The outbreak of monkeypox (MPX) in Ghana
During the prime of the 20th century, an infection similar to smallpox arose in humans called monkeypox (MPX). MPX is a zoonotic orthopoxviral infection caused by the monkeypox virus (MPXV) which belongs to the genus Orthopoxvirus and family Poxvirdiae. MPXV are ovoid or brick-shaped with sizes ranging from 200 to 250 nm and enclosed by folded lipoprotein outer membrane.1 MPXV contains a linear double-stranded deoxyribonucleic acid (DNA) of size 197 kb which is covalently joined by palindromic hairpins and inverted terminal repeats at its ends.2 MPXV appears in two distinct clades, the Central Africa clade and the West African clade with the Central Africa clade being more virulent, and transmissible.3 The diagnostic and confirmation techniques of MPXV include polymerase chain reaction (PCR), enzyme-linked immunosorbent assay (ELISA), tissue culture, and electron microscopy which depends on test availability.4
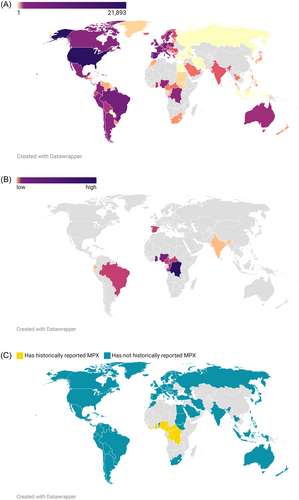
As of 12th September 2022, the World Health Organization (WHO) and Center for Disease Control and Prevention (CDC) reported a total of 57,016 MPX cases in 103 countries (Figure 1A) with 111 deaths5-7 (Figure 1B). Among these countries, 96 were nonendemic while seven were endemic countries (i.e., Ghana, Liberia, Nigeria, Cameroun, Central African Republic, Republic of Congo, and Democratic Republic of the Congo)6 (Figure 1C). A recent phylogenetic analysis of MPXV showed that the 2022 MPXV lineage B.1 shares a similar evolutionary branch as the A.1 lineage from Nigeria which caused the 2017-2018 MPX endemic outbreaks in the United Kingdom, Israel, and Singapore.8
MPX case was first recorded in 1970 from a 9-month-old boy in the Democratic Republic of Congo with subsequent reports in Benin, Cameroun, Gabon, Ivory Coast, Liberia, Nigeria, Sierra Leone, and South Sudan.9 Most of these cases presented similar symptoms such as fever, swollen lymph nodes, intense headache, myalgia, and asthenia. Previous reports showed that MPXV has an incubation period of 5–21 days with symptoms lasting between 2 and 4 weeks, however, this can exceed due to underlying health conditions which decrease patients' immunity.10 The fatality ratio of MPX disease ranges from ~3% to 6% with high severity experienced in children and pregnant women.11 Amidst these symptoms, the MPXV is transmitted either from animal to human or human to human. In the zoonotic transmission (animal to human), the MPXV uses vectors such as the rope squirrel, Gambian pouched rats, and different species of monkeys. Infection occurs when humans come into contact with infected body fluids, blood, or mucosal lesions of animals. In human-to-human transmission, infection can occur from a contact between respiratory secretions, skin lesions of an infected person or recently contaminated objects. A report by Thornhill et al.,12 revealed that among 528 patients with MPX in 16 countries, 98% of the patients were gays and 41% coinfected with the human immunodeficiency virus (HIV). A recent prospective observational cohort study in Spain showed that 166 (92%) of the 188 patients with MPX infection were either gay or bisexual men and 72 (40%) coinfected with HIV.13 In addition, Moschese et al. reported that all the 6 MPX patients had comorbidities such as HIV, hepatitis B virus (HBV), syphilis, gonorrhoea from unprotected sex.14 Having provided this context, this letter aims to highlight MPX case series in Ghana and how the government responded to the outbreak.
Ghana, a West African country recorded a series of the MPX disease on the 24th of May 2022. A report from the Minister of Health indicated that the outbreak began from a man who had recently traveled from the United States to Ghana with mild symptoms of MPX disease.15 The positive cases in Ghana as of 23rd July 2022 had increased to 34 with age ranging from 9 months to 45 years, mostly men. The Regions mostly affected are Greater Accra, Ashanti, Bono, Bono East, Eastern, Upper East, and Upper West.15, 16 As of 12th September, the suspected cases in Ghana were reported to be 87 with 76 confirmed and four death recorded.6 This shows an increase in cases in less than a month. Nonetheless, countries like the United Kingdom, Nigeria, the United States, Morocco, some European and Asian countries have also recorded cases of the MPX disease.6 A wildlife animal (Gambian rats, rope squirrels, dormice, sun squirrels) surveillance in Sogakope, Volta region, and Ada, Eastern region of Ghana showed the presence of antibodies against orthopoxvirus17 indicating the potential endemic circulation of MPXV in Ghana. Moreover, the traceback investigations of the MPX outbreak in Wisconsin, USA was linked to ~800 exotic animals (i.e., African rodents, prairie dogs) imported from Ghana.18, 19
Although the 2022 MPX cases in Ghana have not been high, various isolation centers were setup as it was done during the Coronavirus disease 2019 (COVID-19) outbreak. Infected patients are placed in these centers and treated with appropriate antivirals medications including smallpox vaccine as there is no specific treatment for MPX. The isolation takes 2 weeks, by then patient(s) would have recovered from the disease. Ghanaians have been frightened by the economic impact of Covid-19 on their livelihood, thus adhered to health practices to prevent the spread of MPX disease.20 A population-based cross-sectional study (n = 3259) showed that 45.9% of Ghanaian exhibited stigma and discriminatory tendencies toward COVID-19 survivors21 thus mass education is warranted to prevent similar ordeal against MPX patients. Such discrimination discourages patients from reporting to health centers for testing.
There is a debate in the Ghanaian media as to whether smallpox vaccine was effective against monkeypox22 because people vaccinated against smallpox were presumed to be immune to MPX.23, 24 However, a recent report showed that all the six MPX patients in Italy had medical history of smallpox vaccination in their childhood.14 This notwithstanding, the six MPX patients had different comorbidities such as HIV, HBV and SARS-CoV-2. Thus, thorough investigation is needed to decipher the role of smallpox vaccines in immunity against MPX.
Surprisingly not a single peer-reviewed publication about the MPX case series in Ghana has been reported, partly due to poor data collection and collaborations between the health professionals and researchers at the Universities, which followed a similar pattern during the COVID-19 outbreak.25 In addition, many health professionals lack the enthusiasm to prepare manuscripts about recorded case series for publication.25
Despite the measures put in place by the government of Ghana (GoG) to minimize the spread of MPX disease, the country still faces challenges regarding vaccines, equipment, and other facilities. WHO and other international bodies should support the GoG with vaccines and other medications required to curb the MPX outbreak since it is now declared as a Public Health Emergency of International Concern (PHEIC). Last, the citizens are advised to practice frequent handwashing with soap and water, encourage wearing of nose mask, practice safe sex, discourage overcrowding, eating bushmeat, and encountering wild animals.
AUTHOR CONTRIBUTIONS
Conceptualization: Parise Adadi. Writing—original draft: Emmanuel O. Mensah, Parise Adadi, and Salim Abdul-Razak. Writing—review and editing: Parise Adadi and Salim Abdul-Razak; All authors have read and agreed to the published version of the manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data are available on request from the authors.




