal of the CDC,14 while the data for 2021 and 2022 were collected from the Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) platform.15 This study did not seek approval from the institutional review board as the data are publicly available and deidentified. The conduction and presentation of the study were compliant with the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
2.2 Definitions
International Classification of Diseases–Tenth Revision (ICD-10) codes were used to define the diagnoses used in this study, including acute myocardial infarction (AMI) (I21) and COVID-19 (U07.1). Due to the rapid progression and high risk of complications, AMI may not be listed as the underlying cause of death by nosologists. Therefore, to augment the inclusivity of the study, we included decedents with AMI listed as one cause on the death certificate (a decedent could have multiple causes of death).
To account for seasonal variation in all analyses, we divided the study period into 6-month seasonal segments (i.e., April to September “Spring/Summer” and October to March “Fall/Winter” segments). We defined the period of the COVID-19 pandemic as April 2020 onwards. To facilitate temporal trends analyses, we further characterized the following periods: April 2020 to September 2020 as “Pandemic Epoch 1” (encompassing effects of the first surge), October 2020 to March 2021 as “Pandemic Epoch 2” (encompassing effects of the second surge), April 2021 to September 2021 as “Pandemic Epoch 3” (encompassing effects of the third surge), and October 2021 to March 2022 as “Pandemic Epoch 4” (encompassing effects of the Omicron surge). We considered the following age groups: 25–44, 45–64, and 65 years and above.
2.3 Statistical analysis
We estimated the age-standardized AMI-associated mortality rates, with 10-year age groups from the 2010 US census as a reference, for the entire study period (April 1, 2012, and March 31, 2022) and across the epochs defined above. We first perform a forecast analysis to predict the AMI-associated age-standardized mortality rate (ASMR) for 2020 and 2021, based on trends observed from 2012 to 2019. We evaluated several models (e.g., k-Nearest Neighbors, autoregressive moving-average, autoregressive integrated moving average, linear regression, polynomial regression) to identify the model demonstrating the best model fit for the given distribution of mortality rates. We then calculated the absolute and relative difference between the observed and predicted rates, with model fit evaluated based on the total model R2 value. We estimated the semiannual percentage change (SAPC), between epochs, in mortality rates by age group, sex, and further stratification by the sex-age group. To determine the effect size and directionality of trends in AMI-associated mortality, we used Joinpoint piecewise regression (v.4.9.1.0; NIH) which provides information regarding whether the mortality trend could be explained by ≥1 trend segment(s).16 We used a Monte Carlo permutation analysis to assess the significance of effect sizes.
We categorized the cause of death by COVID-19 and non-COVID-19-associated death during the pandemic to determine the direct and indirect impact of the pandemic on the AMI-associated mortality rate. We also determined the state-level geographic variation of mortality rate and the difference in mortality rate between the two periods during the pandemic. Analyses were performed using R (v.4.0.2) (data management) and Pycharm (v.3.9.0) (predictive modeling) in addition to Joinpoint regression. A two-tailed p < 0.05 was considered statistically significant.
3 RESULTS
3.1 Decedent population and characteristics
A total of 1 522 669 AMI-associated deaths occurred in the United States from 4/1/2012 to 3/31/2022 (Supporting Information: Table S1). Of these, 31 036 (2%) occurred in the 25–44-year age group, 341 510 (22%) in the 45–64-year age group, and 1 150 123 (76%) in the ≥65-year age group. The 881 455 (58%) deaths in males outnumbered the 641 214 (42%) deaths in females.
3.2 AMI-associated mortality by age and sex
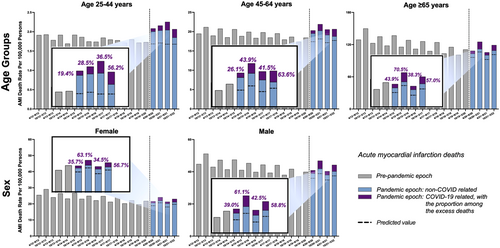
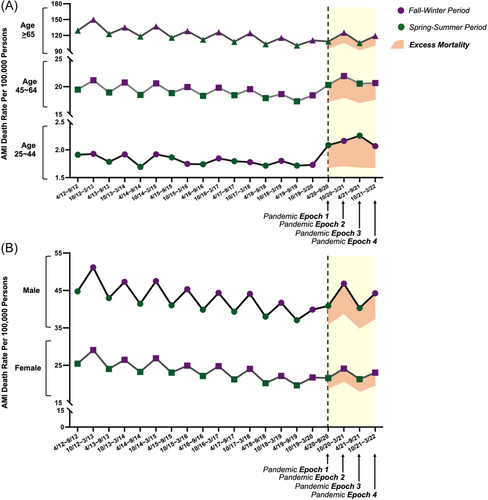
Age-standardized AMI-associated mortality rates increased from prepandemic to postpandemic epochs across all age groups (Figure 1). Despite a reduction in the 4th epoch, the relative increase remained disproportionately pronounced in the youngest age group, with the percent difference between observed and predicted mortality rates ranging from 23% to 34% for the youngest compared to 13% to 18% for the oldest age groups (Table 1); this trend was evident even when accounting for seasonality of events (Figure 2A and Supporting Information: Figure S1). Moreover, the change in the proportion of COVID-19- and non-COVID-19-associated deaths varied substantially across all age groups. While the proportion of COVID-19 increased considerably from the 1st epoch to the 2nd epoch, followed by a decrease in the 3rd epoch for both the middle and oldest age groups, it gradually increased through the first three epochs in the youngest age group. Subsequently, there was a striking increase in the proportions of COVID-19-associated mortality observed in all age groups in the fourth epoch (Figure 1). The excess mortality rates are displayed as an absolute number of deaths in Table 2. More than three-quarters of deaths were aged 65 or above.
| Age-standardized mortality rate (per 100 000 persons) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prepandemic 4/2012–9/2012 | Pandemic epoch 1 4/2020–9/2020 | Pandemic epoch 2 10/2020–3/2021 | Pandemic epoch 3 4/2021–9/2021 | Pandemic epoch 4 10/2021–3/2022 | |||||||||
| Observed | Observed | Predicted [95% CI] | % Differencea | Observed | Predicted [95% CI] | % Differencea | Observed | Predicted [95% CI] | % Differencea | Observed | Predicted [95% CI] | % Differencea | |
| Age | |||||||||||||
| 25–44 | 1.91 | 2.08 | 1.69 [1.48–1.91] | +23.37% | 2.16 | 1.71 [1.56–1.86] | +26.34% | 2.25 | 1.68 [1.45–1.91] | +34.22% | 2.07 | 1.68 [1.52–1.85] | +23.02% |
| 45–64 | 19.47 | 20.31 | 17.39 [16.58–18.20] | +16.80% | 21.92 | 18.10 [17.53–18.66] | +21.11% | 20.56 | 17.14 [16.28–18.01] | +19.93% | 20.66 | 17.70 [17.10–18.31] | +16.70% |
| ≥65 | 129.16 | 108.48 | 96.12 [92.70–99.53] | +12.86% | 125.24 | 106.22 [95.67–116.77] | +17.90% | 105.54 | 92.21 [88.54–95.87] | +14.46% | 119.11 | 101.30 [90.00–112.61] | +17.58% |
| Sex | |||||||||||||
| Female | 25.45 | 21.62 | 18.84 [18.00–19.69] | +14.74% | 24.12 | 20.65 [18.69–22.62] | +16.82% | 21.31 | 18.05 [17.15–18.96] | +18.05% | 23.05 | 19.68 [17.58–21.79] | +17.12% |
| Male | 44.77 | 40.88 | 35.93 [34.66–37.20] | +13.77% | 46.83 | 38.84 [36.12–41.56] | +20.58% | 40.32 | 34.9 [33.54–36.26] | +15.52% | 44.24 | 37.43 [34.51–40.35] | +18.21% |
- a % Difference between predicted and observed values.
| Excess AMI-associated deaths (N) | ||||
|---|---|---|---|---|
| Pandemic epoch 1 4/2020–9/2020 | Pandemic epoch 2 10/2020–3/2021 | Pandemic epoch 3 4/2021–9/2021 | Pandemic epoch 4 10/2021–3/2022 | |
| The number of excess AMI-associated mortality, overall | ||||
| Age group | ||||
| 25–44 years | 1427 | 1464 | 1441 | 1439 |
| 45–64 years | 15 384 | 15 893 | 15 015 | 15 555 |
| ≥65 years | 50 581 | 56 129 | 48 864 | 53 565 |
| Sex | ||||
| Female | 27 114 | 29 860 | 25 957 | 28 426 |
| Male | 40 171 | 43 449 | 39 152 | 41 975 |
| The number of excess AMI-associated mortality, SARS-CoV-2 infection group | ||||
| Age group | ||||
| 25–44 years | 66 | 110 | 180 | 187 |
| 45–64 years | 675 | 1480 | 1229 | 1644 |
| ≥65 years | 2848 | 7041 | 2750 | 5386 |
| Sex | ||||
| Female | 1444 | 3195 | 1568 | 2736 |
| Male | 2145 | 5436 | 2591 | 4481 |
| The number of excess AMI-associated mortality, non-SARS-CoV-2 infection group | ||||
| Age group | ||||
| 25–44 years | 1361 | 1354 | 1261 | 1252 |
| 45–64 years | 14 709 | 14 413 | 13 786 | 13 911 |
| ≥65 years | 47 733 | 49 088 | 46 114 | 48 179 |
| Sex | ||||
| Female | 25 670 | 26 665 | 24 389 | 25 690 |
| Male | 38 026 | 38 013 | 36 561 | 37 494 |
Consistently, in temporal trends analyses, AMI-associated mortality rates significantly decreased during the prepandemic epochs across all age groups and for both sexes (Figures 2 and 3, Supporting Information: Table S2); then, from before the start of the pandemic to the most recent pandemic epoch, AMI-associated mortality rates were observed to reverse direction and overall increase—and this rise was especially pronounced and statistically significant for the youngest and middle-age group among whom the SAPC in AMI-associated mortality increased by 5.3% (95% confidence interval [CI]: 1.6%–9.1%) and 3.4% (95% CI: 0.1%–6.8%), respectively (Supporting Information: Table S2).
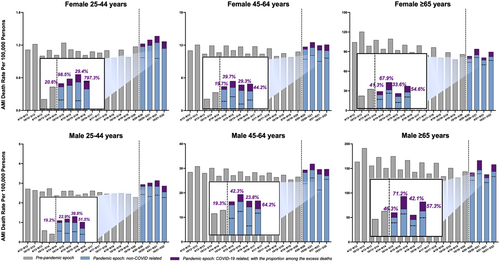
While the trends of excess death were similar for both sexes (Table 1 and Figure 2B), substantial variation was seen across the sex-specific, age-stratified groups. In age- and sex-stratified analyses (Table 3, Figure 3, and Supporting Information: Figures S2 and S3), the percent differences between observed and predicted mortality rates were highest among the youngest age groups for females during the first (+26.3%) and third (+42.3%) epochs of the pandemic, although highest for the youngest age male group (+30.2%) during the second epoch of the pandemic (i.e., Fall/Winter of 2020). In the fourth epoch, the youngest females demonstrated no significant increase in mortality (+1.28%), whereas their male counterparts experienced a 26.2% excess death rate. In the analyses of temporal trends, AMI-associated mortality rates decreased during the prepandemic epochs across all subgroups with significant declines seen for older females (−2.0% [95% CI: −3.1 to −1.0%]) and middle-aged (−0.7% [95% CI: −1.4 to −0.1%]) to oldest (−1.5% [95% CI −2.7 to −0.4%]) males (Supporting Information: Table S3); then, from before the start of the pandemic to the most recent pandemic epoch, these trends reversed with AMI-associated mortality rates increasing and significant rises seen for the youngest-aged females (5.6% [95% CI: 1.1%–10.4%]) and for the youngest (5.1% [95% CI: 1.0%–9.4%]) and middle-aged (3.2% [95% CI: 0.0–6.4]) males (Supporting Information: Table S3).
| Age-standardized Mortality Rate (Per 100 000 Persons) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prepandemic 4/2012–9/2012 | Pandemic epoch 1 4/2020–9/2020 | Pandemic epoch 2 10/2020–3/2021 | Pandemic epoch 3 4/2021–9/2021 | Pandemic epoch 4 10/2021–3/2022 | |||||||||
| Observed | Observed | Predicted [95% CI] | % Differencea | Observed | Predicted [95% CI] | % Differencea | Observed | Predicted [95% CI] | % Differencea | Observed | Predicted [95% CI] | % Differencea | |
| Females | |||||||||||||
| 25–44 | 1.11 | 1.23 | 0.97 [0.81–1.13] | +26.33% | 1.30 | 1.20 [0.94–1.45] | +8.12% | 1.37 | 0.96 [0.79–1.13] | +42.25% | 1.27 | 1.25 [0.90–1.60] | +1.28% |
| 45–64 | 11.01 | 11.71 | 9.42 [8.19–10.65] | +24.31% | 12.53 | 10.12 [8.99–11.24] | +23.77% | 11.96 | 9.01 [7.33–10.70] | +32.70% | 12.10 | 9.61 [8.07–11.16] | +25.88% |
| ≥65 | 104.33 | 83.26 | 73.57 [70.40–76.73] | +13.16% | 94.15 | 80.95 [71.67–90.22] | +16.31% | 80.91 | 69.89 [66.50–73.28] | +15.77% | 89.64 | 76.47 [66.54–86.41] | +17.23% |
| Males | |||||||||||||
| 25–44 | 2.71 | 2.94 | 2.42 [2.11–2.72] | +21.60% | 3.02 | 2.32 [2.02–2.62] | +30.21% | 3.14 | 2.39 [2.07–2.72] | +31.42% | 2.87 | 2.27 [1.95–2.59] | +26.24% |
| 45–64 | 28.46 | 29.40 | 23.75 [21.40–26.11] | +23.79% | 31.84 | 26.07 [25.31–26.82] | +22.12% | 29.62 | 21.20 [16.51–25.89] | +39.74% | 29.69 | 25.48 [24.67–26.28] | +16.52% |
| ≥65 | 163.55 | 141.48 | 125.60 [121.11–130.09] | +12.64% | 166.55 | 139.18 [126.16–152.20] | +19.66% | 137.78 | 121.17 [116.36–125.98] | +13.71% | 158.09 | 133.34 [119.39–147.29] | +18.56% |
- a % Difference between predicted and observed values.
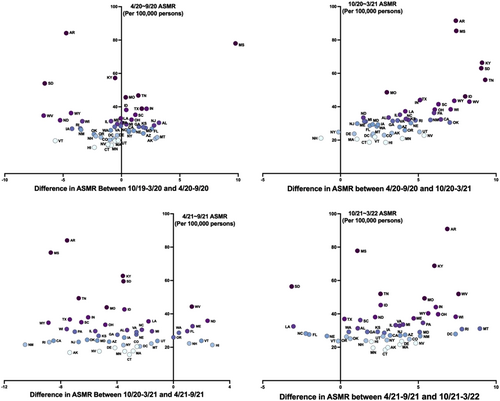
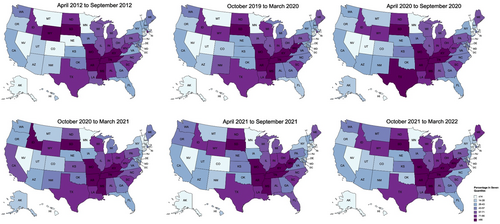
3.3 AMI-associated mortality by region
ASMRs increased from prepandemic to postpandemic epochs across the majority of states, particularly during the second and fourth epochs (Figure 4). The Southern United States experienced the highest rates of AMI-associated deaths during the COVID-19 pandemic between 4/2020–3/2022 (Figure 5). The individual states with the highest increase in the AMI-associated ASMR (per 100 000 persons) throughout the COVID-19 pandemic were Montana (12.5), Kentucky (11.0), West Virginia (10.5), and Mississippi (9.6) (Supporting Information: Table S4). In state-specific analyses during each epoch, Mississippi had the highest increase in AMI-associated death rate between 10/2019–3/2020 and 4/2020–9/2020. Tennessee, Kentucky, and South Dakota experienced the highest growth in AMI-associated death rates between 4/2020–9/2020 and 10/2020–3/2021 (Figure 4 and Supporting Information: Figure S4). Hawaii and North Dakota experienced the highest increase in ASMR for AMI-associated deaths between 10/2020–3/2021 and 4/2021–9/2021, while Montana and Rhode Island experienced the highest growth between 4/2021–9/2021 and 10/2021–3/2022.
4 DISCUSSION
From our temporal trends study of AMI-associated deaths across the United States, we observed several important findings. First, our results confirm that a substantial and significant increase in AMI-associated mortality across the population has emerged since the start of the COVID-19 pandemic. Importantly, this overall rise in AMI-associated mortality has effectively erased within 2 years what was previously a decade-long trend of steadily declining trend, with a majority contributed by non-COVID-19 conditions.6 Second, the excess in AMI-associated mortality has persisted throughout the pandemic, even during the most recent epoch marked by a surge of the presumed less-virulent Omicron variant, notwithstanding temporal variations in rates of non-COVID-19 versus COVID-19-associated mortality. Third, we found that although the increase in AMI-associated death rate during the pandemic was seen across all age groups, the relative rise was most significant among the youngest age group of 25–44 years old. The relative excess in AMI-associated deaths in youngest adults was seen initially in both sexes and then, during the fourth epoch marked by the Omicron surge, appeared to persist in younger males while somewhat improving in younger females.
Our findings extend from recent studies that have documented a substantial increase in cardiovascular morbidity experienced overall and particularly in traditionally high-risk subgroups such as older adults and males.4, 17 Our study expands from prior work by analyzing raw data collected over a longer period of time, comparing observed to predicted mortality rates, further stratifying sex groups by age, and accounting for known seasonal variation in AMI events. Furthermore, we focused on demographic comparisons to clarify how the accentuated and still widening disparities in excess mortality may be distinct from those relevant to morbidity. As shown in recent reports,18 the pandemic can augment absolute differences in outcomes in certain population subsets while augmenting relative differences in outcomes in others. Accordingly, we found that although older compared to younger adults continued to experience the greatest absolute magnitudes of excess AMI risk during the pandemic; younger adults experienced the greatest relative increase in excess AMI-associated mortality. Notably, the death rate increased more in males than females when considered in either absolute or relative terms, particularly during the fourth and most recent epoch. Importantly, even while AMI-associated mortality rates have recently overall improved along with trends in all-cause mortality during the pandemic, the relative disparity in excess AMI-associated deaths among certain at-risk subgroups such as younger-aged males has persisted.
There are several potential explanations for the increased AMI-associated mortality excess in patients with COVID-19.11, 19, 20 Typically, AMI and cardiovascular death typically do not present until years to decades after de novo development or worsening of pre-existing risk factors. However, SARS-CoV-2 infection may activate or accelerate the development of pre-existing subclinical coronary artery disease,21 which may be prevalent, particularly among younger-aged men with clustering of cardiometabolic risk factors.22 While de novo rapid development of AMI during or after SARS-CoV-2 infection is likely to be uncommon; such cases have been reported among individuals without known pre-existing cardiovascular risk traits—especially males affected by more severe forms of COVID-19 illness.23, 24 Proposed mechanisms for the thrombogenicity associated with SARS-CoV-2 infection include downregulation of angiotensin-converting enzyme 2(ACE-2), leading to dysregulation of the renin-angiotensin-aldosterone system, oxidative stress damage, endothelial cell dysfunction, and complement-mediated coagulopathy and microangiopathy.11, 23 Studies have consistently shown that males, independent of age, are more likely to develop more severe forms of SARS-CoV-2 infection than females.25 This male bias could have contributed to the predominance of excess AMI-associated mortality seen among males in our analyses. Psychological stressors associated with the pandemic may have also played a role in triggering events leading to excess AMI-associated mortality. Mental stress-induced ischemia has been shown to be associated with worse cardiovascular outcomes and disproportionately affects young women,25, 26 which could contribute to the excess of AMI-associated mortality seen among young females in our analyses.
Indeed, the effects of social distancing and stay-at-home mandates, reductions in outpatient visits and rehabilitation services, and deferment of elective procedures are all likely to have contributed to the overall excess of AMI-associated deaths during the COVID-19 pandemic.27-30 Importantly, however, we observed improved and yet persistent relative excess in AMI-associated deaths even as health delivery services have adapted to manage care during the most recent surge of the generally less virulent Omicron variant of SARS-CoV-2.
Several limitations of our study merit consideration. Our analyses were based on vital statistics data wherein the cause of death is subject to inaccurate documentation, leading to misclassification of AMI versus non-AMI-associated deaths. For this reason, we prioritized analyses of temporal trends while recognizing potential residual effects of misclassification bias. For subgroup samples with fewer events, particularly over shorter periods, model fit was suboptimal, resulting in wide confidence limits for some estimates. For all analyses, data associated to clinical characteristics, including cardiovascular risk factors and access to cardiovascular care resources, were not available. Therefore, additional studies are needed to investigate correlates and potential determinants of the trends in excess AMI-associated mortality found in our analyses of vital statistics.
5 CONCLUSIONS
Our study revealed that the excess rise in AMI-associated death occurring in the United States during the COVID-19 pandemic had been especially pronounced in younger than older adults, with a sex disparity that has become especially evident during the most recent fourth epoch marked by the Omicron surge. While a recent reduction in non-COVID-19-associated deaths suggests the efficacy of policies designed to curtail the impact of the pandemic, AMI-associated death rates remain in excess. Taken together, our results highlight disparities in mortality that have developed during the COVID-19 pandemic and are persistent through March 2022.
AUTHOR CONTRIBUTIONS
Study design and data analysis: Yee Hui Yeo, Xinyuan He, Fan Lv, Susan Cheng, Fanpu Ji. Drafting of the manuscript: Yee Hui Yeo, Maggie Wang, Xinyuan He, Susan Cheng, Fanpu Ji. Critical review of the manuscript: Jian Zu, Joseph E. Ebinger, Jignesh K. Patel, Susan Cheng. Study conception and study supervision: Susan Cheng, Fanpu Ji. All authors contributed to data interpretation, critical revisions, and approval of the final manuscript.
ACKNOWLEDGMENTS
This study was supported in part by Cedars-Sinai Medical Center and the Erika J. Glazer Family Foundation.
CONFLICTS OF INTEREST
Dr. S. Cheng has received consulting fees from Zogenix outside of the submitted work. Dr. F. Ji has received speaker fees from Gilead Sciences, MSD, and Ascletis, in addition to consulting or advisory board fees from Gilead and MSD, all outside of the submitted work. The remaining authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The NVSS can be accessed through this website: https://wonder.cdc.gov/mcd-icd10-provisional.html.




