Diagnostic value of colour Doppler ultrasound in differentiating malignant and benign nodules in thyroiditis background
Abstract
Introduction
Differentiating malignant thyroid nodules from benign ones is challenging. Sonography is a non-invasive modality that can be helpful in this regard and is far better than invasive methods like fine needle aspiration (FNA). This study aimed to assess the diagnostic value of colour Doppler ultrasonography in distinguishing malignant and benign nodules of thyroid gland.
Methods
The study involved patients with thyroiditis and thyroid nodules, who underwent sonography. Ultrasound findings were assessed. All the nodules were classified according to the FNA into malignant, follicular nodules and lymphatic. Then, sonography findings were compared between these three groups.
Results
There were 216 nodules, including 108 (50%) malignant nodules, 80 (37%) benign and 28 (13%) lymphatic follicles, were evaluated. Micro-calcification was present in 50 (46.3%) malignant cases, 11 (13.7%) benign cases and 2 (2.1%) lymphatic follicles. Decreased or mixed vascularity was reported in 43 (69%) malignant nodules, 4 (5%) benign cases and 7 (25%) lymphatic follicles. Also, 9.7% and 42% of malignant and benign nodules had peripheral circular vascularity, respectively; however, none of the lymphatic follicles had this finding. With 89% specificity, 49% sensitivity and 73.5% accuracy, calcification with or without decreased or mixed vascularity could differentiate benign and malignant nodules.
Conclusion
Decreased or mixed vascularity with or without calcification shows high sensitivity in differentiating malignant and benign nodules.
Introduction
Nearly 5% of adults have a palpable thyroid nodule that shows a highly prevalent condition in clinical practice. However, about 7% of thyroid nodules are malignant.1 Since thyroid cancer is one of the most curable malignancies, it is crucial to correctly evaluate individuals with thyroid nodules. Diagnostic methods must be accurate and less invasive.2
Despite the high diagnostic accuracy of fine needle aspiration (FNA) in thyroid nodules, it is frequently rejected by individuals due to its invasive, time-consuming and expensive nature.3 High-resolution B-mode ultrasound (US) can detect thyroid nodules and reveal their characteristics, location, number and size. Compared to FNA, the advantage of the US is that it is non-invasive and provides immediate information. Using ultrasound, nodules as small as 2 mm can be identified that could otherwise be overlooked by a physical examination.4 The efficacy of US and colour Doppler ultrasound (CDUS) in identifying malignant thyroid nodules has been studied in the literature.5-12
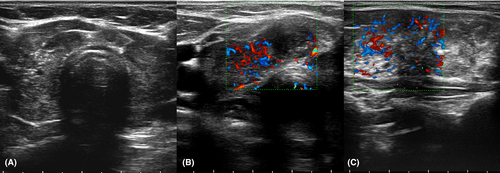
Thyroiditis refers to a broad range of disorders marked by thyroid gland inflammation and lymphocytic infiltration, as well as thyroid fibrosis. Hashimoto's thyroiditis is the most prevalent subtype. Another common type is De Quervain's (subacute) thyroiditis. The condition may also occur after viral or bacterial infections, neck surgery, radiation, pregnancy, or taking certain medications.13 The lymphocyte infiltration in the thyroid parenchyma (lymphatic follicles) causes multi-focal hypo-echogenicity, which is presented as a hypoechoic area with an ill-defined margin14 (Fig. 1). Due to similarity, hypo-echogenicity and indistinct margins of lymphatic follicles can be misdiagnosed as thyroid malignancy.15
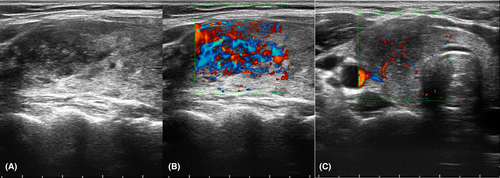
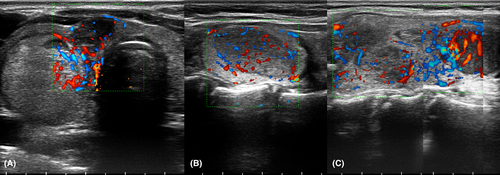
During a long-term thyroiditis, regenerative nodules (benign hyperplastic follicular nodules) can create hyperechoic nodules in the background of hypoechoic thyroid (white knight). In some white knight nodules, degeneration is accompanied by hypoechoic changes that mimic the appearance of malignant lesions (Fig. 2).
Additionally, two benign pathologies including lymphatic follicles and hyperplastic follicular nodules may mimic the appearance of malignant lesions in thyroiditis patients.16 Thyroiditis itself is a risk factor for thyroid cancer, and these patients should be periodically evaluated for malignancy.17 A decrease in thyroid echogenicity pattern in the context of thyroiditis may also cause the appearance of malignant thyroid tumours. Therefore, these situations frequently result in the overtreatment of thyroiditis patients or the failure to detect malignancy in these cases.18 As a result, it may be beneficial to reduce diagnostic errors and unnecessary FNAs by distinguishing these benign thyroid lesions from malignant thyroid nodules in the context of thyroiditis.
It is possible to assess nodular blood flow patterns using CDUS. Although some studies revealed that the malignant nature could be related to hyper-vascular central flow or intra-nodular flow,12 conversely, some studies demonstrated that resistive index value or vascular patterns do not help differentiate between malignant and benign nodules.5, 11, 19, 20 However, there is an ongoing debate over the precise utility of this method in determining whether thyroid nodules are benign or malignant. This study aimed to evaluate the characteristics of ultrasound (B-mode and colour Doppler) and determine its diagnostic value in examining malignant or benign nodules in patients with thyroiditis.
Materials and Methods
Study design, sample and setting
This cross-sectional study was conducted at Omid Cancer Hospital, affiliated with Mashhad University of Medical Sciences in Mashhad, Iran, from January 2019 to January 2021. The study included all patients with thyroiditis and thyroid nodules who were referred at the specified time and met the inclusion criteria.
Patients, who had concurrent thyroiditis and thyroid nodules in sonography, underwent thyroid FNA due to suspicious findings and were referred for further examination. US thyroiditis features can vary depending on the type, severity and phase of the disease. Hypervascular hypoechoic enlargement of the thyroid gland with or without a heterogeneous echogenicity texture is usually the sonography appearance of thyroiditis. Graves' disease shows hyper-vascular hypoechoic enlargement with a homogeneous echogenicity texture. Multifocal hyper-vascular hypoechoic enlargement is seen in sub-acute thyroiditis, and a heterogeneous echogenicity texture is seen in Hashimoto thyroiditis. Peri-thyroid reactive lymph nodes are common, especially at the suprasternal central level. In some cases, thyroiditis diagnosis was confirmed by measuring thyroid peroxidase (TPO) antibodies.
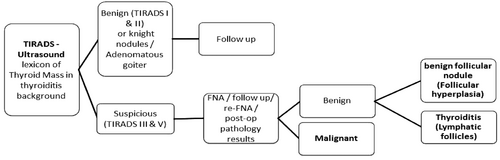
We excluded patients with undetectable thyroiditis on US or TPO, benign nodules (i.e., white knight), spongy nodules (adenomatous goitre) and patients without suspicious findings according to the ACR-TIRADS. The diagnostic approach is presented in Figure 3.
Assessments
Routine sonography of thyroid glands was conducted using an Esoate class C (Italy; Milan) sonography device. Linear transducer with 5–9 MHz frequency was used in this regard. An evaluation of thyroid characteristics was performed, including thyroid echogenicity and thyroiditis type, as well as thyroid size and shape. The volume of thyroid was also measured by ‘three distance volume’ software that is embedded in the sonography device. In case of normal value of thyroid diameter, the mean length is approximately 40–60 mm, with mean anteroposterior diameter of 13–18 mm and mean thickness of the isthmus is 4–6 mm.21 CDUS was performed on nodules associated with thyroiditis to evaluate echogenicity patterns, size, calcification, lymphadenopathy and type of vascularity.
Vascularity types were divided into four groups: peripheral circular vascularity, increased vascularity, decreased vascularity and mixed vascularity. Decreased and mixed vascularity were defined as suspicious vascularity. Peripheral circular and increased vascularity were also defined as benign and non-specific, respectively. All thyroid nodules were classified according to the American College of Radiology Thyroid Imaging Reporting and Data Systems (ACR-TIRADS) criteria. FNA was performed on suspicious nodules, and according to the results of cytology and pathology, nodules were divided into benign nodules (follicular hyperplasia and lymphatic follicles) and malignant. Nodules with borderline cytology results (atypia of undetermined significance and neoplasm) were followed until the final diagnosis (re-FNA or postoperative pathology result) was reached. The pathologist was blinded to the US results. The type of vascularity and also calcification were compared between malignant nodules, benign nodules and lymphatic follicles.
Comparing pathology between benign and malignant groups and types of vascularity between benign and suspicious groups were performed to investigate the diagnostic value of CDUS.
Data analyses
The data were analysed using IBM SPSS software version 20.0 (SPSS Inc., Chicago, IL, USA). Initially, the Kolmogorov–Smirnov test was used to determine the normal distribution. Categorical variables were described as frequencies and percent, and continuous variables were described as mean ± standard deviation (SD). A t-test or Mann–Whitney test was used to compare quantitative variables between benign and malignant groups, depending on the type of distribution. The Chi-square or Fisher's test was used to compare qualitative variables between three groups, including malignant, benign follicular nodule and lymphatic follicle. Sensitivity, specificity and positive and negative predictive value tests were conducted to evaluate the diagnostic value of CDUS. A P-value less than 0.05 was statistically significant.
Ethics
The study protocol was approved by the Ethics Committee of Mashhad University of Medical Sciences (Ethics Code: IR.MUMS.MEDICAL.REC.1398.888).
Results
A total of 216 patients with a mean age of 45.25 ± 13.25 years were included. There were 193 (89.4%) females and 23 (10.6%) males. According to the US findings, 97 (46%) patients were classified as Hashimoto's thyroiditis, 112 (53%) patients as non-specific and 2 (0.9%) patients as typical subacute thyroiditis. Thyroid size was smaller than normal in 33 (15.7%) patients, normal in 79 (37.6%) patients and larger than normal in 98 (46.7%) patients. The thyroid nodules' average size was 24.34 ± 13.0 mm (23.2 mm in malignant cases, 24 mm in benign cases, without a significant difference). Malignant nodules were found in 108 cases (50%), including 99 cases of papillary carcinoma, four cases of medullary carcinoma, three cases of follicular carcinoma and two cases of lymphoma. Eighty cases (37%) had benign follicular nodules (including 45 (20.8%) hyperplastic follicular nodules, 35 (16.2%) adenomatoid goitre) and 28 cases (13%) were lymphatic follicles.
The border of the lesions was examined. A well-defined margin was seen in 51% of malignant masses, 43% of lymphatic follicles and 95% of benign follicular hyperplasia lesions. Regarding calcification of thyroid nodules, 137 (63.4%) cases had no calcification, 58 (26.9%) cases had microcalcification, 16 (7.4%) cases had macrocalcification and 5 (2.4%) cases had both microcalcification and macrocalcification. Microcalcification was observed in 47 (43.5%) of nodules with malignant pathology, 2.1% of thyroiditis nodules (follicle) and 11 (13.7%) of benign follicular nodules. These findings were significantly different between the three groups (P < 0.0001). Macrocalcification was observed in 8.3% of malignant nodes and 7.4% of benign nodes; however, these differences were not statistically significant. The frequency of the different pathologies according to the type of microcalcification and type of vascularity is illustrated in Table 1.
| Variable | Frequency, n (%) | Decreased or mixed vascularity, n (%) | Peripheral circular vascularity, n (%) | Increased vascularity, n (%) | Micro-calcification, n (%) | Micro-calcification ± decreased or mixed vascularity, n (%) |
|---|---|---|---|---|---|---|
| Malignant | 108 (50) | 43 (69) | 5 (45.5) | 14 (40) | 50 (69.5) | 69 (64) |
| Benign follicular nodule | 80 (37) | 4 (5) | 6 (54.5) | 1 (3) | 11 (17.5) | 14 (17.5) |
| Lymphatic follicle (Thyroiditis) | 28 (13) | 7 (25) | 0 | 20 (57) | 2 (3) | 7 (25) |
| P-value | <0.001 | >0.001 | >0.001 | <0.001 | <0.001 | |
| Suggested point | 2 | 0 | 0 | 4 |
Regarding thyroid nodules' vascularity, there was a decreased vascularity in 21 (20.8%) cases, increased vascularity in 35 (34.7%) cases, peripheral circular vascularity in 12 (11.9%) cases and mixed vascularity in 33 (32.7%) cases. CDUS is 69% sensitive and 71% specific in detecting patients with thyroiditis and identifying benign nodules from malignant nodules. This modality also showed a positive predictive value of 79%, negative predictive value of 59% and accuracy of 70%.
Moreover, the diagnostic value of calcification was examined with or without suspicious vascularity. The samples were divided into two categories (calcification, decreased vascularity, or mixed vascularity) as suspicious nodules and (peripheral circular vascularity without calcification) as benign nodules (Fig. 4). Pathology findings of the nodule and calcification with or without suspicious CDUS can have a significant relationship with each other (P-value: 0.001). Calcification and suspicious CDUS were able to diagnose benign and malignant nodules with 89% sensitivity, 49% specificity and 73.5% accuracy, respectively.
Discussion
Two benign pathologies (lymphatic follicles and benign follicular hyperplasia) are commonly present in thyroiditis patients, and they mostly have a typically benign appearance: hypoechoic ill-defined area and white knight nodule. The histopathology of the lesions justifies their typical sonographic appearance. Small round cells in lymph follicles are seen as hypoechoic nodules with indistinct borders, and hyperplastic follicular nodules are seen as echogenic nodules due to Herthle cells and fibrotic bands that create multiple interfaces and multiple sound reflections. The benign hyperplastic follicular nodules create hyperechoic nodules on the background of the hypoechoic thyroid, known as the white knight nodule. Over time, degeneration of these nodules is accompanied by hypoechoic changes that mimic the appearance of malignant lesions.
The lymphocytic infiltration (lymphatic follicles) presents as hypoechoic ill-defined areas and resembles the appearance of malignant thyroid lesions in the US.20 This reduction in echogenicity of the thyroid parenchyma in the context of thyroiditis may result in the disappearance of hypoechoic thyroid tumours. Thyroid cancers in the context of thyroiditis have a more irregular or blurred margin, which makes it harder to distinguish them from nodular thyroiditis.15 In our study, an ill-defined margin was seen in 49% of malignant masses and 57% of lymphatic follicles of thyroiditis. However, more than half of thyroid cancers in these patients have a well-defined border, and in these masses, an appropriate diagnostic approach based on ACR-TIRADS should be performed.
Unfortunately, the cytology results of these patients are often inconclusive, and cases such as atypia of undetermined significance (AUS) and follicular neoplasms are commonly reported. As a result, these conditions often lead to over-diagnosis, over-management and overtreatment of patients with thyroiditis. Therefore, differentiating these benign thyroid lesions in the context of thyroiditis from malignant nodules can help reduce diagnostic errors.
This study evaluated the diagnostic value of US and CDUS in examining malignant or benign nodules in patients with thyroiditis. According to our findings, the size, echogenicity macro-calcification and border of masses could not differentiate malignant nodules from benign ones in patients with suspicious thyroiditis. Micro-calcification and hypo-vascularity (decreased or mixed vascularity) were the best discrimination factors. According to our findings, the sensitivity of CDUS in detecting malignant and benign nodules in thyroiditis was 69%, and the specificity was 71%. The sensitivity, specificity and accuracy of calcification or suspicious CDUS in diagnosing benign and malignant nodules were 89%, 49% and 73.5%, respectively.
There have been several studies performed on the use of CDUS to diagnose malignant thyroid nodules, in which its value was investigated regardless of the thyroiditis background. An investigation by Phuttharak et al. examined the ability of US alone or in combination with CDUS to determine the malignancy of thyroid nodules in 31 patients.22 According to their findings, specificity, sensitivity, negative predictive value and positive predictive value of US were 84.6%, 80.0%, 95.7% and 50.0%, respectively. Additionally, preoperative combined US and CDUS had specificity, sensitivity, negative predictive value and positive predictive value of 96.2%, 40.0%, 89.3% and 66.7%, respectively.22 A combination of US and CDUS improved both the positive predictive value and specificity of malignant thyroid nodules.22
Similar research by Bakhshaee et al.6 assessed CDUS parameters and type of vascularity to differentiate between malignant and benign thyroid nodules in 85 patients. They found that malignancy and the shift to intra-nodular vascularization were significantly correlated (P-value = 0.001). They concluded that vascular pattern and spectral parameters help differentiate benign and malignant thyroid nodules, particularly in cases with suspicious or undetermined FNA.4 Papini et al.1 reported a significant relationship between central vessels and malignancy and between peripheral vessels and benignity (P-value < 0.0001). However, in 20% of malignant nodules, the vasculature was predominantly peripheral.
According to research by Salehi et al.,23 predominant peri-nodular hyper-vascularity was the most typical finding in benign nodules. In contrast, predominance of central hypervascularity was the most typical finding in malignant nodules in CDUS. Predominant central hypervascularity (68%) and exclusively central vascularity (97%) were the most sensitive and specific Doppler sonography findings for malignant nodules, respectively.23 In another study of 1083 nodules, benign nodules typically showed intra-nodular vasculature, but malignant nodules often showed no vasculature. They concluded that vascularity was not as effective as suspicious US features in diagnosing thyroid cancer.19 The reviewed studies examined the value of CDUS in detecting malignant nodules in the context of normal thyroid tissue. Thyroiditis affects not only echogenicity but also parenchymal vascularity and parenchymal hypervascularity is one of the common symptoms of thyroiditis. The literature contains only a few similar studies on thyroiditis. Oppenheimer et al. conducted a study on patients with nodular Hashimoto thyroiditis. In their study, CDUS revealed that 17% of nodules had peripheral hypervascularity, 34% had isovascularity, 14% had diffuse hypervascularity, 32% had hypovascularity and 3% had avascularity.24 According to Chammas' study, malignant lesions had a greater avascularity than benign ones. However, there was no significant relationship between these two entities (P-value = 0.206).20
Based on our findings, in patients with thyroiditis and suspicious nodules, the size, echogenicity macrocalcification and border of masses failed to differentiate malignant nodules from benign ones. In our study, calcification in the US and hypo-vascularity in CDUS improved the sensitivity and specificity for detecting malignant nodules.
There are many signs and points for TIRADS classification. Considering the diagnostic value of the findings of this study and similar research, exact points can be entered in TIRADS. It is suggested that Doppler findings should be included in the ACR-TIRADS criteria in thyroiditis background: two points for decreased or mixed vascularity and four points for microcalcification.
The study also has some limitations. Our study had an acceptable sample size; however, further studies with larger samples are needed to examine the use of Doppler findings in suspicious thyroid nodules in patients with thyroiditis. Due to the high prevalence of thyroiditis and diagnostic challenges in these patients, and especially the limitations of cytology, further studies are necessary to determine benignity and malignancy of the thyroid nodules in these patients.
Conclusion
Considering the high prevalence, it would be ideal to pay attention to the findings of thyroiditis in routine ultrasound examinations. Two benign pathologies (lymphatic follicles and benign follicular hyperplasia) are commonly present in thyroiditis patients, and they mostly have a typically benign appearance, which is hypoechoic ill-defined area and white knight nodule. However, some individuals may mimic the appearance of malignant lesions. More than half of thyroid cancers in these patients have a well-defined border. In these cases, an appropriate diagnostic approach based on ACR-TIRADS should be performed.
Unlike hypervascularity in malignant nodules in the context of normal thyroid, in thyroiditis, reduced or mixed vascularity with or without calcification shows a high sensitivity in differentiating malignant and benign nodules. Paying attention to these findings can prevent the over-management of patients with thyroiditis or missed malignancies with ill-defined borders in thyroiditis. It is suggested that Doppler findings should be included in the ACR-TIRADS criteria in thyroiditis patients.
Acknowledgements
This research was supported by the Vice Chancellor for Research of Mashhad University of Medical Sciences. The results described in this paper are part of a thesis submitted by Masomeh Jaberi for the degree of specialty in radiology. We thank Alireza Omranzadeh for editing the manuscript.
Conflict of Interest
The authors declare no conflict of interest.
Ethics Statement
The patients completed the informed consent forms. Moreover, the study protocol was fully approved by the Ethics Committee of Mashhad University of Medical Sciences in accordance with Helsinki Declaration guidelines (IR.MUMS.fm.REC.1398.888).
Open Research
Data Availability Statement
The dataset generated and analyzed during the current study are available from the corresponding author upon reasonable request and in accordance with ethical issues.