Prevalence of occult HBV among hemodialysis patients in two districts in the northern part of the West Bank, Palestine
Abstract
Occult hepatitis B infection is the case with undetectable HBsAg, but positive for HBV DNA in liver tissue and/or serum. Occult hepatitis B infection among hemodialysis patients in Palestine has been understudied. In this study, 148 hemodialysis patients from 2 northern districts in Palestine, Jenin (89) and Tulkarem (59), were investigated for occult hepatitis B, HBV, HCV infections with related risk factors. ELISA and PCR were used for the detection of anti-HBc and viral DNA, respectively. The overall prevalence of occult hepatitis B infection among the study group was 12.5% (16/128). Occult hepatitis B infection is more prevalent among males with most cases (15/16) from Jenin District. About one-third (42/132) of the hemodialysis patients were anti-HBc positive. Approximately 27% of the hemodialysis patients were infected with HCV. Around 20% (28/140) were positive for HBV DNA, but only 8.2% (12/146) of the hemodialysis patients were positive for HBsAg. The comparison between hemodialysis patients with occult hepatitis B infection and those without occult hepatitis B infection for selected risk factors and parameters as liver Enzyme, age, sex, HCV infection, blood transfusion, kidney transplant, anti-HBc, and vaccination showed no statistical significance between both categories. Duration of hemodialysis significantly affected the rate of HCV infection. HCV is significantly higher in hemodialysis patients with both Diabetes mellitus and hypertension. The prevalence of occult hepatitis B infection among hemodialysis patients is high; requiring stringent control policies. HBsAg assay is insufficient test for accurate diagnosis of HBV infection among hemodialysis patients. J. Med. Virol. 86: 1694–1699, 2014. © 2014 Wiley Periodicals, Inc.
INTRODUCTION
Hepatitis B virus (HBV) and hepatitis C virus (HCV) continue to be endemic in dialysis units despite the development of an effective HBV vaccine and the application of extensive infection control guidelines worldwide [CDC, 1988; Massari et al., 1998]. The prevalence of HBV and HCV infections in hemodialysis patients varies markedly from one country to another based on the prevalence of the these viruses in the selected country and infection control practices recommended for hemodialysis units [Alavian et al., 2008; Van Damme et al., 2012]. Furthermore, the low response rates to the HBV vaccine and the need for vaccine boosters among hemodialysis patients likely contributes to ongoing HBV transmission [Tokars et al., 1998, 2001]. Yet, the presence of occult HBV infection represents another possible explanation for ongoing transmission.
The data from the dialysis outcomes and practice pattern studies showed an HBV infection prevalence of 0–6.6% across dialysis units in Western Europe, Japan, and the USA [Burdick et al., 2003]. In contrast, in Asian/Pacific countries the prevalence of hepatitis B surface antigen (HBsAg) ranged from 1.3% to 14.6% [Yakaryilmaz et al., 2006]. Reports from other smaller studies have indicated HBsAg positivity rates of 13.3% in Turkey, and 2.4–10% in Brazil [Carrilho et al., 2004; Ferreira et al., 2006]. On the other hand, the HCV prevalence in hemodialysis patients ranges from 5% to 25% in the United States, 6.8% in Europe, and 0.7–18.1% in Asian/Pacific countries [Molino et al., 2008; Johnson et al., 2009].
Previously, Palestine, Egypt, Jordan, Oman, Yemen, and Saudi Arabia were considered as areas with intermediate to high endemicity for HBV ranging from 2% to 18.5% with highest prevalence, 18.5%, in Egypt [André, 2000]. Palestine and all of these Middle Eastern countries have reached hepatitis B vaccination coverage of over 80% of their population as part of their Expanded Programme on Immunization (EPI), which eventually reduced the infection rate. In these countries including Palestine, HBV infection is prevalent among hemodialysis patients ranging from 2% to 11.8% [Bdour, 2002; Almawi et al., 2004; Boulaajaj et al., 2005; Al Hijazat and Ajlouni, 2008; El-Ottol et al., 2010].
Occult HBV infection is defined as the presence of HBV DNA in the liver and/or serum with undetectable HBsAg with the available assays, and with or without the presence of HBV antibodies outside the acute phase window period [Allain, 2004; Raimondo et al., 2008; Bremer et al., 2009; Gerlich et al., 2010]. Globally, the prevalence of occult HBV infections among hemodialysis patients ranges from 0% to 58% [Cabrerizo et al., 2000; Fabrizi et al., 2005]. In studies from north American, Turkey, Egypt, Greece, and Iran, which also included HBsAg-negative hemodialysis patients regardless to their seropositivity, 3.8%, 9.8%, 26.9%, 0.9%, and 4.9% respectively, were HBV DNA positive [Minuk et al., 2004; Arababadi et al., 2009; Mina et al., 2010; Elgohry et al., 2012; Joukar et al., 2012; Keyvani et al., 2013].
Dialysis modality has been considered as a major risk factor for infection with HBV and HCV [Johnson et al., 2009]. Compared to the general population, this high prevalence in hemodialysis patients is due to increased exposure to blood and blood components during transfusion, shared hemodialysis equipment, as well as breaching of skin and immunodeficiency. These infections pose problems in the management of patients in the hemodialysis units, because end-stage renal disease (ESRD) patients do not clear these viral infections efficiently [EASL, ]. Recently, several studies had shown that HBV and HCV are still of the main complications in hemodialysis patients, which not only affect the quality of patients' lives, but also increase the mortality rate and decline the long-term survival rate following renal transplantation [Wang et al., 2010].
This aim of this study was to investigate the prevalence of occult HBV, HBsAg, and anti-HCV among hemodialysis patients in two northern districts in Palestine and to address the major risk factors of HBV transmission among these patients.
MATERIALS AND METHODS
Study Patients
This cross-sectional study was conducted in the period from September 2012 to September 2013. It included 148 patients on chronic hemodialysis from two Palestinian districts in the northern part of the West Bank. Serum was collected from patients prior to hemodialysis to evaluate the HBV serology (anti-HBc) and HBV DNA. Patient files in the two hemodialysis units were reviewed for the latest test results of the liver function tests; alanine amintotransferase (ALT), aspartate aminotransferase (AST), and alkaline phosphatase (ALP), HBV serology; HBsAg, and HCV serology; anti-HCV. The hemodialysis patients were interviewed to fill a questionnaire that included demographic data (age, sex, and place of residence) and the clinical history that focused on the duration of hemodialysis, blood transfusion, and frequency of hemodialysis per month, suspected causes of hemodialysis, kidney transplantation, and HBV vaccine. Patients were invited to participate in this study by an informed consent and an approval from the Ministry of Health in Palestine.
Anti-HBc Antibodies
Anti-HBc was measured in 132/148 (89.2%) of the available serum samples using an enzyme-linked immunosorbent assay (ELISA; Human Gesellschaft Fur Biochemica und Diagnostica, Wiesbaden, Germany) according to the manufacturer instructions.
HBV DNA Molecular Assay
Viral DNA was extracted from 200 µl of 140 serum samples, using the QIAamp viral DNA extraction kit according to the manufacturer instructions (Qiagen, Hilden, Germany).
The HBV-DNA was amplified using nested PCR with two primer sets targeting the viral polymerase gene described previously by Selabe et al. [2007]. In brief, the nested PCR was carried out as follows: In round one, a master mix of 2 µl of each primer, 1.25 µl dimethylsulfoxide (DMSO), and 17.75 µl of nuclease-free water was prepared in Ready Mix tube (Syntezza, Jerusalem, Israel). Two microliters of DNA templates were added. Amplification was carried out in Biorad C1000 thermal cycler. Amplicons (2 μl) from the first round were amplified using the internal primers, as described [Selabe et al., 2007] and the products from the second round electrophoresed on 2% agarose gels stained with ethidium bromide. The appearance of a 647-bp band was considered a positive result. Negative (nuclease-free water) and positive controls were used in each PCR assay.
Statistical Analysis
EPi Info™ free software from Centers for Disease Control and Prevention (CDC) was used for data analysis. Association between variables and groups was calculated using Fisher's exact test. Comparison between means of groups was calculated by Mann–Whitney test assuming non-Gaussian distribution. P-value smaller than 0.05 was considered statistically significant.
RESULTS
A total of 148 patients from 2 northern districts in Palestine, 89 patients from Jenin and 59 patients from Tulkarim, were included in the study. The age of the study group ranged from 14 to 82 years with a mean age of 49 ± 15 years. Seventy five percent were above 40 years old. About 60% (88/148) were males while 40% (60/148) were females. In this study, occult hepatitis B case was defined as negative for HBsAg by ELISA, but at the same time positive by PCR for HBV-DNA (polymerase gene). The overall prevalence of occult hepatitis B infection among hemodialysis patients was 12.5% (16/128) with male showing more tendency to occult infection than female (Fig. 1). Majority of occult hepatitis B cases were from Jenin city (15/16). Of the 132 hemodialysis patients tested for anti-HBc, 31.8% (42) were found to be positive. Approximately 27.4% of the hemodialysis patients suffered from HCV infection, and only 2% (3/148) had co-infection with HBV and HCV. Twenty-eight out of 140 were positive for HBV-DNA by PCR (20%), while 8.2% (12/146) of hemodialysis patients were positive for HBsAg when tested by ELISA. The latter is considered overt or chronic HBV infection. Of the 130 hemodialysis patients with reported causes of ESRDs, 70.7% were found be due to Diabetes mellitus and/or hypertension.
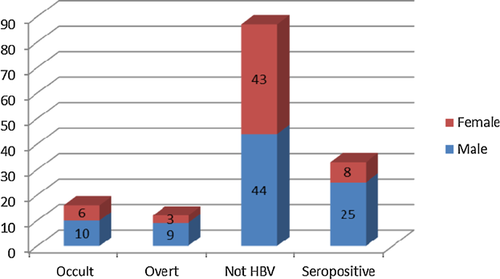
Statistical analysis of the risk factors related to occult hepatitis B infection in the study patients included Liver enzymes profile, age, sex, HCV infection, blood transfusion, kidney transplant, anti-HBc, and vaccination. Liver enzymes were considered abnormally high if values ≥1.5-fold the normal value; 17, 24, and 120 U/L for ALT, AST, and Alkaline phosphatase, respectively, as indicated by the manufacturer's kit leaflet. No correlation between liver enzyme values and the presence of occult hepatitis B infection was observed (Table I). Table II shows the results obtained for each test used in the study, HBsAg, anti-HBC, anti-HCV, PCR, and HBV-HCV co-infection versus factors that may have potential influence on the binomial outcome of these tests. No relation between age of hemodialysis patients and any of the tests, expect for the presence of anti-HBC antibodies that were borderline (P = 0.07). Significantly more males gave positive anti-HBc tests than females (P = 0.01), and males were approximately three times more likely to show anti-HBc positive results. Duration of hemodialysis significantly affected the rate of HCV infection in hemodialysis patients (P < 0.0001). The longer the duration of hemodialysis (70.1 ± 47.9 months), the more prone patient is to HCV infections, while those on hemodialysis less than 33.9 ± 24.3 months were free from HCV infection. The frequency of hemodialysis per months was close to statistical significance of attracting HCV infection (P = 0.09), but did not affect the outcome of the rest of tests. Diabetes mellitus and hypertension together, were significantly higher in hemodialysis patients with HCV infection (P = 0.01) and close to significance in affecting outcome of PCR test and HBV-HCV co-infection.
| Parameter | OHB+ | OHB− | P-value | Stat. Sig. |
|---|---|---|---|---|
| Sex | ||||
| Male | 9 | 53 | 1.0 | No |
| Female | 6 | 46 | ||
| Age (years) | ||||
| ≥14 | 0 | 2 | 1.0 | No |
| >14 | 16 | 123 | No | |
| ALT (U/L) | ||||
| High | 7 | 52 | 0.79 | No |
| Normal | 9 | 80 | ||
| AST (U/L) | ||||
| High | 5 | 30 | 0.53 | No |
| Normal | 11 | 102 | ||
| ALKP, U/L | ||||
| High | 9 | 68 | 0.79 | No |
| Normal | 7 | 65 | ||
| Anti HBC | ||||
| Positive | 5 | 37 | 1.0 | No |
| Negative | 11 | 79 | ||
| Anti HCV | ||||
| Positive | 6 | 34 | 0.38 | No |
| Negative | 10 | 96 | ||
| Blood transfusion | ||||
| Yes | 16 | 117 | 0.58 | No |
| No | 0 | 9 | ||
| Kidney transplant | ||||
| Yes | 1 | 8 | 1 | No |
| No | 15 | 118 | ||
| Vaccine | ||||
| Yes | 16 | 122 | 1 | No |
| No | 0 | 5 | ||
| Parameter | HBsAg | Anti-HBC | Anti-HCV | HBV-PCR | HCV-HBV | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative | |
| Age (years) | 54.3 ± 14 | 48.9 ± 15.4 | 53.8 ± 13.3 | 47.2 ± 15.6 | 47.8 ± 14.5 | 50 ± 15.6 | 49.6 ± 15.6 | 49.2 ± 49.2 | 48.7 ± 10.2 | 49.5 ± 15.4 |
| P-value | 0.22 | 0.07 | 0.29 | 0.70 | 0.85 | |||||
| Sex | ||||||||||
| Male | 9 | 77 | 33 | 49 | 23 | 63 | 19 | 65 | 2 | 68 |
| Female | 3 | 57 | 9 | 41 | 17 | 43 | 9 | 47 | 1 | 59 |
| P-value | 0.36 | 0.01 | 0.85 | 0.33 | 0.99 | |||||
| Duration on HD (months) | 43.6 ± 28.9 | 43.5 ± 36.1 | 48.6 ± 46.6 | 41.8 ± 31.3 | 70.1 ± 47.9 | 33.9 ± 24.3 | 54.8 ± 47.7 | 40.5 ± 33 | 61.3 ± 19 | 42.6 ± 35.7 |
| P-value | 0.67 | 0.90 | <0.0001 | 0.11 | 0.08 | |||||
| Frequency of HD | 9.7 ± 2.7 | 10.0 ± 2.1 | 10.3 ± 2.2 | 10.1 ± 2.1 | 10.6 ± 1.9 | 9.8 ± 2.2 | 9.9 ± 2.4 | 10.1 ± 2.1 | 10.7 ± 2.3 | 10 ± 2.2 |
| P-value | 0.74 | 0.50 | 0.09 | 0.77 | 0.61 | |||||
| Causes | ||||||||||
| DM/HTN | 6 | 86 | 28 | 53 | 18 | 78 | 10 | 76 | 0 | 96 |
| Others | 5 | 33 | 7 | 27 | 14 | 20 | 8 | 24 | 2 | 32 |
| P-value | 0.29 | 0.18 | 0.01 | 0.08 | 0.06 | |||||
- Mean ± SD. DM, diabetes mellitus; HTN, hypertension; HD, hemodialysis patients.
DISCUSSION
Blood-borne viruses, particularly HBV and HCV, are considered a major hazard for both patients and health staff in hemodialysis facilities worldwide [Feher and Ambuhi, 2004]. During the last decade, several studies showed that the implementation of universal screening tests including HBsAg for HBV and Anti HCV for HCV and the widespread implementation of HBV vaccination have significantly reduced the prevalence of the viral hepatitis, particularly HBV [Köhler, 1994; Feher and Ambuhi, 2004]. Despite all these precautions, outbreaks of HBV infection continue to occur in hemodialysis facilities and the prevalence rates of HBV and HCV remain unacceptably high [Edy et al., 2010].
In the Palestinian normal population, the prevalence of HBV is 1.8% while its 0.2% for HCV [Palestinian Health Information Center, 2005]. In this study, the prevalence of overt HBV (HBsAg positive) and HCV infection in hemodialysis units in the two northern Palestinian districts, Jenin and Tulkarem was shown to be 4.5 and 137 times higher than in normal population, respectively (8.2% vs. 1.8 for HBV and 27.4% vs. 0.2 for HCV). Furthermore, the present study showed that the HBV-DNA was detected in 28 of 140 (20%) of the hemodialysis patients, including 16 of 128 (12.5%) with occult HBV infections. Interestingly, only 12 (42.8%) of the 28 HBV-DNA positive patients were also HBsAg positive. This leads us to conclude that the detection of HBV in serum samples of hemodialysis patients using HBsAg assay underestimates the true prevalence of HBV infection. This finding is further supported by recent studies, which assessed the true rate of HBV infection and occult hepatitis B infection in hemodialysis patients using highly sensitive PCR method (HBV-DNA) targeting different genes [Minuk et al., 2004; Siagris et al., 2006; Yakaryilmaz et al., 2006; Mina et al., 2010; Elgohry et al., 2012; Keyvani et al., 2013].
The data of the current study showed that occult HBV infection was common among hemodialysis patients (12.5%). This prevalence is lower than that found in Egypt (26.8%) and southern Greece (20.4%), but higher than in Turkey (2.7%), central Greece (0.9%), central Canada (3.8%), and Iran (4.9%) [Minuk et al., 2004; Siagris et al., 2006; Goral et al., 2006; Yakaryilmaz et al., 2006; Mina et al., 2010; Elgohry et al., 2012; Joukar et al., 2012; Keyvani et al., 2013]. The wide range of occult hepatitis B infection prevalence among hemodialysis patients worldwide in general, and the high variation in prevalence between the two hemodialysis units in this study (15 occult hepatitis B cases from Jenin and 1 case from Tulkarim) could be attributed to several factors including the sensitivity and specificity of the PCR assay, characteristics of study population, and the difference in geographical endemicity of HBV infection. In 2012, the total number of reported HBV infections, cases and carriers, was 36 in Tulkarim compared to 65 cases in Jenin [Palestinian Health Information Center, 2012]. This explains partly the increased prevalence of the HBsAg positive cases among hemodialysis patient from Jenin District (9%) relative to that of Tulkarim (6.8%). Another plausible explanation for this variation is the difference in the degrees of implementation of universal precautions taken in each of the two investigated hemodialysis units.
The prevalence of anti-HBc positive cases among the hemodialysis patients is relatively high (31.8%). However, it is lower than in Greece (48%) and Turkey (44.7%), but higher than Iran (10.13–13%) [Yakaryilmaz et al., 2006; Mina et al., 2010; Ramezani et al., 2010; Joukar et al., 2011]. Since anti-HBc positivity indicates previous exposure to HBV infection, such finding might suggest previous contact with HBV during adulthood, though it cannot be safely ascertained if this has taken place in an hemodialysis facility or not. Furthermore, such data reflect a high HBV endemicity in our study hemodialysis patients as well as in those in other countries like Turkey and Greece. In this study, the one-third anti-HBc positive was split equally between the occult hepatitis B positive (5/42, 11.9%) and occult hepatitis B negative (11/79, 13.9%) groups indicating the absence of any diagnostic value of anti-HBc in the overall diagnosis of occult hepatitis B infection. This is in agreement with several previous studies that showed the absence of any statistical significant difference between the occult hepatitis B infection among hemodialysis patients with positive anti-HBc test and those with negative results [El-Sherif et al., 2009; Mina et al., 2010, Ramezani et al., 2010; Keyvani et al., 2013]. This could be attributed to false positive results for anti-HBc, degree of endemicity of HBV, and the nature of study population. Therefore, despite the high number occult hepatitis B cases with anti-HBc positive and the recommendations raised by several investigators to use anti-HBc as a surrogate of PCR assay, yet high number of occult hepatitis B negative for anti-HBc still exists [Yakaryilmaz et al., 2006; Keyvani et al., 2013].
The rate of anti-HCV positive among the hemodialysis patients in this study is extremely high (27.4%) with increased variation between the two districts (6.8% in Tulkarim 41.3% in Jenin). Again and as in HBV infection, the endemicity of HCV in the general Palestinian public is widely variable between the two areas with only two reported carriers in Tulkarim compared to 16 in Jenin [Palestinian Health Information Center, 2012]. This result is comparable with the rate of HCV among hemodialysis patients in Jordan (28%) [Al-Jamal et al., 2009], but higher than in southern districts of Palestine (Gaza) (17.9%) [El-Ottol et al., 2010] and Greece (24%) [Mina et al., 2010]; yet, lower than in Egypt (35%) [Khodir et al., 2012]. In general, this difference in the prevalence of HCV between hemodialysis centers could be again attributed to the geographical HCV endemicity and to the degree of commitment to safety precautions taken in each hemodialysis facility.
In this study, 6 of the 40 (15%) anti-HCV positive hemodialysis patients were occult hepatitis B cases (HBV DNA positive). On the other hand, 10 of the 106 (9.4%) of anti-HCV negative hemodialysis patients were occult hepatitis B cases (HBV DNA positive). Such a data runs parallel with the rate of occult hepatitis B infection (14.2%) among hemodialysis patients with chronic HCV infection in one study in Turkey [Kanbay et al., 2006]; but lower than in another Turkish study that showed a significant number of occult hepatitis B cases (36.4%) among hemodialysis patient with chronic HCV [Besisik et al., 2003]. Siagris et al. [2006] found a significantly high number of occult hepatitis B cases (20.4%) in hemodialysis patients with chronic HCV compared to a lower rate of occult hepatitis B infection (6.3%) among HCV-infected but otherwise normal patients (none-hemodialysis). Therefore, despite the significant number of occult hepatitis B cases among hemodialysis patients with chronic HCV infections, HCV could not be considered a contributing factor to occult HBV infection in hemodialysis patients.
Overall, age, sex, duration of hemodialysis, frequency of hemodialysis and blood transfusion, biochemical parameters (ALT, AST and alkaline phosphatase), anti-HBc, anti-HCV, and vaccination did not show any statistically significantly difference in patients with and those without occult hepatitis B infection. Such data in this study are in agreement with several previous ones on hemodialysis patients which also failed to establish any statistically significant relationship in the aforementioned parameters between patients with occult hepatitis B infection and those without occult (overt) hepatitis B infection [Siagris et al., 2006; El-Sherif et al., 2009; Mina et al., 2010; Motta et al., 2010].
In conclusion, the prevalence of occult hepatitis B infection among hemodialysis patients is high. This study showed that HBsAg assay is not sensitive enough to give accurate diagnosis of HBV infection among hemodialysis patients as it leads to underestimation of the prevalence of HBV. Furthermore, anti-HBc, duration of hemodialysis, frequency of blood transfusion, levels of liver enzymes, and rate of HCV infection are not risk factors and do not help to distinguish between hemodialysis patients with and without occult hepatitis B infection.
ACKNOWLEDGMENT
We thank Mrs Hanan Al-Jawabreh of the LRU-Jericho who helped to organize molecular biology work.