Introducing fitting models for estimating age-specific dose and effective dose in paediatric patients undergoing head, chest and abdomen–pelvis imaging protocols: a patient study
Abstract
Introduction
Concerns regarding the adverse consequences of radiation have increased due to the expanded application of computed tomography (CT) in medical practice. Certain studies have indicated that the radiation dosage depends on the anatomical region, the imaging technique employed and patient-specific variables. The aim of this study is to present fitting models for the estimation of age-specific dose estimates (ASDE), in the same direction of size-specific dose estimates, and effective doses based on patient age, gender and the type of CT examination used in paediatric head, chest and abdomen–pelvis imaging.
Methods
A total of 583 paediatric patients were included in the study. Radiometric data were gathered from DICOM files. The patients were categorised into five distinct groups (under 15 years of age), and the effective dose, organ dose and ASDE were computed for the CT examinations involving the head, chest and abdomen–pelvis. Finally, the best fitting models were presented for estimation of ASDE and effective doses based on patient age, gender and the type of examination.
Results
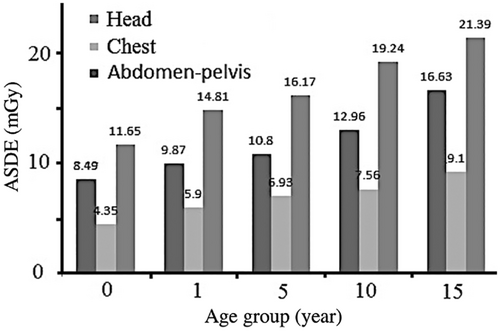
The ASDE in head, chest, and abdomen–pelvis CT examinations increases with increasing age. As age increases, the effective dose in head and abdomen–pelvis CT scans decreased. However, for chest scans, the effective dose initially showed a decreasing trend until the first year of life; after that, it increases in correlation with age.
Conclusions
Based on the presented fitting model for the ASDE, these CT scan quantities depend on factors such as patient age and the type of CT examination. For the effective dose, the gender was also included in the fitting model. By utilising the information about the scan type, region and age, it becomes feasible to estimate the ASDE and effective dose using the models provided in this study.
Introduction
Over the past two decades, use of computed tomography (CT) has increased and one of its important consequences is increasing of radiation exposure for nearly 50% of the total collective dose (person-Sieverts) to the population.1 Although CT greatly has enhanced diagnostic abilities, its ionising radiation dose is 100–500 times more than conventional radiography.2 This becomes concerning when we take into account the annual increase in the number of CT examinations for both children and adults. For instance, in the United States, this number experienced a 10% annual rise from 1993 to 2011.3 Consequently, there is an urgent need for increased attention to this matter, especially in the context of paediatric and younger patients. Radiation deterministic effects occur following receive of relatively high radiation doses, and these effects have been encountered in interventional radiology and in CT studies.4 This trend is mirrored in other developed and developing countries as well.5
The concerns about increased radiation risk hold greater significance in children due to their heightened radiosensitivity6 and extended lifetimes, which could potentially magnify long-term radiation effects.7 In such cases, the precise quantification of patient dose becomes a critical task to assess radiation risks stemming from the escalating number of CT scans, particularly among paediatric patients.8 In this sense, the recommendation of the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) is to avoid using the same generalisations for the radiation risks and effects for both adults and children.9 Calculation of dosimetric quantities on patient doses from CT examination for children has been an active area of research.10-13
To determine CT radiation exposure, CT dose index (CTDI) has been introduced.14 Essentially, the CTDI value is used to evaluate the average dose to patients resulting from a specific CT scan, and this value is represented as the volume-averaged CTDI (CTDIvol). The CTDIvol indicates the differences in dose between scan protocols and different scanners.15 Moreover, when CTDIvol combines with the scan length it forms the dose length product (DLP), which is linked to effective doses.10, 16 Here, both DLP and CTDIvol are the most useful parameters for comparing the received radiation doses from particular protocols of scanning or examination and the biological risk they have to the patient.3 It is worth mentioning, CTDIvol does not consider the patient's size and is not absorbed dose to organs of the patient.
The CTDI (and consequently CTDIvol and DLP metrics) is influenced by scan parameters such as tube current-, tube voltage-, pitch-, collimation- and scanner-dependent factors such as gantry diameter, filtration and tube current modulation. These quantities are useful metrics to evaluate and compare relative patient dose to diagnostic reference levels.17 However, CTDI is obtained via dosimetry in a cylindrical phantom geometry and is not a metric that could estimate the patient-specific dose quantities. Due to patient shape and size difference, the above metrics are not sufficient to accurately estimate the actual patient dose. Specifically, the doses of patients smaller than the standard acrylic phantoms are underestimated.18-20 This leads to an underestimation of the dose for average-sized adults and paediatric by 40–70%.21 To address this concern, conversion factors to acquire size-specific dose estimates (SSDEs) for specific patients have been suggested.15, 22 The SSDE is introduced to set the CTDIvol to show the effect of sizes of the patients on the average radiation dose, particularly for overweight patients with larger sizes and paediatric patients with smaller sizes.23, 24 The approaches and recommendations of calculating the SSDE have been updated in a later report;25 however, its accuracy in estimating individual organ dose has been limited.3, 19 The inclusion of SSDE information is thought to be an updated method for estimation of patient dose from CT examination.
There are two methods for estimating a patient's organ dose from CT examinations. The first is experimental measurement of dose through the use of physical anthropomorphic phantoms and a dosimeter. The second is software calculations of dose using computational phantoms and Monte Carlo simulation techniques.2, 10, 11, 26, 27 The use of the Monte Carlo method can provide the closest estimate for patient dosimetry, which is commonly considered the gold standard in dosimetry techniques. Recent studies have examined the relationship between SSDE and organ dosimetry in adults, presenting a timely and accurate approach to CT patient dosimetry.28, 29 The outcomes of these studies show that by using SSDE it may be possible to create a simple method for patient-specific dosimetry in CT by employing organ dose estimations.30 The aim of the presented work is to introduce fitting models for estimation of SSDE respect to age of patient which we name it age-specific dose estimates (ASDE) and effective dose from patient age, gender and examination type in paediatric head, chest and abdomen–pelvis CT examinations.
Method
Research ethics approval was obtained from Shahid Beheshti University of Medical Sciences (IR.SBMU.MSP.REC.1395.399).
Patient data and CT scanning protocol
In this study, 583 children underwent three different CT examinations, head, chest and abdomen-pelvic, were included in the evaluations. The patients were categorised into five age groups (Table 1), allowing their data to be input into the ImPACT software (version 2.3, PHE Company, London, UK).31
| Group number | Age range |
|---|---|
| 1 (0 y/o) | Birth to ≤3 months (0-year-old patients) |
| 2 (1 y/o) | >3 months to ≤2 y/o and 6 months (1-year-old patients) |
| 3 (5 y/o) | >2 y/o and 6 months ≤7 y/o and 6 months (5-year-old patients) |
| 4 (10 y/o) | >7 y/o and 6 months ≤12 y/o and 6 months (10-year-old patients) |
| 5 (15 y/o) | >12 y/o and 6 months ≤15 y/o (15-year-old patients) |
- y/o, years old.
Data were acquired at high speed using a 16-slice multidetector GE Lightspeed CT scanner. Scanning conditions including type of CT examination, tube voltage, tube current × rotational time (mAs), pitch, interval, slice thickness, number of slices and number of patients for different age groups are presented in Table 2. Based on this table, it is clear that the scanning conditions were adjusted based on the type of examination and age group. Within each age group and examination, the slice thickness remained consistent across all patients, but the number of slices was changed depending on the patient size. For the abdomen–pelvis CT examination, a 7.5-mm slice thickness was selected, as this setting necessitates less detail and contributes to lower patient doses. Patients were selected randomly; however, there was an effort to ensure adequate sample sizes in all age groups. Being randomised the selection of the patients means that there was not any preference in selection of the patients. The selection criteria considered factors such as the target organ for imaging, patient size, scanner capabilities and standard imaging practices. Table S1 in the Supporting Information indicates the application of tube voltages of 100, 110 and 120 kVp for both male and female patients. No tube current modulation was implemented during the CT scans, but the tube current and rotational time were selected based on the CT examination and patient conditions (age and size).
| Protocol | A | B |
|---|---|---|
| Abdomen–pelvis | 0.49 | 8.66 |
| Chest | 0.27 | 5.09 |
| Head | 0.59 | 13.01 |
The length, width and depth of patients' scanned body regions were read by using the measurement utility tool of the CT console. Information on tube voltage, tube current × rotation time, inclination, movement of the table in the axial position, and so on can be obtained from the main screen of the console and was recorded using the DICOM recording system.
Age-specific dose estimate calculation
It is worth mentioning that SSDE is indeed not an organ-specific quantity. It represents an estimate of the radiation dose that accounts for patient size while considering the entire body rather than individual organs. The rationale behind incorporating organ-specific parameters is to provide a comprehensive analysis of the potential radiation exposure in different regions of the body.
Effective dose, DLP and organ dose calculations
Continuing with the workflow, the next step involved by entering the scanning conditions to conveniently calculate effective dose, DLP and organ dose values. The definition of effective dose is based on organ doses and tissue weighting factors from the ICRP publication 103.33 In this study, effective dose was calculated by the ImPACT software by entering the imaging conditions into the software. For introducing CTDIvol for the head protocol a 16-cm phantom and for the other CT examinations, a 32 -cm-diameter phantom was selected in the ImPACT software.
Results
In this section, both effective dose and DLP were tabulated for head, chest and abdomen–pelvis scans with tube voltages of 100, 110 and 120 kVp for male and female patients. Head scans were performed in 162 of the total 583 patients participating in the study CT (males = 77, females = 85), chest scans in 206 CT (males = 89, females = 117) and abdomen–pelvis scans in 215 CT (males = 111, females = 104).
Age-specific dose estimate results
The results of the coefficients obtained from the fitting of ASDE (at same direction of SSDE) to the age are presented in Table 2.
The size-specific dose estimation for both male and female in different age groups was calculated for abdominal–pelvic, chest and head CT examinations. ASDE (mGy) versus age group for head, chest and abdomen–pelvis CT examinations is presented in Figure 1.
In Table 3, the results of ASDE range, average value and the standard deviation for different examination in all CT scans for the five age groups presented.
| Protocol | Age (years) | Median mGy | Range mGy | Standard deviation |
|---|---|---|---|---|
| Abdomen–pelvic | 0 y/o | 8.49 | 6.11–10.93 | 1.14 |
| 1 y/o | 9.87 | 7.21–12.42 | 1.23 | |
| 5 y/o | 10.8 | 7.93–13.23 | 1.51 | |
| 10 y/o | 12.96 | 9.85–15.73 | 1.19 | |
| 15 y/o | 16.63 | 13.39–19.76 | 1.25 | |
| Chest | 0 y/o | 4.35 | 2.53–5.18 | 0.97 |
| 1 y/o | 5.90 | 3.86–6.97 | 1.17 | |
| 5 y/o | 6.93 | 4.72–8.21 | 1.54 | |
| 10 y/o | 7.56 | 5.17–9.24 | 1.35 | |
| 15 y/o | 9.13 | 6.69–10.87 | 1.12 | |
| Head | 0 y/o | 11.65 | 8.23–13.79 | 1.85 |
| 1 y/o | 14.81 | 11.18–16.95 | 1.13 | |
| 5 y/o | 16.17 | 12.37–19.24 | 1.97 | |
| 10 y/o | 19.24 | 16.02–22.71 | 1.41 | |
| 15 y/o | 21.39 | 19.66–23.97 | 1.96 |
- y/o—years old.
According to the results for each scanned region (abdominal–pelvic, chest and head) provided in the above table, we found the best fit for the data compared to different ages. ASDE (which is at the same concept as SSDE) can be calculated based on patient age (eq. 1 in the Methods section) using coefficients A and B, whose values for head, chest and abdomen–pelvis imaging protocols are presented in Table 3.
Effective dose and DLP results
The results of the coefficients obtained from the fitting of effective dose to the age are presented in Table 4.
| Protocol | Sex | a | b | c | d |
|---|---|---|---|---|---|
| Abdomen–pelvis | Male | 2.25 | −3.02 | 11.18 | −0.035 |
| Female | 2.35 | −1.97 | 11.11 | −0.031 | |
| Chest | Male | 41.85 | −37.16 | 2.08 | 0.030 |
| Female | 1.38 | −2.50 | 2.12 | 0.031 | |
| Head | Male | 0.97 | −0.59 | 3.04 | −0.053 |
| Female | 1.02 | −0.66 | 3.18 | −0.048 |
Table 5 lists the mean, range and standard deviation of the effective dose, and the DLP data for abdomen–pelvis for male and female patients on five age groups. The other related tables list same parameters of the effective dose (Table S2) and the DLP data (Table S3) for head, chest and abdomen–pelvis CT examinations for male and female patients on five age groups than can be found under the Supporting Information. The results for effective dose for head CT examination show that using the head size for calculation of effective dose results in a higher conversion coefficient. Effective dose (mSv) versus age group for head, chest and abdomen–pelvis CT examinations for male and female patients is presented in Figure S1 under the Supporting Information. Exponential coefficients for calculation of effective dose (eq. 2) for head, chest and abdomen–pelvis CT examinations are presented in Table 4.
| Age | Median | Range | Standard deviation | Number of patients |
|---|---|---|---|---|
| Male | ||||
| 0 y/o | ||||
| Effective dose (mSv) | 12.8 | 10.3–13.3 | 1.01 | 12 |
| DLP (mGy-cm) | 261 | 208–327 | 49.34 | 12 |
| 1 y/o | ||||
| Effective dose (mSv) | 10.9 | 8.3–12.1 | 0.93 | 15 |
| DLP (mGy-cm) | 263 | 290–617 | 98.21 | 15 |
| 5 y/o | ||||
| Effective dose (mSv) | 9.1 | 4.8–12 | 1.09 | 21 |
| DLP (mGy-cm) | 607 | 310–825 | 127.37 | 21 |
| 10 y/o | ||||
| Effective dose (mSv) | 8.5 | 6.1–10 | 0.81 | 20 |
| DLP (mGy-cm) | 425 | 314–540 | 62.42 | 20 |
| 15 y/o | ||||
| Effective dose (mSv) | 6.1 | 3–9.9 | 1.12 | 23 |
| DLP (mGy-cm) | 413 | 220–923 | 182.41 | 23 |
| Female | ||||
| 0 y/o | ||||
| Effective dose (mSv) | 13 | 10.1–14.9 | 1.35 | 9 |
| DLP (mGy-cm) | 283 | 212–319 | 51.29 | 9 |
| 1 y/o | ||||
| Effective dose (mSv) | 11.1 | 9.3–14 | 1.47 | 17 |
| DLP (mGy-cm) | 361 | 301–628 | 86.52 | 17 |
| 5 y/o | ||||
| Effective dose (mSv) | 9.3 | 6.9–12.8 | 1.53 | 22 |
| DLP (mGy-cm) | 618 | 310–825 | 147.31 | 22 |
| 10 y/o | ||||
| Effective dose (mSv) | 8.7 | 6.2–11.4 | 1.11 | 19 |
| DLP (mGy-cm) | 439 | 331–572 | 73.17 | 19 |
| 15 y/o | ||||
| Effective dose (mSv) | 6.7 | 4.4–8.16 | 1.41 | 18 |
| DLP (mGy-cm) | 408 | 247–997 | 152.14 | 18 |
Organ dose results
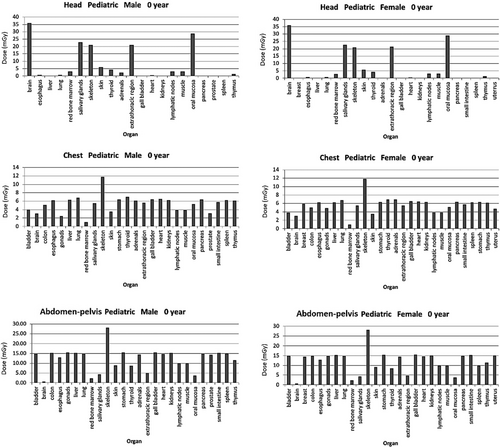
Here, in Figure 2 the organ dose (mGy) for head, chest and abdomen–pelvis CT examinations for male and female genders based on one age groups (0 year age) is presented. The figures for the other age groups are presented in the Figures S2–S5 (see Supporting Information).
Discussion
The SSDE has been the primary focus of several recent studies, since CTDI cannot correspond to patient dose in the CT examinations.35, 36 In the current study, all data were concluded scripting in MATLAB, and simple and user-friendly models were proposed to calculate ED and ASDEs using patients age and scan protocols. In the present study, fitting models were presented for estimation of ASDE and effective dose from patient age, gender and CT examination type in paediatric head, chest and abdomen–pelvis CT examinations for paediatrics population of 583 patients.
Abdominal–pelvic CT scan
Our result suggested that an increase in the age of patients, both females and males, leads to a decline in their effective dose. As shown in Figure S1 in Supporting Information, the increase of age results in decline of effective dose in abdominal–pelvic CT scans. Also, absorbed dose in the organ is reduced by an increase in the age of patients. Since body size usually increases with age, the organ doses are influenced, and the results of this study indicated a noticeable decrease. In the aforementioned section, the effect of body size on the effective dose was discussed. Despite their small body size, the effective dose is higher in newborns than in older children. As children age increases, the body size increases and the effective dose decreases. This may be due to decrease of sensitivity with age, although the ICRP report number 10333 tissue weighting factors used by ImPACT software in calculation of effective dose are age-averaged, and no age-specific sensitivity was reported in such factors. The organ sensitivity normally shows its effect on the effective dose by including the tissue weighting factors in the calculations.33 This point should be also noted that the ICRP report 103 factors used by ImPACT software used for calculation of effective dose are age-averaged factors; therefore, this figure of age-specific effective dose cannot reflect age-specific risk per unit dose, but rather the effect of other factors such as examination conditions, patient size and organ development stage differences.
A study by Thomas et al.37 suggested that increased age results in reduced organ-absorbed dose; however, it reached a peak at age 10 years and then at age 15 years decreased again. In our study, the decrease in organ-absorbed dose continued. Note that effective dose was the same in both studies. Our results were consistent with a study by Houda et al.;21 nevertheless, he suggested lower effective dose for children of all ages. A study by Theocharopoulos et al.38 revealed the same results, but for some cases, the recorded dose was lower than that of our study. In this study, dose of females is slightly higher than that of males. Here, SSDE increases in accordance with age as shown in Figure 1. SSDE of newborns, 1-year-olds, 5-year-olds, 10-year olds and 15-year-olds were 8.49, 9.87, 10.8, 12.96 and 16.63, respectively. This increase is in accordance with the findings of AAMP report no. 204.32 It should be noticed that while SSDE has the same basic definition in different reports, there are different calculation methods for its calculation in different studies. The differences in the SSDE values and the trends from this study and other studies may be due to the differences in the calculation methods. Most of the previous studies on calculation of SSDE are based on size and CTDIvol, while the method used in this study is based on multiple factors, which deviate from the definition of SSDE.
Chest CT scan
The current study suggested that an increase in the age of patients from 0-year-olds to 15-year-olds first leads to a decline in the effective dose of both females and males, and then, the dose increases again. In fact, the lowest level of effective dose belonged to the 1-year-old group. The results are shown in Figure 1 and Figure S1 in Supporting Information. The ImPACT software used consistently calculated higher effective doses for females than for males. The high level of effective dose in newborns is due to their sensitivity; despite their small body size, their effective dose is high. This suggests that, in the effective dose, sensitivity is more important than the body mass exposed to radiation. With age, sensitivity decreases; however, body size affects the amount of organ-absorbed dose and effective dose. Since body size increases with age, body size plays a more important role from 1 to 2 years of age, so that the effective dose increases. As the body size is changed, the distances of the organs from the imaging region are changed; therefore, the organ doses are changed. By the change in the organ doses, the effective dose is affected, since it is the sum of the organ dose contributions from different body organs. Another possible reason for this effect might be that the tube current (and, therefore, CTDIvol) has not been adjusted to age and was kept constant for all ages, although a lower tube current would result in the same image quality for the smaller bodies. Our findings were in same manner as Houda et al.,21 in which organ-absorbed doses in head CT scans for adults were higher than the newborns. However, our results were in contrast with that of Thomas et al.37 only in terms of the group of the lowest effective dose. He suggested that the lowest effective dose belonged 0-year-old children, and then, the dose showed an increase. In terms of the level of dose, our results were in consistent with the study by Theocharopoulos et al.,38 but he suggested that effective dose was constantly decreasing. Chest CTs proved that increased age causes increased SSDE. Figure 1 depicts the upward trend. The average SSDE (or in our case ASDE) of 0-year-olds, 1-year-olds, 5-year-olds, 10-year olds and 15-year-olds were 4.35, 5.9, 6.93, 7.56 and 9.1 mGy, respectively.
The results were in accordance with AAPM report no. 204 and 220.25, 32 Another point which can be considered from the SSDE and effective dose in Figure 1 and Figure S1 in Supporting Information is that the trends of SSDE and effective dose with age are not similar. This could be justified by considering that, in principle, the purpose of SSDE is to provide a dose estimate that is much more patient-specific than CTDIvol (therefore effective dose).
Head CT scan
The results revealed that children head CT effective dose declines with increasing age (Fig. S1 in Supporting Information). The downward trend is the same in male and females. Although the radiation sensitivity of newborns is high, it decreases with age; therefore, the effective dose also decreases. In addition, the size of the body mass of the head exposed to radiation increases less with age than other examinations, which means that sensitivity plays a more important role in the effective dose in paediatrics head CT. In other words, an increase in age results in a larger body mass, therefore, in a decrease in effective dose. With a larger body mass, the distances of the body organs from the radiation field and the absorbed dose distribution in the organs are changed and this will have effect on the effective dose.
A possible reason for this effect could be that the tube current (therefore CTDIvol) has not been adjusted for age and kept constant for all age groups, although a lower tube current would result in the same image quality for the smaller bodies. This downward trend accorded with the results of the study of Houda et al.,21 which suggested a decrease in absorbed dose according to an increase in age. Also, it is in accordance with the findings of the study of Thomas et al.,37 which suggested a constant downward trend with increasing age. The dose level of the study is completely similar to that of these two studies, mentioned above. In comparison with the study by Theocharopoulos et al.,38 the strict downward trend is the same, but the level of dose reported by him was lower. As shown in Figure 1, SSDE goes up with increasing age; the calculated values are in accordance with AAPM report no. 204 and 220.25, 32 SSDE of 0-year-old, 1-year old, 5-year-old, 10-year-old and 15-year-old group was 11.65, 14.81, 16.17, 21.24 and 21.39, respectively. Moreover, the organ dose showed an upward trend with increasing age.
Organ dose results
From the data presented in Figure 2 and Figures S2–S5 (in the Supporting Information) on the organ dose (mGy) for head, chest and abdomen–pelvis CT examinations for male and female, it is clear that the organ dose depends on organ type, examination, patient gender and age. Regarding the dependence of the organ dose on the organ type, it can be mentioned that organs in the CT scan region received higher radiation dose. For example, in head CT examination the dose to brain, salivary gland, oral mucosa, and so on is higher. Due to a similar reason, when the CT examination is changed, the imaging region is changed and therefore the organ dose is affected. Regarding the patient gender, the gender has effect on the radiation sensitivity (therefore on the effective dose). In other words, the biological effects of ionising radiation VII (BEIR VII) report mentioned that females may have a significantly greater risk of suffering and dying from radiation-induced cancer than males exposed to the same dose of radiation.6 However, this is not a matter of reason for organ dose because sensitivity has not effect on organ dose. On the other hand, by change in gender the body anatomy is changed; therefore, the distances of the body organs from the imaging region are changed and this affects the organ doses. Due to a similar reason, when the patient age is increased, the body size is changed, this would have effect on the organ doses. The data on the organ doses in this study are useful to see whether which organs receive a higher dose in a specific CT examination, thereby consider adequate radiation protection strategies to lower the dose to that organ. The radiation protection strategies can include training of the staff, supervision on the execution of radiation protection regulations and optimising radiation exposure conditions.
The fitting models for estimation of SSDE (or equivalent term ASDE) and effective dose from paediatric CT examinations presented in this study were obtained from dosimetric calculation for only one CT scanner model. It is obvious that the obtained results cannot be simply extended for other CT scanner models. Therefore, it is suggested that the models presented in this study be developed for different available CT scanners to evaluate the accuracy of extension of the present results. While this approach has limitations in terms of generalisability, it serves as an initial exploration of the relationship between patient age, scan protocol type and radiation dose. It is important to acknowledge that the development of a universally applicable, scanner-independent dose estimation model would require a more extensive dataset that includes multiple scanner models. The results of this study cannot be used to estimate dose to embryos in CT examinations of pregnant patients, since the geometry of an embryo inside the mother is completely different from that of a newborn, and the maternal tissues surrounding the embryo that absorb part of the primary radiation lead to a completely different exposure situation. Therefore, future studies can be performed to estimate embryo and pregnant women organ dose from CT scans and to develop similar models. In future work, we propose to work with similar patient data and derive the dose distributions in real time using the concept of deep learning, as some studies have recently focused on this.39, 40 This study lacks evaluation of the accuracy of the obtained fitting models using new data or quantitative comparisons with literature, and it is suggested that numerical values, such as ratios or percentage differences, be used to show how the results of the proposed models can be compared among the related literature.
Conclusions
The fitting model presented in this study for SSDE can be used for estimation of SSDE from patient age, and CT examination type in paediatric head, chest and abdomen–pelvis CT examinations. The fitting model for effective dose can be also used for estimation of effective dose from patient age, gender and CT examination type in these examinations. In CT, the absorbed dose to the body organ depends on the type of scan, anatomical region, age and body measurements. The proposed work has shown that if the type of scan, region and age is known, it is possible to estimate the SSDE and effective dose based on the model created in the study. Future work could be based on the patient's body diameter in the study region. It is suggested that the models presented in this study be developed for different available CT scanners to evaluate the accuracy of extension of the present results.
Conflict of Interest
The authors declare no conflict of interest.
Ethics Approval and Consent to Participate
This study was approved as a human study by Shahid Beheshti University of Medical Sciences, following the declaration of the University (approval ID IR.SBMU.MSP.REC.1395.399). The informed consent of patients, parents or guardians was waived. All methods were carried out in accordance with relevant guidelines and regulations.
Open Research
Data Availability Statement
The data used and/or analysed during the current study are available from the corresponding author on reasonable request.